A special oropharyngeal oxygenation device to facilitate apneic oxygenation in comparison to high flow oxygenation devices
2022-09-10WolfgangWetschDanielSchroederSimonRichardFinkeDavidSanderHannesEckerBerndttigerHolgerHerff
Wolfgang A.Wetsch,Daniel C.Schroeder,Simon-Richard Finke,David Sander,Hannes Ecker,Bernd W.Böttiger,Holger Herff
1 University of Cologne,Faculty of Medicine,Cologne,Germany
2 University Hospital of Cologne,Department of Anesthesiology and Postoperative Intensive Care Medicine,Cologne,Germany
3 Department of Anesthesiology and Intensive Care,German Armed Forces Central Hospital of Koblenz,Koblenz,Germany
Abstract Oxygen application and apneic oxygenation may reduce the risk of hypoxemia due to apnea during awake fiberoptic intubation or failed endotracheal intubation.High flow devices are recommended,but their effect compared to moderate deep oropharyngeal oxygen application is unknown.Designed as an experimental manikin trial,we made a comparison between oxygen application via nasal prongs at 10 L/min(control group),applying oxygen via oropharyngeal oxygenation device (at 10 L/min),oxygen application via high flow nasal oxygen with 20 L/min and 90% oxygen (20 L/90% group),oxygen application via high flow nasal oxygen with 60 L/min and 45% oxygen (60 L/45%group),and oxygen application via sealed face mask with a special adapter to allow for fiberoptic entering of the airway.We preoxygenated the lung of a manikin and measured the decrease in oxygen level during the following 20 minutes for each way of oxygen application.Oxygen levels fell from 97 ± 1% at baseline to 75 ± 1% in control group,and to 86 ± 1% in oropharyngeal oxygenation device group.In the high flow nasal oxygen group,oxygen level dropped to 72 ± 1% in the 20 L/90% group and to 44 ± 1% in the 60 L/45% group.Oxygen level remained at 98 ± 0% in the face mask group.In conclusion,in this manikin simulation study of apneic oxygenation,oxygen insufflation using a sealed face mask kept oxygen levels in the test lung at 98% over 20 minutes,oral oxygenation device led to oxygen levels at 86%,whereas all other methods resulted in the decrease of oxygen levels below 75%.
Key words:airway management;apneic oxygenation;HFNO;high flow nasal oxygen;intubation;nasal oxygen;oxygen;tracheal intubation
INTRODUCTION
Awake fiberoptic intubation is the so-called “gold standard”for airway management in case of expected difficult airway.1,2The awake procedure however is perceived to be highly uncomfortable by patients.3,4As a consequence,the technique is usually performed under conscious sedation.5However,sedative medication dose-dependently decreases ventilation efforts and can cause severe hypoxemia and other severe side effects.6-8Thus,preoxygenation and oxygen application are prerequisites to maintain oxygenation at high and safe levels throughout the procedure.Failure to provide sufficient oxygenation may have deleterious consequences for the patient,as standard airway management has a high probability to fail due to the (known) difficult airway.
Several strategies to maintain sufficient oxygenation during awake fiberoptic intubation have been reported.In a publication by Mir et al.,9the authors described a “transnasal humidified rapid-insufflation ventilatory exchange” by the application of high-flow oxygen to maintain oxygenation.Further,actual anaesthesia guidelines (e.g.,for difficult airway management in obstetric anaesthesia) are postulated to apply high flows of oxygen via a nasal cannula.10We developed a special oropharyngeal oxygenation device,which allows the deep laryngeal insufflation of oxygen,thus facilitating apneic oxygenation in difficult airway scenarios,while still offering the option to fiberoptically intubating the patient.11We connected a special commercial oropharyngeal tube split on the front forming a path for the bronchoscope,with an oxygen line ending at the top of the oropharnygeal tube (Figure 1).In this experimental manikin study,using a test lung and full preoxygenation,we evaluated oxygen decrease in this test lung while oxygenating either via oropharyngeal oxygenation device or via several other standard or high flow oxygenation devices.We hypothesized that we would find no difference in oxygen level decline between the groups.
