Impact of preoperative carbohydrate loading on gastric volume in patients with type 2 diabetes
2022-06-27XinQiangLinYuRenChenXiaoChenYuPingCaiJianXinLinDeMingXuXiaoChunZheng
lNTRODUCTlON
Overall, 80 patients with T2D who received surgery under general anesthesia from December 2019 to December 2020 were enrolled in the study. Of them, 2 patients were excluded due to unclear images of the gastric antrum. Finally, 78 patients with complete follow-up data were included in the study. The flow chart of the study is presented in Figure 1. The day before surgery, patients who fulfilled the study criteria and provided written consent were randomly allocated to 4 groups. Randomization was performed using computer-generated random numbers indicating different volumes of carbohydrate loading. Patients received a clear carbohydrate drink (0, 100, 200, or 300 mL) 2 h before anesthesia induction on the day of surgery. Each group uses the same concentration of carbohydrate drink that contains 14.2 g of carbohydrate
100 mL (Yichang Human Medical Food Co., Ltd.). Randomization was performed using computer-generated four-digit random numbers indicating the treatment, which were kept in sealed envelopes. An envelope was opened according to the random number from small to large based on the time sequence of inclusion of each subject. The ultrasound examiner was blinded by the study protocol, as was the staff involved in the medical procedures and data collection process. All patients received surgery under general endotracheal anesthesia. Intraoperative fluid management was limited to a glucose-free solution, and no exogenous insulin was administered. Postoperative care was standardized as clinically indicated.
Author contributions: All authors contributed to the study conception and design; Zheng XC designed the study;Material preparation, data collection and analysis were performed by Lin XQ, Chen YR and Chen X; Cai YP, Lin JX and Xu DM contributed sample collection and intellectual input; The first draft of the manuscript was written by Lin XQ and all authors commented on previous versions of the manuscript; All authors read and approved the final manuscript; Lin XQ and Chen YR contributed equally to this study.
为了有效利用护理人力资源,充分调动护理人员的工作积极性,不断提高护理质量,我院根据卫生部关于事业单位实施绩效工资、完善分配激励机制的相关决策要求,在重症监护病区(ICU)率先开展了护理绩效考核制度的建立与实施,取得很好的效果,现报道如下。
More than 10% of the world population is reported to have diabetes[6], and nearly 15% of surgical patients have type 2 diabetes (T2D)[7]. Complications and hospital stays are greater in these patients than in non-diabetic patients[8,9]. Delayed gastric emptying (gastroparesis) is also more frequent in patients with diabetes[10,11]. Therefore, preoperative carbohydrate loading may adversely affect gastric volume (GV) in diabetic patients. Moreover, carbohydrate loading-induced hyperglycemia may outweigh the potential benefits of ERAS protocols in such patients. Laffin
[12] found no significant difference in the hyperglycemic incidence between the groups with and without carbohydrate loading[12]. However, other studies have reported high rates of adverse outcomes, such as postoperative wound infections, cardiac events, and other complications caused by hyperglycemia, in diabetic patients receiving preoperative carbohydrate loading[13]. It is important to further study the change in blood glucose levels in diabetic patients receiving preoperative carbohydrate loading.
Perlas used ultrasound to grade GV, which was measured in the right decubitus and supine positions to assess the risk of aspiration, The visualization of gastric antrum content was scored using the Perlas grading system: Grade 0, no content visible in the supine or right lateral (RLD) position; grade 1, clear gastric fluid content only in the RLD position, but not in the supine position; and grade 2, clear gastric fluid content visible in both supine and RLD positions[14]. Perlas grade II and GV > 1.5 mL/kg have been reported to be associated with a high risk of reflux and aspiration[15,16]. Therefore, ultrasonography is used to evaluate GV both qualitatively and quantitatively. It is an economical, safe, noninvasive, and repeatable technique to assess the risk of anesthesia before surgery[17]. Data on preoperative carbohydrate loading in patients with T2D are limited[18,19]. In this study, we assessed GV, the incidence of hyperglycemia, and the risk of gastric reflux and aspiration using ultrasonography.We also evaluated the time and dose of preoperative carbohydrates using stratified analysis. These assessments allowed us to determine the safety and feasibility of preoperative carbohydrate loading in patients with T2D.
MATERlALS AND METHODS
Inclusion and exclusion criteria
Data of adult patients (age: 40-80 years) who received surgery under general anesthesia were enrolled according to the following inclusion criteria: (1) American Society of Anesthesiologists Physical Status Classification System (ASA) classified as II-III; (2) Definite diagnosis of T2D for > 2 years; (3)Preoperative blood glucose < 10 mmol/L; (4) Glycosylated hemoglobin (HbA1c) < 8.5%; and (5) Body mass index (BMI) of 18-35 kg/m
. Patients were excluded from the study if they had any of the following: (1) Pregnancy; (2) Cardiac or renal dysfunction; (3) Hypothyroidism; (4) Obesity (BMI > 35 kg/m
); (5) Digestive system diseases, including gastroesophageal reflux, peptic ulcer, digestive system tumors, cholelithiasis or history of upper gastrointestinal surgery; (6) Receiving antiemetic drugs or other drugs affecting gastrointestinal motility before operation; (7) Preoperative gastrointestinal decompression or nutrition; or (8) Unwilling to participate in the study.
