Simulation-based mastery learning in gastrointestinal endoscopy training
2022-09-22HasanMaulahelaNagitaGiantyAnnisaTiffanyKonstantinAriFahrialSyamRoySoetikno
INTRODUCTION
Endoscopy is the gold standard technique for the diagnosis of various gastrointestinal (GI) tract diseases and also allows examiners to directly provide therapeutic interventions if needed.This procedure is performed by a trained gastroenterologist or endoscopic surgeon.The need for endoscopic procedures is projected to increase every year due to the growing prevalence of GI diseases and technical improvements in GI endoscopy[1].Most GI endoscopy training still follows the traditional apprenticeship model of “see one,do one,teach one.” This model relies on the number of exposures to procedural caseloads,which causes varying results among trainees[2].This lack of a standardized curriculum has recently come under intense scrutiny because it is associated with patient safety risks,as trainees cannot safely perform a medical procedure after having observed it only once[3].
A mastery learning model is an approach to competency-based training,in which participants must acquire specific skills before moving on to the next stage of training.The basic principle of mastery learning is that all participants can achieve the highest standard of learning objectives with the minimum possible variation in results.Meta-analyses show that mastery learning significantly leads to skill improvement,has a moderate effect on patient outcomes compared to the traditional apprenticeship method,but might demand more time than other methods.Mastery learning-based training provides consistent positive results and has a beneficial effect on both patient care and the budget spent during the training process[4].
A simulation-based training (SBT) method has been also proposed as an alternative to replace the old teaching method.The use of simulators to acquire psychomotor abilities has been widely studied and recommended by leading educational institutions.With a SBT method,trainees can achieve procedural competence without compromising patient safety,particularly in those procedures that require practical experience and visual-spatial skills[5].Additionally,skills of the operator can be improved and the length of the procedure reduced by using a simulator.Finally,simulators can also be used to evaluate trainee progress[6].
42.Promised:Cinderella promises to leave the ball before midnight but ultimately breaks this promise with her late departure. The breaking of the promise gives Cinderella a slight hint of imperfection and humanity. It also shows how much she is enamored with the prince.Return to place in story.
SBT and mastery learning methods have several benefits over the traditional apprenticeship model.This article reviews the role of simulation-based mastery learning (SBML) in GI endoscopy and describes the planning and management for the implementation of this model,including experiences regarding its application.
Luckily Grumedan did not perceive this, as he was too much occupied in whipping up the frogs, many of whom perished miserably35 from fatigue36, since he did not allow them to rest for a moment
DEVELOPMENT OF GI ENDOSCOPY TRAINING
There he sat, lighted up by the flames from the burning house opposite, both hands holding tightly12 on his red cap, in which lay the treasure; and now he knew what his heart really valued most--to whom he really belonged
The current state of endoscopy training is defined by the conventional apprenticeship model,with a strong emphasis on case/procedure volume and without a formal curriculum.Trainees are usually assigned the minimum number of cases or procedures they need to achieve competency or practical eligibility.The duration of the training program is commonly fixed,and an assessment is conducted near the end of the program.This training method has potential variability in terms of skill outcomes.As trainees might be overwhelmed at the start of the program,the initial cases they encounter can be ineffective for learning.A European survey showed significant differences in various gastroenterology training among 16 European countries,ranging from the minimum number of procedures required,training period,form of supervision to whether some interventional procedures were performed[12].Recently,curriculum-based medical education (CBME) has recently been proposed to improve endoscopy training.The CBME model includes The American Society of Gastrointestinal Endoscopy Skills,Training,Assessment,and Reinforcement program with a curriculum that combines hands-on training,formative feedback,and postcourse skills and knowledge assessments[13].
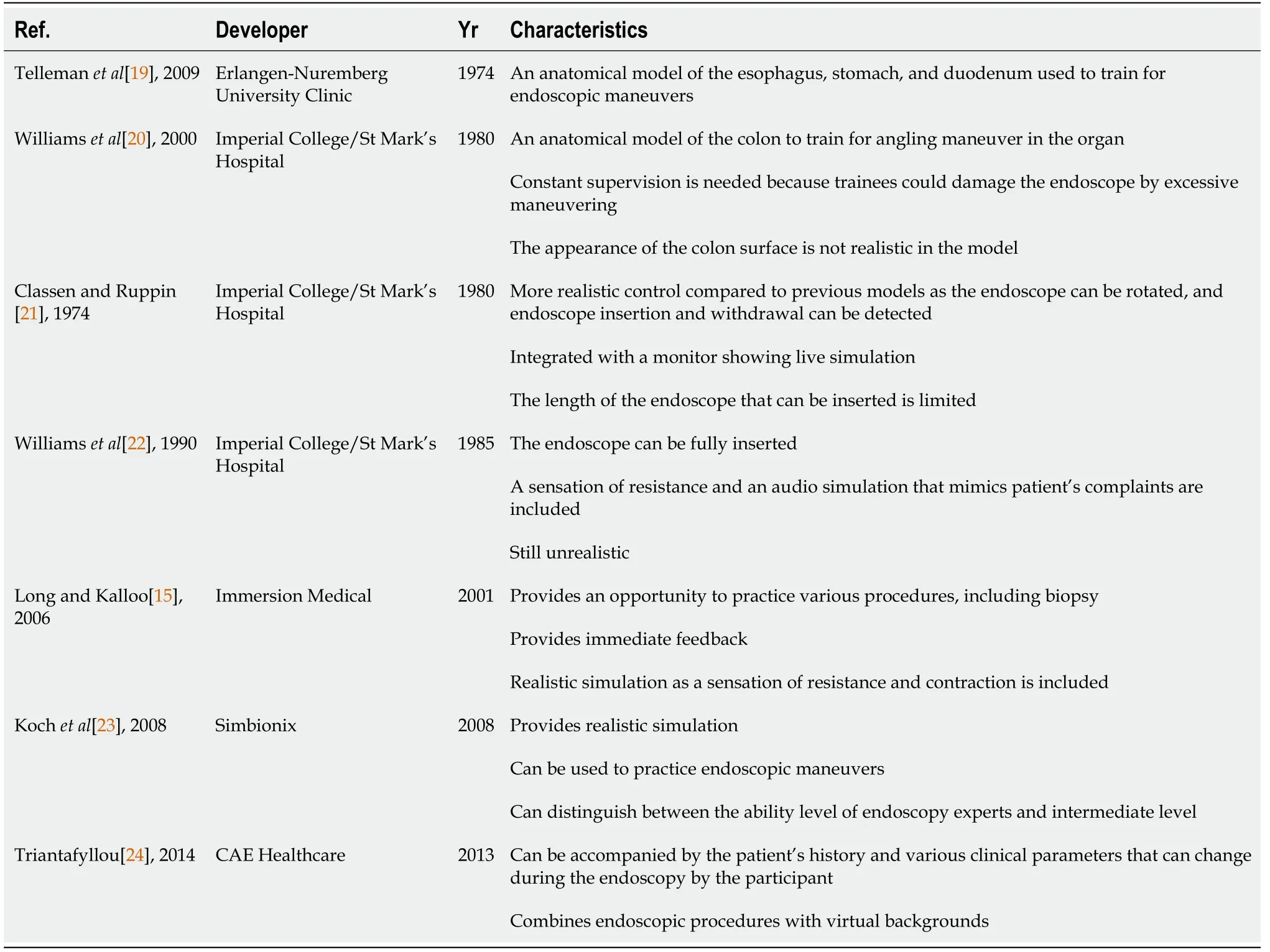
One of the learning methods that has been developed for endoscopy training is a simulated-based approach.Endoscopy simulator models have continued to be developed and advanced in the last decades,ranging from mechanical simulators,animal model simulations,and computer simulators[14].The evolution of endoscopy simulators is described in Table 1.These developments provide opportunities for trainees to learn various diagnostic and therapeutic techniques.Generally,these simulators use an endoscope that is inserted into a mannequin.Consequently,trainees can be more familiar with endoscopic procedures and be able to practice them on an actual patient.Some advanced computer simulators also provide a realistic picture on the monitor and can simulate a patient’s response.The computer simulator also combines training to learn hand-eye coordination,recognition of pathological features,and immediate feedback output[15].A systematic review showed that skills acquired from SBT were transferable to the clinical setting,as participants of SBT scored higher global assessment scores and fewer errors[16].Moreover,forms of simulation that can be considered in endoscopy training include the following[17-24].
