早期床旁运动干预在心脏手术后患者心脏康复中的应用效果
2022-09-14RafiHAMIDI陈轶洪弥守玲陆云涛王文硕HosnaHAMIDISalimBAHRAMANDAliAteelDAIFOLADIBabrakSAYEDZADA王春生
M. Rafi HAMIDI, 陈轶洪, 弥守玲, 陆云涛, 丛 硕, 王文硕, Hosna HAMIDI,杨 晔, M. Salim BAHRAMAND, Ali Ateel DAIFOLADI, Babrak SAYEDZADA, 刘 欢, 魏 来*, 王春生
1.复旦大学附属中山医院心血管外科,上海心血管病研究所,上海 200032
2.世界卫生组织区域卫生组,喀布尔 1001,阿富汗
3.红新月会卫生部,喀布尔 1001,阿富汗
4.喀布尔Amir Hajizada 医院心血管外科,喀布尔 1001,阿富汗
5. 法国母婴研究所心血管外科,咯布尔 1001,阿富汗
Cardiac rehabilitation was started in the 1950s for patients with myocardial infarction[1-3]and is now included in the international guidelines as a postoperative intervention for all patients who have undergone cardiac surgery[4]. The 6-minute walk test (6MWT) determines the maximum distance that a subject can walk in 6 min. This test is easy to perform, requires no specific equipment, and can be incorporated into normal activities of daily living[5].The 6MWT is used in the cardiac rehabilitation setting to assess patients with heart failure before and after surgical intervention. Several studies have confirmed that this test is superior to the shuttle walk test and the 200-m fast-walk test in patients with chronic heart failure. Older age, female sex, poor left ventricular function, and comorbidities such as cerebrovascular disease or chronic obstructive pulmonary disease are negative predictors of 6MWT after inpatient cardiac rehabilitation[6].
Walk tests can be used to monitor functional performance and effectiveness of treatment and to check that it is safe to discharge a patient from hospital. The 6MWT is a safe and effective method for predicting the effects of intervention in the perioperative period in patients undergoing valve surgery. However, there is no standardized mathematical model that can be used to define or measure important variables affecting performance on the 6MWT postoperatively in patients with cardiovascular disease.
Therefore, this study aimed to elucidate the safety and efficacy of exercise intervention at the bedside in terms of vital signs and walking capacity in patients requiring cardiac rehabilitation after surgery for isolated valvular heart disease.
1 PATIENTS AND METHODS
1.1 Study subjects 58 adult inpatients with mitral,aortic, and/or tricuspid valve disease who underwent isolated valve repair or replacement surgery at zhongshan Hospital, Fudan University between January 2018 and February 2019 were selected. The following exclusion criteria were applied: coronary artery disease; atrial fibrillation; a left ventricular ejection fraction of <40%; inability to participate in regular exercise training; leg claudication; abnormal blood pressure; post-traumatic stress disorder;and history of stroke. The study participants were randomly assigned to an intervention group or a control group (Figure 1). The study protocol was approved by the ethics committee of Zhongshan Hospital, Fudan University (B2019-012R). All study participants provided written informed consent.

Figure 1 Intervention process and flow of patients through the study
1.2 Physical assessment Patients in both study groups were closely observed by a resident and a registered nurse in cardiac surgery with extensive experience in the management of patients with valvular heart disease and use of the 6MWT in the setting of a cardiac rehabilitation program. Laboratory investigations, including fasting blood glucose, lipid profile, N-terminal pro B-type natriuretic peptide,cardiac troponin T, and creatine kinase-MB, and electrocardiographic and echocardiographic screening were performed in all cases. Upper limb function was evaluated by grip strength and lower limb function by the unipedal stance test. Cardiovascular risk factors,including hypertension, diabetes, dyslipidemia, alcohol abuse, and history of smoking, were considered as independent variables. Laboratory examinations were repeated before discharge from hospital.
1.3 Six-minute walk test All subjects performed the 6MWT, whereby they walked for 25 m along a flat ward corridor with continuous monitoring of blood pressure and oxygen saturation (SpO2) and an electrocardiogram. The maximal distance walked over 6 min was recorded before and after surgery according to the protocol recommended by the American Thoracic Society Pulmonary Function Standards Committee[7].
