Review on hepatitis B virus precore/core promoter mutations and their correlation with genotypes and liver disease severity
2022-07-02RajeshKumar
Rajesh Kumar
Rajesh Kumar, Department of School Education, Haryana Government, Panchkula 134109, Haryana, India
Abstract Of 350 million people worldwide are chronically infected with hepatitis B virus (HBV) and are at risk of developing cirrhosis and hepatocellular carcinoma (HCC) later in life. HBV is the most diverse DNA virus, and its genome is composed of four open reading frames: Presurface antigen/surface antigen gene (preS/S), precore/core gene (preC/C), polymerase gene (P), and the X gene (X). HBV produces quasispecies naturally or in response to antiviral agents because of the absence of proofreading activity amid reverse transcription and a high replication rate. The virus has 10 genotypes (A to J) with different geographical distributions. There are various HBV mutations in the HBV genome, including preC/C mutations, preS/S mutations, P gene mutations, and X gene mutations. The core promoter region plays a vital part in the replication, morphogenesis and pathogenesis of the virus. The precore region also plays a crucial role in viral replication. Both core promoter and precore mutations rescue the virus from host immune surveillance and result in the formation of mutated strains that may have altered pathogenicity. preC/C mutations are associated with liver disease progression. Precore mutations stop hepatitis B e antigen (HBeAg) production and basal core promoter mutations downregulate HBeAg production. Mutations in the basal core promoter are also associated with increased HBV replication and an increased incidence of advanced liver diseases such as cirrhosis and HCC. The emergence of antiviral-resistant mutations is the main reason for treatment failure. This review focuses mainly on preC/C promoter mutations and their correlation with genotypes and liver disease severity. Thorough perception and knowledge of HBV genetic variety and mutants could be vital to discover techniques for the prognosis and control of HBV infection.
Key Words: Hepatitis B virus; Hepatitis B virus e antigen; Hepatocellular carcinoma; Basal core promoter; Core promoter region; Precore region; Fulminant hepatitis; Acute hepatitis
INTRODUCTION
The hepatitis B virus (HBV) epidemic exists as a leading public health issue worldwide even with the accessibility of effective vaccines[1,2]. Worldwide, almost 350 million people are chronically infected with HBV and it accounts for more than 1 million deaths as a result of progressive liver diseases like cirrhosis and hepatocellular carcinoma (HCC)[3]. Persistent HBV infection leads to various clinical manifestations like inactive carrier state, chronic hepatitis, cirrhosis, and HCC[3].
HBV is an enveloped virus of theHepadnaviridaefamily. The genome of this virus has partially double-stranded circular DNA of around 3200 nucleotides. There are four overlapping open reading frames (ORFs) that make up the polymerase (P), core (C), surface antigen (S), and X protein[4-7].
Based on an intergroup divergence of more than 7.5% in its complete genome, this virus can be divided into nine genotypes (A to I)[8,9], and based on nucleotide divergence of more than 4%, these genotypes are further subdivided into subgenotypes[8,9]. A to H have long been established as individual genotypes. Two new genotypes (I and J) were suggested more recently[10,11]. Evidence supports that HBV genotypes play a significant role in deciding HBV disease severity. Several studies have revealed that genotype A evolves more rapidly than genotype D, which causes challenges for treatment[12]. In addition, genotype-C-infected patients have more advanced liver disease than patients infected with genotype B[13]. Genotype-F-infected patients have higher mortality than patients infected with genotype A or D[14]. In an Indian study, genotype D was related to more advanced liver disease than other genotypes were[15]. In a study from the United States, genotype D acted as an independent risk factor for fulminant hepatitis (FH)[16]. In another study, genotype-F-infected patients had a higher rate of liver-related death than genotype-D-infected patients had[17]. Generally, patients infected with genotype C and D are more associated with liver disease severity (HCC) than patients infected with genotype A and B[18].
Replication in HBV occurs by reverse transcription of RNA intermediates. This virus has a high error rate during reverse transcription, leading to various mutations in the HBV genome[19]. These mutations have clinical and epidemiological significance. Various mutations (preC/C and preS/S deletion) are related to advanced liver disease and the possibility of HCC[19]. The basal core promoter (BCP) and precore mutations are frequently appearing natural variants of HBV. In this review, we discuss preC/C mutations and their correlation with genotypes and severity of liver disease.
