Current and emerging trends in antimalarial drugs:a comprehensive review
2022-11-04SeemaRohillaAnkurRohillaDavinderKumar
Seema Rohilla ,Ankur Rohilla ,Davinder Kumar
1Department of Pharmay,Panipat Institute of Engineering and Technology(PIET),Smalkha 132102,India.2Department of Pharmacology,University Institute of Pharma Sciences,Chandigarh University,Gharuan 140413,India.3Department of Pharmaceutical Sciences,Maharishi Dayanand University,Rohtak 124001,India.
Abstract Malaria is a ubiquitous tropical disease which occurs by the bite of malaria parasite of genus Plasmodium spp.The procurement and treatment of malaria depend on the cost and emergence of drug resistance,chemical compositions of drug molecules,and different complications and toxic effects associated with them.The antimalarials are classified as gametocidal,prophylaxis,blood schizonticides,tissue schizonticides and sporontocides.In addition,new antimalarial drugs have been discussed in the present review that offers the advantage singly or in combination with other drugs.The ridiculous vector control methods,appearance of drug-resistant parasites,and deficiency of effective vaccines against malaria are the main aspects responsible for the expansion of malaria.Hence,the development of a new drug is the need of hour to conquer the clinical failures of traditional chemotherapy.Though,the discovery and development of a new drug is a costly and lengthy process,hence different nanotechnological techniques may recommend hopeful approaches for the procurement of malaria amid minimum side effects.Delivery of traditional anti-malarial drugs in nanoform offers an opportunity to improve their therapeutic efficacy,reduced side-effects by targeted delivery and improved patient's compliance.This review article will critically highlight the different traditional,hybrid and new anti-malarial drugs.Moreover,different nanocarriers discovered for the site specific liberation of antimalarials to enhance the therapeutic efficiency of these drugs have been comprehensively discussed in this review.
Keywords: malaria; Plasmodium;antimalarials;nanocarriers
Background
Malaria is an awfully contagious disorder,which is dangerous for public health all over the world.It is a protozoal infection caused byPlasmodium(P.) spp.,by the bite of infected female Anopheles mosquitoes [1].It introduces different species ofPlasmodiuminto the blood of host and spreads infection[2,3].P.falciparum,P.malariae,P.knowlesi,P.ovale,andP.vivaxare the differentPlasmodiumgenuses that are toxic to humans[4,5].P.vivaxandP.falciparumare the most prevalent source of malaria [6,7],whileP.vivaxproduces a hypnozoite in dormant liver stage that can elicit reversion after primary infection [8].Low birth weight,anemia,and neurological problems are the severe morbidities that have been found to occur in millions of children from malaria prevalent areas.To evade the threat of drug resistance,the accessible antimalarials were fabricated to target the different pestilential blood stages of parasite in patients[9].Lack of proper diagnosis,inaccurate dosing,poor quality of drug and poor patient compliance are the different factors that are liable for disappointment of malaria treatment [1,10].It has been reported that the malaria parasite became resistant from the main classes of conventional antimalarial drugs like aryl amino-alcohols(lumefantrine,mefloquine and quinine),antifolates,antibiotics(doxycycline and clindamycin),4-aminoquinolines (amodiaquine,chloroquine,and piperaquine),napthoquinone (atovaquone),and artemisinin derivatives [11].This led to the dissuasion of monotherapy of these drugs and developed an instant requirement to invent delivery systems that will deliver the suitable quantity of drug at target site,improve patient compliance,reduce drug toxicity,and block parasite transmission to avoid drug resistance and eradicate the asymptomatic and cryptic hepatic symptoms associated with conventional antimalarials [12,13].Antimalarial hybrid compounds,combination therapy,new malarial therapy,or repurposed anti-infective drugs alongwith antimalarial drug entrapped in nanocarriers have presented as the alternative treatment options to eliminate drug resistance[1,14-18].The merozoite surface is adorned with proteins that mediated the incursion of human erythrocyte,so,a drug delivery technique that involved integration of groups to deliver drug at the target sites on parasite surface is needed [19].The present review will comprehensively discuss different combination therapies for malaria,the antimalarial hybrid composites,new malarial therapy and use of nanotechnology to encapsulate conventional antimalarials as new treatment options for malaria.They could represent a possible future solution against malaria by introducing targeted drug release from nanocarriers to enhance the therapeutic efficacy.
Wheel-of-life of malaria parasite
The wheel-of-life ofP.falciparumis shown in Figure 1.Biorhythm of malaria parasite initiates by introduction of sporozoites from the salivary glands of an infected female mosquito in blood of human host.On bite of infected female Anopheles mosquito,the sporozoites enter into the blood of host through its salivary glands and reach the mammalian liver within minutes [20,21],which then grow and form schizonts.These schizonts bursts and release haploid merozoites,which attacks the proteins through precise receptors present on the erythrocyte surface and re-enters into the blood circulation [22].The pathogenic vulnerabilities of these parasites could be beleaguered by minute particles [23].Drug molecules having ability to target the different stages of parasite in liver would provide safety against infection and could eradicate the enigmatic hypnozoite formed byP.vivaxandP.ovale.
The symptoms of malaria are observed during the blood stage as merozoites are discharged from liver into the systemic circulation.These merozoites assault in red corpuscles and begin asexual developmental cycle through trophozoites,rings,and schizonts upto 48 h.In this cycle,some of the parasites developed into gametocytes by the process of gametocytogenesis [13],and send out to the mosquito.After maturation,gametocytes are converted into microgametocytes and macrogametocytes;and leaches into the red blood cell (RBC),which by exflagellation generate male and female gametes in the vital fluid of human host that act as a meal for infected mosquito [23].Thereafter,the fertilization occurs and zygote is differentiated into motile and insidious ookinete.In this,the diploid genome undergoes meiosis [24,25].The existing ookinetes converts into oocysts during passage through the gut wall of mosquito and undergoes endomitosis to produce thousands of daughter sporozoites,which migrates from its gut wall towards the salivary gland of mosquito where the lifecycle instigates again.To eradicate malaria,it is mandatory to invent new drugs that would obstruct the transfer of parasite between the mosquito vector and the host.The invention of new and efficient antimalarial drugs is the need of the hour to eradicate the drug toxicity and to eliminate the risk of drug resistance againstP.falciparum[26,27].
Traditional therapeutics for malaria treatment
Antimalarial drugs are categorized depending on their chemical composition and antiplasmodial potential in the malaria life process(Figure 2).