Patient simulation: A simulated mannequin that resembles a human with respiration,pulse,and other vital signs is used.This type of simulation can be used for simple physical examination scenarios.
Clinical environment simulation: In this simulation,a room that resembles an actual clinical practice room,for example,an operating room,is prepared.Thus,trainees become more familiar with the actual situation.
Virtual procedure simulation: These simulations have equipment relevant to the procedure,such as esophagogastroduodenoscopy or colonoscopy,and can also present various disease scenarios according to the needs of trainees.
Electronic medical record simulation: This simulation uses artificial data about cases,including disease history and laboratory results,which can be integrated with other systems.
I hadn t heard Ernie talked much about his father. One day, I worked up my courage to ask him what on earth his father had done so that he became such a special person. Ernie said quietly, As a child until I left home at 18, Al came into my room every night, gave me a kiss and said, love you, son.
MASTERY LEARNING IN GI ENDOSCOPY
Mastery learning is a form of competency-based training in which trainees have to achieve specific skills or be deemed good enough to perform a procedure before moving on to the next stage of training.Competence is the minimum level of skill,knowledge,or expertise acquired through training necessary to perform a task or procedure and to ensure that safe and technically successful procedures are carried out and that observations and results are accurate[25,26].Mastery learning focuses on the trainees instead of the patient.The old teaching has resulted in inconsistent teaching,testing,and retention of skills,while mastery learning demands trainees to acquire and maintain specific skills and knowledge through deliberate practice without time limit.Deliberate practice consists of nine elements: highly motivated learners with good concentration,clear learning objectives,an appropriate difficulty level,repetitive practice,rigorous measurements,informative feedback,monitoring and error correction,performance evaluation,and advancement to the next task[27].Mastery learning effectively develops both therapeutic skill and high self efficacy to utilize the skill[28].
When they grew up, he was suddenly seized with a wish to know if they, on their part, truly loved him, and he made up his mind that he would give his kingdom to whichever best proved her devotion
As stated above,the SBML program requires a developed and tested curriculum to ensure that all trainees can achieve competence in endoscopy.Kern
[65] constructed a six-step approach to build an SBML curriculum.The steps are problem identification and general need assessment,specific need assessment,targets and objectives,educational strategies,implementation,and evaluation and feedback.Hospitals and medical institutions should delegate a specific team to plan the SBML curriculum.After planning,a pilot study should be conducted to evaluate satisfaction of trainees with the program and patient outcomes.Once SBML has been implemented,continuous monitoring and evaluation should be performed to maintain the quality of the program[37].
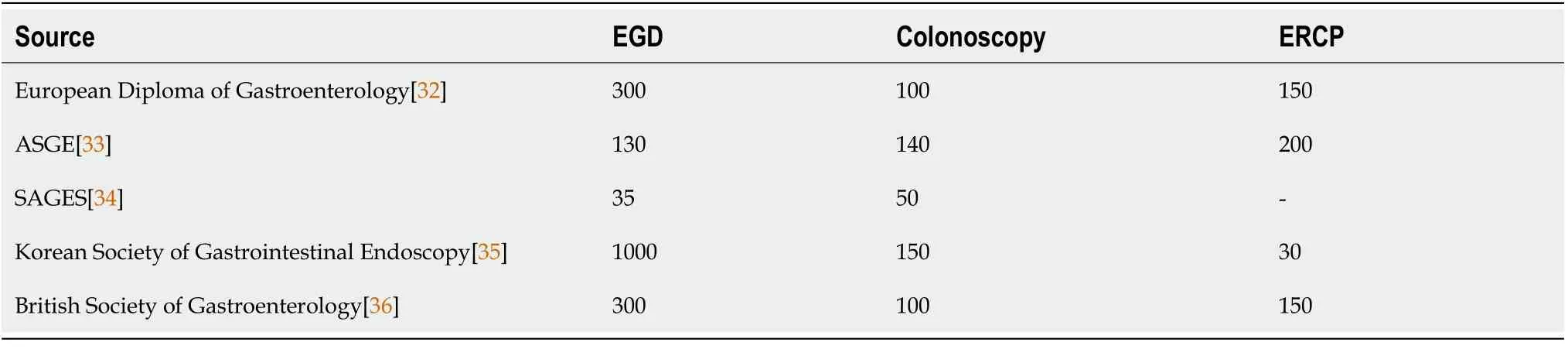
Traditionally,competence in endoscopy is acquired after completing a specific number of recommended procedures based on expert opinions published by medical gastroenterology societies or associations,as described in Table 2.However,according to the aforementioned mastery learning principles,competence cannot be determined only by the number of procedures performed.A defined and detailed assessment tool should be incorporated to objectively assess trainees to deliver highquality care[31].
To ensure competence in mastery learning,two aspects are needed: training and subsequent assessment by endoscopy experts or trainers.Through this training,trainees acquire the necessary technical and cognitive skills[25].Examples of technical and psychomotor skills associated with endoscopy include scope handling and strategies for scope advancement,loop reduction,recall,and mucosal inspection.Cognitive competence reflects knowledge acquired about endoscopy and its application in clinical practice.Cognitive skills include choosing the most appropriate endoscopy test to assess and treat clinical problems,recognizing the lesion,and managing sedation.Crucial integrative competencies to endoscopy include decision-making,teamwork,communication,leadership,awareness of the situation,professionalism,and patient safety awareness[26].
