多囊卵巢综合征患者血清炎症因子及性激素水平的变化及二甲地黄汤的作用
2022-07-15林群徐丽霞陈青华石明晴
林群 徐丽霞 陈青华 石明晴

[摘要] 目的 探討多囊卵巢综合征(PCOS)患者血清炎症因子及性激素水平的变化及二甲地黄汤的作用。方法 选取2018年1月~2020年6月浙江省丽水市中医院妇产科门诊治疗的PCOS患者40例作为试验组。试验组患者予以二甲地黄汤治疗,1剂/d,连用3个月经周期。观察试验组治疗前后血清炎症因子[超敏C反应蛋白(hs-CRP)和肿瘤坏死因子-α(TNF-α)]及性激素[促卵泡生成素(FSH)、雌激素(E2)和促黄体生成素(LH)]水平的变化。另选择同期笔者医院体检中心的健康体检者30例作为对照组,对照组仅在纳入时测定血清hs-CRP、TNF-α、LH、FSH和E2水平。 结果 试验组血清hs-CRP和TNF-α水平显著高于对照组,差异有统计学意义(P<0.01);试验组血清LH水平明显高于对照组,血清FSH和E2水平明显低于对照组,差异有统计学意义(P<0.05)。治疗3个月经周期后,试验组血清hs-CRP和TNF-α水平较治疗前明显下降,差异有统计学意义(P<0.01);试验组血清LH水平较前明显下降,血清FSH和E2水平较前明显上升,差异有统计学意义(P<0.05)。 结论 PCOS患者存在血清炎症因子水平异常和性激素紊乱。二甲地黄汤治疗PCOS患者不仅可降低血清炎症因子水平,控制炎症反应,而且可纠正内分泌紊乱,调节性激素水平。
[关键词] 多囊卵巢综合征;炎症因子;性激素;二甲地黄汤
[中图分类号] R711.7 [文献标识码] B [文章编号] 1673-9701(2022)16-0124-04
Changes of serum inflammatory factors and sex hormones in patients with polycystic ovary syndrome and the effect of dijiadihuang decoction
LIN Qun1 XU Lixia1 CHEN Qinghua1 SHI Mingqing2
1. Department of Laboratory, Lishui Hospital of Traditional Chinese Medicine in Zhejiang Province,Lishui 323000,China;2.Department of Obstetrics and Gynecology, Lishui Hospital of Traditional Chinese Medicine in Zhejiang Province,Lishui 323000,China
[Abstract] Objective To explore the changes of serum inflammatory factors and sex hormone levels in patients with polycystic ovary syndrome(PCOS) and the effect of Dijiadihuang Decoction. Methods A total of 40 PCOS patients treated in the Obstetrics and Gynecology Department of Lishui Traditional Chinese Medicine Hospital from January 2018 to June 2020 were selected as the experimental group. The patients in experimental group were treated with Erjiadihuang Decoction, 1 dose/d, for 3 consecutive menstrual cycles. The changes of serum inflammatory factors [hypersensitive C-reactive protein (hs-CRP) and tumor necrosis factor-α (TNF-α)] and sex hormones [follicle stimulating hormone (FSH), estrogen (E2) and luteinizing hormone [LH] in experimental group before and after treatment] levels. In the same period, 30 healthy subjects from the physical examination center of our hospital were selected as the control group, the serum hs-CRP, TNF-α, LH, FSH and E2 levels were examined including in the study. Results The serum hs-CRP and TNF-α levels of patients in experimental group were significantly higher than those in control group, and the difference was statistically significant between two groups(P<0.01);the serum LH level of patients in experimental group was significantly higher than that in control group, and the serum FSH and E2 levels of patients in were significantly lower than that in control group, the difference was statistically significant between two groups(P<0.05). After treatment for 3 menstrual cycles, the levels of serum hs-CRP and TNF-α in experimental group were significantly lower than before treatment, the difference was statistically significant before and after treatment(P<0.01); the levels of serum LH in experimental group were significantly lower than before, and the levels of serum FSH and E2 were significantly higher than before, and the difference was statistically significant before and after treatment(P<0.05). Conslusion Patients with PCOS have abnormal levels of serum inflammatory factors and disorders of sex hormones. Erjiadihuang Decoction in the treatment of PCOS patients can not only reduce the level of serum inflammatory factors and control the inflammatory response, but also correct endocrine disorders and regulate the level of sex hormones.
