Extracorporeal membrane oxygenation successfully treated massive right ventricular myocardial infaction with aneurysm
2022-09-06ChengDuoZHANGLiJieSUNBaoXiaCHENJiangLiHANShaoMinCHENXinYuWANGYuanYuanFANDanLIXinYeXU
Cheng-Duo ZHANG, Li-Jie SUN✉, Bao-Xia CHEN, Jiang-Li HAN, Shao-Min CHEN, Xin-Yu WANG, Yuan-Yuan FAN, Dan LI, Xin-Ye XU
Department of Cardiology, Peking University Third Hospital, NHC Key Laboratory of Cardiovascular Molecular Biology and Regulatory Peptides, Beijing, China
Acute obstruction of the right coronary artery (RCA) can lead to right ventricular myocardial infarction (MI), which rarely lead to cardiogenic shock (CS). Hemodynamic stability could be restored through fluid resuscitation and vasoactive drugs in most circumstances. Here,we present a highly representative case of refractory CS caused by massive right ventricular MI with apical aneurysm formation, who was successfully treated with extracorporeal membrane oxygenation (ECMO)post severe complication of acute right coronal dissection. Through this typical case, we aimed to provide a more in-depth understanding of ECMO for the treatment of high-risk patients such as CS caused by right heart failure, which is resistant to conservative treatment.
A 76-year-old male patient who experienced persistent angina pectoris for about 3 h. At the primary medical contact, the patient‘s blood pressure (BP) was 72/43 mmHg, atrial fibrillation with heart rate 42 beats/min. He was irritable with wet and cold extremities, cyanosis of mouth and lip, clear lung fields and low heart sound. The electrocardiogram revealed ST-segment elevation with atrial fibrillation and the third degree of atrioventricular block (Figures 1 &2). A temporary pacemaker was placed. As CS attacked with serum lactate of 14.6 mmol/L, rapid fluid resuscitation, acid correction as well as vasopressors were administered, and then, emergency coronary angiography was performed. A diffused dissection throughout the RCA with TIMI flow grade I blood flow was observed (Figure 3A). The left anterior descending artery and the left circumflex artery showed unrestricted blood flow (Figure 4).The revascularization was performed with five drug-eluting stents replacement in series to the RCA (Figure 3B & 3C). However, the coronary flow did not completely recover after the operation with TIMI flow grade I. Owing to the hypotension during operation, intra-aortic balloon pumping (IABP)was implanted with maximum dose of intravenous dopamine 20 ug/kg per min and norepinephrine 1 ug/kg per min. Non-invasive ventilation was used to correct his hypoxia state. After above treatment,BP was maintained at a level of 120/70 mmHg with dopamine decreased to 12 ug/kg per min and norepinephrine 0.2 ug/kg per min, lactic acid dropped to 3-4 mmol/L for a time.

Figure 1 Electrocardiogram showed ST-segment elevation in leads II, III, aVF and V4-V6 leads with atrial fibrillation and the third degree atrioventricular block in emergency.
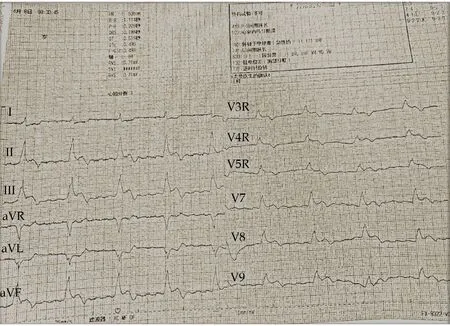
Figure 2 Electrocardiogram showed ST-segment elevation in leads II, III, aVF, V3R-V5R and V7-V9 leads while placing temporary pacemaker in emergency.
Troponin T level > 10 ng/mL and creatine kinase-MB up to 209 U/L suggested massive MI. On the third day of admission, his BP decreased to 100/60 mmHg with heart rate 130-140 beats/min, and oxygen saturation rapidly decreased to 90% which could not be corrected at 100% oxygen concentration with endotracheal intubation. As the central venous pressure rose to 22 mmHg, we conducted a transthoracic echocardiogram, and it demonstrated decreased left ventricular ejection fraction (LVEF) of 35% with tricuspid annular plane systolic excursion(TAPSE) of 12 mm, inferior vena cava obviously widened and respiratory movement disappeared, all indicating a significant reduction in primary right ventricular function (Figure 5).
Considering his CS with ineffective drug treatment post-massive MI, veno-arterial-ECMO (VAECMO) was conducted. After that, hemodynamics stabilized rapidly, vasopressors were down-regulated and stopped within 12 h with lactate acid to be normal. And hypoxemia was rectified quickly.

Figure 3 Coronary angiography results of the right coronary artery. (A): Coronary angiography before stent; and (B & C): coronary angiography after stent.

