Noninvasive diagnosis of periportal fibrosis in schistosomiasis mansoni: A comprehensive review
2022-07-02JoelmaCarvalhoSantosCarolineLouiseDinizPereiraAnaciaCoutinhoDominguesEdmundoPessoaLopes
Joelma Carvalho Santos, Caroline Louise Diniz Pereira, Ana Lúcia Coutinho Domingues, Edmundo Pessoa Lopes
Joelma Carvalho Santos, Caroline Louise Diniz Pereira, Ana Lúcia Coutinho Domingues, Edmundo Pessoa Lopes, Postgraduate Program in Tropical Medicine, Center of Health Sciences, Universidade Federal de Pernambuco, Recife 50670-901, Pernambuco, Brazil
Ana Lúcia Coutinho Domingues, Edmundo Pessoa Lopes, Gastroenterology Division, Department of Internal Medicine of Center of Health Sciences, Hospital das Clínicas - Universidade Federal de Pernambuco, Recife 50670-901, Pernambuco, Brazil
Abstract Schistosomiasis mansoni is a neglected disease and key public health problem, mainly due to its high prevalence, the scarcity of public policies, and the severity of some clinical forms. Periportal fibrosis (PPF) is the commonest complication of chronic schistosomiasis mansoni and its diagnosis requires different techniques. Even though wedge biopsy of the liver is considered the gold standard, it is not justified in non-surgical patients, and percutaneous liver biopsy may be informative but does not have sufficient sensitivity. Noninvasive PPF tests mostly include biological (serum biomarkers or combined scores) or physical assessments (imaging assessment of fibrosis pattern or tissue stiffness). Moreover, imaging techniques, such as ultrasound, computed tomography, magnetic resonance imaging, and elastography are applied not only to support the diagnosis of schistosomiasis, but also to assess and detect signs of portal hypertension and organ damage due to chronic schistosomiasis. A combination between a comprehensive history and physical examination with biomarkers for liver fibrosis and imaging methods seems to offer the best approach for evaluating these patients. In addition, understanding their strengths and limitations will allow a more accurate interpretation in the clinical context and can lead to greater accuracy in estimating the degree of fibrosis in patients with Schistosomiasis mansoni (S. mansoni) infection. This review will discuss the different noninvasive methods that are currently available for the evaluation of PPF in S. mansoni infection, and their application, advantages, and limitations in clinical practice.
Key Words: Schistosoma mansoni; Parasitic liver diseases; Liver fibrosis; Biomarkers; Elasticity imaging techniques; Ultrasonography
INTRODUCTION
Schistosomiasis mansoni is a neglected parasitic disease of chronic evolution and a key public health problem, mainly due to its high prevalence, the scarcity of public policies, and the severity of some clinical forms. As it is endemic in over 78 resource-constrained countries, schistosomiasis is considered one of the indicators of poverty[1,2].
The World Health Organization (WHO) estimates that at least 241 million people required preventive treatment[3]. In Brazil, the economic burden of schistosomiasis mansoni is high and results in loss of productivity, and it is a big challenge to public health[4]. Approximately 200 thousand deaths are attributed to this disease annually and they occur in up to 29% of those who present bleeding varices even with full hospital care. Community-based studies suggest that periportal fibrosis (PPF), which is the term more frequently used after the advent of ultrasonography in schistosomiasis, is the commonest complication ofSchistosomiasis mansoni (S. mansoni)chronic infection[5].
Additionally, Symmers fibrosis or “pipestem fibrosis” is the advanced PPF form that occurs in patients with hepatosplenic schistosomiasis (HSS) and it is defined as a moderate to advanced PPF, with or without hepatomegaly, but always with splenomegaly, on ultrasound (US). In endemic areas, it is possible to find patients with advanced PPF (Symmers fibrosis) without splenomegaly, also known as the hepatic form of the disease. On the other hand, a few individuals with splenomegaly without PPF can also be found, which is due to other causes of splenomegaly, and if there were no US, these patients would be misdiagnosed, based on the clinical examination, as HSS.