Based on the psychological aspect,three factors underlie mastery learning: Behavioral development,constructive learning,and social cognition.Behavioral development pursues the acquisition and maintenance of technical and communication skills.Clinical thinking,community approach,ethics,advocacy,and regular self-reflection aim to shape social and cognitive constructs.Social cognition is a prerequisite for professionalism.These three aspects support the formation of SBML,which includes a curriculum design to set learning objectives[32-37].
SIMULATION-BASED TRAINING IN GI ENDOSCOPY
Learning targets should be determined from the beginning of the SBML program and arranged according to the SMART acronym: specific,measurable,attainable,relevant,and time-bound[59,60].Trainees,trainers,and supervisors have to understand learning targets before starting the program.This understanding is beneficial because trainees can focus their learning on the important and necessary skills,and trainers and supervisors can provide structured feedback.Feedback is important in SBML and should be delivered in a specific manner: with only one or two important points at a time and preferably immediately after the procedure or simulation to be properly understood by trainees[67,68].Feedback should also be constructive and not vague,allowing trainees to self-reflect and come up with potential solutions[31].
Several studies in other fields of medical procedural training have shown the benefits of SBT and mastery learning over the traditional apprenticeship model.A meta-analysis by Harrison
[40] included 14 studies involving 633 trainees in cardiology procedures and found that SBT followed by structured training provided superior results than traditional methods.The quality of patient care and patient feedback obtained by this method were better than those obtained by a conventional training approach.A meta-analysis by Cook
[41] included 82 studies evaluating SBML in procedural settings such as surgeries and airway management.They found that SBML was significantly better at improving procedural skills than traditional methods but might takes more time.A systematic review on patient outcomes in simulation based medical education also reported small to moderate patient benefits in comparison with no intervention[38].A study published in 2014 revealed the effectiveness of colonoscopy training with virtual simulation in the early learning curve of novices.Performance improvements were also found later during patient-based colonoscopy[42].Another multicenter study found higher objective competency rates during the early phase of colonoscopy training[43].
And when, through the window, she saw the sun thus rising, she said, Cannot I, too, order the sun and moon to rise? Husband, she said, poking25 him in the ribs26 with her elbows, wake up! go to the Flounder, for I wish to be even as God is
A prospective randomized study that evaluated the diagnostic abilities of trainees using upper GI endoscopy concluded that structured SBT was superior to SBT or clinical training alone.This study also found that the use of the simulator was valuable as the first step in developing diagnostic skills to perform upper GI endoscopy,but it was not sufficient to ensure the overall competencies[30].Several reports on SBT for GI endoscopy are described in Table 3.

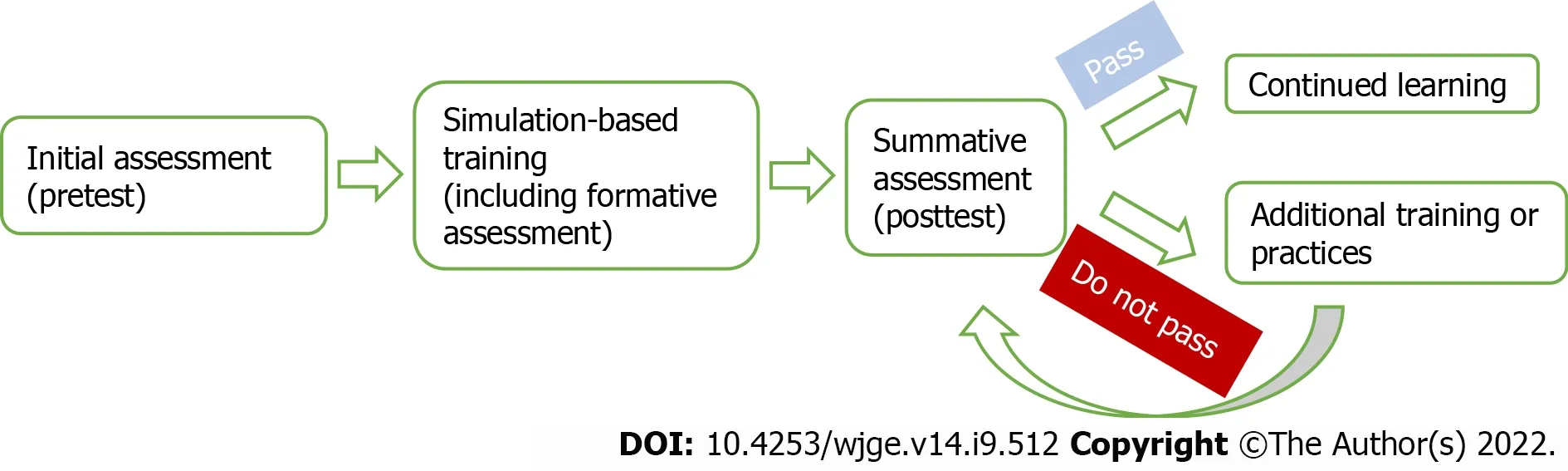
SBML begins with an initial assessment of the knowledge and abilities of trainees.After training,students will be tested again,and training will continue until they meet the minimum passing standards.Once trainees meet the minimum passing standards,they can advance to the next stage of training (Figure 1).Periodic examinations will be conducted along with planned practices to ensure that expected competencies are maintained[37].Some training centers might provide materials for self learning before the simulation starts to improve the initial knowledge of trainees.A study by Cheung
[66] showed that preparation before SBML is substantial to improve the effectiveness of SBML.They found that web-based observational practice is superior to reading materials alone,as it increases learner engagement with instructional materials.
Okay, he said, helping9 me down the stairs and to the curb10, I m going to stay here and keep an ear out for the babies. I ll tell you when it s safe to cross. You go over to the Coke machine, get your Coke and come back out. Wait for me to tell you when it s safe to cross back.
However,some systematic reviews have reported inconclusive evidence supporting SBT as a replacement for conventional training.SBT might be more beneficial as a supplement to conventional training,especially in the early phase.Nevertheless,reducing patient-based training in favor of SBT is not recommended as it cannot replace conventional patient-based training[48,51,52].Hence,simulation must be accompanied by direct clinical experience with patients in order to understand the actual clinical setting[39].A study conducted in 2004 found that simulation without feedback from experts did not improve the skills of trainees.Providing trainees access to a simulator cannot guarantee appropriate learning by itself.Therefore,SBT should be delivered purposefully within a developed curriculum to allow trainees to practice essential skills,receive feedback from experts,and develop skills gradually and appropriately to achieve mastery[55].Feedback and debriefing are essential in SBT to allow trainees identify their weakness and improve their performance accordingly[56].Simulation with a proper environment or scenario is also beneficial to the improvement of endoscopic non-technical skills such as communication and teamwork,situation awareness,leadership,judgment,and decision making[57].A previous study showed that integrating endoscopic non-technical skills training improved novice trainees’ performance and competency,which might benefit patients[58].