MATERIALS AND METHODS
Experimental setup
We attached a male intubation manikin (Laerdal,Stavanger,Norway) to a rigid test lung with a capacity of 2.5 L,equalling the functional residual capacity (FRC) of a typical male adult.12,13A side-stream port was connected to the bottom of the test lung that continuously takes a gas probe at 200 mL/min.This probe was analysed with a paramagnetic oximeter of a Primus anaesthesia machine (Draeger,Luebeck,Germany)with an accuracy of ±(2.5 Vol% + 2.5% relative).The gas probe volume nearly equals the amount of oxygen consumption during apnoea in an adult with the corresponding functional residual capacity.14
For the oropharyngeal oxygenation device (OOD) group,a special oropharyngeal oxygenation device (with insufflation of oxygen into the deep laryngeal space) was used.Further,this device additionally provides the option to fiberoptically intubate the patient.This device was self-created using a special commercial split oropharyngeal tube together with an oxygen line ending at the top of the oropharnygeal tube (Figure 1A and B).The device has been described in detail.11
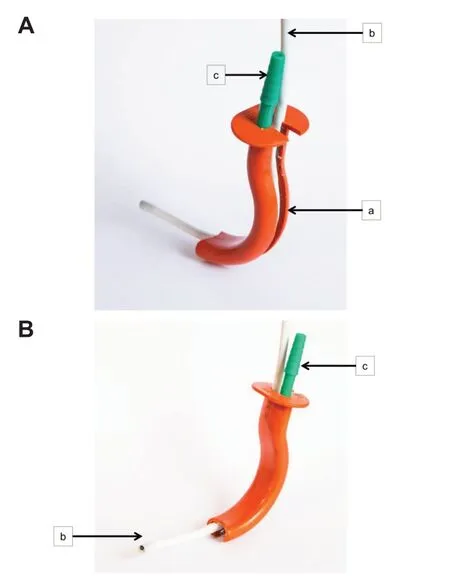
Figure 1:Oropharyngeal oxygenation device (OOD).
For high-flow nasal oxygen (HFNO),the Airvo2 HFNO machines (Fisher&Paykel Healthcare Ltd.,Auckland,New Zealand) with OptiFlow cannulas (Fisher&Paykel Healthcare Ltd.) were used.
For continuous positive airway pressure (CPAP),a Dräger Primus (Primus,Dräger,Lübeck,Germany) was used.It was set to manual mode with 100% oxygen at a flow of 10 L/min,with the adjustable pressure limiting valve set to 5 cmH2O,thus generating a corresponding positive end-expiratory pressure.The facemask was fit tight to the manikin’s face using rubber straps,and a special adapter (Mainzer Adapter,Karl Storz,Tuttlingen,Germany) to allow the entering of the airway with a bron-choscope was used.
Experimental procedures
In the setting,we always made five consecutive experiments with each device,in a randomized order.After preoxygenating the test lung to an oxygen level of 97 ± 1%,the experiments were performed for each of the five groups,measuring the decrease in oxygen levels at the bottom of the test lung during a period of 20 minutes;values at each full minute were recorded.Typical apneic oxygenation strategies are achieved as follows:application of oxygen with a flow of 10 L/min via a standard nasal cannula (control group);application of oxygen with a flow of 10 L/min via the OOD (OOD group);application of HFNO with a special nasal cannula with a flow of 20 L/min and 90% oxygen (HFNO 20 L/90% group),application of HFNO with a special nasal cannula with a flow of 60 L/min and 45%oxygen (HFNO 60 L/45% group);and application of oxygen using CPAP with positive end-expiratory pressure 5 cmH2O and 100% oxygen via a sealed face mask (CPAP group).