HBV CORE PROMOTER MUTATIONS AND RELATEDNESS WITH GENOTYPE AND ADVAN-CEMENT OF LIVER DISEASE
Core promoter region
The CP region (nt 1575-1849) of the virus genome plays a vital part in the replication and morphogenesis of the virus[20]. CP region controls transcriptional initiation for the synthesis of the precore mRNA and pregenomic RNA (pgRNA). The CP region includes BCP (nt 1743-1849) and upper regulatory region (URR, nt 1613-1742). BCP has a crucial role in the replication of virus by promoting the formation of precore and pgRNAs[20]. The URR contains positive and negative regulatory elements that regulate activity of the promoter[20]. Hence, core promoter mutations may have an impact on virus gene expression and/or replication, and contribute to viral pathogenesis. Now, we discuss various core promoter mutations and their correlation with genotypes and the advancement of liver disease.
A1762T/G1764A double mutation
A1762T/G1764A double mutation is the most commonly observed core promoter mutation and it is associated with hepatitis B e antigen (HBeAg) negativity and one of the causes of advanced liver disease. There are various observations associated with this double mutation described below.
Kimet al[21] observed the role played by the precore mutation G1896A and the BCP double mutation A1762T/G1764A in the progression of HBV-related liver diseases. BCP double mutation A1762T/G1764A may prevent the formation of HBeAg by inserting a premature stop codon into the concerned ORF or may enhance the pgRNA transcription by evacuating of the nuclear-receptor-binding motif and led to the feeble immune response that causes HCC[22,23]. From transfection studies, it was observed that HBeAg negativity caused by BCP double mutation A1762T/G1764A was linked with serious liver disease[24].
BCP mutant may increase the host immune response towards HBV-infected hepatocytes by reducing circulating HBeAg, leading to apoptosis and regeneration of hepatocytes, which contribute to liver injury[22,25]. In anin vivostudy, A1762T/G1764A mutant was related to cytoplasmic positioning of intracellular HB core antigen, which were strongly linked with active necroinflammation of hepatocytes[26]. The A1762T/G1764A double mutation was found to influence the amino acid sequence of X gene of HBV, upregulating S-phase kinase-associated protein 2 and downregulating its target, cyclin kinase inhibitor p21. The combined action of the above-mentioned events may lead to inhibition of precore mRNA and an increase in pgRNA transcription, followed by increased viral replication, which may finally lead to HCC[27].
It was found that A1762T/G1764A mutation usually appeared almost 10 years before the identification of HCC and could be an early episode in hepatocarcinogenesis[28]. The BCP double mutation A1762T/G1764A was found to be related to more progression of HCC[29] independently of HBV genotype[24,30] and viral load[30,31]. The mutations A1762T, G1764A, and A1762T/G1764A played a vital part in the progression of chronic HBV infection to HCC[25,32,33]. In a study from East Kalimantan, Indonesia, BCP mutations, mainly the double mutation A1762T/G1764A and T1753V, were linked with the risk of advanced liver disease (ALD)[34].
HCC patients with genotype C had more chance of carrying the A1762T/G1764A double mutation than those with genotype B[35]. In China, A1762T/G1764A mutation is a familiar mutation and found generally in HBeAg-negative chronic hepatitis B patients with genotype C and may be related to the progression of chronic HBV infection[36]. In a study on HBV-infected children in China, the frequency of BCP mutations in genotype C samples was significantly higher than that of genotype B samples[37]. From a Taiwanese study, genotype C and A1762T/G1764A mutations may be the cause of liver cirrhosis and could act as molecular markers for the diagnosis of the clinical symptoms of chronic HBV disease[38]. From a North Indian study, genotype-D-infected patients had more advanced liver disease and higher frequency of BCP mutations A1762T/G1764A than patients infected with genotype A had[39].