Figure 1 Wheel-of-life of malaria parasite

Figure 2 Classification of anti-malarial drugs
Quinine
Quinine is extracted from Cinchona bark,which is also known as Cardinal's bark,Jesuits'bark,or sacred bark.It is related to aryl amino alcohol group and is considered as the former victorious drug used to cure malaria.It alters the hemoglobin digestion ability of intra-erythrocytic malaria scroungers that increase the quantity of partially degraded hemoglobin up to toxic level [28].It can be consumed both by oral and parenteral routes,and within 1-3 h accomplishes peak concentrations in blood circulation and is having a half-life of 11-18 h.It binds with alpha-1 acid glycoprotein and works as gametocytocidal againstP.malariaeandP.vivax.It is used in combination with clindamycin to improve its anti-malarial effect[29].The common side effects associated with quinine are cinchonism,impairment of hearing,producing tinnitus,nausea,and headache alongwith blindness and dizziness.In addition,severe adverse effects associated with quinine are asthma,psychosis,hepatic injury,and thrombocytopaenia[30].
Chloroquine
Hans Andersag discovered chloroquine in 1934 as an antimalarial drug to treat harsh malaria.It is reasonable,highly stable,enormously endured by people in high doses [31].Chloroquine has been reported to prohibit the proliferation of parasite during erythrocytic stage by impeding the hemoglobin digestion capacity of parasite.It accruses in thePlasmodiumparasite and forms chloroquine heme complexes that inhibits the assimilation of hemozoin crystal.This complex undergoes peroxidation process and damages the double layer of lipid membrane present on surface ofPlasmodium.The accretion of the chloroquine is diminished in the digestive vacuole of defiant parasite as Pfcrt genes are highly articulated in it.Continuous use of chloroquine in higher concentration for longer duration leads to different side effects like blindness,neuromyopathy,retinopathy and diplopia[32,33].
Mefloquine
During 1970s,Mefloquine was invented as a potent antimalarial drug by the United States Army.It is related to the aryl amino acid group of anti-malarial agents that targets theP.falciparum80S ribosome.It is effective against all five strains of malaria known to affect humans[34].It has been reported to act as a blood schizonticidal agent and forms toxic complexes against the parasite with free form of heme.It is used in prophylaxis of travelers and efficient against the multidrug-resistantP.falciparummalaria.It is safe for pregnant and breast feeding mothers,and has a half-life of 2-4 weeks [35].It gets metabolized into carboxymefloquine by cytochrome P450 3A4 in the liver and this metabolite cause drug interactions [36].The dose-related side effects associated with it include vomiting,nausea and dizziness [37].Due to its neuropsychiatric unfavorable effects,it is contraindicated for psychiatric patients.
Primaquine
Primaquine,introduced in 1950s is an 8-aminoquinoline analogue which is synthesized from plasmoquine.It is a pro-drug that is metabolized by oxidative deamination process with the help of monoamine oxidase A (MAO-A) into carboxy-primaquine,that has been found to exhibit potent activity against hypnozoites [38].It has also been demonstrated that primaquine shows its efficacy against hypnozoites by interfering with its electron transport chain.It generates reactive oxygen species that assassinates the mature gametocytes,dormant hypnozoites,schizonts and developing parasites in liver,liable for reversion of malaria activated due toP.ovaleandP.vivax[39].It is the single commonly accessible antimalarial drug that neuters establishedP.falciparumgametocytes rapidly [40].It produces synergestic effect with a blood schizonticidal agent due to their partial asexual stage activity.It causes rigorous haemolysis in glucose-6-phosphate dehydrogenase (G6PD) enzyme deficient people [41].The deficiency of this enzyme leads to lysis of premature RBCs [42].The severity of haemolysis is based on the dose and level of deficiency.
Atovaquone
Wellcome laboratories launched atovaquone (hydroxy-1,4-naphthoquinone) in 1980s as an antimalarial medicine,which is active against both blood and liver phases ofPlasmodiumparasite,and hence used as a broad-spectrum antiprotozoal agent [43].It has shown inhibition of mitochondrial electron transport chain of parasite without causing any harm to host mitochondria.During infection at erythrocytic stage,mitochondrion of merozoite form parasite,in presence of dihydroorotate dehydrogenase enzyme converted dihydroorotate into orotate and syenthesized pyrimidine ring.Further,GlaxoSmithKline developed Malarone (mixture of proguanil and atovaquine) for the threapy and protection ofP.falciparummalaria.Proguanil is quickly absorbed while atovaquone is weakly absorbed from the gastrointestinal tract.It is available in different combinations like for adults(Proguanil (100 mg)and atovaquone(250 mg))and for pediatrics (proguanil (25 mg) and atovaquone (62.5 mg)).It is a potential broad-spectrum antiviral drug that acts potentially by influencing viral RNA replication,by inhibiting the biosynthesis pathway of pyrimidine [44],or prohibiting the viral entry by interfering with viral glycoprotein-mediated membrane fusion [45,46].It is found to be active against arboviruses,chikungunya virus,dengue virus and Zika virus [44,45].
Tafenoquine
Tafenoquine is an 8-aminoquinoline derivative and has been approved as monotherapy in dosage of 200 mg/day for 3 days and then followed by weekly maintenance doses approx.200 mg thereafter for travelers’prophylaxis [47,48].It is the single drug that can be used for once-weekly prophylaxis in chloroquine-and mefloquine-resistant parasites and in combination with chloroquine for the preclusion of reversion ofP.vivaxinfection [49].Tafenoquine destabilizes the cellular homeostasis in established hypnozoites and metabolizes into highly active and unstable multiple hydroxylated species that further converts into quinoneimine metabolites.Under aerobic conditions,these metabolites can be reconverted into the hydroxylated derivatives leading to redox recycling and accretion of hydrogen peroxide.The parasite of infected hepatocytes was demised due to accumulation of reactive oxygen species [50].It can cause rigorous hemolytic anemia in G6PD-deficient persons.G6PD deficiency is an inherited X-linked genetic disorder that is widespread in malaria endemic regions and thus affects a huge population that is vulnerable to malaria contagion [50].
Artemisinin
Artemisinin is sesquiterpene lactone peroxide obtained from the leaves of Artemesia annua shrub also known as Qinghao in China[51,52].Endoperoxide bridge of Artemisinin is responsible for its activity againstPlasmodiumspecies [53].This bridge on rupturing generates a highly reactive oxygen species that can alkylate sensitive proteins and cellular metabolites,leading to the demise of parasites [54,55].Artemisinin and its derivatives like arteether,artesunate dihydroartemisinin,and artemether are highly efficient against blood and early gametocyte phases ofP.falciparum[56].These derivatives solved the problems like solubility and bioavailability that were associated with artemisinin.Among different derivatives,artemether as oil-soluble is delivered intramuscularly whereas dihydroartemisinin and artesunate are water-soluble and delivered by oral route but in severe cases artesunate is administered via intravenous route.The combination therapies are used to avoid the probability of resistance due to oral monotherapy [52,57].This combination therapy is highly effective and suggested as first-line treatment for simple malaria.To improve the efficacy of artemisinin,different monomers like dimers,trimers,and tetramers have been amalgamated [58,59].Artesunate is a polar derivative that can be delivered by different routes like rectal,oral,intravenous and intramuscular.