EXPERIENCES IN SIMULATION-BASED MASTERY LEARNING FOR ENDOSCOPY TRAINING
Several studies have shown endoscopy mastery learning experiences.Nguyen-Vu
[59] reported a 2-wk course for gastroenterology fellows at the University of California with no prior experience in endoscopy.They divided the learning period into two phases: the 1
week for learning the basics of endoscopy and the 2
week for learning various therapies in endoscopy.These phases were further divided into specific endoscopic skills such as endoscopic tip control,image documentation,biopsy,and clip administration.Trainees were assigned readings and underwent online assessments before attending hands-on training with a simulator.They had to pass the competency assessment for a specific skill before moving to the next topic.This study showed that the SBML program could rapidly help trainees acquire endoscopic skills through a comprehensive curriculum.Online reading and assessments enabled trainees to learn at their own pace,and using a simulator provided them with a chance to engage in repetitive practice.Dividing endoscopic skills also allowed trainees to focus on the specific skills they needed to refine.
King Gridelin had no sooner set eyes upon the lady than with a cry of joy he clasped her in his arms, for it was no other than his long- lost wife, Santorina, about whose imprisonment in Fairyland you may perhaps read some day
In all my years of driving a taxicab, I have never had any trouble with the public, not even with drunks. Even if they get a little headstrong(,) once in a while, I just agree with them and then they behave themselves.
One day about eight years ago in the departure lounge of a flight from New York s LaGuardia airport to O Hare in Chicago, I spotted1 a young boy in tears and obvious emotional distress2. His mother at his side also appeared upset. Being a parent, I was naturally curious if I could be of assistance.
Since 1962,the American Society for Gastrointestinal Endoscopy has held symposiums about teaching methods in GI endoscopy and later formed a formal endoscopy training program.Along with the development of science and advancement in the complexity of endoscopic procedures,gastroenterological education began to be developed independently as part of a subspecialty of internal medicine[4].The development of specific training in endoscopy and gastroenterology also impacted the education period for this field,which initially consisted of 1 year to 2 years and then was extended to 3 years[4].Currently,there is no global standardization of the gastroenterology education length.Some countries,such as the Netherlands,are now expanding their gastroenterology curriculum to 3 years to 4 years,starting with 2 years of general internal medicine training[7,8].In Korea,endoscopy training is conducted for 1 year to 2 years during a gastroenterology fellowship program[9].Meanwhile,in Japan,a physician must complete 3 years of internal medicine residency and 5 years of gastroenterology fellowship to become a board-certified endoscopist[10].The World Gastroenterology Organization states that a student must complete 3 years of internal medicine residency before pursuing gastroenterological-specific education and training for the next 3 years[11].
Soetikno
l[61] developed a 6-wk SBML program for 1
-year gastroenterology fellows of the Philippine Society of Digestive Endoscopy.SBML involved learning fine-tip control,structured upper endoscopy examination,and endoscopic therapies.Basic knowledge and interpretation of endoscopy findings were learned simultaneously.Interestingly,the first 5 wk of the program were conducted remotely using virtual coaching.Trainees used simulators and recorded their own performance,number of attempts,and completion time for each attempt,and then supervisors provided feedback based on these attempts.During the last week,trainees underwent in-person endoscopic therapy training after having passed the standard for fine-tip control and structured upper endoscopy examination.This study found that the adoption rates for basic endoscopic techniques such as image documentation and biopsy were 93% and 100%,respectively,after 2 mo of training.Meanwhile,the adoption rates of endoscopic therapies such as clipping,band ligation,and injection were more variable (7%-79%)[63].Soetikno
[64] also conducted an SBML course in GI bleeding endoscopic therapy and found that SBML quickly disseminated technical knowledge and skills.They proposed SBML as an additional method for teaching before trainees performed the procedure on patients.
PLANNING AND MANAGEMENT OF SIMULATION-BASED MASTERY LEARNING IN GI ENDOSCOPY
Mastery of basic endoscopic techniques is essential for every endoscopist,because if the procedure is performed incorrectly,it can cause severe complications that might threaten the condition of patients.The essential steps of endoscopy are endoscope insertion,precise observation,and appropriate imaging[29].Skills developed by each endoscopist may vary and are influenced by differences among supervisors during the procedure.Hence,standardized training is necessary to maintain the competence of trainees[30].
Ritter
[60] reported an endoscopy training system (ETS) using an SBML curriculum implemented with general surgery residents to pass the Fundamentals of Endoscopic Surgery (FES) skills examination.They divided ETS into five tasks which were organized in two tabletop units.The first unit included scope manipulation,tool targeting,and retroflexion tasks using a simple endoscopic tool.The second unit consisted of loop management and mucosal inspection tasks using a stylized body form.Most participants completed this simulation-based curriculum in less than 1 wk with more than 90 min of practice per day.This study suggested that the application of the SBML curriculum to flexible endoscopes provides significantly improved results on posttraining assessments compared with pretraining assessments.This study also found that after five sessions of SBT,participants could produce posttest scores equivalent to those of doctors who had performed 150-300 endoscopy procedures.This result implies that vast clinical experience is not needed to participate in the SBML program.The ETS was further developed by setting the training standards for the SBML curriculum,resulting in attainable standards that improved FES scores in the skills exam[61].Another subsequent study published in 2021 evaluated the effect of SBML curriculum implementation early in residency.It revealed that early implementation of SBML curriculum for flexible endoscopy training resulted in comparable performance to those with high level of clinical endoscopic experience[62].
Generally,studies on SBT in GI endoscopy training have shown favorable results,especially in the early phase of training,as it reduces the time required to reach technical competence and the number of endoscopic procedures needed to perform it independently.With SBT,trainees can perform the procedures and exercises repeatedly using a simulator.This repetition improves the cognitive and practical skills of students and allows them to become more acquainted with endoscopic features and settings.A meta-analysis showed that simulation can increase patient safety and decrease the risk of adverse events,as trainees are more skilled and familiarized with the clinical settings at the moment of performing the endoscopy[44-49].It also provides an opportunity for trainees to learn at their own pace[50-54].
The SBML method uses an instructional approach,meaning that trainees must have a certain level of competence in a simulated environment before performing procedures on actual patients[24].With this method,trainees progress through different simulations with increasing difficulty.SBML provides opportunities for students to practice as often as possible to improve their performance before operating on patients.This method can optimize clinical outcomes and reduce the risk of complications or other hazards for patients that may occur during the operation period of a novice endoscopist[17,38].In addition,SBML can minimize variations between trainees upon completion of the program[24,39].
