Acceptability of a task sharing and shifting model between family physicians and physiotherapists in French multidisciplinary primary healthcare centres: a cross- sectional survey
2022-07-26AmlieKechichianFranoisDesmeulesPaulineGirardNicolasPinsault
Amélie Kechichian , François Desmeules, Pauline Girard, Nicolas Pinsault
ABSTRACT
lNTRODUCTlON
Musculoskeletal disorders (MSD) are a common reason for consulting in family practice or in emergency departments.1–3The increasing demand for healthcare services and ageing population substantially increase the primary care workload in France to a point of saturation. In addition, workforces are unequally divided up within the country. Non- optimal resources allocation and reduced access to care may lead to poorer quality of care.4Internationally, many models of primary care delivery have been proposed to promote healthcare team approaches.56Multidisciplinary task management is a way to help facing the challenge of access to primary care services, while maintaining or even improving the quality of patient care.7These models require interprofessional collaboration to improve patient functional outcomes,professionals’ adherence to recommended practices and the promotion of an efficient use of healthcare resources.They are applicable for various health conditions including MSDs.89This close collaboration between team members can sometimes lead to an expansion of the professionals’roles.610To this end, the scope of each professional role may be redefined.11As an example, models of task sharing and task shifting (TS/S) from family physicians to non- physician professionals can partially solve the issue of medical workforce shortages.12–15TS/S involves the redistribution of healthcare tasks within workforces and communities.16Task shifting occurs when a task is transferred or delegated, task sharing occurs when tasks are completed collaboratively between providers with different levels of training.17
In France, improving access to primary care is a health policy priority. The reorganisation of primary care professionals is expected, especially by the implementation of new models of collaborative practice including TS/S. In this context, a new model of physiotherapy care for non- urgent and regular MSD is being implemented.18Within multidisciplinary healthcare centres where family health teams are working collaboratively, family physician are now able to delegate consultations to physiotherapists for patients with acute low back pain (LBP).19Eligible patients may consult directly the physiotherapist instead of the family physician.This model expands the usual scope of practice of French physiotherapists, allowing them to deliver medical sick leave certificates and prescribe certain analgesics. It is intended to be deployed at a national level and could include other MSD in the future.15
Acceptability of this innovative model of care by all stakeholders and clinicians is needed so that the model can be successfully implemented.2021Acceptability is influenced by the perceptions of roles and competencies of the healthcare professionals.2223Internationally,several studies have shown a positive perception of the role and skills of physiotherapists by other primary care professionals including family physicians who supported their integration into primary care teams.24–28The aim of this study is to investigate the acceptability of a new model of care involving TS/S by family physicians and physiotherapists working within multidisciplinary primary healthcare centres of the Auvergne- Rhône- Alpes region in France. The acceptability of this new model is documented through three subquestions: (1) How do family physicians (FPs) and physiotherapists (PTs) perceive the model? (2) What is the perception of physiotherapists’competencies in managing acute LBP? (3) How do FPs and PTs perceive the implementation of the model?
METHODS Study design
This descriptive study used a cross- sectional survey design.The survey was defined according to methodology paper about survey research.2930
Description of the TS/S model
The questionnaire referred to the legislative text published in the French official journal which describes the TS/S model as a protocol- based care.19Patients aged 20–55 years with low back pain since less than 4 months may consult directly the PT, without having to see the physician first. They are redirected to the FP if red flags are identified or in the case of a third episode within the past 12 months. Shifted tasks from FP to PT are to diagnose LBP, to prescribe analgesic medication, oral non- steroidal inflammatory drugs, sick leave and to refer patient to traditional physiotherapy when necessary. The objectives of the model are to give physicians more time to care for patients with more serious or complex pathologies, to reduce delays and visits to emergency services and to improve quality of care. FPs and PTs share a training of 10 hours before implementation, can communicate using an electronic platform and meet every 3 months to make sure the care model runs smoothly. A graphical description of the TS/S model is available in online supplemental materials.
Target population
The target population was defined as FPs and PTs working in multidisciplinary primary healthcare centres in the Auvergne- Rhône- Alpes region in France. These healthcare centres are group practices in which a team of primary healthcare practitioners (FPs, PTs, nurses,pharmacists, dentists…) are working together toward the common goal of addressing the local population’s care needs. The Auvergne- Rhône- Alpes region include around 150 multidisciplinary primary healthcare centres.All these centres with a membership to theFédération des Maisons de Santé de la région Auvergne-Rhône-Alpes (Femas Aura) were contacted (n=94). In January 2021, an email including a link to complete an online questionnaire was sent to the 94 participating primary healthcare centres.Coordinators forwarded the email to FPs and PTs of said healthcare centres. The email detailed the purpose of this study as well as the procedure to complete the survey. A reminder email was sent 4 weeks after the initial invitation. Finally, a third reminder was sent 2 weeks later and the survey was closed at the end of March 2021. No identifying data were collected. TheLimeSurveyweb platform was used to administer the survey, which is secured with a data encryption protocol. Participants’ informed consent was obtained prior to completion in accordance with the French General Regulation for Data Protection.
Questionnaire development
The survey was developed based on the current available literature regarding acceptability of new models of care for advanced practice PTs working in primary and secondary care settings worldwide and previously developed by members of our team.3132Literature about interprofessional collaboration in primary care including PT was also used in the development of the survey.833–36
The questionnaire included a total of 38 questions divided in nine sections : (1) Demographic characteristics of participants, (2) Characteristics of the primary healthcare centres, (3) Experience of respondents regarding interprofessional collaboration, (4) Knowledge about the TS/S models, (5) Perception and acceptability of the TS/S model for acute LBP, (6) Perception of PTs skills for the management of acute LBP, (7) Perception of the barriers and facilitators to the implementation of the model, (8) Ability to set up the model and (9) Perception of the deployment of the model. The survey is available in online supplemental materials.
