Inflammation-based different association between anatomical severity of coronary artery disease and lung cancer
2022-09-06YaWeiZHAOKaiXinYANMingZhuangSUNYiHaoWANGYunDaiCHENShunYingHU
Ya-Wei ZHAO, Kai-Xin YAN, Ming-Zhuang SUN, Yi-Hao WANG, Yun-Dai CHEN,Shun-Ying HU,✉
1. Department of Cardiology, Chinese PLA General Hospital, Beijing, China; 2. Medical School of Chinese PLA, Beijing,China
*The authors contributed equally to this manuscript
ABSTRACTBACKGROUND Coronary artery disease (CAD) is associated with cancer. The role of inflammation in the association of CAD with cancer remains unclear. The study investigated whether inflammation could impact the relationship between CAD and lung cancer.METHODS The study involved 96 newly diagnosed lung cancer patients without receiving anti-cancer therapy and 288 matched non-cancer patients. All the patients underwent coronary angiography and were free from previous percutaneous coronary intervention or coronary artery bypass grafting. SYNTAX score (SXscore) were used to assess severity of CAD. High SXscore (SXhigh)grade was defined as SXscore > 16 (highest quartile). Neutrophil-to-lymphocyte ratio (NLR) served as an inflammatory biomarker.NLR-high grade referred to NLR > 2.221 (median).RESULTS Among 384 study patients, 380 patients (98.96%) had NLR value (median: 2.221, interquartile range: 1.637-3.040). Compared to non-cancer patients, lung cancer patients had higher rate of SXhigh among total study patients (P = 0.014) and among patients with NLR-high (P = 0.006), but had not significantly higher rate of SXhigh among patients with NLR-low (P = 0.839). Multivariate logistic regression analysis showed that SXhigh was associated with lung cancer [odds ratio (OR) = 1.834, 95% CI: 1.063-3.162, P = 0.029]. Subgroup analysis showed that SXhigh was associated with lung cancer among patients with NLR-high (OR =2.801, 95% CI: 1.355-5.794, P = 0.005), however, the association between SXhigh and lung cancer was not significant among patients with NLR-low (OR = 0.897, 95% CI: 0.346-2.232, P = 0.823).CONCLUSIONS Inflammation could lead different association between anatomical severity of CAD and lung cancer. Severity of CAD was significantly associated with increased risk of lung cancer among patients with high inflammation rather than among patients with low inflammation.
Atherosclerotic cardiovascular disease(ASCVD) and cancer are chronic diseases which are considered as two main causes of death all over the world.[1,2]ASCVD and neoplasms are generally considered to be two independent diseases, with very different clinical manifestations and prognosis, however, more research showed that ASCVD and cancer often coexisted in a same individual, and that patients with atherosclerosis have an increased risk of cancer, while patients with cancer also have a significantly increased risk of atherosclerosis.[2]The Sakakibara Health Integrative Profile cohort study showed that prevalence and mortality of cancer were higher in patients with ASCVD than in patients without ASCVD.[3]The study showed that ASCVD may have a potential risk for cancer developments.[3]Another study showed that carotid atherosclerosis was significantly related to the occurrence of colorectal tumor.[4]
Lung cancer is the most common incident cancer and the leading cause of cancer death.[5]Our previous study indicated that anatomical severity of coronary artery disease (CAD) was associated with increased risk of lung cancer.[6]The study indicated that there was direct link between CAD and cancer,[6]however, the mechanism underlying the link between CAD and lung cancer is not fully clear.
Inflammation is considered a common risk factor for both CAD and cancer.[7,8]A large number of studies showed that inflammation plays a key role in the pathogenesis of CAD and cancer, respectively.[9-12]Whether inflammation can impact the association of anatomical severity of CAD with cancer is currently rarely known. Based on our previous study, the present study was to investigate whether inflammation differences exist in the relationship between CAD and lung cancer and ascertain the impact of inflammation on the association of anatomical severity of CAD with lung cancer. To make sure whether there is inflammation-related different association between CAD and lung cancer will be beneficial to better manage the two critically threatening human health diseases.