A1762T/G1764A mutation also acted as a significant viral marker for cirrhosis development[40]. From a study of chronic HBV infection, it was observed that A1762T/G1764A mutation was an independent factor for advancement to cirrhosis instead of HCC[41]. Table 1 showed various qualitative and quantitative factors associated with HBV-related HCC.
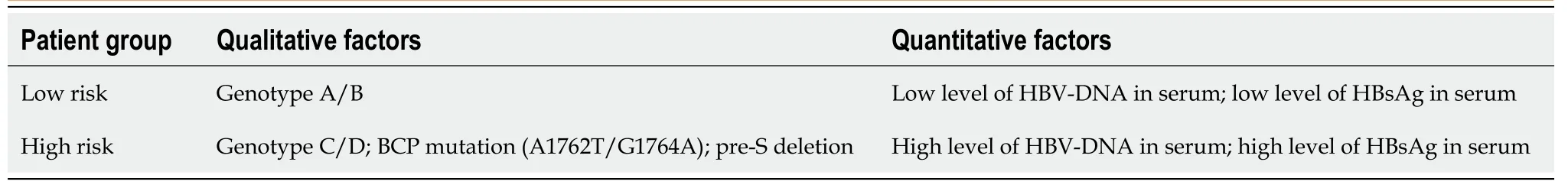
Table 1 Qualitative and quantitative factors and the level of each factor associated with hepatitis B virus-related hepatocellular carcinoma
1753 mutation
1753V (V represents C/A/G) is one of core promoter mutations that is associated with advanced liver diseases like cirrhosis and HCC. In a study from East Kalimantan, Indonesia, BCP mutations, mainly the double mutation A1762T/G1764A and T1753V, were linked with the risk of ALD[34]. BCP T1753V mutation was associated with an increased risk of HCC[28]. The T1753C mutation was treated as one of the hot spot mutations of the protein-X encoding gene[28] and was shown to increase the transactivation and antiproliferation activity of protein X in HBV genotype D and led to carcinogenesis[42]. In a study on HBeAg-positive genotype C1 carriers, 1753 mutation was detected as a prognostic factor for HCC[28].
In a study from China, T1753V mutation in combination with BCP A1762T/G1764A double mutation was assumed to be related to HCC progression, notably in HBV/C1-infected patients[43]. In a Mongolian study, patients infected with HBV/D, C1752, and/or T1753V mutation were found to be related to HCC[42]. In a study from Southern Guangxi, China, BCP mutations were associated with HCC risk and the add-on impacts of A1762T/G1764A double mutations and T1753V mutations along with dietary aflatoxin B1 exposure for HCC risk[44]. In a study from Chiba, Japan, preC mutation (A1896) and CP mutations (T1753V and 1754) were observed more often in FH patients than in acute self-limited hepatitis patients[45]. In a study from Taiwan, the frequency of genotype C and frequency of various mutations (A1762T/ G1764A, T1753C, T1766/A1768, and A1896) increased and the frequency of various mutations (T/G1752, T1773, G1799, and C1858) declined with advancing liver diseases[38].
T to C/A mutation at nt 1753 in BCP and G to A mutation at nt 1899 in the precore region were more frequently found in liver cirrhosis patients than in the other clinical states[46]. 1653T/1753C mutation may be observed as a marker for hepatic failure[47].
1757 mutation
1757 mutation is one of the core promoter mutations. It is associated with the severity of liver disease. G1757 mutation and BCP A1762T/G1764A double mutation are directly linked with the high level of serum HBV DNA[48]. Various CP mutations (M1386, T1485, B1499, A1613, T1653, G1727, A1757/T1764/G1766, G or C1753, T1773, and T1766/A1768) are related to progression to HCC. These mutations individually and/or in combination are prognostic markers of HCC[49-51].
1764/1766 mutation
1764/1766 mutation is one of the core promoter mutations. It is associated with patients with severe liver disease. 1762/1764/1766 and 1753/1762/1764/1766 mutations showed increased viral replication and decreased HBeAg expression compared with 1762/1764 mutations alone; however, 1753/1762/1764 mutant showed only a small decrease in HBeAg expression like that of 1762/1764 mutant. So, core promoter mutations other than mutation (1762 and 1764) can have an influence on viral DNA replication and HBeAg expression[52].