Hence, Symmers fibrosis is the most prominent feature of liver pathology in schistosomiasis mansoni and it is represented by a process of portal fibrosis that extends from the smallest to the largest portal spaces[6]. Granulomas around the parasite eggs can be seen in abundance in the portal spaces, at the beginning of the disease, which disappear when it becomes chronic and the fibrosis remains. There are also obstructive vascular lesions secondary to granulomas, thrombosis, phleboscleorosis, and fibrous intimal thickening. The major liver pathology of egg granulomas results from physical obstruction and tissue compression, while splenomegaly results from both chronic passive congestion and reactive hyperplasia of the reticuloendothelial system due to immune dysregulation[7]. The main clinical manifestation of HSS is portal hypertension (non-cirrhotic) and porto-systemic collateral circulation, notably esophageal varices[8,9].
The hepatic parenchyma maintains its usual acinar structure, and this is reflected in patients exhibiting a normal hepatocyte function despite the signs of portal hypertension, without stigmata of chronic liver disease, unlike cirrhosis. However, in some cases, compensated HSS may turn into decompensated HSS with the presence of stigmatas, ascites, muscular loss, and hepatic failure[8]. These cases of progression from schistosomiasis to liver cirrhosis, with the capacity of the synthesis of hepatocytes being impaired, are sometimes observed in clinical practice in patients who have recurrent episodes of digestive bleeding and repeated necrosis of hepatocytes.
In these decompensated cases, it should also be remembered that there is the possibility of coinfection of schistosomiasis with hepatitis B, C, and E viruses, with the non-alcoholic steatohepatitis or chronic alcohol abuse[10-12].
Schistosomiasis mansoni is commonly diagnosed due to detecting parasite eggs in stool using the Kato-Katz technique. Immunological methods are favored for monitoring communities in areas with low infection rates, and for patients with mild and chronic infections where parasitological tests are negative. Polymerase chain reaction-based diagnostic techniques are more sensitive, but expensive. The Point-of-care Circulating Cathodic Antigen test method appeared to be a promising feature in the diagnosis, but many false positive cases were reported in low endemic areas[2,3,13].
Recently, studies in low prevalence areas for schistosomiasis in Brazil have shown that the primary diagnostic approach performed by the Schistosomiasis Control Country Program may underestimate the real prevalence of this infection. In addition, there have been reports of a high proportion of infected individuals in the urban area, the presence of infected snails, a random distribution of vectors, and the absence of an association between classical risk factors and the human infection[14]. In low endemic countries, the determination of infected patients should combine different methods and algorithms for accurately estimating the prevalence and the indicators that could be used in the control of schistosomiasis[2].
Moreover, diagnosing PPF requires different techniques. Wedge liver biopsy is considered the gold standard, but it is not justified in non-surgical patients. Alternatively, percutaneous liver biopsy may be informative but does not have sufficient sensitivity[15,16]. Imaging techniques like US, computed tomography (CT), magnetic resonance imaging (MRI), and elastography, on the other hand, are used not only to support the diagnosis of schistosomiasis but also to assess and detect signs of portal hypertension and organ damage due to chronic schistosomiasis disease[17-20]. A combination between a comprehensive history and physical examination with biomarkers for liver fibrosis, and imaging methods seems to offer the best approach for evaluating these patients[7,17].
In this review, we will discuss the different noninvasive methods that are currently available for evaluating PPF in chronic schistosomiasis mansoni, and their application, advantages, and limitations in clinical practice.
NONINVASIVE MARKERS OF PPF
Noninvasive markers of liver fibrosis can be divided into two groups: Serum biomarkers and imaging techniques. Table 1 summarizes the main features of these methods. Besides the clear advantage of being noninvasive, some of them can offer a more objective interpretation of numerical test results and may overcome the intra- and inter-observer variability of US techniques.