New antimalarial drugs
The different projects related to antimalarial drugs for the discovery and launch of new antimalarials in market is supported by MMV(Medicines for Malaria Venture) since last decade.MMV in collaborations with its partners has widened the scope of antimalarial drugs.Different drugs and their combinations are under clinical trials.A list of new drugs is shown in Table 1.

Table 1 List of new anti-malarial drugs under clinical trial
KAF156/Lumefantrine
A team from the Genomics Institute of Novartis Research Foundation identified a new antimalarial drug KAF156,belonging to imidazolopiperazine class,which is also known as ganaplacide[60].It is highly effective and more biocompatibile than other formulations[61].It could block transmission,avoid infection and cure acute malaria as preclinical studies evidenced the antimalarial activity of KAF156 against different stages ofPlasmodium[62].Its pharmacokinetic (PK) profile from results demonstrated it as a well tolerated single-dose regimen for 3 days without any adverse effect in humans [63].Currently the combination KAF156 and lumefantrine is under clinical trials in phase IIb of that evidenced its improved bioavailability in daily administration [64].KAF156 has shown a fast clearance rate against the defiant strains ofP.vivaxandP.falciparum[65].Thus,it is introduced as a next generation antimalarial candidate,with enhanced charcteristics.Further investigation is needed to be conducted in order to recognize its mechanism of action and to identify its activity alongwith safety and efficacy on simultaneous administeration of lumefantrine.
Artefenomel
OZ439 is a novel synthetic peroxide anti-malarial candidate,also known as Artefenomel due to similarity of some of its chemical groups with artemisinin derivatives [66].Its preclinical studies evidenced its good antimalarial properties with minimum adverse effects in rats[67].Furthermore,the outcomes from phase I clinical trials confirmed its safety and results from phase II that evidenced its parasitemia clearance subsequent to a solitary dose [68].It has potential against artemisinin-resistantPlasmodiumstrains [69].
Ferroquine
Ferroquine has potential to avoid chloroquine resistance towardsPlasmodium[69].It has been shown to generat hydroxyl radicals due to formation of the ferriquinium salt in aerobic environment of the digestive vacuole of malarial parasites due to emendable one-electron redox reaction.This causes lipid peroxidation near to the membrane of digestive vacuole that inhibits the formation of hemozoin.The generation of reactive oxygen species (ROS) leads to death of the malarial parasites.Due to long half-life,it can be used as a candidate in combination therapy for malaria treatment [70].It is also effective against artemisinin combination therapies(ACT)-resistant malaria and all asexual stages of parasite [71].Recently,the combination of artefenomel-ferroquine is under phase IIb of clinical trials to evidence its efficacy and safety as a solitary dosage regimen.This amalgamation is a potent TPP1 candidate with excellent anti-malarial properties.It has long half-life and has a limitation not to assault all gametocytes.
Cipargamin
KAE609 or Cipargamin is an antimalarial drug of spiroindolone family.It was discovered by Novartis,Wellcome Trust,MMV,and the Swiss Tropical and Public Health Institute in partnership.It has been reported to show potent activity against all blood stages of parasite[72].It has shown potent action against different stages ofP.falciparum,[73],including gametocytes.It blocked the transmission of infection in single-or multiple-dose regimen [74].Phase II of clinical trial evidenced different advantages of KAE609 like rapid action,an excellent safety profile,desired potency and exceptional efficiency against simple malaria [83].Now KAE609 is under consideration to study its efficacy as single dose regimen against uncomplicated or severe falciparum malaria [84].Outcomes of Phase II clinical study of cipargamin evidenced it efficacy againstP.falciparumandP.vivaxmalaria [75].
MMV048
A research group from the University of Cape Town and Griffith Research Institute for Drug Discovery in collaboration invented a novel antimalarial drug MMV048,also known as MMV390048 from the aminopyridine class [60].It is active against numerous asexual blood phases of the parasite,alongwith maximum efficiency against the schizont form.It is a broad spectrum antimalarial candidate having efficacy against gametocytes that blocks transmissions and suitable for treatment.The outcomes from preclinical studies conducted on animals demonstrated its potential as a prophylactic agent,transmission-blocker,and as a single-dose curative therapy.It has long half-life and is effective orally against different liver stages of parasite [76].Different clinical trials were conducted on MMV048 to evidence its safety,tolerability,and to recognize the PK profile of drug.Their results demonstrated the safety and effectiveness of drug as a solitary-dose case-management drug [77].Further studies are needed to be conducted to recognize the precise safe dosage and synergestic combinations of MMV048 with other drug partners.Its teratogenicity potential limited its application by MMV.
M5717
The Drug Discovery Unit from the University of Dundee and MMV in collaboration produced a product M5717,which belongs to quinoline-4-carboxamide scaffolds family.Primarily,it is also known as DDD498.It has shown inhibition of the elongation factor 2 ofP.falciparum[78].The outcomes of preclinical studies have evidenced the exceptional blood stage activity of M5717 without any severe side-effects,and confirmed its ability as single-dose regimen [79].The phase I of clinical trial was conducted to evaluate its PK details,safety,tolerability,and parasite clearance in fit persons followed byP.falciparuminfected persons[80].It has long half-life and is suitable for solitary-dose regimen when amalgamated with other immediate-acting molecules.As it has activity against liver-stage schizonts,so it is considered as a TPP2 candidate.More studies are needed to evidence its safety,efficacy,and PK profile,as well as for the estimation of resistance evolution.
P218
P218 is active against bothP.falciparumschizonts in the liver stage and the blood stages ofPlasmodium[81].It can be administered parentrally as a single dose due to its long half life.This drug is developed by collaboration of Janssen and MMV.The foremost studies conducted in phase I of clinical trial demonstrated its good tolerance,safety,and PK profile and confirmed its antimalarial potential [82].The subsequent studies of phase I clinical trials were conducted to confirmed its safety and admissibility with excellent protective efficacy.It has a short half-life that may limit its future development as antimalarial agent and discontinued by MMV [82,83].
PA92
PA92 is a pyrazoleamide derivative that affected the cation pumping and induced a rapid disruption of Na+regulation in the blood-stage of intraerythrocyticP.falciparumparasites.An increase in Na+in the cytoplasm of parasite is predicted to increase the intake of water,swelling of cells and eventually cause bursting of the parasite.It has shown prohibition in the creation of male and female gametes [84,85].PA92 led to quick clearance of parasite when given orally toP.falciparum-infected immunodeficient mice [86].Preclinical studies evidenced its safety margin,high oral bioavailability as well as transmission blocking potential.