[Key words] Polycystic ovary syndrome; Inflammatory factors; Sex hormones; Dimethyl Dihuang Decoction
多囊卵巢综合征(polycystic ovarian syndrome,PCOS)是妇产科常见病,育龄妇女多发,发病率占育龄妇女的6%~13%,主要表现为内分泌和代谢功能异常,可引起高雄激素血症、月经紊乱,导致不孕[1,2]。PCOS的发病机制至今国内外尚未研究清楚,近年来研究发现慢性炎症反应及性激素紊乱引起的胰岛素抵抗在PCOS发病中起着极其重要的作用[3,4]。近年来研究发现中医中药在PCOS的治疗上发现具有独特之处,可通过改善内分泌紊乱,促进卵泡发育,治疗PCOS效果较好,但有关中医中药对PCOS患者血清炎症因子及性激素水平的影响国内外报道较少[5,6]。本研究分析PCOS患者血清炎症因子及性激素水平的变化及二甲地黄汤的干预作用,现报道如下。
1 资料与方法
1.1 一般资料
选取2018年1月~2020年6月浙江省丽水市中医院妇产科门诊治疗的PCOS患者40例作为试验组。纳入标准[7]:①符合2012年制定的PCOS的诊断标准[8];②育龄妇女。排除标准[9]:①合并其他原因引起不孕者;②合并其他生殖系统疾病者。试验组年龄21~40岁,平均(28.81±4.36)岁;体重41~82 kg,平均(51.22±4.81)kg。另选择同期浙江省丽水市中医院体检中心的健康体检者30例作为对照组,年龄23~38岁,平均(28.45±4.51)岁;体重42~80 kg,平均(51.92±3.78)kg。两组年龄和体重等比较,差异无统计学意义(P>0.05),具有可比性。本方案通过笔者医院医学伦理委员会批准,纳入患者均签署知情同意书。
1.2 方法
试验组予以二甲地黄汤治疗,药物组成:炙龟版和炙鳖甲各20 g,生地黄、山药、山茱萸、麦冬、茯苓、丹皮和莲子心各6 g,1剂/d,水煎取汁约200 ml分早晚2次口服,连用3个月经周期。观察试验组治疗前后血清炎症因子[超敏C-反应蛋白(hypersensitive3 C-reactive protein, hs-CRP)和肿瘤坏死因子-α(tumor necrosis factor-α, TNF-α)]及性激素[促卵泡生成素(follicular hormone,FSH)、雌激素(estrogen 2,E2)和促黄体生成素(luteinizing hormone,LH)]水平的变化,对照组仅在纳入时测定血清指标1次。
1.3 观察指标
1.3.1 标本采集 抽取空腹静脉血3~5 ml,3000 r/min离心10 min分离出血清,置于-70℃的冰箱内保存。
1.3.2 血清炎症因子及性激素水平测定 采用乳胶增强免疫散射比浊法测定血清hs-CRP水平,试剂盒由深圳迈瑞生物医疗电子有限公司提供;采用酶联免疫吸附法测定血清TNF-α水平,试剂盒由北京中杉金桥生物技术有限公司提供;采用电化学发光测定血清FSH、E2和LH水平,试剂盒由罗氏诊断产品有限公司提供。
1.4 统计学方法
采用SPSS 22.0统计学软件进行数据分析,计量资料以均数±标准差(x±s)表示,采用t检验。计数资料以[n(%)]表示,采用χ2检验,P<0.05为差异有统计学意义。
2 结果
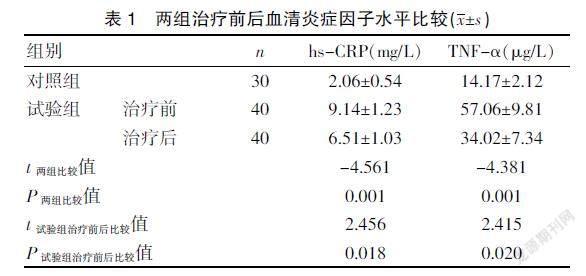
2.1 两组治疗前后血清炎症因子水平比较
试验组血清hs-CRP和TNF-α水平显著高于对照组(P<0.01),治疗3个月经周期后,试验组血清hs-CRP和TNF-α水平较治疗前明显下降(P<0.01)。见表1。
2.2 两组治疗前后血清性激素水平比较
试验组血清LH水平明显高于对照组,血清FSH和E2水平明显低于对照组(P<0.05);治疗3个月经周期后,试验组血清LH水平较前明显下降,血清FSH和E2水平较前明显上升(P<0.05)。见表2。
3 讨论