1809-1812 mutation
1809-1812 mutations (Kozak region mutations) are responsible for HBeAg negativity and are found mainly in genotype A; subgenotype A1. Several mutations can reduce HBeAg expression: 1762T1764A mutation at the transcriptional level; 1809-1812 mutations at the translational level and 1862T mutation at the post-translational level. A1762T/G1764A mutation and 1809-1812 mutations cumulatively reduce HBeAg expression[53]. In a study from Kenya, mutations in the Kozak region (1809-1812) or precore start codon (1814-1816) were responsible for HBeAg-negativity in patients with subgenotype A1[54]. Table 2 shows the clinical potency of frequently found BCP mutations.

Table 2 Prevalent basal core promoter mutations and their clinical importance
HBV PRECORE MUTATIONS AND RELATEDNESS WITH GENOTYPE AND ADVANCEMENT OF LIVER DISEASE
Precore region
The precore gene spans the length from nt 1814 to 1901. This region has the start site for synthesis of pgRNA, direct repeat 1, and RNA encapsidation signal. The precore region plays a crucial role in viral replication. The presence of mutations in this region disrupts viral replication and results in the formation of defective replicative intermediates. These replicative intermediates (which are not encapsidated) in hepatocytes, increase the chances for integration of HBV DNA into chromosomal DNA and lead to advanced liver disease like HCC[55].
1896 mutation
1896 mutation is the one of most important precore mutations. It causes HBeAg negativity and advanced liver diseases like HCC. Moreover, the precore mutation G1896A and BCP double mutation A1762T/G1764A play a significant part in the progression of HBV-related liver diseases[21]. The precore region mutation G1896A is one of the most frequently observed mutations in ALD and chronic HBV patients[56].
The G1896A mutation gives rise to a premature stop codon and reduces HBeAg synthesis. This mutation stops HBeAg formation by checking the translation of HBeAg, and the existence of a stop codon mutation may be a cause of immune evasion[56,57]. The most commonly observed precore mutation, G1896A, stops HBeAg formation by substitution of a tryptophan residue at amino acid position 28 with a premature stop codon[58]. This mutation was observed in more than 50% of individuals with chronic hepatitis B in Asia and the Mediterranean area[58]. This mutation suppresses HBeAg production, thus causing increased HBV replication and liver disease progression[21,59,60]. Precore 1858-1896 mutations are related to high serum HBV DNA levels[61].
In a meta-analysis among Asians, G1896A mutation was found to be related to a greater chance of HCC and liver disease severity[62]. Various mutations and combinations, notably at nt 1762/1764 and nt 1896/1899 in the BCP-preC region were observed to induce HBeAg negativity, liver function impairment, and HCC progression[63]. In some of the studies listed below, G1896A mutation was associated with less severity of liver disease. In a study from Taiwan, the G1896A mutation was linked with a low HCC risk[64].
1858 mutation
1858 mutation is one of the precore mutations and is related to greater liver disease severity. In a study from Vietnam, genotype-C-infected patients contained a high rate of C-1858 mutation (70%) and it could play a decisive role in generating severe chronic liver disease[65].
1858C mutation was found to be related to A, F and H genotypes, and 1858T mutation with B, D and E genotypes[66]. C-1858 strains may be more infectious, but more investigations are required to determine the pathogenesis of this strain[67]. High serum HBV DNA level was related to precore 1858-1896 mutations. These BCP/precore mutations may act as a prognostic marker for HBV DNA increase[61]. TCC at positions 1856 to 1858 of the precore region of HBV might cause more severe liver disease than other HBV strains with genotype C[68].
The presence of C rather than T at nt 1858 prevents G1896A mutation because the above-mentioned mutations diminish the stem-loop structure of the RNA encapsidation signal. So, CCC polymorphism and 1896 mutation are mutually exclusive[69]. HBV-infected patients with C at nt 1858 have a greater prevalence of core promoter mutations, while patients infected with T at position 1858 have only precore stop codon mutations[70].