SJ733
SJ733 is a dihydroisoquinolone derivative that is responsible for fast apprehension of Na+homeostasis in the parasite.This disturbance leads to different physical alterations in the infected cells like augmented membrane firmness and externalization of phosphatidylserine,regular erythrocyte suicide.It has shown persuasive potential against erythrocyticP.falciparumand acquiesced quick parasite clearance,as clinically studied inP.falciparum-infected immunodeficient mice [87].The outcomes from Phase 1 clinical studies and PK/PD models demonstrated that due to moderately clearance rate of SJ733,it is used as a curative dose in pharmaco-enhanced therapy.The preclinical studies and phase I clinical trials were conducted to identify its pharmacokinetic and safety profiles [88].It is used as anti-malarial in multiple doses.
Combination therapy
Different combination therapies have been reported to show potent antimalarial effects,which are:
(1) Artefenomel-ferroquine: This is a combination synthetic ozonide based artefenomel and a 4-aminoquinoline based ferroquine.Artefenomel have elimination half-life in the range of 46-62 h [89].The main aim of combination therapy is to make a single-dose remedial therapy.Ferroquine has a long elimination half-life(16 days)and has potential to retain its activity against chloroquine-and piperaquine-resistant parasites.It has been found effective to treat uncomplicated falciparum malaria on combination with artesunate but it is fairly effective as monotherapy [90].
(2) In Lumefantrine-KAF156: This combination is a potent imidazolopiperazine and an aryl-amino alcohol are given simultaneously.It has an elimination half-life of 44.1 ± 8.9 h [65].A new formulation of lumefantrine in solid dispersion can be given once daily to study their safety,efficacy and pharmacokinetic profile[64].(3) Fosmidomycin-piperaquine: Fosmidomycin is an inhibitor of isoprenoid biosynthesis used as antibacterial drug.It has a good safety profile[70].
Antimalarial hybrid compounds
This has been demonstrated that the hybrid compounds are more efficient againstPlasmodiumparasite than the individual drugs.The antimalarial activity of these compounds was depended on the design and the type of the linker between the hybridized molecules.Some hybrid compounds have shown cytotoxic effects on mammalian cells.Antimalarial hybrid compounds are categorized according to pharmacophores that are hybridized simultaneously such as artemisinin-based hybrid compounds and non-artemisinin hybrid compounds.
Artemisinin-based hybrid compounds
Smit et al.esterified chalcones with dihydroartemisinin to form dihydroartemisinyl-chalcone esters [91].These compounds have shown efficacy against both chloroquine-resistant and sensitive strains of parasite.The antimalarial activities of these compounds are similar to dihydroartemisinin but more effective than artesunate against the W2 and 3D7 strains of thePlasmodiumscroungers.Thermally,these hybrids were found to be more stable than dihydro-artemisinin,hence they can be stored at hot environments and in sultry malaria-endemic areas [91].Lange et al.attached ferrocene via piperazine linker with dihydroartemisinin and prepared a new artemisinin-based hybrid compounds.They were found effective against both chloroquine-resistant and chloroquine-sensitive strains ofP.falciparumparasites [92].These hybrids did not induce cross-resistance.Moreover,they were highly selective towardPlasmodiumparasite than mammalian cells.Capci et al.combined artemisinin with different selected natural products to produce new hybrid compounds[93] and demonstrated their good antiplasmodial efficacy than individual drugs.They are more effective than artesunic acid and chloroquine.Wang et al.hybridized artesunate with quinoline derivatives to improve their antimalarial activity.This compound has shown a significant decrease in parasitemia [94].Furthermore,Walsh et al.used ester linkage to hybridize dihydroartemisinin with quinine carboxylic acid[95]and demonstrated good antimalarial activity than the individual artemisinin and quinine.Joubert et al.hybridized artemisinin and acridine pharmacophores by an aminoethyl ether connecter by a microwave-assisted radiation method [96].These compounds have shown good antiplasmodial activity against both sensitive and resistant strains of chloroquine.These compounds showed seven-fold more effectiveness against both NF54 strain ofP.falciparumand the gametocytocidal strain due to ethylenediamine linkage than chloroquine[97].
Nonartemisinin-based hybrid compounds
Quinoline-based and ferrocene-based hybrid compounds are other compounds that have been synthesized from artemisinin derivatives.They are also effective againstPlasmodiumparasite on the basis of thePlasmodiumlife cycle.
Quinoline-based hybrid compounds.Bhat et al.incorporated 4-aminoquinoline with 1,3,5-triazine and primed a sequence of 4-aminoquinoline-based hybrid compounds [98].In vitro preclinical studies were conducted to evaluate its antiplasmodial potential against chloroquine-sensitive and resistant strains ofP.falciparum.The antiplasmodial activities of these compounds are due to presence of different functional groups like fluoro,chloro,and morpholino on aromatic ring.They have similar potential like chloroquine against both strains ofP.falciparumbut highly active than proguanil.The docking studies were used for further investigation of antiplasmodial activities of these hybrids on wild type and quadruple dihydrofolate reductase-thymidylate synthase ofP.falciparum.The antimalarial activities of hybrids enclosing 4-aminoquinoline and 1,3,5-traizine are due to existence of aromatic lipophilic side chain.They act by inhibiting the production of beta-hematin [97].Maurya et al.syenthesized hybrid compounds from 4-aminoquinoline-pyrimidine and evaluated their in vitro antiplasmodial efficacy against both chloroquine-susceptible and resistant strains ofP.falciparum[99].These hybrid compounds have shown good antimalarial activity than the standard drug.Docking studies on Pf-DHFR demonstrated the active position for attachment to heme.Thus,heme is an interesting target site for hybrid compounds [100].The antimalarial activity of hybrid compound is due to existence of m-nitrophenyl substituent at C-4 position of the pyrimidine ring.The hybrid molecule with a three-methylene spacer has low antimalarial activity than a hybrid molecule with four-methylene spacer.The incorporation of an eliphatic chains with a piperazinyl linker diminsihed its antimalarial activity.The polymerization of heme to hemozoin is delayed by head to head piling of the quinoline moiety with the heme,which is encouraged by steric restriction occurred due to piperazinyl linker[101].Kholiya and coworkers synthesized hybrid compounds from 4-aminoquinoline-piperonyl-pyrimidine that were more active than chloroquine.The antimalarial activity of hybrids is based on the position of pyrimidine ring on 4-aminoquinoline-piperonyl intermediates [102].Barteselli et al.synthesized novel indenoquinolines hybrid compounds and examined them against chloroquine-resistant strains ofP.falciparumin vitro studies [103].The existence of aminoguanidine functional group,methylpiperazinoethylamino and piperidino-ethylamino moieties augmented the antimalarial activity of hybrids.The antimalarial activity of the hybrid molecules can also be enhanced by introduction of the quinolineamine group among the trifluoromethylquinoline ring and the non-polar region.The hybrid molecule with 3-methyl-1,2,4-triazole substituent has more antimalarial potential than chloroquine [104].The antiplasmodial activities of hybrids can be enhanced by inserting alanine moeity in between the dioxoisoindoline core and amide linkage.The antimalarial activity of primaquine hybrids can be improved by introduction of chlorine group at 7th position [105].Moreover the antimalarial activity of 1,3-dioxoisoindoline-4-aminoquinolines hybrid compounds’ can be augmented by increasing the length of their chain which is adequate in β-alanyl and glycyl bonded compounds [104].