Table 1 Major advantages and limitations of noninvasive periportal fibrosis markers in Schistosomiasis mansoni infected patients
Serum biomarkers
Serological biomarkers of liver fibrosis are frequently classified as direct or indirect biomarkers. Whereas direct biomarkers reflect extracellular matrix (ECM) turnover and the changes in the fibrogenic cell type, indirect biomarkers mostly estimate the degree of fibrosis[21].
In advanced stages of fibrosis, the liver contains approximately six times more ECM components than normal, including collagens (I, III, and IV), fibronectin, undulin, elastin, laminin, hyaluronic acid (HA), and proteoglycans[22]. Therefore, qualitative and quantitative ECM changes in liver fibrosis can be measured in the blood or urine using these serological biomarkers[23].
Direct and indirect markers may be used alone or in combination to produce composite scores, which can be relatively simple or can be based on complicated formulas[21]. These markers should be reliable and sensitive so as to indicate advanced lesions and also have prognostic value for identifying early disease[17]. Table 2 summarizes the major advantages and limitations of these markers.

Table 2 Major advantages and limitations of noninvasive periportal fibrosis markers in Schistosomiasis mansoni infected patients
Direct markers
Direct markers are usually fragments of the components of the ECM of the liver produced by hepatic stellate cells during the ECM remodeling process and they usually reflect its deposition or removal[24]. However, they do not indicate the extent of ECM protein distribution[21] and since they are not liver specific, they have a tendency to be more elevated when associated with high inflammatory activity and tend not to be detected in the presence of minimal inflammation[24].
These biomarkers are classified into three groups: Those that measure matrix deposition [procollagen I carboxy terminal peptide, procollagen III amino terminal peptide, tissue inhibitors of metalloproteinase (MMP), transforming growth factor beta and tenascin], those that reflect matrix removal or degradation (procollagen IV C peptide, procollagen IV N peptide, collagen IV, MMP, undulin, urinary desmosine, and hydroxylysylpyridinoline), and those that cannot clearly determine the relationship to the matrix deposition or removal (HA, chitinase-3-like protein 1, and laminin)[23].
Even though direct markers are less useful in clinical practice due to their high cost and difficult procedures, their potential role in the diagnosis and assessment of PPF in schistosomiasis warrants further investigation. The most promising and studied serum markers for the evaluation of PPF are HA, collagen type III, chitinase-3-like protein 1, and laminin[17,23,25].
Since the latest studies referring to these markers have been previously described in complete review articles[17,23,24], the present paper will not be well on them but rather will concentrate on the most recent markers.
Indirect markers
Indirect markers include molecules synthesized, regulated, excreted by the liver or released into the blood in response to liver inflammation, or impairment of the liver function[24].
These markers include common clinical biochemistry tests, such as enzymes, proteins, platelets, and coagulation factors, which do not necessarily reflect ECM turnover or fibrogenic cell changes[24]. Moreover, most indirect biomarkers of fibrosis are integrated with one or more biomarker panels that predict fibrosis.
The most prevalent markers to assess PPF are the platelet count, aspartate aminotransferase to platelet ratio index (APRI)[26,27], Fibrosis-4 (FIB-4)[4], gamma glutamyl transferase (GGT)[17,28], and the Coutinho Index[29,30]. Table 3 summarizes the performance of these markers that has been reported in the literature.

Table 3 Performance of indirect periportal fibrosis markers in Schistosomiasis mansoni infected patients
In addition, Nascimentoet al[4] (2018) noted a correlation tendency between the scores for APRI and FIB-4 (Spearmanr= 0.87,P< 0.0001), transient elastography (TE) and FIB-4 (r= 0.70,P= 0.01), and TE and GGT (r= 0.68,P< 0.01) in a small sample of 17 patients with schistosomiasis. Therefore, further studies with a larger sample are required to confirm these results and to determine if this correlation can be used clinically.