In addition to training or lesson planning,an assessment plan is needed to create a training environment with maximum results.Assessment is vital to provide trainees with future directions for improvement and to ensure patient safety by issuing a passing standard[69].At the beginning of mastery learning,a pretest has to be conducted to evaluate the initial knowledge of trainees[67].Within the program,assessments are classified as formative or summative assessments.Formative assessment aims to direct training and support the self reflection and intrinsic motivation of trainees[70].Meanwhile,summative assessment seeks to evaluate competency and practice eligibility[71].There are five criteria to indicate the quality of an assessment: reliability,which shows the accuracy and reproducibility of a test: validity,which shows whether the test can be performed to evaluate the intended focused parameter;future impact of the assessment;acceptability by trainees and supervisors;and reasonable cost.Assessments can be conducted through written examinations,direct evaluations by clinical supervisors,direct observations,clinical simulations,or portfolios[69].
THE FUTURE OF SIMULATION-BASED MASTERY LEARNING IN GI ENDOSCOPY
It is reasonable and expected that novice endoscopists do not perform endoscopic procedures on human patients unless they have shown satisfactory skills on a simulator.Endoscopy training should move from the traditional apprenticeship model to objective competency-based mastery learning,integrating simulators,deliberate practice,and prompt feedback from supervisors.The SBML curriculum is acknowledged as a method to boost the efficiency and efficacy of endoscopy training through repetitive practice and expert feedback,which allow trainees to learn the basic structure of endoscopic techniques.One of the limitations of the traditional apprenticeship model is the reduced time for questions,feedback,and adequate skill assessment during a procedure on an actual patient,which results in self learning;thus,not all trainees might develop a proper form and technique.Incorporating simulators can reduce this limitation of the conventional apprenticeship model by allowing trainees to practice basic endoscopic maneuvers repeatedly,as each trainee has a different absorption rate.In fact,acquiring proper techniques is essential for trainees,as they can progress to the next stage of training which is more complex.Simulators also limit the possibility of patient discomfort and injury,thereby allowing trainees to improve their skills.Additionally,the standardization of simulator-based instruction methods is essential to maximize the positive impact of the training method[8].The integration of simulator in endoscopy training should be within a structured curriculum that combines constructive feedback and complementary knowledge[72].A previous randomized trial compared the outcome of structured comprehensive curriculum to progressive learning-based curriculum,and revealed that those who received SBT that progressed in complexity and difficulty had superior technical and communication skills and global performance in the simulated setting[73].
A proper SBML curriculum for GI endoscopy should subsequently consist of cognitive,technical,and integrative skill training.The coronavirus disease 2019 pandemic has accelerated the acceptance of online video/web-based learning,video mentoring,and video proctoring.Web-based learning in the form of online modules is now expected for cognitive skill training,which allows trainees to review learning modules at their own pace and to avoid cognitive overload due to a stressful environment[59].The main drawbacks of simulation-based learning are model realism and less real-world experience for new endoscopists.Hence,hybrid learning that combines simulator-based and one-on-one training is ideal for building the learning curves of trainees and identifying their deficiencies[74].Improved performance in simulator training has been shown to translate into the clinical area[60].
CONCLUSION
The traditional apprenticeship model in GI endoscopy training must be revised to ensure competency and practical eligibility of novice endoscopists.By moving the focus from a case volume-based to a competency-based training,mastery learning can help lower the variability between skills of trainees and provide optimal results.Previous experiences with the SBML program in endoscopy training showed promising results and positioned that method as an additional course to be incorporated before the apprenticeship is started and also as a complementary course to one-on-one training.The use of a simulator in SBML can help trainees become acquainted with the endoscopic equipment,settings,and situations that might arise during their direct practice on patients.The SBML program should be planned and managed by a specific team and conducted within a developed and tested curriculum.
Maulahela H conceived the study,and wrote and edited the manuscript;Annisa NG performed the data analysis and drafted the manuscript;Konstantin T edited and finalized the manuscript for submission;Syam AF and Soetikno R reviewed and approved the submitted manuscript.
All authors declares that they have no conflict of interest.
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Indonesia
Bow-wow! That was the end of happiness! The Snow-man, however, was not listening to him any more; he was looking into the room where the housekeeper lived, where the stove stood on its four iron legs, and seemed to be just the same size as the Snow-man
Hasan Maulahela 0000-0002-0396-4433;Nagita Gianty Annisa 0000-0001-9708-0454;Tiffany Konstantin 0000-0003-2086-9531;Ari Fahrial Syam 0000-0003-0041-3553.
World Endoscopy Organization;American College of Gastroenterology;American Society for Gastrointestinal Endoscopy;The Indonesian Society of Digestive Endoscopy;The Indonesian Society of Gastroenterology.
Wang LL
A
Wang LL
1 Seward E,Lumley S.Endoscopy provision: meeting the challenges.
2017;8: 90-93 [PMID: 28839891 DOI: 10.1136/flgastro-2016-100764]
2 Huang C,Hopkins R,Huang K,Demers L,Wasan S.Standardizing Endoscopy Training: A Workshop for Endoscopy Educators.
2020;16: 11015 [PMID: 33204839 DOI: 10.15766/mep_2374-8265.11015]
3 Matharoo M,Haycock A,Sevdalis N,Thomas-Gibson S.A prospective study of patient safety incidents in gastrointestinal endoscopy.
2017;5: E83-E89 [PMID: 28191498 DOI: 10.1055/s-0042-117219]
4 McGaghie WC.Mastery learning: it is time for medical education to join the 21st century.
2015;90: 1438-1441 [PMID: 26375269 DOI: 10.1097/ACM.0000000000000911]
5 Mahmood T,Scaffidi MA,Khan R,Grover SC.Virtual reality simulation in endoscopy training: Current evidence and future directions.
2018;24: 5439-5445 [PMID: 30622373 DOI: 10.3748/wjg.v24.i48.5439]
6 Finocchiaro M,Cortegoso Valdivia P,Hernansanz A,Marino N,Amram D,Casals A,Menciassi A,Marlicz W,Ciuti G,Koulaouzidis A.Training Simulators for Gastrointestinal Endoscopy: Current and Future Perspectives.