1.4 Psychosocial assessment A psychosocial assessment was performed to evaluate health-related quality of life[8]. All participants completed three self-administered questionnaires, namely, the 36-item short form health survey (SF-36), the international physical activity questionnaire (IPAQ)-9, and the generalized anxiety disorder 7-item scale (GAD-7), on the first day of hospital admission and at the time of discharge from hospital.
1.5 Exercise intervention at the bedside Patients in the intervention group performed supervised cycling exercise for 3 min/d starting on postoperative day 3, 4, or 5 through until discharge. Each patient was required to perform lower limb exercise training on a pedal exercise bike with monitoring of vital signals.
1.6 Cardiovascular function assessment Upper limb grip strength was assessed in both study groups using an electronic hand dynamometer. Lower limb muscle extension strength was assessed using the unipedal stance test with eyes open maneuver over 30 s before surgery and on postoperative day 3.Resting blood pressure was measured using an automated blood pressure monitor and resting SpO2was measured using a pulse oximeter. Heart rate (HR)was monitored continuously during exercise.
1.7 Statistical analysis Continuous variables were presented asand were compared using the Student’s t test. Categorical variables were shown as the n(%) and were compared using the chi-square test. All statistical analyses were performed using GraphPad Prism version 7.0 and SSPS 22.0. The significance level was set at α=0.05.
2 RESULTS
2.1 Baseline characteristics Six of the 58 patients did not complete the assessment, 4 refused to participate in the intervention, 7 received only 1 or 2 exercise interventions during the immediate postoperative period, and 1 patient could not participate because of depression, leaving 40 patients for inclusion in the study. Twenty subjects were allocated to the intervention group and 20 to the control group. There were no statistically significant between-group differences in the demographic data,comorbidities, cardiovascular indices, or distance walked on the 6MWT before exercise intervention at the bedside (Table 1).