The Coutinho index is the alkaline phosphatase (ALP) to platelet ratio {[ALP/upper limit of normality (ULN)]/platelet count (106/L) × 100}. This index was developed to identify patients with more advanced fibrosis (Niamey’s US classification D, E, and F patterns) in endemic areas, without the need for US. These patients, once recruited, were evaluated and, if necessary, sent to a referral hospital. Barretoet al[29] initially studied 120 patients at the referral hospital in Pernambuco, Brazil. After analyzing different enzymes that change during the course of this disease, they developed this index. Subsequently, in another study, this index was validated in an endemic area of the same state, with 378 patients who took a parasitological test that was positive forS. mansoni[30].
Moreover, Gundaet al[31] have also indicated a positive correlation between the presence of esophageal varices and higher APRI levels (> 1.5 m/s,P< 0.001) with a higher sensitivity (82.5%) and specificity (80.1%) in discriminating varices among patients with PPF due to schistosomiasis mansoni. The most common diagnostic approaches to stratify patients based on the risk of variceal bleeding include the use of US and platelet count[32].
In this context, Aghaet al[33] in a case-control study in Saudi Arabia, and Xuet al[34] in a cohort in China, investigated, independently, the platelet count/spleen diameter ratio and reported high specificity (83% to 92%) and sensitivity (85% to 100%) for the presence of esophageal varices in HSS patients.
Although the results of some of these studies are promising with regard to evaluating PPF with these indices, more studies with a larger number of patients will be necessary in order to demonstrate the validity of applying these indices in clinical practice.
Imaging techniques
The early detection of serious complications is vital in the management of chronic schistosomiasis. Thus, making use of diagnostic imaging modalities, such as US, CT, and MRI, is very important as each of them has a vital role in diagnosing and assessing the severity of target organ involvement[35,36].
Since US is a convenient and reliable method, it is routinely used in the diagnosis and evaluation of patients with schistosomiasis and it has become the most well-established tool for evaluating PPF. It can be applied to demonstrate classical features of schistosomal hepatic damage and to grade schistosomiasis disease patterns and status, based on criteria published by the WHO[37].
US is a simple, inexpensive, and safe tool and the technique is more sensitive with respect to diagnosing advanced PPF (Symmers fibrosis) than its milder stages. Since the advent of the WHO protocol[37] and later the Niamey-Belo-Horizonte Protocol (2001), US has become the gold standard in the diagnosis of PPF and in the classification of its intensity, which is mainly based on the use of pictorial image patterns (Table 4 and Figure 1). Other previously used protocols, such as Cairo and Managil, were abandoned due to flaws in classifying mild forms of the disease[38,39].