Ferrocene-based hybrid compounds.Kumar et al.primed and evaluated a series of ferrocenylchalcone-β-lactam hybrid composites against chloroquine-resistant and sensitive strains ofP.falciparum[106].The antiplasmodial efficacy of the β-lactam nucleus is increased by ferrocene moiety.The moiety present at N-1 position of β-lactam ring inclined the antiplasmodial activity of the hybrid.Raj et al.amalgamated and observed in vitro antimalarial activity of 7-chloroquinoline-chalcone and 7-chloroquinoline-ferrocenylchalcone hybrid compounds against the chloroquine-resistant strain ofP.falciparum.Different methods like increasing the length of carbon chain and introducing methoxy group as a side chain at the para position of another ring on chalcones can be used to enhance the antiplasmodial activity of these hybrids compounds[107].The studies revealed the safety,efficacy and selectivity of these hybrid compounds against mammalian cells andP.falciparum.Garcia-Barrantes and coworkers premeditated and amalgamated novel hybrid composites by 3-(ferrocenylmethyl)-1,4-naphthoquinone and then investigated them in vitro against chloroquine-sensitive and resistant strains ofP.falciparum[108].Ferrocene molecule is allied with a basic alkylamine and 4-aminoquinoline covalently to form Ferroquine [109].The outcome of Phase 2 demonstrated its effectiveness either alone or in combination with artesunate against chloroquine-resistant and multiresistant strains of parasite.It forms complex with haematin by targeting the non-poalr site of hemozoin,thus,inhibited the β-haematin formation [110].It undergoes reversible redox reaction and generates hydroxyl radicals in aerobic surroundings of the digestive vacuole ofPlasmodiumscroungers that influenced its stability [111].Chopra et al.prepared ferrocene-pyrimidine hybrid molecules.The lipophilicity and antimalarial potentials of these compounds can be increased by inserting ethyl and isopropyl as a side-chain at the C-5 position of the pyrimidine ring[112].
Nanotechnological approaches for malaria therapy
Recent antimalarial therapy has been known to relay on chemotherapy that includes severe lethal effects and appearance of resistant parasites,which ultimately causes unsuccessful malaria therapy.The development of new antimalarial therapy is the need of the hour to prevail the clinical failures encountering during therapy.The development of new drug is a time consuming and expensive process [113].Various charitable organizations like MMVs,different research institutions,universities and pharmaceutical industries have planned and amalgamated new antimalarial compounds and evaluated them in different in vitro and in vivo models againstPlasmodiumparasite [114].The researchers have to face great challenges to discover new drugs for malaria therapy due to speckled positions of malaria parasite during erythrocytic and exo-erythrocytic stages in the host,complication of parasite life cycle and deficient information about pathology and biology of malaria parasite[115].In recent times,nanotechnological approaches have achieved importance due to improved safety and efficacy alongwith targeted drug delivery [116].Nanotechnologies play an important role for pharmaceutical and biotechnological industries in designing and preparation of nanocarriers encapsulated with antimicrobial agents and in avoiding the toxic effects associated with them[117].The main aim of malaria therapy with nanocarriers is the targeted delivery of drugs in parasite infected hemocytes and intracellular parasitic vacuoles.Moreover,the emergance of nanomaterials would augment the safety,efficiency,modify the solubility and pharmacokinetic profile of drugs,selectivity,prevent drug deprivation and approve sustained liberation of drug directly at target site.Nano-vectors encourage combination therapy by encapsulating more than one drug to produce synergistic effects [118].Different nanocarriers like solid lipid nanoparticles (SLNs),liposomes,metallic nanoparticles,nanostructured lipid carriers (NLCs),polymeric nanoparticles and nano-emulsions have been investigated and found applications as nanocarriers for targeted drug delivery [119].Surface adorned antimalarials loaded nanoparticles increases targeted delivery and enhanced its safety and efficacy [28].Various research groups have designed nanobased formulations containing antimalarial drugs and investigated its efficacy againstPlasmodiumparasite-infected animal models.Few conventional antimalarial drugs with purposed nanocarriers antimalarials are given discussed in Table 2.
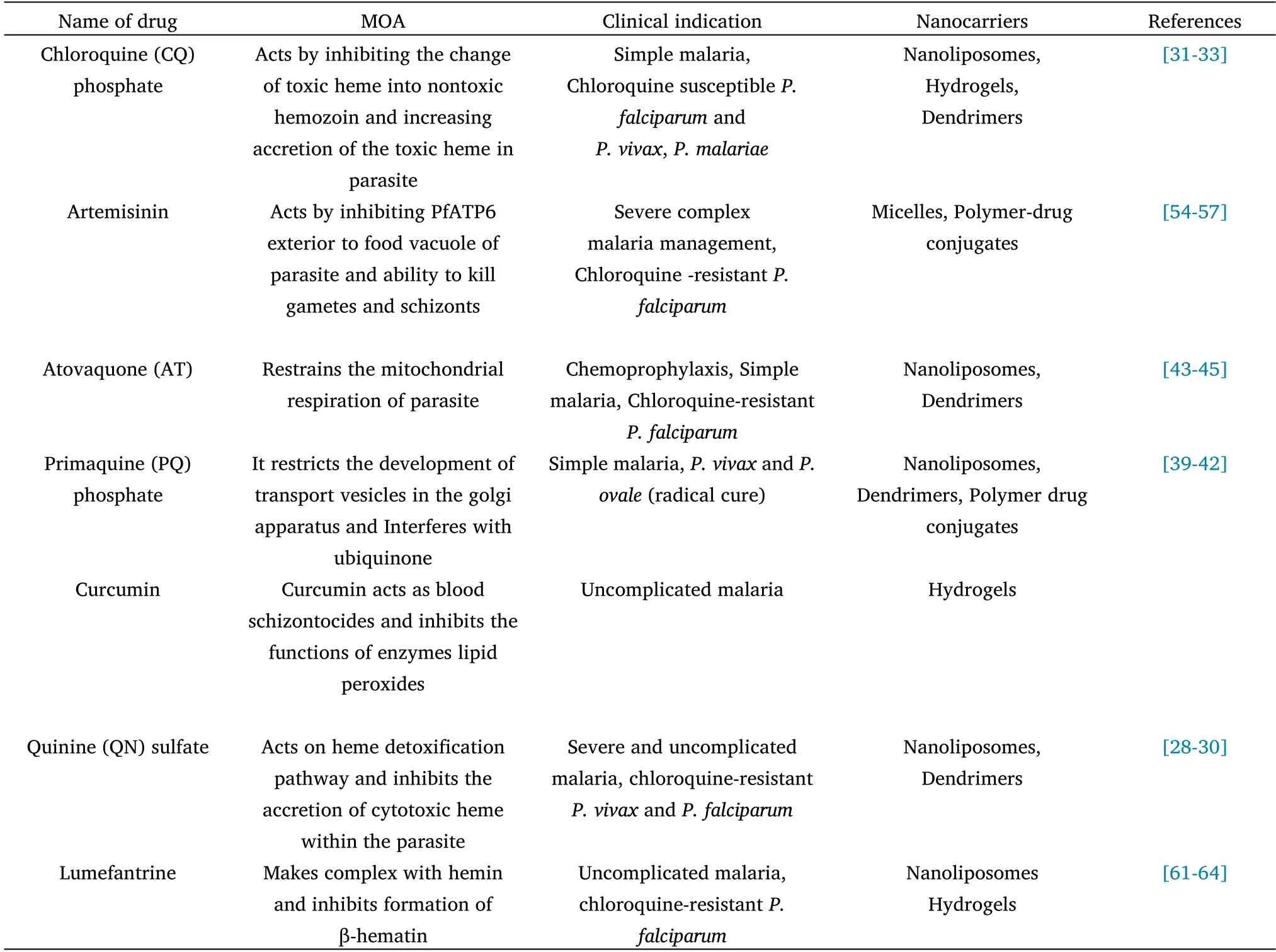
Table 2 List of conventional anti-malarial drugs with their purposed nanocarriers
Liposomes