2.2 Changes in cardiovascular function SpO2was significantly higher and HR was significantly lower post-6MWT in the intervention group than in the control group after surgery (both P<0.05; Table 2,Figure 2). Exercise-induced SpO2was more strongly associated with the frequency than the amount of cycling at the bedside.

Figure 2 Post-6MWT hemodynamic changes after the 6-minute walk test after surgery
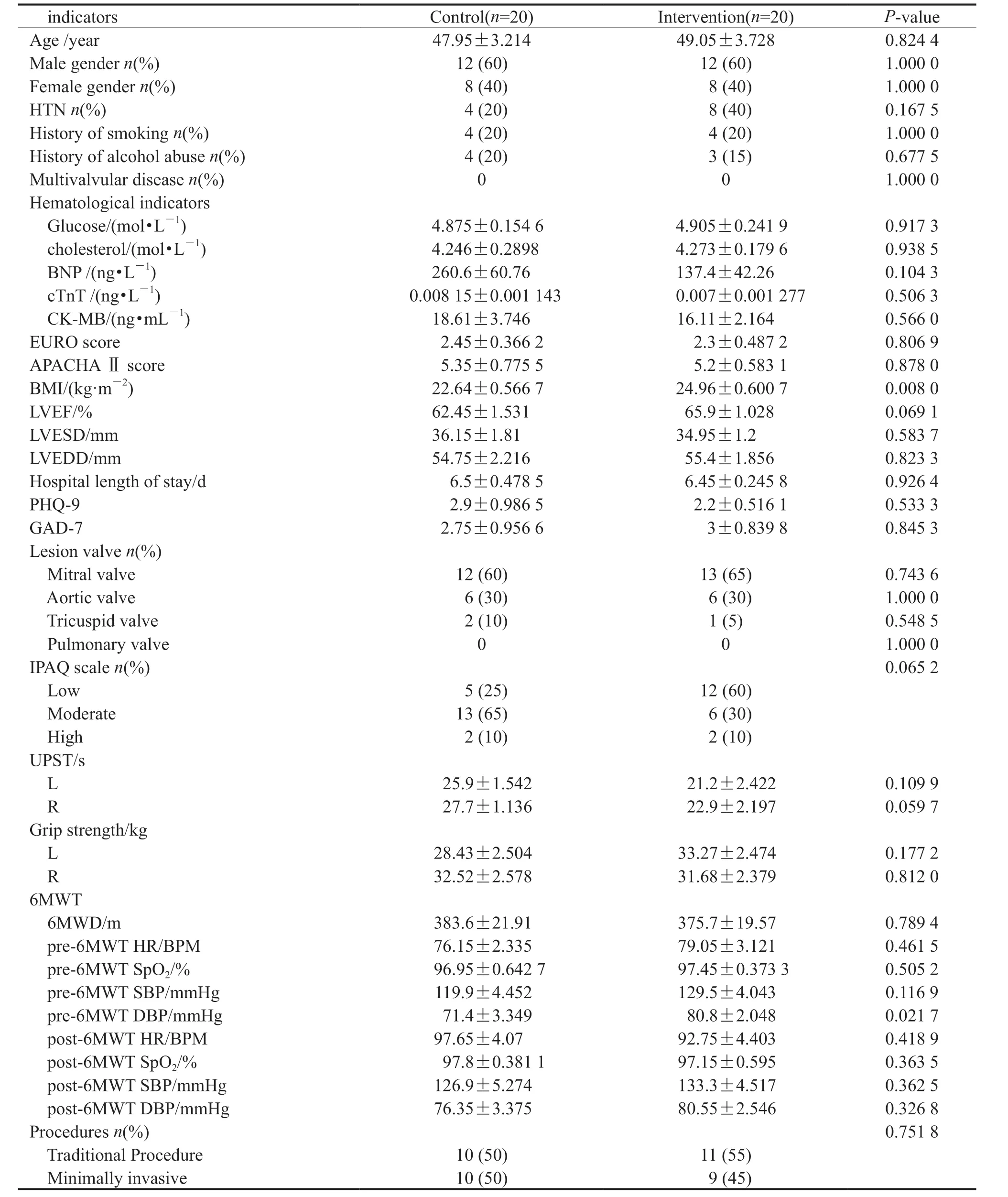
Table 1 Baseline demographics and clinical characteristics
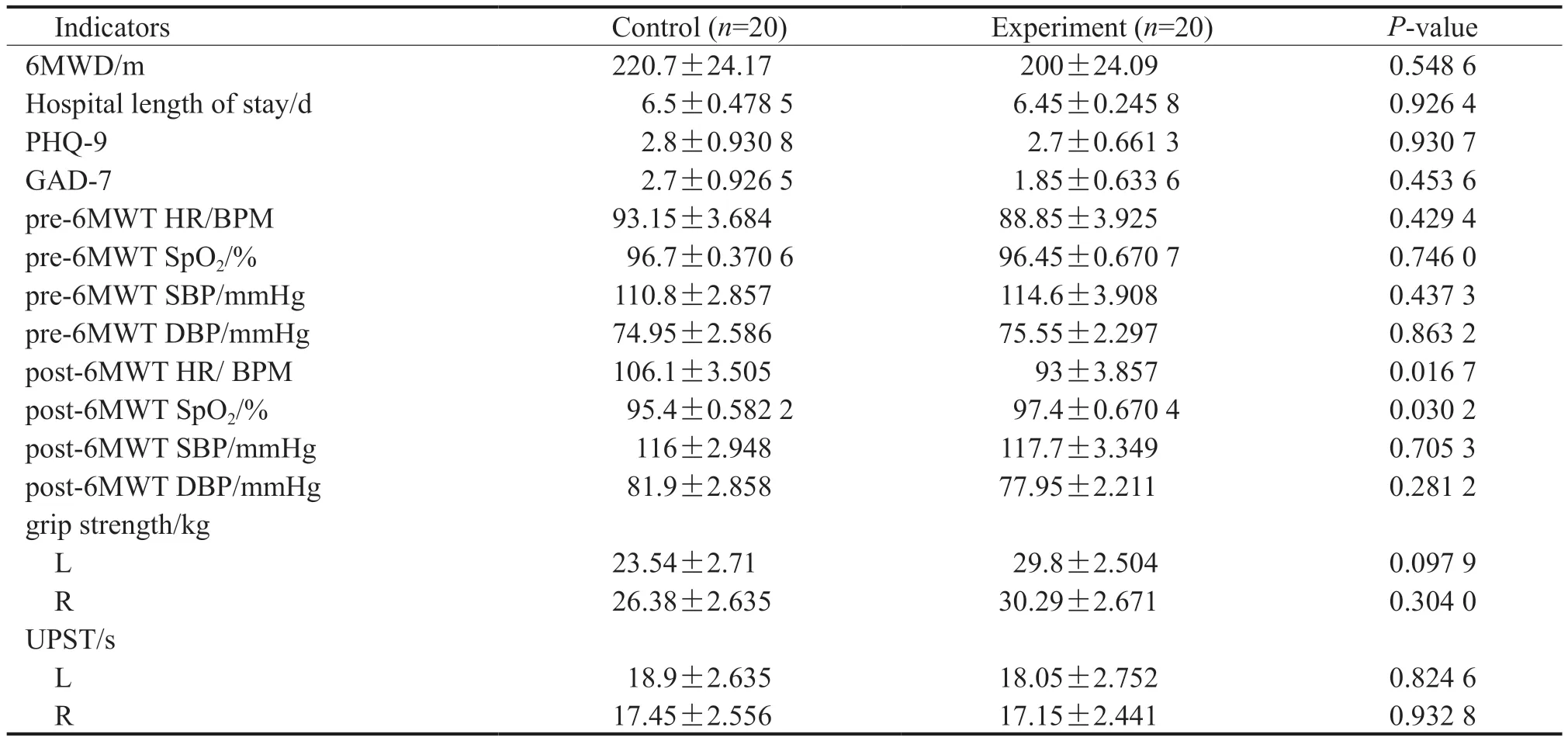
Table 2 Effects of postoperative bedside exercise intervention on cardiovascular function
3 Discussion
This study investigated the effect of exercise at the bedside on cardiac function after isolated mitral and/or aortic valve surgery by comparing the distance walked on the 6MWT and vital signs between an exercise intervention group and a control group.
Roul et al[9]investigated the prognostic value of the 6MWT in 121 patients with New York Heart Association class Ⅱ or Ⅲ heart failure who were followed up with cardiopulmonary exercise testing and the 6MWT for a mean of 1.53±0.98 years[2].They found that patients who could walk for <300 m on the 6MWT were somewhat weaker than those who could walk for longer distances, that the distance walked on the 6MWT after physical training was associated with left ventricular function. Roberts et al[1]assessed HR recovery in 30 patients with acute coronary syndrome or coronary artery disease using the 6MWT and measurement of the C-reactive protein level for 8 weeks. They found that HR during the 6MWT improved in the setting of an exercise-based cardiac rehabilitation program.