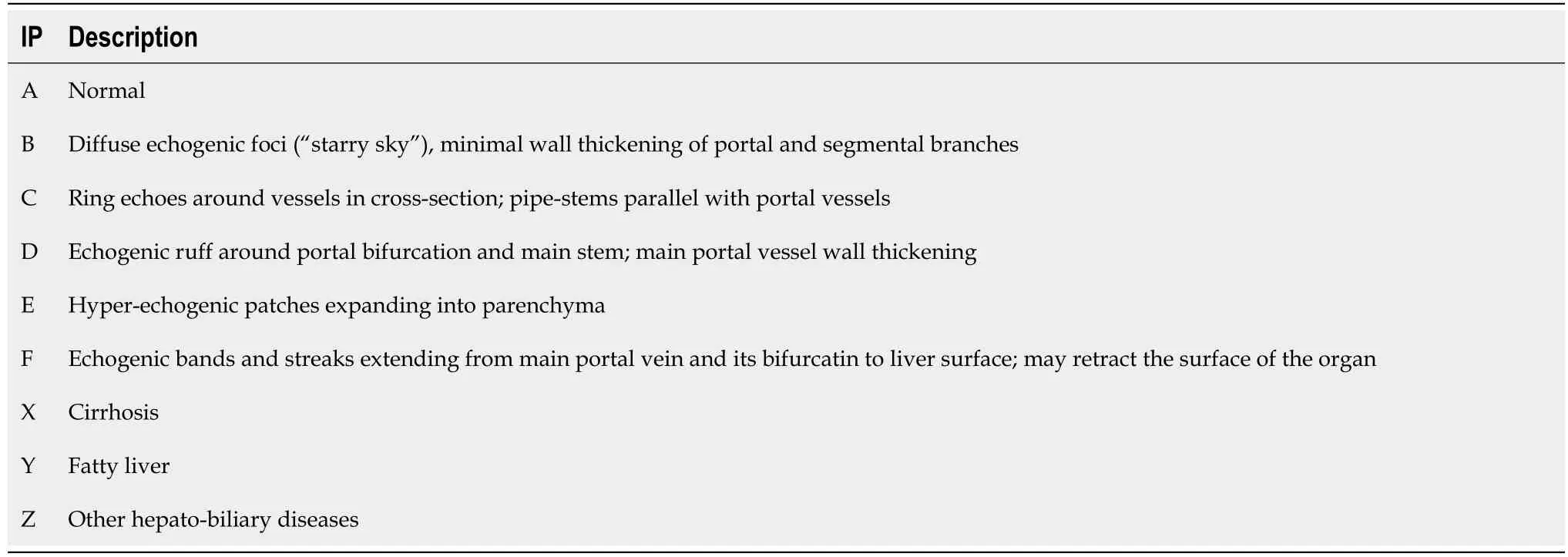
Table 4 Image pattern classification of periportal fibrosis according to the World Health Organization[37]

Figure 1 Ultrasound-based liver images obtained from patients with periportal fibrosis due to Schistosomiasis mansoni infection, by a Siemens scanner based on Niamey’s pattern, Pernambuco, Brazil, 2020. A: Pattern C; B: Pattern D; C: Pattern E; D: Pattern F.
Santoset al[14] demonstrated moderate to substantial reproducibility in the PPF classification according to the WHO protocol, mainly using image patterns. In field studies, using these patterns is reported to be simpler and more reproducible than applying other measurements, such as the thickness of the wall of the portal branch and the diameter of the portal, which are also recommended in the WHO protocol[40,41].
Furthermore, the imaging patterns B, C, and D can also be found in other diseases, such as congenital liver fibrosis, viral and autoimmune hepatitis, primary sclerosing cholangitis, and liver cirrhosis. Consequently, a more rigorous analysis by the observer is required to find other signs that will lead to a differential diagnosis of schistosomiasis liver fibrosis[42].
More advanced portable US equipment, like color Doppler US, can characterize portal vein perfusion to predict disease prognosis and with this, decisions can be made on the best treatment options for portal hypertension complications, such as portal vein thrombosis[18].
In our opinion, as US is an operator-dependent technique, the previous experience of the ultrasonographist is very important in evaluation of the image patterns and therefore, to obtain more consistent results. That is the reason why it is unsuitable for the PPF evaluation by US scan to be performed by non-physicians in rural areas, even if they are well trained. Well-trained physicians who know about other diseases that may affect the liver would apply the Niamey protocol in the evaluation of PPF in patients withS mansoni. However, in endemic areas, this protocol is not widely applied by every physician that usually performs US, but only by the few who are trained and interested in research projects.
CT and MRI can also be applied to diagnose PPF. The main features of CT in the fibrotic liver with HSS are round, low-density periportal zones enhanced after contrast administration, and linear bands in longitudinal sections of portal veins[43]. On the other hand, MRI is described as a more sensitive imaging technique than US in the diagnosis of Symmers fibrosis, because it can differentiate fibrosis from fatty liver disease and inflammatory infiltrate.
However, these techniques are not routinely used for schistosomiasis diagnosis in resource-poor settings, due to the use of contrast and the associated risks and the costs[44-46]. In addition, some places do not have an adequate structure for installing these sophisticated devices.