It is well known that there are various types of inflammatory biomarkers such as C-reactive protein,interleukin 6, and tumor necrosis factor α, et al.[13]Neutrophil-to-lymphocyte ratio (NLR) has been claimed to reflect systemic inflammation and which can be easily obtained from complete blood cell counts.[14]NLR also has been confirmed to be associated with cardiovascular diseases and cancer, respectively.[8,15-19]In the present study, we assessed the inflammatory status of study patients with NLR as the other studies.[15,18]Further we analyzed the association between CAD and lung cancer among subgroup patients stratified by NLR in order to detect the effect of inflammation on the association of CAD with lung cancer.
METHODS
Study Population
In Department of Cardiology, the First Medical Centre, Chinese PLA General Hospital, Beijing, China,all information of inpatients was kept in the medical record system including coronary angiograms.There were 201 patients with lung cancer (ICD-10 code:34), and 51,106 patients without any cancer among 51,928 patients who underwent coronary angiography (ICD-9-CM codes: 88.5, 88.55, 88.56, and 88.57)from January 1, 2009 to December 31, 2020. The study protocol was approved by the Institutional Review Board of Chinese PLA General Hospital (S2022-254-01).
Lung cancer diagnosis was validated according to pathological diagnosis. Among the 201 lung cancer patients, 96 newly diagnosed lung cancer patients without receiving any anti-cancer treatments or previous percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) were enrolled in this study. From the 51,106 non-cancer patients, 288 control patients were enrolled by propensity score matching to the included lung cancer patients (1:3) according to gender, age, family history of CAD, body mass index (BMI), smoking, hypertension, diabetes mellitus, and hyperlipidemia.All the included patients had not history of any connective tissue disease or other inflammatory diseases, and had not history of PCI or CABG before the indexed hospitalization. A flow chart of study patients enrollment process was shown in Figure 1.
Assessment of Inflammatory Status in Patients
In order to assess inflammatory status of study patients, we made use of NLR as inflammatory marker.[8,18]Complete blood cell counts, which included the total white blood cells, neutrophils, and lymphocytes, were obtained from the medical record system which was tested at admission. NLR was calculated as neutrophil count divided by lymphocyte count. In the study, the median of NLR was 2.221, so we defined NLR grade as NLR-low (NLR ≤ 2.221)and NLR-high (NLR > 2.221).
Assessment of Anatomical Severity of CAD Based on Coronary Angiography