2021;13 [PMID: 33804773 DOI: 10.3390/cancers13061427]
7 Caspritz T,Arnold M,White C,Schultz M.A Critical Analysis of the gastroenterology specialist workforce in New Zealand.Wellington: New Zealand Society of Gastroenterology,2018.[cited 20 April 2022].Available from: https://www.nzdoctor.co.nz/article/undoctored/critical-analysis-gastroenterology-specialist-workforce-new-zealand
8 Greenwald DA,Freeman ML.The Endoscopic Management of Immediate Complications of Therapeutic Endoscopy.In: Cohen J.Successful Training in Gastrointestinal Endoscopy.Second Edition.Oxford: Wiley-Blackwell,2022: 351-356
9 Kim JS,Kim BW.Endoscopy training in Korea.
2019;34: 237-241 [PMID: 30840806 DOI: 10.3904/kjim.2019.028]
10 Hatanaka H,Yamamoto H,Lefor AK,Sugano K.Gastroenterology Training in Japan.
2016;61: 1448-1450 [PMID: 26860507 DOI: 10.1007/s10620-016-4065-x]
11 World Gastroenterology Organisation Education &Training Committee.Standards in gastroenterology training: a comprehensive guide to basic standards in gastroenterology.Munich: World Gastroenterology Organisation,2007
12 Maida M,Alrubaiy L,Bokun T,Bruns T,Castro V,China L,Conroy G,Trabulo D,Van Steenkiste C,Voermans RP,Burisch J,Ianiro G.Current challenges and future needs of clinical and endoscopic training in gastroenterology: a European survey.
2020;8: E525-E533 [PMID: 32258375 DOI: 10.1055/a-1093-0877]
13 Waschke KA,Coyle W.Advances and Challenges in Endoscopic Training.
2018;154: 1985-1992 [PMID: 29454788 DOI: 10.1053/j.gastro.2017.11.293]
14 Chin MW,Forbes GM.Should simulator use become mandatory in endoscopy training?
2008;23: 996-997 [PMID: 18707595 DOI: 10.1111/j.1440-1746.2008.05476.x]
15 Long V,Kalloo AN.AccuTouch Endoscopy Simulator: development,applications and early experience.
2006;16: 479-487 [PMID: 16876720 DOI: 10.1016/j.giec.2006.03.014]
16 Dawe SR,Windsor JA,Broeders JA,Cregan PC,Hewett PJ,Maddern GJ.A systematic review of surgical skills transfer after simulation-based training: laparoscopic cholecystectomy and endoscopy.
2014;259: 236-248 [PMID: 24100339 DOI: 10.1097/SLA.0000000000000245]
17 Park KS.Introduction to Starting Upper Gastrointestinal Endoscopy: Proper Insertion,Complete Observation,and Appropriate Photographing.
2015;48: 279-284 [PMID: 26240799 DOI: 10.5946/ce.2015.48.4.279]
18 Lateef F.Simulation-based learning: Just like the real thing.
2010;3: 348-352 [PMID: 21063557 DOI: 10.4103/0974-2700.70743]
19 Telleman H,Burger TF,Mulder CJ.Evolution of gastroenterology training.
2009;15: 1793-1798 [PMID: 19370773 DOI: 10.3748/wjg.15.1793]
20 Williams CB,Saunders BP,Bladen JS.Development of colonoscopy teaching simulation.
2000;32: 901-905 [PMID: 11085481 DOI: 10.1055/s-2000-8089]
21 Classen M,Ruppin H.Practical Endoscopy Training Using a New Gastrointestinal Phantom.Endoscopy.
1974;6: 127-131 [DOI: 10.1055/s-0028-1098609]
22 Williams CB,Baillie J,Gillies DF,Borislow D,Cotton PB.Teaching gastrointestinal endoscopy by computer simulation: a prototype for colonoscopy and ERCP.
1990;36: 49-54 [PMID: 2311883 DOI: 10.1016/s0016-5107(90)70923-6]
23 Koch AD,Buzink SN,Heemskerk J,Botden SM,Veenendaal R,Jakimowicz JJ,Schoon EJ.Expert and construct validity of the Simbionix GI Mentor II endoscopy simulator for colonoscopy.
2008;22: 158-162 [PMID: 17516114 DOI: 10.1007/s00464-007-9394-6]
24 Triantafyllou K,Lazaridis LD,Dimitriadis GD.Virtual reality simulators for gastrointestinal endoscopy training.
2014;6: 6-12 [PMID: 24527175 DOI: 10.4253/wjge.v6.i1.6]
25 Faigel DO,Baron TH,Lewis B,Petersen B,Petrini J,Popp JW,Jack PS,Dipalma A,Pike IM,Flax IL.Ensuring Competence in Endoscopy.AGSE Taskforce and American College of Gastroenterology Executive and Practice Management Committees.[cited 20 April 2022].Available from: https://www.asge.org/docs/defaultsource/education/practice_guidelines/doc-competence.pdf?sfvrsn=6
26 Walsh CM.In-training gastrointestinal endoscopy competency assessment tools: Types of tools,validation and impact.
2016;30: 357-374 [PMID: 27345645 DOI: 10.1016/j.bpg.2016.04.001]
27 McGaghie WC,Issenberg SB,Cohen ER,Barsuk JH,Wayne DB.Medical education featuring mastery learning with deliberate practice can lead to better health for individuals and populations.
2011;86: e8-e9 [PMID: 22030671 DOI: 10.1097/ACM.0b013e3182308d37]
28 Mann DD,Eland DC.Self-efficacy in mastery learning to apply a therapeutic psychomotor skill.
2005;100: 77-84 [PMID: 15773696 DOI: 10.2466/pms.100.1.77-84]
29 ASGE Training Committee,Adler DG,Bakis G,Coyle WJ,DeGregorio B,Dua KS,Lee LS,McHenry L Jr,Pais SA,Rajan E,Sedlack RE,Shami VM,Faulx AL.Principles of training in GI endoscopy.
2012;75: 231-235 [PMID: 22154419 DOI: 10.1016/j.gie.2011.09.008]
30 Ende A,Zopf Y,Konturek P,Naegel A,Hahn EG,Matthes K,Maiss J.Strategies for training in diagnostic upper endoscopy: a prospective,randomized trial.
2012;75: 254-260 [PMID: 22153875 DOI: 10.1016/j.gie.2011.07.063]
31 Han S.Achieving Competence in Endoscopy.
2019;6: e00155 [PMID: 31737697 DOI: 10.14309/crj.0000000000000155]
32 Beattie AD,Greff M,Lamy V,Mallinson CN.The European Diploma of Gastroenterology: progress towards harmonization of standards.
1996;8: 403-406 [PMID: 8781913 DOI: 10.1097/00042737-199604000-00021]
33 Eisen GM,Baron TH,Dominitz JA,Faigel DO,Goldstein JL,Johanson JF,Mallery JS,Raddawi HM,Vargo JJ 2nd,Waring JP,Fanelli RD,Wheeler-Harbough J;American Society for Gastrointestinal Endoscopy.Methods of granting hospital privileges to perform gastrointestinal endoscopy.