Nevertheless, Voietaet al[47] aimed to classify schistosomal PPF intensity and observed a moderate agreement between imaging techniques (US and MRI) (κ= 0.41). However, it was only after re-grouping the grades (absent and slightvsmoderate and intense) that it was observed that the concordance was substantial (κ= 0.63). On the other hand, the agreement between US and MRI and histology was poor.
Moreover, Silvaet al[15] described a poor correlation between US and MRI in PPF assessment using WHO patterns (κ= 0.14), and even after grouping image patterns such as “A-D”, “Dc-E” and “Ec-F”, the agreement between US and MRI remained weak (κ= 0.39). The authors recommended that new patterns should be constructed to better reflect MRI findings. Accordingly, Scortegagnaet al[48] reported that MRI presented a good reproducibility in the evaluation of PPF in later stages of schistosomiasis, with a global interobserver agreement of 70%. However, the correlation between MRI and US was poor, showing only a 30% agreement.
Recently, elastography-based imaging techniques, such as TE and point shear wave elastography (pSWE) using acoustic radiation force imaging (ARFI), have received substantial attention with respect to the non-invasive assessment of the mechanical properties of tissue. These techniques have emerged as complementary to US images in the study of liver fibrosis in many hepatic diseases[49,50] including schistosomiasis mansoni[19,20,51-54].
These techniques take advantage of changes in the elasticity of soft tissue according to the involvement of certain organs, including the liver and spleen, as this yields qualitative and quantitative information that could be used for diagnostic and prognostic purposes[55].
Recent studies have suggested an association between the degree of liver fibrosis in chronic hepatitis C virus (HCV) infection, reflected by the shear wave speed in the liver, and the severity of liver disease (advanced, compensated, decompensated, or hepatocellular carcinoma). Additionally, in 358 patients with schistosomiais mansoni, Carvalho Santoset al[19] evaluated the PPF by hepatic pSWE (ARFI), thus revealing that this technique could be useful in the diagnosis of advanced forms of schistosomiasis mansoni. The ARFI was able to accurately differentiate mild PPF from significant PPF. Table 5 summarizes the performance reported in the literature of noninvasive PPF imaging techniques inS. mansoniinfected patients.

Table 5 Performance reported in the literature of noninvasive periportal fibrosis imaging techniques in Schistosomiasis mansoni infected patients
Similarly, an association has also been reported between splenic elastography and signs of portal hypertension, including the presence of esophageal varices, in some chronic liver diseases[56]. However, these are still initial studies in assessing schistosomiasis portal hypertension[52].
In fact, recent studies have shown that the measurement of spleen stiffness by TE and pSWE correlates with that of liver stiffness and of portal hypertension in patients with HSS[20,52]. Accordingly, spleen stiffness may also be a predictor of variceal bleeding in HSS and may be further investigated for predicting HSS complications[57].
Furthermore, it is relevant to highlight that, in schistosomiasis, massive splenomegaly occurs due to the hyperplasia of the reticuloendothelial system. Hence, there is an increase in blood flow in the splenic vein and also obstruction for the venous flow by intra-hepatic granulomas resulting in portal hypertension[9,58]. The pathophysiology of portal hypertension in (non-cirrhotic) schistosomiasis should contribute to more changes in splenic parenchyma stiffness compared to cirrhosis, since the spleen undergoes passive congestion (without hyperplasia). As a result, splenic elastography should be more accurate than liver elastography for evaluating disease morbidity and portal hypertension signs in patients with schistosomiasis mansoni[59,60]. Table 6 summarizes the advantages and limitations of noninvasive PPF techniques that are frequently used in clinical practice with regard toS. mansoniinfected patients.