The survey was preceded by a short text informing the participant of the objectives of this survey. Informations about the model were provided at the beginning of sections 4 and 5. The questionnaire used multiple choice questions for the majority of questions, and 5- point or 6- point Likert scale response options. Open questions were also used in the seventh section on barriers and facilitators to the implementation of the model.
The study protocol, methodology and survey were reviewed by authors, two trained PTs (NP and FD) and one FP (PG). The survey was pretested by one PT and one FP working in multidisciplinary centres in order to validate the questions understanding, ease of completion and format of the survey. Both of them reported that the questions were understandable and the survey format was appropriate, but the questionnaire was too long. Modifications were done to shorten the survey after these tests.
Analyses
Raw data were exported into an Excel spreadsheet (Microsoft Redmond, Washington, USA). Descriptive analyses were first conducted with calculations of frequency distributions, means and SD. Results were graphically represented with centred bar plots. Statistical analyses and graphical presentation of results were performed using the R software (R Core Team, 2014).
This study is in line with the French general regulation for data protection and was defined in accordance with the methodological and ethical reference of the French National Commission for Informatics and Liberty.
RESULTS
The response rate calculated per healthcare centre was 85%. A total of 174 respondents answered the survey; 102 participants fully completed the survey and 72 participants partially completed the survey.
Participants’ characteristics
Demographic characteristics of participants
Eighty- one participants (51%) were PTs and 85 (49%)were FPs. Ninety- seven participants were women (56%),and 77 were men (44%). The mean age of participants was 40.3 years old (SD: 10.4). The mean duration of experience within multidisciplinary healthcare centres was 5.04 years (SD: 5.11). The participants worked in 80 multidisciplinary healthcare centres, spreading over the 12 departments of the Auvergne- Rhône- Alpes region.Practice areas were represented as follows: rural area(32%), semi- rural area (27%), urban peripheral area(6%), urban area (24%) and mountain area (10%).
Previous experience with interprofessional collaboration
The majority of FPs and PTs reported to collaborate either frequently (FPs: n=53, 68% and PTs: n=42, 55%) or occasionally (FPs: n=19, 24% and PTs: n=27, 35%) during the past 12 months. None of the participants reported to have never collaborated with either FP or PT in the past 12 months.
Both types of providers reported to frequently refer patient care to each other (FPs: n=64, 82% and PTs: n=36,47%). Interprofessional collaboration activities were frequently or occasionally conducted, including: discussion about patients under common care (FPs: n=23, 29%and PTs: n=32, 42%), meetings to discuss professional and clinical practice issues (FPs: n=19, 24% and PTs: n=34,45%) and conjoint care for patients (FPs: n=24, 31% and PTs: n=33, 43%). Specific details about these activities are available in online supplemental materials.
FPs and PTs’ perception of the model
Perception of the objectives of the TS/S model
Regarding the objectives of the TS/S model, participants mostly agreed that it would favour interprofessional collaboration (FPs: n=55, 98% and PTs: n=47, 96%), highlight PTs’ skills (FPs: n=52, 96% and PTs: n=42, 89%), improve quality of care (FPs: n=47, 89% and PTs: n=42, 88%) and reduce risk of chronicity for patients with LBP (FPs: n=46,90% and PTs: n=40, 98%) (figure 4). Compared with PTs,a larger proportion of FPs disagreed that this TS/S model would reduce their workload (FPs: n=18, 31% and PTs:n=4, 9%) and would reduce emergency department visits(FPs: n=13, 23% and PTs: n=5, 11%). Compared with previous objectives, a larger proportion of both PTs and FPs disagreed that the TS/S model could reduce wait times for patients (FPs: n=20, 39% and PTs: n=16, 36%)(figure 1).
Perception of the specific components of the TS/S model
The majority of PTs and FPs found that the patient’s inclusion criteria for the model to be mostly or totally appropriate (figure 2). The majority of participants perceived the redirection criteria as mostly or totally appropriate(figure 3).
The outcome measures related to performance(number of delegated consultations, redirection rate and mean waiting time before consultation) were considered as mostly or totally sufficient by the majority of participants (figure 4). Most of the participants considered the interprofessional training required before the implementation of the model as mostly or totally sufficient (figure 4). Compared with physiotherapists, a larger proportion of family physicians found mostly or totally relevant the three monthly team meetings needed to ensure that the TS/S model performs according to the intended protocol and to discuss any potential adverse events (FPs: n=52, 98%and PTs: n=41, 87%).