PCOS是临床常见的内分泌和代谢紊乱的综合征,以育龄期女性多见,患者出现内分泌紊乱和代谢异常的情况,临床表现为卵泡发育异常和排卵功能丧失,患者体内的雄性激素异常升高,出现月经失调紊乱、闭经和不孕等情况,对患者的生活质量影响较大[10]。随着社會环境的不断变化,PCOS的发病率近年来有逐年上升的趋势,导致育龄期妇女月经紊乱和不孕,不仅影响患者身心健康,而且给其家庭、社会和婚姻等带来极大的伤害,需积极干预治疗[11]。
PCOS的病理机制较复杂,其中炎症反应异常及下丘脑-垂体-卵巢轴功能紊乱障碍是其主要影响因素[12,13]。研究发现PCOS患者存在慢性亚临床炎症反应状态,炎症可能导致下丘脑-垂体-性腺轴功能发生障碍及卵泡发育异常的整个过程,分泌多种炎症相关细胞因子及免疫调节分子,参与调节卵巢多种功能,如卵泡形成、排卵及黄体形成及撤退过程[14~16]。本研究显示,试验组血清hs-CRP和TNF-α水平显著高于对照组。提示PCOS患者存在血清炎症因子水平异常升高,体内存在慢性亚临床炎症反应状态。研究亦发现PCOS患者存在下丘脑-垂体-卵巢轴功能紊乱,使得下丘脑促性腺激素释放激素分泌脉冲频率增加,增加垂体对促性腺激素释放激素的敏感度,使垂体分泌LH的频率及幅度增加,LH分泌增加会降低FSH和E2的合成和分泌[17~19]。本研究发现血清LH水平明显高于对照组,血清FSH和E2水平明显低于对照组,提示PCOS患者存在血清性激素紊乱,表现为血清LH水平明显上升,血清FSH和E2水平明显下降。
PCOS是一个影响内分泌、代谢、生殖、性腺等多系统的复杂疾病,中医学上无此病名,结合临床实践认为其主要病理病机多为肾气不足、冲任失资、脏腑功能失常,中医对本病的治疗是站在整体调理的高度,以肾虚为立足点,兼健脾化痰、祛湿理气、化瘀等[20~22]。二甲地黄汤方中炙龟版、炙鳖甲滋阴潜阳散结,生地黄壮水滋阴;山药补肾健脾;山茱萸补益肝肾,益精潜阳;茯苓益气健脾利水;丹皮清热凉血;麦冬清心润肺;莲子心清心安神。本研究显示,治疗3个月经周期后,试验组患者血清hs-CRP和TNF-α水平较前明显下降,且试验组血清LH水平较前明显下降,血清FSH和E2水平较前明显上升。提示二甲地黄汤治疗PCOS患者不仅可降低血清炎症因子水平,控制炎症反应,而且可纠正内分泌紊乱,调节性激素水平。
综上所述,PCOS患者存在血清炎症因子水平异常和性激素紊乱。二甲地黄汤治疗PCOS患者不仅可降低血清炎症因子水平,控制炎症反应,而且可纠正内分泌紊乱,调节性激素水平。
[参考文献]
[1] Korkmazg GG,Altinoglu E,Civelek S,et al. The association of oxidative stress markers with conventional risk factors in the metabolic syndrome[J].Metabolism,2018,62(6):828-835.
[2] Huang G, Coviello A. Clinical update on screening diagnosis and management of metabolic disorders and cardiovascular risk factors associated with polycystic ovary syndrome[J].Curr Opin Endocrinol Diabetes Obes,2018,19(6):512-519.
[3] Cutler DA,Pride SM,Cheung AP. Low intakes of dietary fiber and magnesium are associated with insulin resistance and hyperandrogenism in polycystic ovary syndrome: A cohort study[J].Food Sci Nutr,2019,7(4):1426-1437.