Liposomes are widely used nano-vectors that are prepared by using cholesterol or other natural phospholipids for the targeted drug delivery.They can modify the cellular and tissue uptake and augment the delivery of medicines to specific sites,thus,improve the therapeutic benefits by site specific delivery of active therapeutic agents[120].These are spherical shape vesicular structures comprised of one or more coextensive lipid bilayers,surrounded by distinctive polar space.Lipid composition,small particle size,charge,hydrophilic-hydrophobic balance,number of lamellae,biocompatibility,ability to incorporate both lipophilic and hydrophilic therapeutic moieties and further morphological alteration by using different ligands and polymers are the unique characteristics that are necessary for site specific targeted delivery of drug.They have prolonged circulation and high retention time[121,122].Bangham,a British haematologist was the first to describe liposomes as ‘smectic mesophases’ and afterward named as ‘liposomes’ by Gerald Weismann,an American physician [123].Their unique characteristics made them a suitable candidate to encapsulate and for targeted delivery of antimalarials [124,125].Ibrahim et al.prepared trans platinum-chloroquine diphosphate dichloride loaded liposomes with potent antiplasmodial activity [126].Aditya et al.used thin-film hydration method to prepare curcminoid-loaded liposomes and united them with α/β arteether [127].The preparation was injected to evaluate its efficacy inP.berghei-infected mice.Rajendran et al.used distearoyl phosphatidylethanolamine-methoxy-polyethylene glycol 2000,soya phosphatidylcholine and cholesterol to prepare liposomes for the targeted deliverance of monensin and artemisinin.This amalgamation has shown outstanding effect in killing the parasites,repressed parasite recrudescence and improved survival [128] at the trophozoite and schizont stages.The liposome formulation encapsulated artemisinin can be used in resistant strain ofP.falciparumand avert reoccurrence of malaria.The improved uptake of liposomes in brain tissue further recommends its potential against cerebral malaria caused due toP.falciparuminfection.Artesunate encapsulated in liposomes with β-artemether for sustained release of drug has been shown to reduce the dose frequency and is found beneficial in malaria-resistant treatment [129].Liposomes acted by different mechanisms like encapsulation of chloroquine in pH-sensitive liposomes or membrane fusion have been reported to conquer drug-resistant malaria [125].However,their use is limited in drug delivery due to cytotoxic effects,expensive production and complicated storage and sterilization.Recently,polyethylene glycol,phosphatidylglycerol and phosphatidylethanolamine have been put in combination in order to prepare negatively charged liposomes for the targeted delivery of antimalarial drugs[29].
Solid lipid nanoparticles(SLNs)
SLNs,launched in 1991,include the inner core composed of solid lipid and surfactants[130].The matrix of SLNs is composed of lipids having high melting points [131-133].The lipid core of matrix regulates the discharge pattern and protects the entrapped drugs from enzymatic and chemical deprivation [131].Small particle dimension,elevated drug loading capacity,huge surface area and the interactivity of segments at the interfaces are the exclusive characteristics of SLNs that made them interested candidate to encapsulate nutraceuticals,pharmaceuticals and other materials [134].Lipid-based formulations have been known to improve the bioavailability of formulations,hence used as a carrier to deliver drugs in different parasitic syndromes like malaria,leishmaniasis,tuberculosis,human African trypanosomiasis and cancer [135,136].Dihydroartemisinin encapsulated in SLNs improved the water solubility,pharmacokinetic and pharmacodynamics properties alongwith potent anti-plasmodial activity [137].The antimalarial activity of chloroquine loaded SLNs can be improved by modifying the surface of nanoparticles with heparin against chloroquine sensitive strains ofP.falciparum[138].The safety and efficacy of lumefantrine and artemether has improved after encapsulation in SLN [139].Transferrin and quinine dihydrochloride are conjugated to encapsulate in SLNs for targeted delivery of drug in brain to treat cerebral malaria [140].
Nanostructured lipid carriers (NLCs)
Nanostructured lipid carriers (NLCs) are used as a substitute of SLNs as the second generation lipid carriers in different therapeutic applications to nullify the complications associated with SLNs.The NLCs are drug-delivery system with different benefits like improved permeability,solubility and bioavailability,storage stability,site specific delivery,diminished toxicity and extended half-life [141].NLCs are gaining value and have been broadly investigated due to their exceptional potential like non-immunogenic character,biological compatibility and harmless behavior [142].Artemether-loaded NLCs have shown more prominant antimalarial activity without any safety issue than sole artemether againstP.bergheiANKA-infected C57BL/6 mice[143].World Health Organization(WHO)permitted a mixture of artemether-lumefantrine in fixed amount for malaria therapy,but their use is restricted due to troubles of little solubility and deprived oral bioavailability.The anti-plasmodial efficacy of NLCs-loaded curcumin is much better than free curcumin againstP.berghei-infected mice[144].