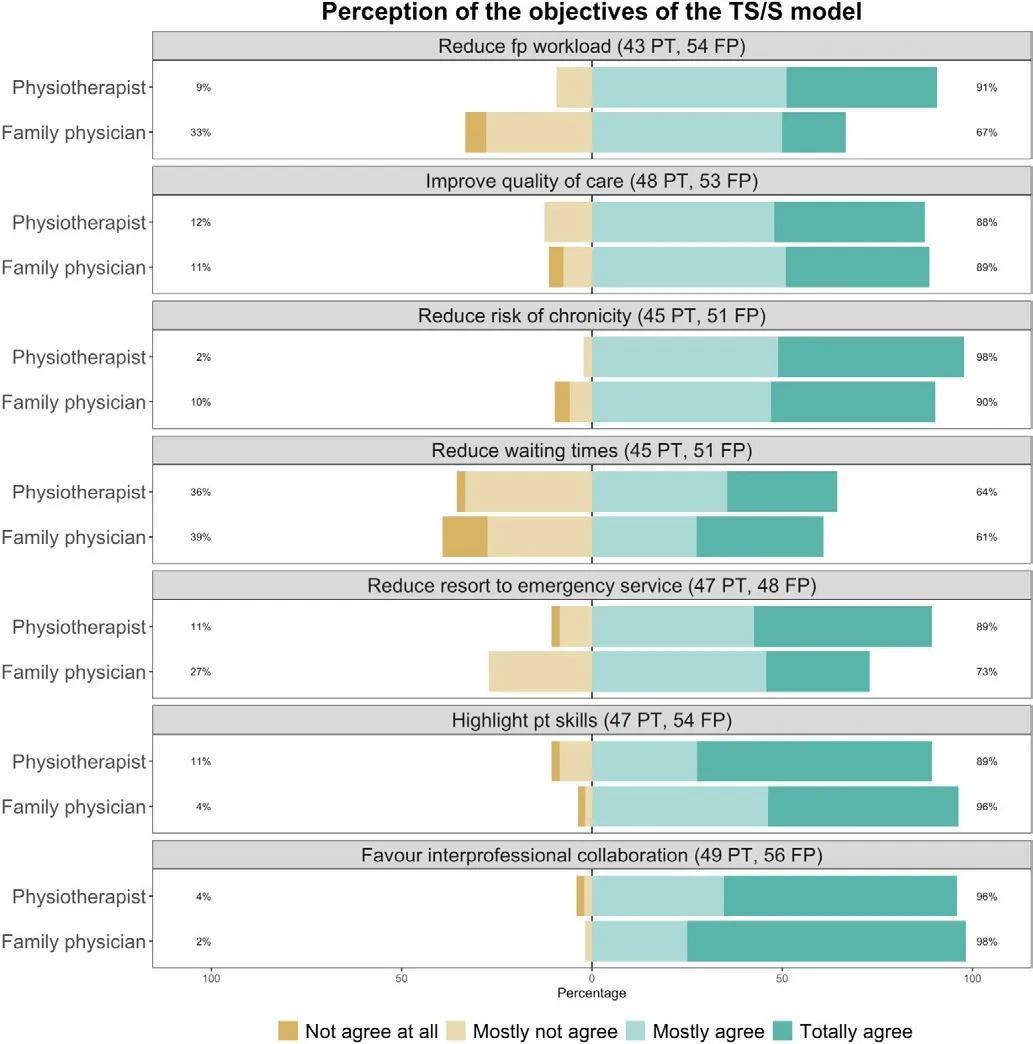
Figure 1 Physiotherapists and family physicians did not unanimously agree with the objectives of the task sharing and shifting model (n=95-105; year=2021). FP, family physician;PT, physiotherapist; TS/S, task sharing and task shifting.
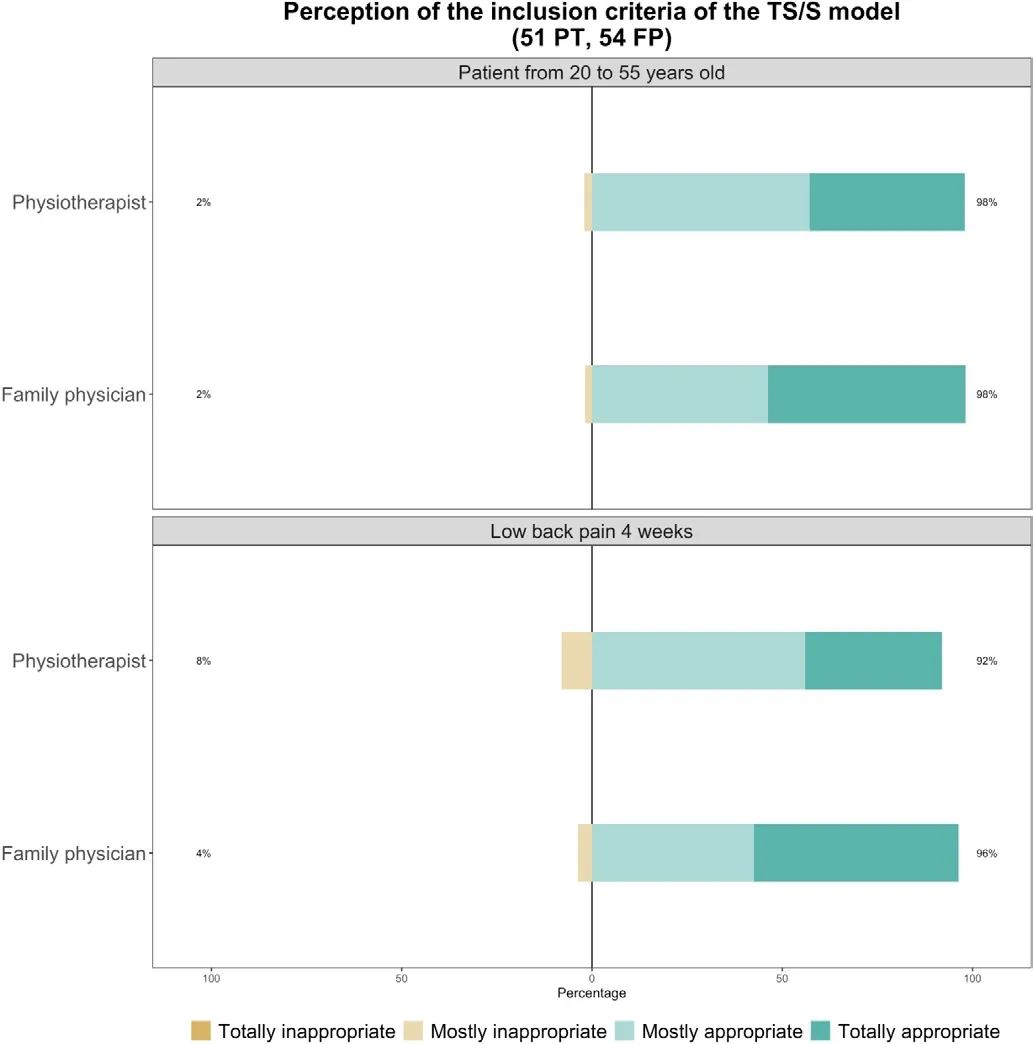
Figure 2 Nearly all physiotherapists and family physicians find the task sharing and shifting model inclusion criteria appropriate (n=105; year=2021). FP, family physician; PT,physiotherapist; TS/S, task sharing and task shifting.