Figure 4 Coronary angiography results of the left anterior descending artery (A) and the left circumflex artery (B).
After 3 days’ support of ECMO, the patient’s liver and renal function recovered, so we halted IABP.Echocardiography reexamination showed right ventricular aneurysm formed and LVEF were 40%-45%(Figure 6). One week later, echocardiography showed TAPSE increased to 14 mm, so ECMO was discontinued. His condition gradually stabilized. Three weeks after MI, TAPSE returned to be 17 mm and LVEF 52%, one month later, the patient was able to engage in simple activities of daily life at home. Cardiac magnetic resonance imaging revealed a right ventricular apical aneurysm with right ventricular enlargement and right ventricular ejection fraction of 18% (Figure 7).
Primary right ventricular failure arisen from MI will lead to decreased ejection fraction of the right ventricle, an elevated right ventricular end diastolic volume from baseline.[1]It will in turn lead to decreased left ventricular filling and hence a low cardiac output state and hypotension, and then progressing to CS. It is reported that CS caused by right ventricular MI is rare, but with a mortality as high as 56%.Bowers, et al.[2]emphasized successful RCA trunk and right ventricular branch revascularization can quickly improve hemodynamics. Unfortunately, in this case, percutaneous coronary intervention to the diffused dissection throughout RCA might likely do not revascularize the proximal RCA and the right ventricular branches. The large infarcted area involved right ventricular wall, leading to gradual enlargement of the right ventricle and right ventricular aneurysm. Ischemia-induced right ventricular aneurysm are rare.[3-6]A significant positive relationship between right ventricular aneurysm and mortality after acute MI has been demonstrated before.[7]

Figure 5 Transthoracic echocardiogram demonstrated a tricuspid annular plane systolic excursion of 12 mm.
Medication should include optimizing preload,augmenting contractility with vasopressors and inotropes. The current view tends to select appropriate candidates and best timing for mechanical circulatory support (MCS) as 40%-50% of CS patients can not survive with sufficient medical therapy.[8,9]Although studies have shown that the use of IABP can reduce biventricular afterload and increase myocardial oxygen supply to improve right ventricular function.[9]To our patient, severe progressive right ventricular failure would still lead to increased preload of right ventricle and decreased preload of left ventricle and eventually reduction of cardiac output, leading to CS. As the gradual deterioration of multiple organ dysfunction, more advanced MCS was necessary.

Figure 6 Transthoracic echocardiogram demonstrated right ventricular aneurysm formed.
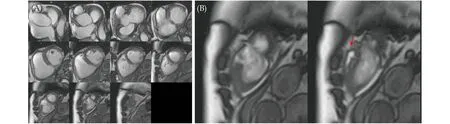
Figure 7 Cardiac magnetic resonance imaging showed right ventricular enlargement (A) and apical RVA during systole (B, red arrow indicates RVA) in movie series. RVA: right ventricular aneurysm.
The right ventricular circulatory support was the appropriate option, but it was not approved for use in China. ECMO was undoubtedly the best choice for this patient, because VA-ECMO can pump enough blood from the right heart system to the arterial circulation, so as to unload the high-volume of the right ventricle, provide systemic circulation perfusion, and maintain systemic oxygenation. As we can see that, after VA-ECMO implantation, his condition rapidly stabilized. The use of VA-ECMO is increasing rapidly with CS as the most common indication, while the data for typical CS after acute right ventricular MI are limited. Therefore, we suggest early initiation of advanced MCS, just before the onset of refractory CS to shorten the duration of hypoperfusion and reduce complications.
To our knowledge, this is the first report of a patient with inferior posterior wall combined with right ventricular MI, right ventricular aneurysm and CS caused by diffused dissection throughout the RCA.We successfully treated him through VA-ECMO combined with IABP. This case demonstrates the value of ECMO in assisting right heart failure to ensure stable hemodynamics and myocardial recovery in patients with refractory CS caused by acute massive right ventricular MI.
We address an active consideration for advanced MCS like ECMO in a drug resistant right ventricular failure patient, aiming to provide auxiliary support during the acute insult period and avoid irreversible damage to vital organs.
ACKNOWLEDGMENTS
All authors had no conflicts of interest to disclose.
杂志排行
Journal of Geriatric Cardiology的其它文章
- Effect of uninterrupted dabigatran or rivaroxaban on achieving ideal activated clotting time to heparin response during catheter ablation in patients with atrial fibrillation
- Inflammation-based different association between anatomical severity of coronary artery disease and lung cancer
- Long-term outcome of percutaneous or surgical revascularization with and without prior stroke in patients with threevessel disease
- Relationship between arterial stiffness and cognitive function in outpatients with dementia and mild cognitive impairment compared with community residents without dementia
- Serum triglycerides concentration in relation to total and cardiovascular mortality in an elderly Chinese population
- The predictive value of triglyceride-glucose index for in-hospital and one-year mortality in elderly non-diabetic patients with ST-segment elevation myocardial infarction