Table 6 Advantages and limitations of noninvasive periportal fibrosis techniques frequently used in clinical practice with regard to Schistosomiasis mansoni infected patients
COST-EFFECTIVENESS OF NONINVASIVE MARKERS OF FIBROSIS
Despite their increased use in clinical practice, Non-invasive tests were not designed to follow longitudinal changes in fibrosis or disease activity nor to reflect the dynamic process of fibrogenesis and differentiate between adjacent disease stages regardless of their increased application in clinical practice. Comprehending their strengths and limitations will result in a more accurate interpretation in the clinical context[61].
Therefore, liver fibrosis biological markers allow an objective interpretation of results and significantly reduce the risk of bias due to variability that occurs in liver biopsy, in addition to which these markers have the advantage of not being invasive. Associating the various non-invasive methods can lead to greater accuracy in estimating the degree of fibrosis in patients with schistosomiasis mansoni disease[4].
Crossanet al[62] in a cost-effectiveness study of non-invasive tests for assessment and monitoring of liver fibrosis and cirrhosis in patients with chronic liver disease in the United Kingdom, reported that high-quality studies with a low risk of bias are required to allow sufficient validation of specific cut-offs to stage fibrosis in different disease etiologies.
Moreover, Crossanet al[62] suggested that, for HCV and hepatitis B virus (HBeAg-negative) infected patients, treating all patients without prior diagnostic testing and regardless of fibrosis level was the most cost-effective option. Nevertheless, the findings from these models may not be transferable to a resource setting where funds are limited and the ability to treat all patients is not a realistic option[63].
In rural areas with few resources, it becomes very difficult to implement imaging methods, such as elastography, for example, or even for there to be a trained physician available to perform US and define the fibrosis pattern using the Niamey-Belo Horizonte protocol. Certainly, the use of serum markers, especially the platelet count and the Coutinho index, should be the most cost-effective, straightforward, and objective noninvasive way to identify and select patients who may have the most advanced forms of PPF.
CONCLUSION
By undertaking this literature review, we have observed that noninvasive PPF tests mostly include biological (serum biomarkers, indices, or combined algorithms) or physical assessments (imaging assessment of the fibrosis pattern or tissue stiffness). Even though currently available approaches have shown some advantages with respect to overcoming the limitations set out in the previous section, the reason for requesting a test is what will determine the best one for each case.
To date, the platelet count and the Coutinho index appear to be the most applicable noninvasive tests for evaluating PPF in endemic zones where schistosomiasis mansoni occurs. These tests are simple and inexpensive and thus are used to select the cases that will need more accurate evaluation (US assessment of the fibrosis pattern or tissue stiffness). However, they are not always available in endemic areas. Therefore, in such cases, hepatosplenic patients should be referred, if necessary, to hospitals where more specialized imaging tests, such as MRI and CT, can be conducted.
FOOTNOTES
Author contributions:Santos JC and Pereira CLD wrote the paper; Domingues ALC and Lopes EP contributed to the concept and the revision of the paper.
Conflict-of-interest statement:All authors declare that there is no conflict of interest to disclose.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Brazil
ORCID number:Joelma Carvalho Santos 0000-0002-3949-6766; Caroline Louise Diniz Pereira 0000-0002-5955-0774; Ana Lúcia Coutinho Domingues 0000-0002-1824-7090; Edmundo Pessoa Lopes 0000-0002-3470-1564.
S-Editor:Wang JJ
L-Editor:Wang TQ
P-Editor:Wang JJ
杂志排行
World Journal of Hepatology的其它文章
- Revolution in the diagnosis and management of hepatitis C virus infection in current era
- Evidence-based approach to management of hepatic encephalopathy in adults
- Direct oral anticoagulant administration in cirrhotic patients with portal vein thrombosis: What is the evidence?
- Review on hepatitis B virus precore/core promoter mutations and their correlation with genotypes and liver disease severity
- Assessment of periportal fibrosis in Schistosomiasis mansoni patients by proton nuclear magnetic resonance-based metabonomics models
- Baicalin provides protection against fluoxetine-induced hepatotoxicity by modulation of oxidative stress and inflammation