As in previous studies, we assessed the anatomical severity of CAD using SYNTAX score (SXscore)based on coronary angiography,[20-23]which was described in full elsewhere.[24,25]All of the angiographic variables pertinent to SXscore calculation were computed by two blinded experienced interventional cardiologists. When the SXscore of each patient was different between the two cardiologists, they would discuss the angiograms and give a common SXscore.Final SXscores were calculated per patient and saved in a dedicated database. SXscore of 16 was the highest quartile among total study patients. Low SXscore(SXlow) was defined as SXscore ≤ 16 and high SXscore (SXhigh) was defined as SXscore > 16. In logistic regression analysis, we defined SXhigh as positive.
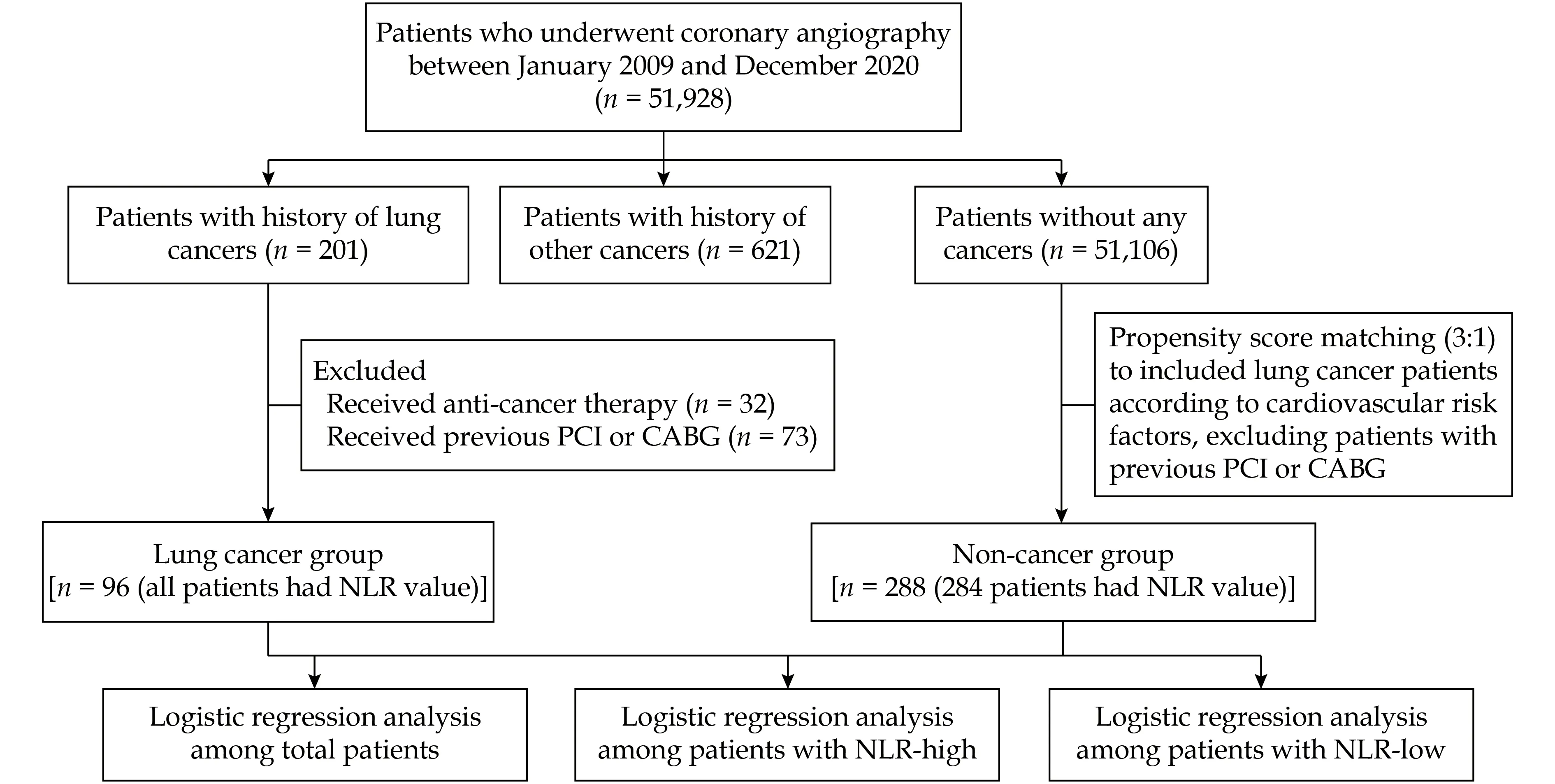
Figure 1 Flow chart of study patients. CABG: coronary artery bypass grafting; NLR: neutrophil-to-lymphocyte ratio; PCI: percutaneous coronary intervention.
Statistical Analysis
Descriptive statistics were presented as counts (percentages) for categorical variables, and mean ± SD or median [interquartile range (IQR)] for continuous variables according to normality of the data. We assessed the normality of the data using skewness and kurtosis normality tests. The Pearson’s chi-squared test or Fisher’s exact probability test were used to examine differences for categorical variables. We used the independent samples t-test to compare means between two groups when variables were normally distributed. The Mann-Whitney U non-parametric statistical test was used to compare difference between two groups for continuous variables without normal distribution.
We assessed the relationship between CAD severity and lung cancer by logistic regression analysis,adjusting for common related risk factors including gender, age, BMI, smoking history, cancer family history, hypertension, diabetes mellitus, and hyperlipidemia. Two-sided P-value < 0.05 were considered statistically significant, and odds ratio (OR) was presented with 95% confidence interval (CI). Statistical analysis was performed using SPSS 22.0 (SPSS Inc., IBM,Chicago, IL, USA).
RESULTS
Patients Characteristics
384 study patients were with 63.66 ± 9.31 years, 86 patients (22.40%) were female. All of the included 96 lung cancer patients had pathological evidence of cancer, 87 patients (90.6%) were diagnosed as nonsmall cell lung cancer, the other nine patients (9.4%)were with small cell lung cancer. 60 patients (62.50%)were at stage I or II, 14 patients (14.58%) were at stage III, six patients (6.25%) were at stage IV, and the other 16 patients (16.67%) could not been confirmed the disease stage. Six patients (6.25%) were metastatic. All the lung cancer patients had not received any anti-cancer treatments before the index coronary angiography.