Metallic nanoparticles
Nanoparticles prepared from oxides of different metals like aluminium,chloroauric acid,copper,iron,silver nitrate and zinc are extensively used for diverse medical applications [145].Silver based nanoformulations have been used to cure numerous microbial contagions.Silver based nanoparticles have revealed their efficacy againstP.falciparum[146],which act by degrading the β-hematin.The anti-plasmodial activity of metal nanoparticles is enhanced by adorning their surface with poly 4,4′-diaminodiphenyl sulphone(PDSS).The aqueous extract ofMomordica charantialeaf has been used as a stabilizer and reducing agent to manufacture titanium oxide(TiO2) nanoparticles to screen its efficacy againstP.falciparum.These nanoparticles have shown protective effects against chloroquine-sensitive and resistant strains ofP.falciparum[147].Artesunate encapsulated in surface modified iron-oxide nanoparticle are more efficient against theP.falciparumthan free artesunate.They showed their anti-plasmodial effects by enhancing the release of reactive oxygen species in parasitic food vacuoles[148].
Emulsomes
Emulsomes (nanoemulsions) are new colloidal nanocarriers,having the inner core comprised of solid lipid surrounded by a phospholipid double layer.Lecithin in high concentration is used as a stabilizer for oil/water emulsion.Nanoemulsions are lipid-based drug delivery vehicles but can encapsulate both hydrophobic and lyophobic drugs.Clotrimazole in the form of nanoemulsions have potential against the blood stage parasites inP.berghei-infected Swiss mice [149].Primaquine in form of nanoemulsion has been found effective to overcome the relapsing problem associated with the liver stage of malaria parasites [150].This has been well accepted that a drug in nanoemulsion form shows improved bioavailability [151].Artemether-curcumin is delivered in brain synergistically via olfactory route in form of nanoemulsion to target cerebral malaria.These nanoemulsions have shown valuable outcomes inP.bergheiANKA-infected murine model of cerebral malaria [152].Entrapment of artesunate and quercetin in self-nanoemulsifying drug delivery system augmented the bioavailability of drugs and parasite clearance without any safety issues.
Micelles and dendrimers
In polymeric micelles,the surfactant molecules are self-assembled in nano size range [153].These nanocarriers have elongated polymeric hydrophobic chains and hydrophilic head groups to load drugs according to their nature [154].They have different advantages like improved bioavailability,reduced drug toxicity,sustained and site specific drug release,suitable for hydrophobic drugs [155].Dendrimers are highly bifurcated,monodispersed,polymeric nanocarriers having three-dimensional structures [156].These polymeric materials have less polydispersity index,high biocompatibility and controlled molecular weight [157].They can encapsulate different therapeutic agents and targeted moiety on the basis of functional groups on the exterior of dendrimers.The important applications of these delivery systems include improved drug bioavailability,controlled drug release and reduced drug associated side effects [158].Shi et al.designed polymeric micelles encapsulated chloroquine and docetaxel for combination therapy[159].The micelles loaded with poly(ethylene oxide)-block-poly(propyleneoxide)-block-poly(e-caprolactone)and D-α-tocopheryl poly(ethylene glycol)exhibited in vitro sustained drug release.These micelles are safe to be used as they exhibited less hemolysis rate.Simultaneous administration of both drugs in polymeric micelles can minimize toxic side effects as they are effective in less concentration.Movellan et al.used 2,2-bis(hydroxymethyl)propionic acid (bis-MPA) and pluronic polymers as polymers to encapsulate primaquine and chloroquine in dendrimers [160].These dendrimers specifically targeted thePlasmodium-infected erythrocytic cells than the non-infected erythrocytes that reveal the prospective of dendrimers to purge out the malarial infections.
Hydrogels and in situ gels
Hydrogels are polymeric carriers prepared from synthetic and natural polymers.They have three-dimensional networks like structure [161]with capability to absorb a large amount of water and biological fluids.The porosity of polymeric hydrogels depends on the composition of polymers,the materials from which the polymers are derived and the preparation methods of hydrogels etc.[162].Slabs,nanoparticles,microparticles and films are the different forms of hydrogels[163].Good biocompatibility,non-toxicity,non-immunogenicity,affordability,environmental sensitivity,and their modified drug release mechanism are the unique characteristics of this system.The polymers that are utilized to form hydrogels include pectin,carrageenan,thiolated chitosan,xanthan gum and guar gum are the polymers used to prepare gels that helps in site specific delivery [164].Aderibgbe et al.encapsulated curcumin and 4-aminoquinoline into gum acacia-based hydrogels that revealed sustained and prolonged release of curcumin [165].The hydrogels have good swelling capability,biodegradability and pH sensitivity.The release of chloroquine and curcumin from hydrogel depends on position of drugs in network and the extent of crosslinking of the hydrogel.The hydrogels have potential to work as a delivery system for two antimalarial drugs that can release in different periods of time[166].Dawre and coworkers designed polymeric hydrogels of artemether-lumefantrine by using poly(lactic-glycolic acid).These systems can be administered by intramuscular route.The outcomes of drug release studies were their sustained and controlled drug release profiles.These formulations have potency to cure and eradicate malaria without signs of relapse[167].
Nano-and Microcapsules
Polymeric capsules have been known to entrap the therapeutic agents between core and a protective shell [167] by different methods like self-assembly of block copolymers,monoemulsion polymerization and solidification of droplet shell,etc.[168].The polymeric capsules are classified into two groups on the basis of their dimension i.e.nanocapsules and microcapsules [169].They revealed different advantages like enhanced drug bioavailability,controlled and continued drug release profile,biodegradability,high drug-loading capacity and reduced drug toxicity [167].Velasques et al.incorporated curcumin and quinine in nanosized polymer capsules using polysorbate as the polymer.The outcomes of in vitro evaluation studies revealed reduced toxicity and demonstrated its potential againstP.falciparum[170].
Polymeric nanoparticles
Polymeric nanoparticles have augmented the efficiency of antimicrobial agents by increasing the cellular uptake of therapeutic agents.They are highly biocompatible and biodegradable,and have the ability to disperse from the intracellular membranes [171].These nanoparticles have different advantages like improved drug solubility,bioavailability,high biocompatibility and enhanced safety and efficiency of therapeutic products.Polar polymer-conjugated amino chloroquine has shown more efficacy against chloroquine susceptible strains ofP.falciparum[166].Polymeric nanoparticles loaded curcumin-artesunate and poly D,L-lactic-co-glycolic acid by solvent evaporation method have shown amplified efficacy againstP.berghei-infected Swiss mice with restricted lethal effects [172].Jawahar et al.designed chloroquine and azithromycin loaded polymeric nanoparticles for combination therapy of malaria for their antiplasmodial efficacy [173].Anand et al.encapsulated doxorubicin and artemisinin in β-cyclodextrin polymer nanoparticles.These nanoparticles have improved drug bioavailability with sustained and regulated drug release [174].Oyeyemi and coworkers prepared artesunate and curcumin loaded polymeric nanoparticles by single emulsion method for the targeted delivery of drugs against the parasite schizonts in liver or spleen.The formulation has shown its efficacy in low concentration against malaria parasites [172].