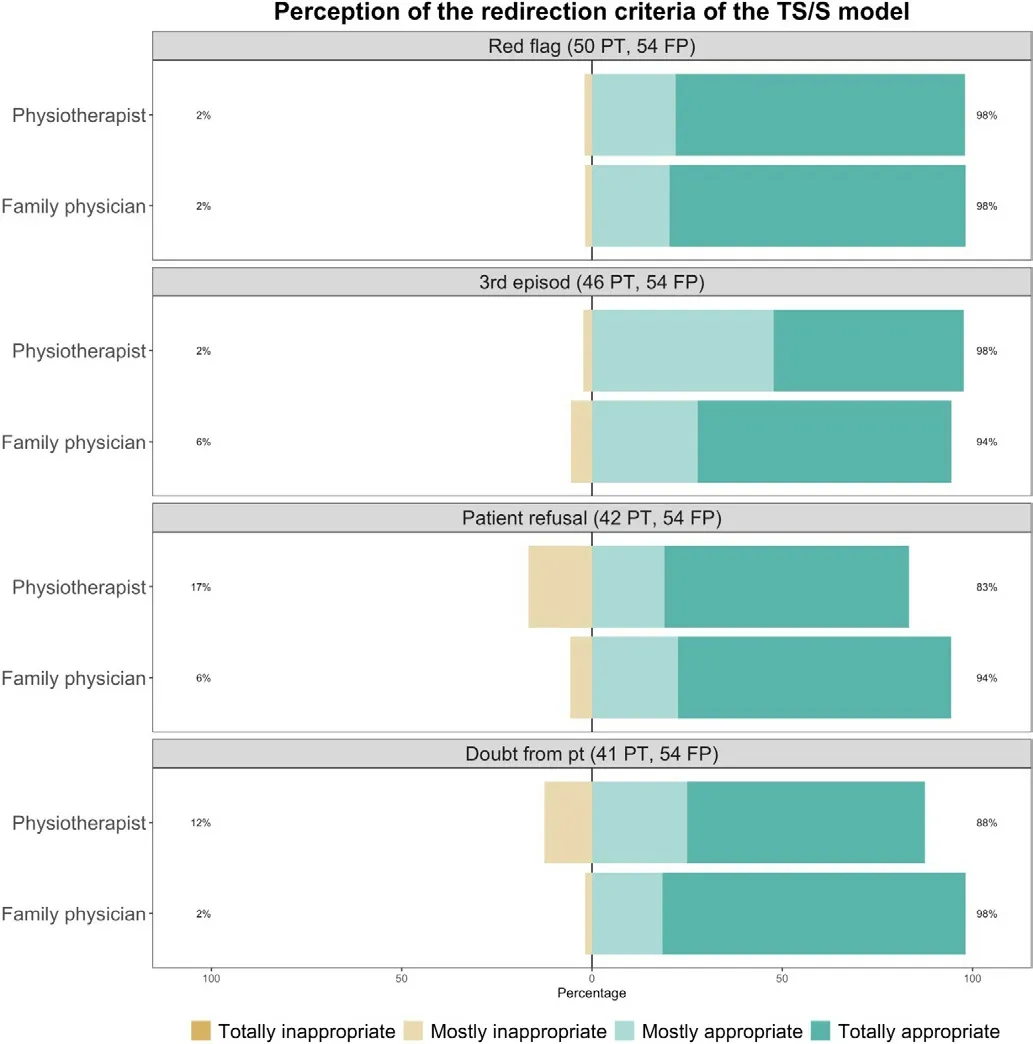
Figure 3 Nearly all physiotherapists and family physicians find the task sharing and shifting model redirection criteria appropriate (n=95-104; year=2021). FP, family physician; PT,physiotherapist; TS/S, task sharing and task shifting.
Perceived PTs competencies in managing acute LBP
Perceived overall competencies of PTs
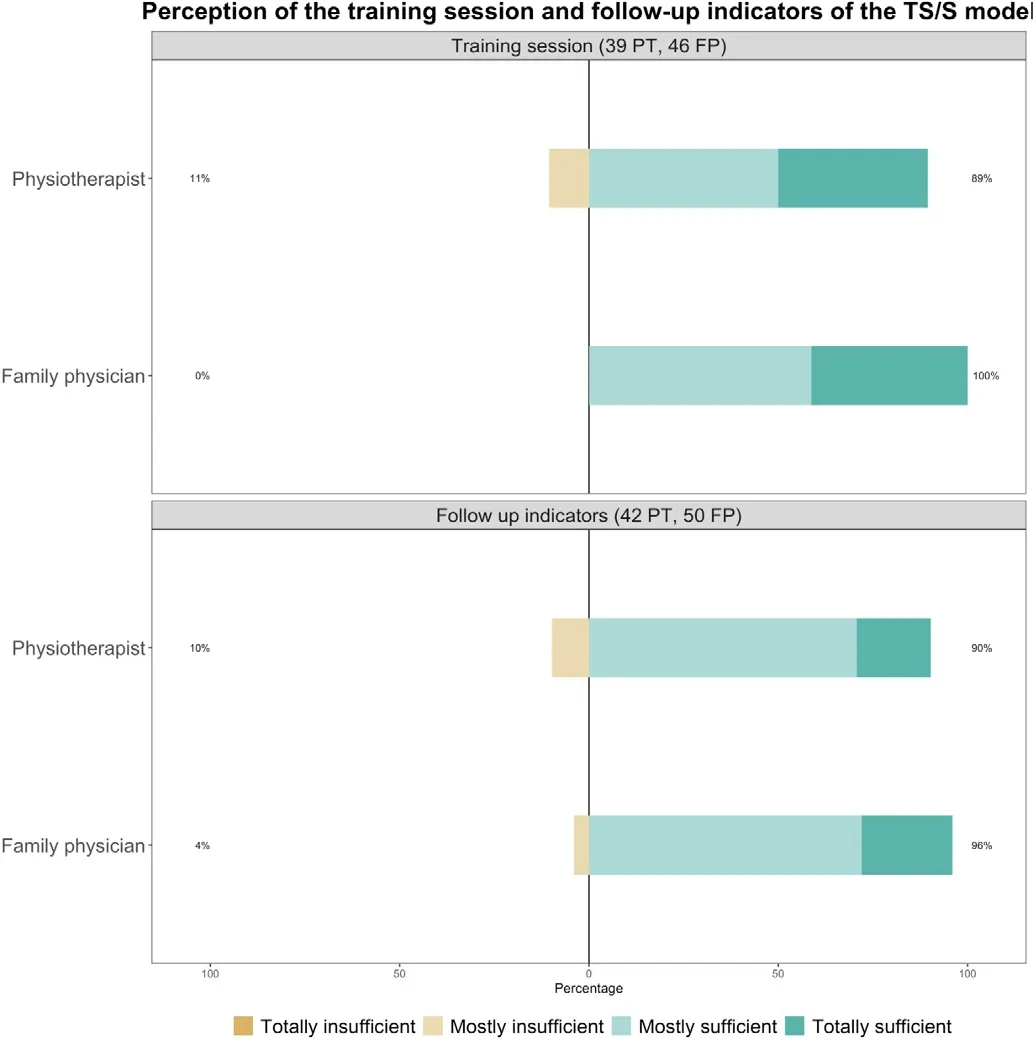
Figure 4 A majority of physiotherapists and family physicians have a positive perception of the follow- up indicators and the interprofessional training session of the task sharing and shifting model (n=85-92; year=2021). FP,family physician; PT, physiotherapist; TS/S, task sharing and task shifting.