There was no significant difference for gender, age,smoking history, BMI, family history of CAD, hypertension, diabetes mellitus, hyperlipidemia and cancer family history between lung cancer patients and non-cancer patients. Ejection fraction, lipid profile and fasting blood glucose were comparable between lung cancer patients and non-cancer patients (Table 1).
Overall SXscore ranged from 0 to 40, with a median of 10 (IQR: 4.0-16.4). Highest quartile of SXscore was 16. According to definition of SXhigh and SXlow by highest quartile of SXscore as the cut-off value,96 patients (25%) had SXhigh and 288 patients (75%)had SXlow. Lung cancer patients had higher SX-score than non-cancer patients (median: 12.00, IQR:5.00-19.75 vs. median: 9.00, IQR: 3.00-15.00, P = 0.038)(Table 1).

Table 1 Clinical characteristics of study patients.
Inflammatory Status Among Study Patients
Among 384 study patients, 380 patients (98.96%)had NLR value (median: 2.221, IQR: 1.637-3.040), and four patients had not NLR value because they did not test complete blood cell count during hospitalization. NLR was stratified as NLR-high (NLR > 2.221)and NLR-low (NLR ≤ 2.221) with the median of 2.221 as cut-off value. NLR was significantly higher among patients with SXhigh than among patients with SXlow(median: 2.629, IQR: 1.889-3.548 vs. median: 2.102,IQR: 1.571-2.853, P = 0.001) (Figure 2). Rate of NLRhigh in SXhigh patients was higher than that in SXlow patients (62.80% vs. 45.80%, P = 0.004) (Figure 3).
Impact of Inflammation on Association of CAD with Lung Cancer

Figure 2 NLR among patients stratified by SYNTAX score grades. NLR of patients with SXhigh was significantly higher than that of patients with SXlow (median: 2.629, IQR: 1.889-3.548 vs.median: 2.102, IQR: 1.571-2.853, P = 0.001). IQR: interquartile range; NLR: neutrophil-to-lymphocyte ratio; SXhigh: high SYNTAX score; SXlow: low SYNTAX score.

Figure 3 Distribution of NLR grades among patients stratified by SYNTAX score grades. The rate of NLR-high was higher among patients with SXhigh compared to patients with SXlow (62.80%vs. 45.80%, P = 0.004). NLR: neutrophil-to-lymphocyte ratio; SXhigh: high SYNTAX score; SXlow: low SYNTAX score.
We compared the difference of SXscore grades between lung cancer patients and non-cancer patients among total patients and among subgroup patients stratified by NLR grades. Among total patients, lung cancer patients had higher rate of SXhigh compared to non-cancer patients (34.4% vs. 21.9%, P = 0.014). Moreover, lung cancer patients had higher rate of SXhigh than non-cancer patients among patients with NLRhigh (45.5% vs. 25.2%, P = 0.006), however, lung cancer had not significantly higher percentage of SXhigh than non-cancer patients among patients with NLR-low (19.5% vs. 18.1%, P = 0.839) (Table 2).
Logistic regression analysis was used to assess the association of CAD and lung cancer. Among total patients, univariate logistic regression analysis showed that OR of SXhigh for lung cancer was 1.871(95% CI: 1.129-3.101, P = 0.015), and multivariate logistic regression analysis showed that SXhigh was associated with increased risk of lung cancer with an OR of 1.834 (95% CI: 1.063-3.162, P = 0.029) after adjusting for gender, age, BMI, smoking, cancer family history, hypertension, diabetes mellitus and hyperlipidemia (Table 3).
Further, we made subgroup analysis stratified by level of inflammation according to NLR. Among the patients with NLR-high, univariate logistic regression analysis showed that OR of SXhigh for lung cancer was 2.475 (95% CI: 1.282-4.779, P = 0.007). After adjusted for gender, age, BMI, smoking, cancer family history, hypertension, diabetes mellitus and hyperlipidemia, SXhigh was associated with the increased risk of lung cancer compared with SXlow (OR =2.801, 95% CI: 1.355-5.794, P = 0.005) (Table 3).