Nanotechnology based vaccines
Numerous research organizations have worked to invent new vaccines to target malaria.WHO provided a list that includes the name of malaria vaccines or its constituents that are under continuous preclinical or clinical phase [175].To improve the immunological response against malaria parasite,recombinant vaccines have been formulated with one or more peculiar antigens.Mosquirix vaccine is the first licensed vaccine to target malaria that gets approval of European regulators in July 2015.The outcomes of clinical trials evidenced its safety and efficacy [176].In this vaccine,the S-antigen of hepatitis B virus was fused with C-terminal ofP.falciparumcircumsporozoite protein,and the N-acetylneuraminic acid phosphatase.The liposomal form of vaccine has shown improved immune results[177].Nanoparticles induced the protective immunity by targeted delivery and by improving the cellular uptake by immune cells [178].Merozoite surface proteins loaded with polystyrene nanoparticles have provided sensible protection against parasites in blood stage [179].A liposomal form of vaccine has been found to be more effective than conventional form.They can induce development of more antibody and T-cell responses by eliciting major histocompatibility complex (MHC) I and MHC II pathways.The development strategies of malaria vaccine need regular improvement due to resistance problem of recombinant antigens.
Green nanotechnology panorama towards malaria
Green nanotechnology has been integrated to invent safe and ecological nanocomplexes that fight against the obstacles distressing the human fitness or atmosphere[180].Andrographis paniculata Nees encapsulated silver nanoparticles were synthesized by green nanotechnology that has shown anti-plasmodial effect againstP.falciparum.Silver nanoparticles encapsulated extracts from the leaves of Neem and Ashoka have ability to restrainPlasmodiumparasites[181].In vitro study of silver nanoparticles containing Catharanthus roseus have demonstrated their anti-plasmodial potential [182].Zinc oxide nanoparticles entrapped aqueous peel decoction ofLagenaria sicerariawere found to inhibit the hemozoin formation,which is mandatory for the survival ofPlasmodiumparasite[183].
Other potential targets
Natural and herbal medicinal products represent a potential target in the treatment and prevention of malaria.Traditionally,the herbal drugs have structured the backbone for the treatment and prevention of malaria over many generations.As,herbal drugs are considered safe,they have been well accepted by many generations against fatal diseases [184,185].Numerous in vitro studies have confirmed the antimalarial potential of stem,root,leaf and fruit extracts role of various herbal plans likeVernonia amygdalina,Gynostemma pentaphyllum,Moringa oleifera,Cryptolepis sanguinolenta,Balanites aegyptiaca,Aloe camperi,Morinda morindiodes,Carica papaya,Azadirachta indica,Ageratum conyzoides,Uvaria chamae,Khaya grandifoliaandTelfaria occidentalison[185-187].Furthermore,some ayurvedic preparations and formulations have shown promising results in the treatment and prevention of malaria.The Central Council for Research in Ayurvedic Sciences (CCRAS) developed an ayurvedic formulation called AYUSH-64,which is a combination of four ayurvedic drugs namelyAlstonia scholaris,Picrorhiza kurroa,Swertia chirataandCaesalpinia crista.The formulation showed potent antimalarial effect in an experimental model againstP.bergheiandP.yoelii nigeriensisin Swiss mice [188,189].In addition,few preparations and formulations likeBisam-jwar-har-lauhandMalaria-samharak-vati,have shown promising potential for the treatment and management of malarial fever [190].The herbal formulations have been considered resourceful in the production of protein drugs by virtue of introduction of genetic engineering technology like molecular.farming in the recent times [191].
Future prospectives
Nanocarriers and green nanotechnology have great future in medicinal industries.The producers of antimalarials would now band up with progression of nanotechnology,but the panorama of the industry will be based on the encroachment in technologies made by omics sciences.They will get benefits in assessing the biological reaction at the cellular and tissue levels against the bioactive compounds and specific antimalarial formulations by using machine learning approaches with big data analysis.This scenario is well-equipped with the concept of precautionary or remedial effect of products.There has been regular endeavor for the radical treatment of malaria.Drug resistance is the biggest difficult hurdle against the success of antimalarial therapy.So,most of the research has to focus in order to conquer the spread and emergence of drug resistance by one or the other methods.There is an urgent need to develop new drugs with new mechanism of action to overcome the problem of drug resistance.Different methods like early cure of malaria disease with combination therapies,emergence of antimalarial hybrid compounds,intermittent protective treatment for pregnant ladies (IPTp),and emergence of nanotechnological based anti-malarial therapies and green nanotechnology will be used to cure malaria in future.
Conclusion
Malaria is a rigorous health concern around the world.Severe toxic effects of accessible anti-malarial drugs,manifestation of drug-resistant parasites,and lacking of suitable vector control procedures and vaccines to treat malaria lead to failure of malaria treatment.Numerous research associations were involved in the work of development of new therapeutic approaches to fight against malaria but no suitable outcomes were observed.However,for the past two decades,the progress of nanotechnological methods has opened the ways to develop safe and eco-friendly nanocarriers for conventional antimalarial drugs to eradicate malaria.The emergence of sophisticated techniques in nanotechnology like development of hybrid compounds,introduction of green nanotechnology,invention of site-specific nano-pores and nano-bio-circuits,the introduction of numerous nanocarriers like solid lipid nanoparticles (SLNs),liposomes,metallic nanoparticles,polymeric nanoparticles,nanostructured lipid carriers (NLCs),and nanoemulsions have explored the new ways to eradicate malaria without any severe side-effects.The reported results like targeted drug delivery,improved drug hydrophilicity,continued and controlled drug release,and maintaining the drug activity in biological environment,suggested that delivery of antimalarials in nanocarriers is a potential approach to be explored in near future.Thus,there is an urgency to invent additional polymer-based nanocarriers to encapsulate conventional antimalarials.Persistent and frequent research on the nanocarriers and hybrid compounds for the delivery of antimalarials will open the new pathways to eradicate malaria.
杂志排行
Drug Combination Therapy的其它文章
- Progress in the study of antiplatelet and antithrombotic effects of salvia polyphenolic acid for injection
- Publicly thanks to peer-reviewers 2022
- Antiurolithiatic activity of Aavarai Bhavanai Chooranam a Siddha polyherbal formulation on ethylene glycol-induced urolithiasis in Wister albino rats
- Theory exploration of ginseng-jujube-licorice group in the prevention and treatment of type 2 diabetes mellitus