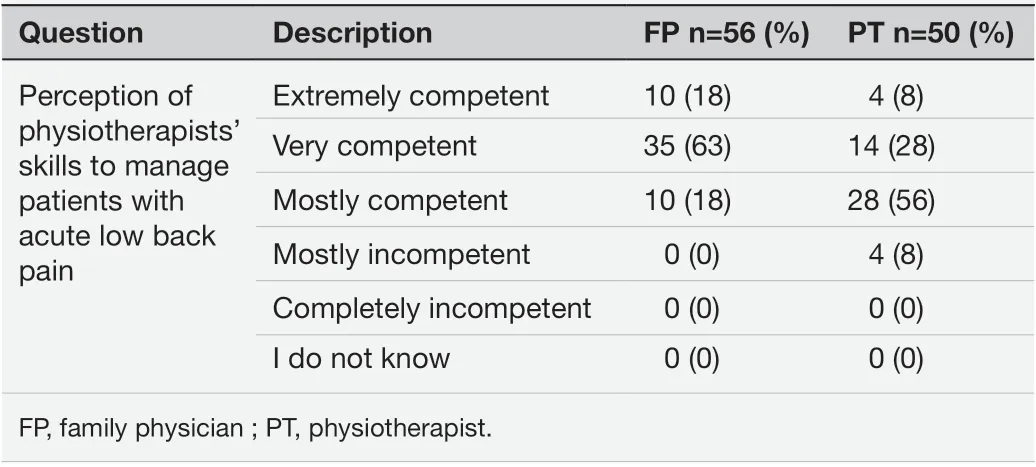
Table 1 Family physicians and physiotherapists have a positive perception of the physiotherapists’ overall competencies to manage acute low back pain (n=106;year=2021)
All FPs had a positive opinion of the PTs’ overall competencies to manage patients with acute LBP. When compared with PTs, a larger proportion of FPs considered PTs as very or extremely competent to manage patients with acute LBP (FPs: n=45, 81% and PTs: n=18, 36%).The majority of PTs considered themselves as mostly competent (table 1).
Perceived competencies of PT to manage acute LBP in their usual role
Regarding tasks which are usually performed by PTs,participants were confident that PTs could provide appropriate care to patient with acute LBP within the new model (figure 5). FPs were either mostly, very or extremely confident that PTs could appropriately identify red and yellow flags, manage patients with active exercises, promote physical activity and provide therapeutic education (figure 5).
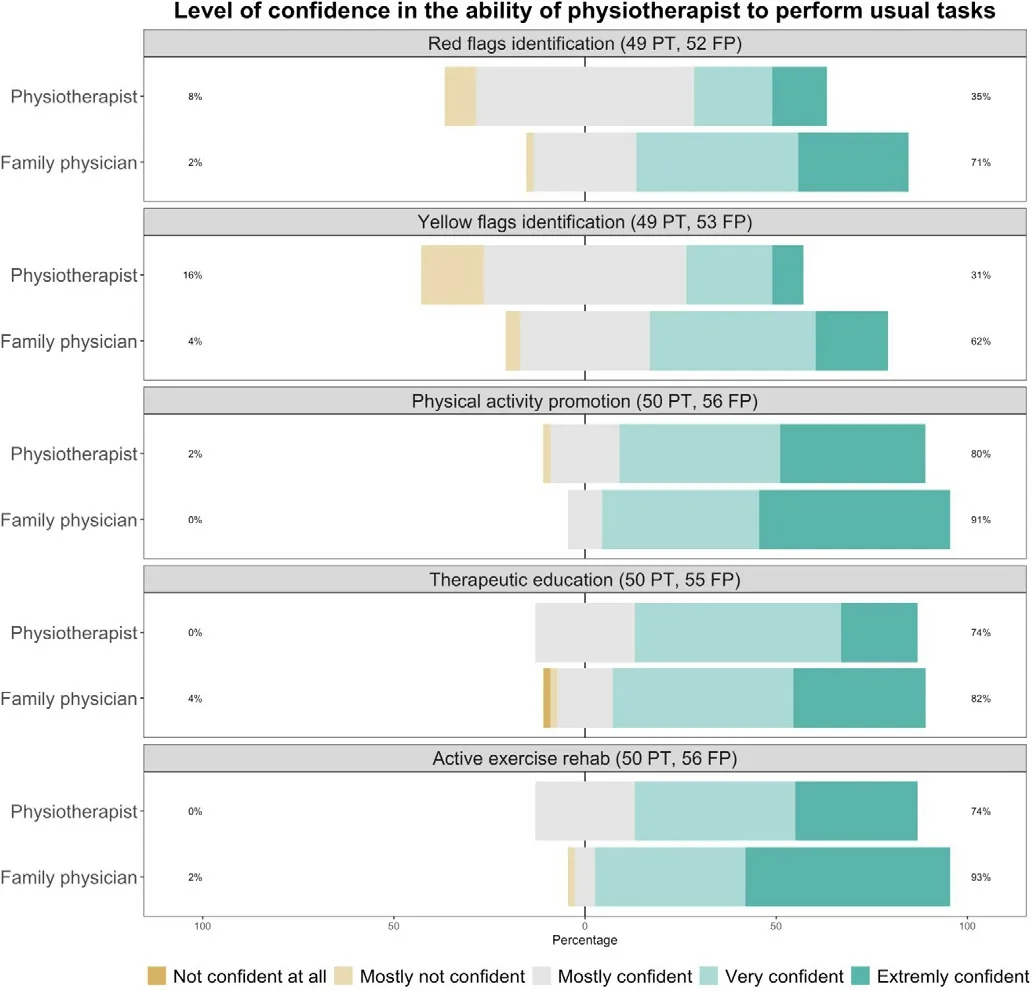
Figure 5 Physiotherapists and family physicians are confident in the physiotherapists’ competencies to perform tasks within their usual scope of practice (n=101-106,year=2021). FP, family physician; PT, physiotherapist.