Among the patients with NLR-low, OR of SXhigh for lung cancer was 1.095 (95% CI: 0.455-2.635, P = 0.839)in univariate logistic regression model, and was 0.897(95% CI: 0.346-2.232, P = 0.823) in multivariable logistic regression model, respectively. The results didnot show that SXhigh was significantly associated with the risk of lung cancer in patients with NLRlow (Table 3).
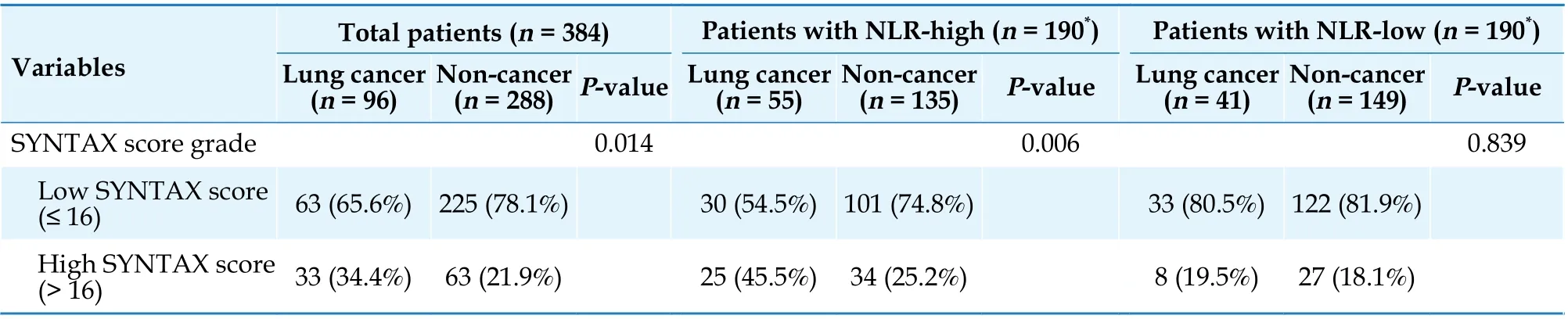
Table 2 Comparison of SYNTAX score grades between lung cancer patients and non-cancer patients.

Table 3 The OR and 95% CI of high SYNTAX score for lung cancer in total patients and subgroup patients stratified by NLR.
DISCUSSION
To our knowledge, the present study was the first to demonstrate inflammation-based different association between anatomical severity of CAD and lung cancer. The study showed that severity of CAD was associated with lung cancer, however, CAD was significantly associated with lung cancer among patients with high inflammation rather than among patients with low inflammation. The results indicated that inflammation could affect the association between anatomical severity of CAD and lung cancer.
Both CAD and cancer are the diseases causing great health burden on human all over the world. There has been growing interest in the relationship between cardiovascular diseases and cancer, however, more attention has been attracted by anti-cancer treatmentinduced cardiotoxicity.[7,20,21]Currently, more and more evidence show that CAD is directly associated with risk of cancer.[3,6,26,27]The epidemiology, pathobiology, and treatment of CAD and cancer have been the focus of intensive study for decades, and it is a consensus that both CAD and cancer are multifactorial diseases.[1,28]Preclinical and clinical evidence indicate that cancer progression is determined not only by the tumor genetic landscape, but also by complex interactions within the tumor microenvironment and systemic host milieu.[29,30]Inflammation is one of important microenvironment elements.[29]Chronic inflammation is a pathological condition characterized by continued active inflammation response and tissue destruction which contributes to the development of cardiovascular diseases and cancer,respectively.[31,32]
NLR has been confirmed to be associated with various diseases as an inflammatory marker.[8,15,18,19]Comparing with other inflammation biomarkers,[13]NLR is more easily and economical to be obtained from routine complete blood counts. In the present study,98.96% (380/384) of patients had NLR value, so we make use of NLR to assess the inflammatory status of the patients. The results showed that NLR was higher in patients with high SXscore than in patients with low SXscore. The results were consistent with the up-regulated inflammatory status among cardiovascular disease patients.[9,32]The present study showed lung cancer patients had higher SXscore than non-cancer patients among total study patients as well as among patients with NLR-high,however, the difference was not significant between lung cancer patients and non-cancer patients among patients with NLR-low. The results indicated that inflammation may play an important role on the association of CAD and lung cancer.