2002;55: 780-783 [PMID: 12024127 DOI: 10.1016/s0016-5107(02)70403-3]
34 Pearl J,Dunkin B,Pauli E,Trus T,Jeffrey M,Fanelli R,Meara M,Stefanidis D,Richardson W.Guidelines for Privileging and Credentialing Physicians in Gastrointestinal Endoscopy.Los Angeles: Society of American Gastrointestinal and Endoscopic Surgeons,2016.[cited 20 April 2022].Available from: https://www.sages.org/publications/guidelines/guidelines-privileging-credentialing-physicians-gastrointestinal-endoscopy/
35 Kim JS,Kim BW.Training in Endoscopy: Esophagogastroduodenoscopy.
2017;50: 318-321 [PMID: 28783922 DOI: 10.5946/ce.2017.096]
36 Farthing MJ,Walt RP,Allan RN,Swan CH,Gilmore IT,Mallinson CN,Bennett JR,Hawkey CJ,Burnham WR,Morris AI,Tibbs CJ,Bowling TE,Cobb C,Catnach S,Farrell C,Towle A.A national training programme for gastroenterology and hepatology.
1996;38: 459-470 [PMID: 8675103 DOI: 10.1136/gut.38.3.459]
37 McGaghie WC.Mastery Learning: Origins,Features,and Evidence from the Health Professions.In: McGaghie WC,Barsuk JH,Wayne DB.Comprehensive Healthcare Simulation: Mastery Learning in Health Professions Education.Cham,Switzerland: Springer,2020: 27-46 [DOI: 10.1007/978-3-030-34811-3_2]
38 Zendejas B,Brydges R,Wang AT,Cook DA.Patient outcomes in simulation-based medical education: a systematic review.
2013;28: 1078-1089 [PMID: 23595919 DOI: 10.1007/s11606-012-2264-5]
39 Ferlitsch A,Glauninger P,Gupper A,Schillinger M,Haefner M,Gangl A,Schoefl R.Evaluation of a virtual endoscopy simulator for training in gastrointestinal endoscopy.
2002;34: 698-702 [PMID: 12195326 DOI: 10.1055/s-2002-33456]
40 Harrison CM,Gosai JN.Simulation-based training for cardiology procedures: Are we any further forward in evidencing real-world benefits?
2017;27: 163-170 [PMID: 27986510 DOI: 10.1016/j.tcm.2016.08.009]
41 Cook DA,Brydges R,Zendejas B,Hamstra SJ,Hatala R.Mastery learning for health professionals using technologyenhanced simulation: a systematic review and meta-analysis.
2013;88: 1178-1186 [PMID: 23807104 DOI: 10.1097/ACM.0b013e31829a365d]
42 Koch AD,Ekkelenkamp VE,Haringsma J,Schoon EJ,de Man RA,Kuipers EJ.Simulated colonoscopy training leads to improved performance during patient-based assessment.
2015;81: 630-636 [PMID: 25475901 DOI: 10.1016/j.gie.2014.09.014]
43 Cohen J,Cohen SA,Vora KC,Xue X,Burdick JS,Bank S,Bini EJ,Bodenheimer H,Cerulli M,Gerdes H,Greenwald D,Gress F,Grosman I,Hawes R,Mullin G,Schnoll-Sussman F,Starpoli A,Stevens P,Tenner S,Villanueva G.Multicenter,randomized,controlled trial of virtual-reality simulator training in acquisition of competency in colonoscopy.
2006;64: 361-368 [PMID: 16923483 DOI: 10.1016/j.gie.2005.11.062]
44 Di Giulio E,Fregonese D,Casetti T,Cestari R,Chilovi F,D'Ambra G,Di Matteo G,Ficano L,Delle Fave G.Training with a computer-based simulator achieves basic manual skills required for upper endoscopy: a randomized controlled trial.
2004;60: 196-200 [PMID: 152WJG-28-5203 DOI: 10.1016/S0016-5107(04)01566-4]
45 Shirai Y,Yoshida T,Shiraishi R,Okamoto T,Nakamura H,Harada T,Nishikawa J,Sakaida I.Prospective randomized study on the use of a computer-based endoscopic simulator for training in esophagogastroduodenoscopy.
2008;23: 1046-1050 [PMID: 18554236 DOI: 10.1111/j.1440-1746.2008.05457.x]
46 Ferlitsch A,Schoefl R,Puespoek A,Miehsler W,Schoeniger-Hekele M,Hofer H,Gangl A,Homoncik M.Effect of virtual endoscopy simulator training on performance of upper gastrointestinal endoscopy in patients: a randomized controlled trial.
2010;42: 1049-1056 [PMID: 20972956 DOI: 10.1055/s-0030-1255818]
47 Haycock A,Koch AD,Familiari P,van Delft F,Dekker E,Petruzziello L,Haringsma J,Thomas-Gibson S.Training and transfer of colonoscopy skills: a multinational,randomized,blinded,controlled trial of simulator versus bedside training.
2010;71: 298-307 [PMID: 19889408 DOI: 10.1016/j.gie.2009.07.017]
48 Qiao W,Bai Y,Lv R,Zhang W,Chen Y,Lei S,Zhi F.The effect of virtual endoscopy simulator training on novices: a systematic review.
2014;9: e89224 [PMID: 24586609 DOI: 10.1371/journal.pone.0089224]
49 Singh S,Sedlack RE,Cook DA.Effects of simulation-based training in gastrointestinal endoscopy: a systematic review and meta-analysis.
2014;12: 1611-23.e4 [PMID: 24509241 DOI: 10.1016/s0016-5085(14)62687-1]
50 Ekkelenkamp VE,Koch AD,de Man RA,Kuipers EJ.Training and competence assessment in GI endoscopy: a systematic review.
2016;65: 607-615 [PMID: 25636697 DOI: 10.1136/gutjnl-2014-307173]
51 Khan R,Plahouras J,Johnston BC,Scaffidi MA,Grover SC,Walsh CM.Virtual reality simulation training for health professions trainees in gastrointestinal endoscopy.
2018;8: CD008237 [PMID: 30117156 DOI: 10.1002/14651858.CD008237.pub3]
52 Smith R,Zhao M.P74 Simulation in endoscopy training: a systematic review and meta-analysis.
2021;70: A78 [DOI: 10.1136/gutjnl-2020-bsgcampus.149]
53 Zhang W,Liu X,Zheng B.Virtual reality simulation in training endoscopic skills: A systematic review.
2021;4: 97-104 [DOI: 10.1016/j.lers.2021.09.002]
54 ASGE Training Committee,Sedlack RE,Coyle WJ,Obstein KL,Al-Haddad MA,Bakis G,Christie JA,Davila RE,DeGregorio B,DiMaio CJ,Enestvedt BK,Jorgensen J,Mullady DK,Rajan L.ASGE's assessment of competency in endoscopy evaluation tools for colonoscopy and EGD.