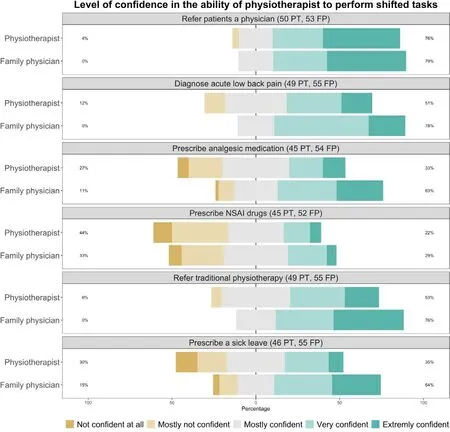
Figure 6 Physiotherapists and family physicians are generally confident regarding the ability of physiotherapists to perform tasks outside of their usual scope of practice excepted for prescribing non- steroidal anti- inflammatory drugs (n=97-104, year=2021). FP, family physician; PT,physiotherapist.
The majority of PTs were also very confident in their ability to perform these tasks which are part of their usual practice (figure 5). However, compared with FPs’ perceptions, a larger proportion of PTs felt mostly unconfident to adequately identify red (FPs: n=1, 2% and PTs: n=4,8%) and yellow flags (FPs: n=2, 4% and PTs: n=8, 16%).Compared with FPs’ perceptions, a lower proportion of PTs were extremely confident that they could manage patients with active exercises (FPs: n=30, 54% and PTs:n=16, 32%) (figure 5).
Perceived competencies of PTs to manage acute LBP in their extended role
Regarding FPs’ usual tasks that are shifted towards the PTs in the new model, all FPs were mostly, very or extremely confident that PTs could appropriately diagnose acute LBP, refer patient to the physician if required and refer patient to conventional physiotherapy when appropriate. The majority of physicians were also mostly,very or extremely confident that PTs could appropriately prescribe analgesic medication such as paracetamol and deliver sick leave certificates for workers (figure 6).
The majority of PTs were also mostly, very of extremely confident in their ability to diagnose acute LBP, refer patient with back pain to a physician if required and refer patient to traditional physiotherapy. A large proportion of PTs also felt confident to prescribe analgesic medication and sick leave. A few of them were not confident(mostly not or not confident at all) to perform these two tasks beyond their usual scope of practice (n=12, 27% for prescription of analgesic medication and n=14, 30% for sick leave prescription) (figure 6).
A minority of PTs and FPs were not confident (mostly not or not confident at all) in the ability of PTs to prescribe oral non- steroidal anti- inflammatory drugs (FPs: n=17,33% and PTs: n=20, 44%).
The confidence level of FPs compared with PTs was higher regarding the ability of PTs to diagnose LBP, to refer patient to traditional physiotherapy, to prescribe analgesic medication or to prescribe sick leave (figure 6).
FPs and PTs’ perception of the implementation of the model
Perception of the implementation and deployment of the model
Most of the participants were totally favourable (FPs:n=17, 30% and PTs: n=20, 41%) or mostly favourable(FPs: n=29, 52% and PTs: n=20, 41%) toward the implementation of this new model of care.
The majority of participants agreed or truly agreed that the implementation of this TS/S model should remain limited to multidisciplinary primary healthcare centres(FPs: n=37, 69% and PTs: n=27, 61%).
Compared with FPs, a larger proportion of PTs agreed that this TS/S model could be extended to other MSD (FPs:n=29, 64% and PTs: n=38, 90%). A larger proportion of PTs thought that it could also be extended beyond musculoskeletal care (FPs: n=13, 32% and PTs: n=21, 51%). Figures are available in online supplemental materials.
Perception of the barriers and facilitators to the implementation
Respondents reported that one of the main perceived barriers to the implementation of the TS/S model was the difficulty for PTs to provide appointments in a timely manner because of already important wait time for physiotherapy in France, especially in rural areas (FPs: n=23,PTs: n=14). Another identified barrier was the lack of time to implement the model (FPs: n=9, PTs: n=6), associated with the additional workload generated by the required administrative procedures (FPs: n=9, PTs: n=7). Some respondents answered that FPs could be reluctant with the delegation of medical tasks such as anti- inflammatory drug and sick leave prescription (FPs: n=6, PTs: n=10).Organisational modifications in the management of consultations were also identified as a barrier (FPs: n=5,PTs: n=7), as well as possible lack of confidence in PTs competencies (FPs: n=7, PTs: n=3).