1862 mutation
1862 mutation is one of the precore mutations and is one of the leading causes of HBeAg negativity and advanced liver diseases. In a study on Chinese patients, G1862T mutation caused an amino acid change in codon 17 of the precore protein; a part of the signal peptidase recognition motif. G1862T mutations were found only in genotype-B-infected patients. These variants have reduced capacity to form HBeAg and the absence of or reduced HBeAg may be a causative factor in fulminant disease. G1862 mutation is observed more in FH patients than in chronic carriers[71].
G1862 mutation is mainly found in HBV genotype A (sub-genotype A1). G1862T mutation is associated with HBeAg negativity and low viremia level in genotype-A-infected patients[21]. Sahaet al[72] reported in an East India study that all HBV/A1 isolates had G1862T mutation regardless of HBeAg status. So, the G1862T variant might present a natural mutation in HBV/A1 isolates.
1888 mutation
1888 mutation is one of the precore mutations and is found only in subgenotype A1 and causes HBeAg negative serostatus. The linked loci 1809-1812, 1862 and 1888 are observed regularly in subgenotype A1 and they cause inhibition of HBeAg expression[53]. The 1888A mutation is related to HBV subgenotype A1 and it expresses a start codon upstream from the core ORF and can influence the core protein expression, resulting in lowering of viral level[73].
1915 mutation
1915 mutation is one of the precore mutations and is reported as one of the HCC survival mutations. Xieet al[74] observed five different mutations in the preC/C region (1915, 2134, 2221, 2245 and 2288) and these mutations act as independent predictors of HCC survival. Various newly reported preC/C promoter mutations (1690A, 1695A/T/G, 1700A/C, 1703C, 1850A and 1915A/G) were observed in HBV-infected isolates of Punjab state (North India)[75].
Scanty/rare mutations
Some rare mutations in preC/C promoter region are described below, which contribute to the severity of liver disease. Mutations in the enhancer II/BCP regions (C1653T, T1674C/G, T1753V, A1762T/G1764A and C1766T/T1768A) and mutations in the precore region (G1899A, C2002T, A2159G, A2189C and G2203A/T) are significantly associated with an increased risk of HCC[76]. Various newly reported individual/combination mutations of the X/precore region in HBV genotype D1 act as markers of HCC[50]. These mutations are T1673/G1679, G1727, C1741, C1761, A1757/T1764/G1766, T1773, T1773/G1775 and C1909[50]. Numerous core promoter mutations, 1653T, 1753V, A1762T, G1764A, 1766T and 1768A, have been observed regularly in HCC patients[77].
In anin vitrostudy, individual mutations in the BCP/precore region, T1753V (C/A/G), C1766T, T1768A, G1862T and G1899A, were linked with enhanced viral replication and/or reduced HBeAg expression and related with acute liver failure in some instances[16,52,71,78]. Renet al[79] observed that individual mutations, T1753V (C/A/G), A1762T, G1764A, G1896A and G1899A, were more regularly detected in hepatitis-B-related acute-on-chronic liver failure (ACLF) than chronic hepatitis B (CHB) patients. Patients with precore mutations have a greater risk of a fatal outcome.
Tsaiet al[80] reported that triple BCP mutation 1762/1764/1766 was related to the maximum increase in pgRNA transcription, while 1762/1764 double mutation was not so effective. T1846 and A/G1913 mutations are linked with ACLF in patients infected with genotypes B and C[81]. In Table 3 various precore/CP mutations and their correlation with clinical outcomes are shown.