Statistical analysis
Data are reported in mean ± standard deviation (SD).After testing for normal distribution (Shapiro-Wilk test) and equal variance test (Brown-Forsythe test),a one-way analysis of variance for repeated measurements was made to evaluate the differences between the groups.This was then followed by Tukey’spost hoctest for pairwise multiple comparisons.This was done using the Sigmaplot software (V 14.0;Systat,San Jose,CA,USA).P-values <0.05 were considered as being significant.
RESULTS
One-way analysis of variance found a significant difference between all five groups (P<0.001).After 20 minutes,oxygen levels fell from 97 ± 1% at the beginning to 75 ± 1% in the control group (P<0.003,vs.HFNO 20 L/90% group;P<0.001,vs.all other groups) and to 86 ± 1% in the OOD group(P<0.001,vs.all the other groups).When using the HFNO device,oxygen levels dropped to 72 ± 1% in the 20 L/90%group (P<0.001,vs.all other groups) and to 44 ± 1% in the 60 L/45% group (P<0.001,vs.all the other groups) after 20 minutes.O2level remained at 98 ± 0% in CPAP group over the entire 20-minute observation period (P<0.001,vs.all other groups;Figure 2).
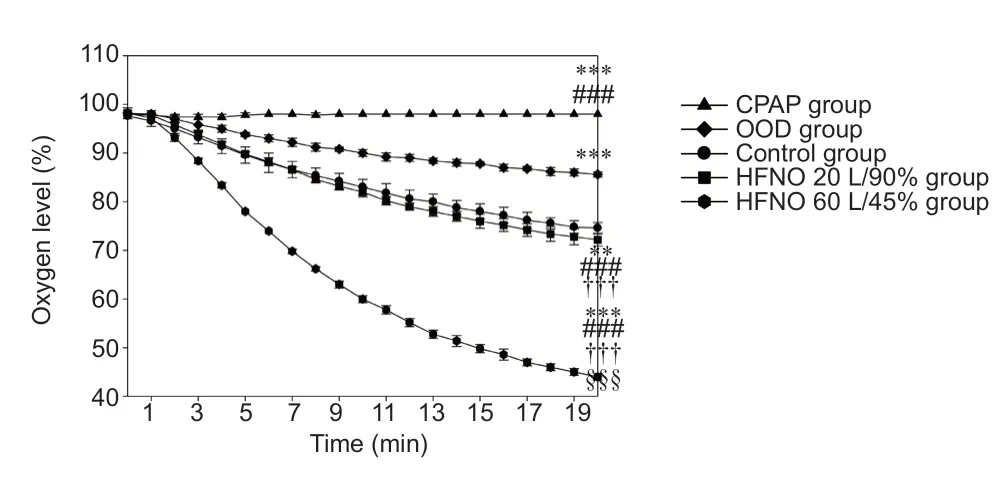
Figure 2:Oxygen levels in the test lung vs.time.
DISCUSSION
In this simulation study,using the OOD for laryngeal oxygen insufflation was more effective in oxygenation than HFNO at any of the used settings,but less effective than using CPAP via sealed face mask.Since desoxygenation regularly occurs during intubation attempts,15-17performing preoxygenation carefully has proven to reduce deoxygenating events during intubation attempts.18-23Applying oxygen in high concentration may be in additional safety tool to maintain apneic oxygenation if breathing of patients is impaired due to sedating agents.