Furthermore, we investigated the impact of inflammation on the association of CAD and lung cancer. We observed significant association of CAD with lung cancer in the present larger sample study which was consistent with the previous study.[6]In the present study, more important was the subgroup analysis stratified by level of inflammation. The results showed that the association of CAD with lung cancer was significant among patients with NLRhigh, however, significant association between CAD and lung cancer was not observed among patients with NLR-low. The results indicated that the association between CAD and lung cancer may be at least partly driven by inflammation. It was reasonable to infer that inflammation plays an important role in the link between CAD and lung cancer, and NLR may be a potential biomarker for the association between CAD and lung cancer.
The results of the study were significant with clinical implications that it would be necessary to screen lung cancer among severe CAD patients with high inflammation. However, in view of the multidimensional mechanism of inflammation in the pathogenesis of atherosclerotic disease and cancer,[9-11,33-35]the reason for why severe CAD patients with low inflammation was not associated with lung cancer is complex. It should be reasonable to hypothesize that high inflammation can put more effect on progress of both CAD and cancer than low inflammation.How inflammation, CAD and lung cancer interact each other in a same individual is worthy of more clinical and basic investigations in future.
STRENGTHS AND LIMITATIONS
The study had several strengths and limitations.A major strength of the study was the use of NLR to investigate the role of inflammation between association of CAD and lung cancer. NLR as an easily obtained inflammation biomarker has the potential to be widely used in clinical practice. However, there were some limitations for the present study. Firstly, it was a hospital-based study, so the selection bias must be taken into account. In order to minimize the selection bias as can as possible, on the one hand, we enrolled all the newly diagnosed lung cancer patients who had not previous history of PCI or CABG, and on the other hand, we enrolled the control patients by propensity score matching to the lung cancer patients from a bigger sample of 51,106 non-cancer patients. Secondly, cigarette is a well-known risk factor for lung cancer and CAD. Regarding the possible effect of smoking, the smoking history had been balanced between lung cancer patients and non-cancer patients in order to control the confounding impact of smoking, and smoking history had been adjusted in the logistic regression analysis. In future study, it would be important to further examine the role of inflammation on association between CAD and lung cancer among never smokers. Last but not least, the present cross-sectional study showed inflammation could change the association of CAD and lung cancer, but could not explain the underlying mechanism. It is necessary to further elucidate the role of inflammation in bigger prospective study and basic research in future. Moreover, it is also necessary to further investigate the effect of types and stages of lung cancer on association between CAD and lung cancer which had not been analyzed due to the small sample of lung cancer patients.
CONCLUSIONS
In brief, the study firstly observed inflammationbased different association of anatomical severity of CAD with lung cancer. It showed that anatomical severity of CAD was associated with lung cancer, however, the association of the two diseases was significant among patients with high level of inflammation rather than among patients with low level of inflammation. The results indicated that inflammation may play an important role in the association between CAD and lung cancer. The results also give us an alert that it may be notable to closely screen lung cancer among patients with severe CAD, especially among patients with high level of inflammation. Even now the study gave us some new indications, it needs bigger prospective clinical studies and basic research to further elucidate the relationship and the underlying mechanism for the association of CAD with lung cancer.
ACKNOWLEDGMENTS
This study was supported by the National Natural Science Foundation of China (No.82173450). All authors had no conflicts of interest to disclose.
杂志排行
Journal of Geriatric Cardiology的其它文章
- Effect of uninterrupted dabigatran or rivaroxaban on achieving ideal activated clotting time to heparin response during catheter ablation in patients with atrial fibrillation
- Long-term outcome of percutaneous or surgical revascularization with and without prior stroke in patients with threevessel disease
- Relationship between arterial stiffness and cognitive function in outpatients with dementia and mild cognitive impairment compared with community residents without dementia
- Serum triglycerides concentration in relation to total and cardiovascular mortality in an elderly Chinese population
- The predictive value of triglyceride-glucose index for in-hospital and one-year mortality in elderly non-diabetic patients with ST-segment elevation myocardial infarction
- Extracorporeal membrane oxygenation successfully treated massive right ventricular myocardial infaction with aneurysm