Postoperative hemodynamic characteristics before and after the 6MWT were compared between the two groups in this study. Bruce et al[8]found that patients with coronary artery disease developed angina pectoris, restricted chronotropic capacity, and a simultaneous decrease in HR and systemic arterial pressure, which could be fatal without knowledge of factors affecting stress. This study found that the SpO2started to improve in patients in the intervention group in the early postoperative period. The mean SpO2value before the 6MWT was similar before and after surgery in the two study groups. The post-6MWT SpO2value was lower in the control group than that in the intervention group (P=0.030 2). This finding confirms that the cardiorespiratory function was improved by bedside cycling for 3 min/d as part of a cardiac rehabilitation program.
A moderately significant HR maintenance to baseline before and during stress was found after surgery in the intervention group, while the control group showed blunting of the HR response. A variety of heart diseases can cause blunting of the HR response during stress for various reasons; for example, it could be associated with systemic arterial hypoxemia in a cyanosed cardiac patient. Therefore,a significant HR response not only excludes intraoperative injury to the sinoatrial node but also helps to regulate the cardiovascular system[9]. A similar study by Westerdahl et al[10]investigated the effects of deep-breathing exercises after coronary artery bypass grafting and found that breathing exercises during the first 4 days after cardiac surgery reduced the risk of postoperative complications,including atelectasis, and improved the arterial blood gas level (arterial hypoxemia) and pulmonary function. Their findings suggest that exercise can significantly improve cardiopulmonary function after valve surgery.
In conclusion, this study indicate that a bedside cycling exercise intervention has a positive effect on patients undergoing cardiac rehabilitation after valve surgery but require confirmation in a larger sample size and in patients undergoing other types of cardiac surgery. In addition, improvement in vital signs was attributed to not only exercise but also long-term medication and dietary intervention and rehabilitation measures.
Conflicts of interest All authors declare that there is no conflict of interest.