Interestingly,in the HFNO 20 L/90% group,oxygen levels decreased faster than in the control group with 10 L/min oxygen application via nasal prongs.At least we would have expected 90% of oxygen percentage in the test lung after 20 minutes if high-flow application had prevented air and thus nitrogen entering the airway,which was obviously not the case.This phenomenon has been described before,and may be a result of mixing of the insufflated oxygen with nitrogen entering through the manikin’s mouth,thereby generating a turbulent flow like a mixing chamber.24In contrast,higher flow of 20 L/min resulted in even more gas mixing than when using 10 L/min.We speculate this could only be explained by more turbulent gas flows and Bernoulli effects that suctioned ambient air (and thus nitrogen) into the airway,as it has been described in detail for emergency ventilation device.25At very high flows in the HFNO 60 L/45% group,this effect was not visible,since we ended at exactly 44% oxygen percentage,which contradicts any additional nitrogen pouring in the airway than that applied by the high flow oxygenation device.Potentially this very high gas flow at high oxygen concentrations may have resulted in oxygen concentrations in the test lung after 20 minutes that may maintain apneic oxygenation.Unfortunately,with the used Airvo2 HFNO system,due to technical limitations,a higher flow with a higher fraction of inspiratory oxygen could not be achieved:45% O2is the maximum achievable oxygen concentration at 60 L/min;and 90%is the upper limit at 20 L/min.If there are devices available that deliver flows of high concentrated oxygen at very high flows,this should be subject of further studies.
Not surprisingly,the completely closed system by applying a tightly sealed CPAP mask was most effective in avoiding nitrogen entering the airway.However,the special adapter used to place the bronchoscope into the airway would not allow a tracheal tube to pass due to a small diameter.A potential solution might be to a place a special long wire over the working channel into the trachea.This wire can then be used to insert intubation stylets and over these a ventilation tube after removing the face mask.However,that needs some effort,could result in displacement any time and does not guarantee correct placement of the tube.
Last,in times of coronavirus disease 2019 (COVID-19),fiberoptic intubation is a high risk maneuver in regard of risk of infection due to highly infectious aerosols from the airway.26Using HFNO devices that are known to create large amounts of highly infectious aerosols in the surrounding of patient may pose an additional risk of infection for the physician who attempts intubation,and requires high levels of personal protective equipment.27Thus,the availability of a non-commercial OOD that could simply be constructed,may be an additional tool to maintain patient’s oxygenation for awake fiberoptic intubation.Due to significantly lower gas flows,one might postulate that fewer infectious areosols might be produced during the use of these devices.28,29
The setting of nay simulation study is always a limitation.Only experiments in humans would have been more realistic in regard of the airway than our manikin model.However,deliberately withholding ventilation in humans to provoke deoxygenating cannot be justified due to potential harm for patients.Further,the principle of apneic oxygenation had been demonstrated long before.30,31Overall,we assume our model was realistic enough to evaluate our hypothesis.
In conclusion,apneic oxygenation by both application of CPAP via sealed face mask kept oxygen levels at 98% over 20 minutes,and application of 10 L O2via the OOD kept it at 86% after 20 minutes,whereas all other methods resulted in a significant decrease of oxygen levels below 75% over time in our simulation study.
Author contributions
All authors contributed to the study conception and design.Material preparation and data collection were performed by DCS,WAW,HH,and SRF.Analysis was performed by HH,BWB,and HE.The first draft of the manuscript was written by DCS,WAW,DS and HH.All authors commented on previous versions of the manuscript.All authors read and approved the final manuscript.
Conflicts of interest
The authors declare that they do not have a conflict of interest.
Financial support
This study was funded by the University Hospital of Cologne.
Copyright license agreement
The Copyright License Agreement has been signed by all authors before publication.
Plagiarism check
Checked twice by iThenticate.
Peer review
Externally peer reviewed.
Open access statement
This is an open access journal,and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License,which allows others to remix,tweak,and build upon the work non-commercially,as long as appropriate credit is given and the new creations are licensed under the identical terms.
杂志排行
Medical Gas Research的其它文章
- Effects of nitrous oxide on end-tidal carbon dioxide measurements in spontaneously breathing patients under general anesthesia
- Xenon as a transdermal enhancer for niacinamide in Strat-MTM membranes
- Effect of an ionic antineoplastic agent Cytoreg on blood chemistry in a Wistar rat model
- Comparing the effect of xenon and sevoflurane anesthesia on postoperative neural injury biomarkers:a randomized controlled trial
- Potential role of hydrogen sulfide in central nervous system tumors:a narrative review
- Role of hyperbaric oxygen in glioma:a narrative review