In terms of perceived facilitators, interprofessional collaboration that already existed between FPs and PTs within multidisciplinary healthcare centres was often cited (FPs: n=21, PTs: n=17). Participants indicated that a high frequency of interprofessional exchanges, regular team meetings and collaborative care can facilitate the implementation of such a model. Utilisation of shared tools as information software and geographical proximity of the team were also identified as positive levers (FPs:n=11, PTs: n=9). Motivation and adhesion from all healthcare professionals to this new form of task management may also strongly support its implementation (FPs: n=7,PTs: n=3), as well as a high confidence level in healthcare practitioner working in collaboration (FPs: n=3,PTs: n=6). The wish to push forward a more autonomous role for PTs in the management of acute LBP was also perceived as a facilitator (FP: n=1, PTs: n=6).
DlSCUSSlON
The main purpose of this study was to investigate the acceptability of a new model of TS/S between PTs and FPs for the management of acute LBP in France. The results of our study highlight that FPs and PTs were generally receptive to the new model of TS/S for the management of patients with acute LBP. A majority of participants had a positive perception of the model. The perceived level of competencies of PTs to manage acute LBP was high. Identified barriers to the implementation of this new model were related to lack of time, additional workload and reluctance with the delegation of medical tasks. Existing interprofessional collaboration was mostly reported as a facilitator to the implementation of the model.
For every question assessing acceptability of this model of care, a majority of the participants considered as appropriate, sufficient or relevant the components of the TS/S model such as the inclusion and redirection criteria, the interprofessional training session and the follow- up indicators. Regarding the objectives of the model, participants did not unanimously agree with the model being able to reduce wait times, FPs workload and visits to emergency services. First, as participants reported important wait times to consult PTs in France to be a barrier, they may consider that the objective of reducing wait times cannot be achieved. In the same way, the perceived inability of this model to solve the issue of excessive professional workload can be explained by the additional administrative work required by the model. Finally, this model is not considered as suitable to reduce further consultations to emergency services according to FPs. Adjustments of the model may be needed to reach these objectives.
The physician- perceived level of competency of PTs to manage acute LBP was generally high in this study. This result can be explained by a high level of existing collaboration between the respondents. FPs and PTs worked collaboratively in teams and may have a good reciprocal knowledge of skills and competencies. The perceived level of competency of PTs is likely to be higher when asking FPs than PTs themselves. PTs may tend to underestimate their competencies when self- evaluating. Previous studies have shown similar result: the perceived skills level was lower when using self- assessments evaluation than when using objective measures of actual competencies,especially in performing highly complex tasks.37–39
Our results show a globally high level of confidence from physicians regarding the ability of the PT to perform tasks within and outside their usual scope of practice.Even so, some PTs did not feel confident with some roles attributed in the model such as identifying red and yellow flags which is considered within their scope of practice.More advanced clinical reasoning, differential diagnosis and triaging processes have only been recently implemented to the entry to practice educational training curriculum of French PTs. PTs who have not recently graduated potentially did not benefit from this training and may not feel skilled enough to manage patients as first- contact primary care practitioners.40Appropriate PTs training should be further explored and implemented to address this lack of confidence as it could be a barrier to the implementation of the model.
In our survey, FPs are more confident than PTs in the PTs ability to accurately diagnose acute LBP. This is an interesting result since diagnosis is symbolically representative of the medical profession in France.41Moreover, all FPs are confident in the ability of PTs to refer patients to the physician if required, and to refer patients to traditional physiotherapy. In France, patients are referred to physiotherapy by a physician. This model gives an opportunity of accessing physiotherapy without being referred by a physician. Our results show that FPs who answered the survey are receptive to the evolution of their gatekeeper positioning regarding medical diagnosis and direct access to other healthcare practitioners.
A larger proportion of FPs are not confident with the autonomous prescription of analgesic medication and sick leave certificate by PTs, compared with other delegated tasks such as medical diagnosis or referring patients to physicians or PTs. With regard to the ability of PTs to prescribe oral non- inflammatory drugs, the level of confidence is lower both for FPs and PTs. Greater caution is warranted with this class of medication because of contraindications and potential adverse events concerning their utilisation.42A careful consideration need to be given in the training of PT regarding this prescription. A change in the perception of professionals’ role is required to improve the acceptability of sick leave prescription by PTs, as this role is usually held by the FP.43
Despite a globally high level of acceptability, most of the participants had not yet implemented this care model. We identified two important potential reasons for this situation. First, the legislative text allowing the model has been published only 1 year prior to this survey, and primary healthcare centres have been heavily involved in the management of the COVID- 19 pandemic during that period. Second, the time and work needed to set up the model and the initial additional work of involved healthcare practitioners with the new model are not easily dealt with.
Working in multidisciplinary healthcare centre is mainly reported as a facilitator to set up the model. This result is consistent with studies showing that introducing interprofessional teams facilitates task reallocation and even leads to mix professionals’ skills and competencies.1344
The development of this model of TS/S could also offer an opportunity to expand direct access and advanced practice physiotherapy in France. Direct access physiotherapy has been defined as the circumstances in which patients can refer themselves to a PT without having to see a physician first, or without being told to refer themselves by another health professional.45International studies showed that the concept of PTs working at first point of contact was strongly supported by the majority of FPs.4647Management of patients suffering from MSDs by direct access PTs have been shown to be efficient and safe and improve access to care in many countries such as Australia, Canada, USA and UK.45Advanced practice physiotherapy care allows PTs to perform tasks that are usually reserved or controlled medical acts in new care settings and often dealing with more complex patients. These may include patient triage,performing a medical diagnosis, ordering medical imagery or prescribing medication. Although not formally define by French authorities as an advanced practice model, this TS/S model conforms to the globally accepted definition within the physiotherapy profession of an advanced practice physiotherapy model of care, according to the World Confederation for Physical Therapy.48
Our results are concordant with other qualitative studies that pointed out the acceptability of PTs as first- contact practitioners by FPs, PTs, nurses, administrative staff and patients in the international context.313249–52One study investigating task shifting in Germany also found a positive perception from the sample of FPs questioned.53In the same way, innovative use of allied health professionals is identified as a strategy to deal with increasing workload for British FPs.54In Denmark, task shifting in general practice was also identified as a way to maintain primary care in the future.55
In the French context, TS/S is a leading and promising health systems strategy to address health workforce shortages, transform healthcare delivery and improve health outcomes.17TS/S gives the opportunity to redistribute responsibilities among the team and change the conventional hierarchies between health providers.17Studies underlined the need to bring about a cultural and societal change, as the FP is often considered as the only first contact practitioner. This process for such a change in perception is long, and requires a collaborative work between health professionals, patients and authorities.