2014;79: 1-7 [PMID: 24239255 DOI: 10.1016/j.gie.2013.10.003]
55 Mahmood T,Darzi A.The learning curve for a colonoscopy simulator in the absence of any feedback: no feedback,no learning.
2004;18: 1224-1230 [PMID: 15457382 DOI: 10.1007/s00464-003-9143-4]
56 Khan R,Scaffidi MA,Grover SC,Gimpaya N,Walsh CM.Simulation in endoscopy: Practical educational strategies to improve learning.
2019;11: 209-218 [PMID: 30918586 DOI: 10.4253/wjge.v11.i3.209]
57 Ravindran S,Thomas-Gibson S,Murray S,Wood E.Improving safety and reducing error in endoscopy: simulation training in human factors.
2019;10: 160-166 [PMID: 31205657 DOI: 10.1136/flgastro-2018-101078]
58 Walsh CM,Scaffidi MA,Khan R,Arora A,Gimpaya N,Lin P,Satchwell J,Al-Mazroui A,Zarghom O,Sharma S,Kamani A,Genis S,Kalaichandran R,Grover SC.Non-technical skills curriculum incorporating simulation-based training improves performance in colonoscopy among novice endoscopists: Randomized controlled trial.
2020;32: 940-948 [PMID: 31912560 DOI: 10.1111/den.13623]
59 Nguyen-Vu T,Malvar C,Chin YK,Kaltenbach T,Liu A,Myint T,Asokkumar R,Shergill A,Soetikno R.Simulationbased mastery learning (SBML) for rapid acquisition of upper endoscopy knowledge and skills-initial observation.
2020;5: 222-225 [PMID: 32529151 DOI: 10.1016/j.vgie.2020.02.014]
60 Ritter EM,Taylor ZA,Wolf KR,Franklin BR,Placek SB,Korndorffer JR Jr,Gardner AK.Simulation-based mastery learning for endoscopy using the endoscopy training system: a strategy to improve endoscopic skills and prepare for the fundamentals of endoscopic surgery (FES) manual skills exam.
2018;32: 413-420 [PMID: 28698900 DOI: 10.1007/s00464-017-5697-4]
61 Franklin BR,Placek SB,Gardner AK,Korndorffer JR Jr,Wagner MD,Pearl JP,Ritter EM.Preparing for the American Board of Surgery Flexible Endoscopy Curriculum: Development of multi-institutional proficiency-based training standards and pilot testing of a simulation-based mastery learning curriculum for the Endoscopy Training System.
2018;216: 167-173 [PMID: 28974312 DOI: 10.1016/j.amjsurg.2017.09.010]
62 Dyke C,Franklin BR,Sweeney WB,Ritter EM.Early implementation of Fundamentals of Endoscopic Surgery training using a simulation-based mastery learning curriculum.
2021;169: 1228-1233 [PMID: 33583604 DOI: 10.1016/j.surg.2020.12.005]
63 Soetikno R,Cabral-Prodigalidad PA,Kaltenbach T;AOE Investigators.Simulation-Based Mastery Learning With Virtual Coaching: Experience in Training Standardized Upper Endoscopy to Novice Endoscopists.
2020;159: 1632-1636 [PMID: 32758502 DOI: 10.1053/j.gastro.2020.06.096]
64 Soetikno R,Asokkumar R,McGill SK,Kaltenbach T.Simulation-Based Mastery Learning for Practicing Gastroenterologists-Renewed Importance in the Era of COVID-19.
2020;115: 1380-1383 [PMID: 32773455 DOI: 10.14309/ajg.0000000000000788]
65 Sawaya RD,Mrad S,Rajha E,Saleh R,Rice J.Simulation-based curriculum development: lessons learnt in Global Health education.
2021;21: 33 [PMID: 33413346 DOI: 10.1186/s12909-020-02430-9]
66 Cheung JJ,Koh J,Brett C,Bägli DJ,Kapralos B,Dubrowski A.Preparation With Web-Based Observational Practice Improves Efficiency of Simulation-Based Mastery Learning.
2016;11: 316-322 [PMID: 27388862 DOI: 10.1097/SIH.0000000000000171]
67 Adams NE.Bloom's taxonomy of cognitive learning objectives.
2015;103: 152-153 [PMID: 26213509 DOI: 10.3163/1536-5050.103.3.010]
68 Ben-David MF.The role of assessment in expanding professional horizons.
2000;22: 472-477 [PMID: 21271959 DOI: 10.1080/01421590050110731]
69 Austin Z.How to design and use learning objective in clinical teaching.
2016;296: 46-48 [DOI: 10.1211/pj.2016.20200251]
70 Anderson L,Krathwohl D,Bloom B.A Taxonomy for Learning,Teaching,and Assessing: A Revision of Bloom’s Taxonomy of Educational Objectives.New York: Addison Wesley Longman,2001
71 Epstein RM.Assessment in medical education.
2007;356: 387-396 [PMID: 17251535 DOI: 10.1056/NEJMra054784]
72 Grover SC,Garg A,Scaffidi MA,Yu JJ,Plener IS,Yong E,Cino M,Grantcharov TP,Walsh CM.Impact of a simulation training curriculum on technical and nontechnical skills in colonoscopy: a randomized trial.
2015;82: 1072-1079 [PMID: 26007221 DOI: 10.1016/j.gie.2015.04.008]
73 Grover SC,Scaffidi MA,Khan R,Garg A,Al-Mazroui A,Alomani T,Yu JJ,Plener IS,Al-Awamy M,Yong EL,Cino M,Ravindran NC,Zasowski M,Grantcharov TP,Walsh CM.Progressive learning in endoscopy simulation training improves clinical performance: a blinded randomized trial.
2017;86: 881-889 [PMID: 28366440 DOI: 10.1016/j.gie.2017.03.1529]
74 Koo CS,Siah KTH,Koh CJ.Endoscopy training in COVID-19: Challenges and hope for a better age.
2021;36: 2715-2719 [PMID: 33871079 DOI: 10.1111/jgh.15524]
杂志排行
World Journal of Gastrointestinal Endoscopy的其它文章
- Endoscopic ultrasound elastography for malignant pancreatic masses and associated lymph nodes:Critical evaluation of strain ratio cutoff value
- Screening for hilar biliary invasion in ampullary cancer patients
- Endoscopic therapy using a self-expandable metallic stent with an anti-migration system for postorthotopic liver transplantation anastomotic biliary stricture
- Clinical profile,diagnostic yield,and procedural outcomes of single balloon enteroscopy: A tertiary care hospital experience
- Role of endoscopic ultrasound in evaluation of patients with missed common bile duct stones
- Isolated esophageal tuberculosis:A case report