[4] 党菲. 控制胰岛素抵抗改善多囊卵巢综合征患者性激素与血脂代谢的效果[J].中国妇幼保健,2018,33(19):4388-4392.
[5] 李蔚,郝霞,丁慧. 影响多囊卵巢综合征不孕症患者受孕结局的中医体质、中医证候相关因素分析[J].中华中医药学刊,2020,31(5):248-251.
[6] 杨艺娇,杨玲,倪晓容. 多囊卵巢综合征中医证型与体质分布及血清炎症因子的相关性研究[J].河北中医,2020, 42(10):1465-1470.
[7] Ozelci R, Dilbaz S, Dilbaz B, et al. Gonadotropin releasing hormone antagonist use in controlled ovarian stimulation and intrauterine insemination cycles in women with polycystic ovary syndrome[J].Taiwan J Obstet Gynecol,2019, 58(2):234-238.
[8] 中华医学会妇产科学分会内分泌学组及指南专家组. 多囊卵巢综合征中国诊疗指南[J].中华妇产科杂志,2018,53(1): 2-6.
[9] Patel R,Shah G. Evaluation of ovarian and metabolic effects of GnRH modulators in two rat models of polycystic ovary syndrome[J].Mol Reprod Dev,2018,85(10):778-789.
[10] Kalhori Z,Mehranjani MS,Azadbakht M,et al. L-Carnitine im-proves endocrine function and folliculogenesis by reducing inflammation,polycystic ovaryoxidative stress and apoptosis in mice following induction of syndrome[J].Reprod Fertil Dev,2019,31(2):282-293.
[11] Escobar-Morreale HF, Luque-Ram rez M, Gonz lez F. Circulating inflammatory markers in polycystic ovary syndrome: A systematic review and metaanalysis[J].Fertil Steril,2011,95(3): 1048-1058.
[12] 谈美华,章丽盈.多囊卵巢综合征所致不孕患者性激素及代谢指标检测分析[J].中国妇幼保健,2020,35(2):302-304.
[13] Deepika ML,Reddy KR,Yashwanth A,et al. TNF -α haplotype association with polycystic ovary syndrome-a South Indian study[J].J Assist Reprod Genet,2018,30(11):1493-1503.
[14] 刘震忠.雷洛昔芬联合坤泰胶囊治疗对多囊卵巢综合征不孕妇女性激素水平及妊娠结局的影响[J].中国妇幼保健,2018,33(12):2774-2777.
[15] Yilmaz N,Inal HA,Gorkem U,et al. Follicular fluid total antioxidant capacity levels in PCOS[J].J Obstet Gynaecol,2016,36(5): 654-655.
[16] 师帅,刘鸿.达英-35与优思明对肥胖型多囊卵巢综合征患者脂代谢 性激素水平及妊娠结局的影响[J].中国妇幼保健,2018,33(10):2217-2221.
[17] Kim CH, Ahn JW, You RM, et al. Pioglitazone treatment decreases follicular fluid levels of tumor necrosis factor-αand interleukin-6 inpatients with polycystic ovary syndrome[J].Clin Exp Reprod Med,2011,38(2):98-102.
[18] 陳琼娣.多囊卵巢综合征患者血清AMH与性激素水平的相关性研究[J].云南医药,2021,42(1):47-48.
[19] Sakumoto R,Vermehren M,Kenngott RA,et al. Localization of gene and protein expressions of tumor necrosis factor-{alpha} and tumor necrosis factor receptor types I and II in the bovine corpus luteum during the estrous cycle[J].J Anim Sci,2011,89(10):3040-3047.
[20] 周贵凤,林色奇.从多囊卵巢综合征的古代病名探究中医病因病机[J].江西中医药大学学报,2021,33(1):5-7.
[21] 冯玉,高月平.江苏地区多囊卵巢综合征中医证型分布规律及与饮食失宜相关性的临床研究[J].中国中药杂志,2014,39(10):1937-1940.
[22] 吴绪祥.中药联合克罗米芬治疗多囊卵巢综合征不孕症临床观察[J].湖北中医学院学报,2010,12(2):15-16.
(收稿日期:2021-03-19)