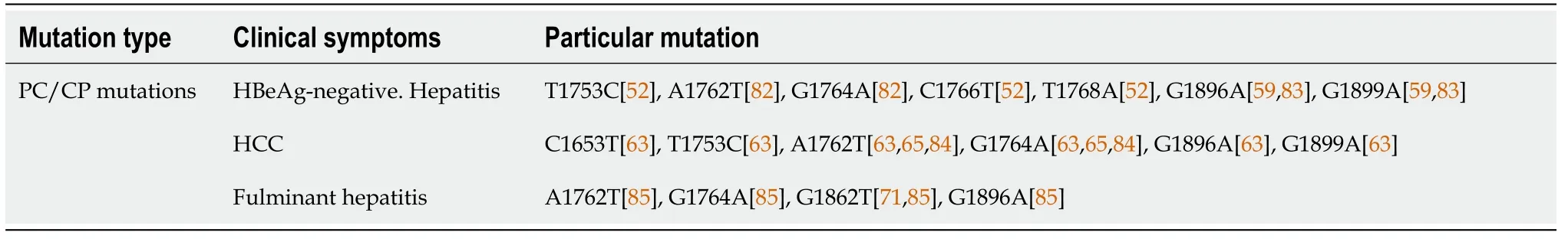
Table 3 Various precore/core promoter mutations and their clinical outcomes
DISCUSSION AND FUTURE PERSPECTIVES
HBV genotypes and viral mutations have a fair connection for various clinical conditions of CHB and this information should be utilized to predict likely clinical course,e.g.,lengthy duration of HBeAg phase and more risk of progression to cirrhosis in genotype C and increased risk of HCC in genotypes C and F. There is evidence to confirm the role of genotypes and subgenotypes in pathogenesis and clinical symptoms of HBV infection. HBeAg seroconversion is delayed in patients infected with genotype C compared to other genotypes[86]. So, more research is needed about the pathogenicity of genotypes E, F and H.
In addition, preS/S region mutations are related to vaccine failure, immune escape, occult HBV infection, and HCC occurrence. P region mutations may create drug resistance to nucleoside analog antivirals. Mutations in the preC/C region are associated with HBeAg negativity, immune escape, and persistent hepatitis. Mutations in the X region play a vital part in developing HCC[86]. Mutations in various parts of the HBV genome could be the reason for unwanted clinical outcomes or evasion of detection by various diagnostic procedures, thus it becomes necessary to detect these mutations for proper evaluation of patients.
Revill and Locarnini[87] observed and recommended that in patients infected with genotype B or C, BCP mutation is a significant biomarker of the risk of cirrhosis. So, identification and quantification of BCP mutants should be used for proper treatment in Asian CHB patients. More work on the importance of these mutations in other genotypes is suggested.
HBV genotypes and mutations act as useful viral biomarkers for the prognosis of disease progression and also assist clinicians to diagnose patients who can be treated mostly from interferon therapy. In the future, clinical trials classified by different genotypes/mutants should be adopted and it is essential to apply individualized treatment regimens for CHB patients.
For population health prospects, proper observation of the pervasiveness of vaccine escape and S escape mutations is needed and more research will be required into vaccines that remain effective against mutant strains of HBV. Identification of resistance profile is important in deciding the exact antiviral agent to start therapy.
CONCLUSION
HBV has more genomic diversity and various HBV mutants are significantly related with response to antiviral therapy, vaccine escape, diagnostic failure, liver fibrosis, liver cirrhosis, and HCC development. Understanding the correlation between various mutations and the clinical manifestations of HBV infection should lead to advances in diagnostic strategies and therapeutic directions.
ACKNOWLEDGMENTS
The authors would like to thank Dr. Jitender Bhardwaj, Assistant Professor, Zoology Department, K.U., Kurukshetra for timely support.
FOOTNOTES
Author contributions:Kumar R wrote, edit the paper and proofread the paper.
Conflict-of-interest statement:There is no conflict of interest among authors.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:India
ORCID number:Rajesh Kumar 0000-0003-2602-7714.
S-Editor:Wang JJ
L-Editor:Kerr C
P-Editor:Wang JJ
杂志排行
World Journal of Hepatology的其它文章
- Revolution in the diagnosis and management of hepatitis C virus infection in current era
- Evidence-based approach to management of hepatic encephalopathy in adults
- Direct oral anticoagulant administration in cirrhotic patients with portal vein thrombosis: What is the evidence?
- Noninvasive diagnosis of periportal fibrosis in schistosomiasis mansoni: A comprehensive review
- Assessment of periportal fibrosis in Schistosomiasis mansoni patients by proton nuclear magnetic resonance-based metabonomics models
- Baicalin provides protection against fluoxetine-induced hepatotoxicity by modulation of oxidative stress and inflammation