The finding of our study can help to change primary care research and practice in the future by highlighting the need to reinforce coordination and collaboration between primary care professionals in order to achieve a good mutual knowledge of each professionals’ role and competencies and to improve the confidence level between them. A high level of confidence is required to implement innovative healthcare pathways integrating TS/S. The implementation of such a model could be a leading and promising health system strategy to address health workforce shortages, transform healthcare delivery and improve health outcomes for patients.
This is the first study to investigate this new model of TS/S acceptability between PTs and FPs in the French context. The next step is the implementation of this new model in primary healthcare centres, and the assessment of its effect on patient access to healthcare, health outcomes, resources use, patient satisfaction and professional practice.17A randomised controlled trial is being conducted in France by our team.
These findings are based on experiences and perceptions of a small and specific sample of participants. They cannot be generalised and have to be interpreted with caution. The respondent population included PTs and FPs that already worked in a collaborative environment. Their previous experience may have influenced their perception of the PTs’skills and competencies. Moreover, a majority of the respondents worked in rural area. That can influence our findings due to the fact that access to care in French rural area is more limited. Overload of FPs and PTs, which was identified as a barrier to the implementation of the new model, may be over- represented in these areas as well. Other barriers related to the modalities of implementation of the model could be identified in the future.
The response rate of this study is not calculable since we did not know exactly how many PTs and FPs worked in the healthcare centres that received our online survey.The response rate calculated per healthcare centre is however relatively high (85%). We noticed a large proportion of incomplete responses that can be imputed to the length of the questionnaire. Responses from all participants who either fully or partially completed the survey were considered for analysis.2956Withdrawals are equally divided up throughout the questionnaire, and results of the survey did not differ when considering only the complete answers, or incomplete and complete answers.That emphasises the robustness of our results.
Because of the exploratory design of our study, we did not rely on inferential statistical analysis to discuss the presence or absence of significant differences. We used descriptive statistics and graphical representation to discuss whether or not a pattern emerges.2957–59
The use of a survey as an original research methodology enable us to collect quantitative data about the acceptability of the TS/S model. However, this survey could have been combined with qualitative data collection through interviews to form a mixed- method research.Mixed- method research could provide more detailed answers, especially to investigate barriers and facilitators to the implementation of the model.6061
CONCLUSlON
Based on a limited sample, there is a positive perception and high acceptability of the TS/S model. The perceived level of competencies of PT to manage acute LBP was generally high, especially according to FPs. TS/S between FPs and PTs is a promising strategy to address primary healthcare workforce shortages for the management of MSDs. Further studies are needed to evaluate its precise effect on access to healthcare, health outcomes, resources use and healthcare and societal costs.
Author affiliations
1Themas Team, TIMC- IMAG Laboratory, UMR CNRS- UGA, Grenoble, France
2Department of Physiotherapy, University Grenoble- Alpes, Grenoble, Auvergne-Rhône- Alpes, France
3Maisonneuve- Rosemont Hospital Research Centre, University of Montreal Affiliated Research Center, Montreal, Québec, Canada
4School of Rehabilitation, University of Montreal, Faculty of Medicine, Montreal,Québec, Canada
5Department of General Medicine, Faculty of Medicine, University Grenoble- Alpes,Grenoble, France
AcknowledgementsThis study could not have been completed without the precious collaboration of both associations, Femas AURA and URPS- MK ARA, as well as all the participants who completed this survey.
ContributorsConcept/idea/research design: AK, NP, FD, PG. Writing: AK, FD, NP.Data collection: AK. Data analyses: AK. Project management: FD, NP. Providing institutional liaisons: NP. Consultation (including review of manuscript before submitting): AK, NP, FD, PG. Guarantor: AK.
FundingThis project was funded to AK by the “Union Régionale des Professionnels de Santé Masseur- Kinésithérapeutes” of the Auvergne- Rhône- Alpes region in France, as part of a doctoral grant.
Competing interestsNone declared.
Patient consent for publicationNot applicable.
Ethics approvalThis study was conducted in conformity with the methodological reference of the University Grenoble- Alpes and in accordance with the French General Regulation for Data Protection. Ethics approval number: Not applicable.Participants gave informed consent to participate in the study before taking part.
Provenance and peer reviewNot commissioned; externally peer reviewed.
Data availability statementAll data relevant to the study are included in the article or uploaded as supplementary information.
Supplemental materialThis content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer- reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines,terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Open accessThis is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY- NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non- commercially,and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non- commercial. See: http://creativecommons.org/licenses/by-nc/4.0/.
ORClD iD
Amélie Kechichian http://orcid.org/0000-0002-1184-6568
杂志排行
Family Medicine and Community Health的其它文章
- Development and validation of the scale for measuring biopsychosocial approach of family physicians to their patients
- Transitions in health service use among women with poor mental health: a 7- year follow- up
- Putting health workers at the centre of health system investments in COVID- 19 and beyond
- COVID- 19 vaccine hesitancy and related factors among primary healthcare workers in a district of Istanbul: a crosssectional study from Turkey
- Patient experience of residents with restricted primary care access during the COVID- 19 pandemic
- Side effects and acceptability measures for thermal ablation as a treatment for cervical precancer in low- income and middle- income countries: a systematic review and meta- synthesis