Patients and study design
Enhanced recovery after surgery (ERAS) is a set of perioperative protocols to reduce complications,facilitate recovery, and decrease the length of hospitalization[1,2]. Insulin resistance is a critical complication of injury or stress. Most patients receiving surgery may develop postoperative insulin resistance. The resulting hyperglycemia is often associated with an increased risk of morbidity and mortality. ERAS recommends preoperative carbohydrate loading to decrease postoperative hyperglycemia by 50%, optimizing recovery[3-5].
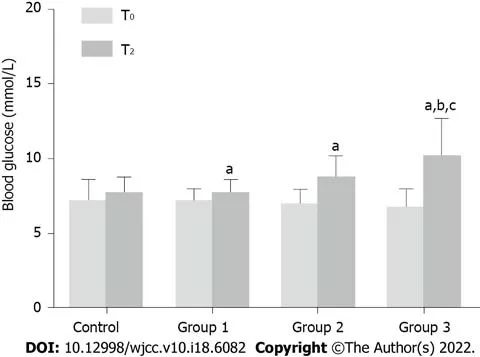
The blood glucose level in all patients was tested before carbohydrate loading (T0) and anesthesia induction (T2). In groups 1, 2, and 3, blood glucose levels increased significantly at T2 compared with that at T0 (
< 0.05). In patients receiving 300 mL of the carbohydrate drink (group 3), the blood glucose level at T2 increased by > 2 mmol/L, which was significantly higher than that in groups 1 and 2. This finding indicates that a 300 mL carbohydrate load may increase the blood glucose level in patients with T2D before anesthesia induction (Figure 4).
数学形态学是一种基于集合的滤波器。这一环节的关键是找好结构元素。在本次实验中选取22x7的矩形作为结构元素,其长宽比例与要识别的车牌是相同的。相应的通过腐蚀之后再膨胀运算能够使得最终的图形更加接近于实际的车牌形状。为了通过数学形态学运算构造连通区域,需要先对二值化之后的图像进行闭运算,填补类似于车牌中字符之间的凹槽,如图4所示。
Data collection and assessment
Ultrasonography was performed by an experienced investigator certified by the Chinese Health Commission. GV was assessed on the day of surgery before carbohydrate loading (T0, basal value), 2 min after carbohydrate loading (T1), and before anesthesia induction (T2). A standard convex ultrasound probe was used to scan the gastric antrum in the sagittal plane between the liver and pancreas, at first in the supine position and then in the RLD position. The gastric antrum content visualization was scored using the Perlas grading system: Grade 0, no content visible in the supine or RLD position; grade 1, clear gastric fluid content only in the RLD position, but not in the supine position; and grade 2, clear gastric fluid content visible in both supine and RLD positions[14]. The longitudinal (D1)and anteroposterior (D2) diameters of the antrum were determined, which were repeated 3 times and averaged (Figure 2). The gastric antral area (CSA) was calculated using the following formula: CSA = π× D1 × D2/4. A mathematical model was used to measure GV: 27 + 14.6 × CSA - 1.28 × age. In addition,blood glucose levels were monitored before carbohydrate loading (T0) and anesthesia induction (T2).Patients with GV
unit weight (GV/W) > 1.5 mL/kg were regarded as having a high risk of reflux and aspiration. Gastrointestinal decompression was performed before anesthesia induction in these patients. If the blood glucose level was > 10 mmol/L at T2, the surgery was delayed until it normalized.
Statistical analysis
The sample size was determined on the basis of the GV/W at different time periods. The average GV/W at T0, T1 and T2 in the control group was 0.66, 0.64, and 0.70 mL/kg, respectively, in our preliminary study. The values at T0, T1, and T2 in groups receiving 100 mL, 200 mL, and 300 mL carbohydrate drink were 0.45, 1.2, and 0.53 mL/kg; 0.70, 3.20, 0.85 mL/kg; and 0.65, 4.67, 0.8 mL/kg,respectively. Based on these values, we found that a sample of at least 20 patients in each group and 80 patients in total would ensure 80% power for the study to evaluate the effect of preoperative carbohydrate loading on GV. The 80% power was calculated considering a two-sided type I error of 0.05 by log-rank test and 20% loss to follow-up.


All statistical analyses were performed in SPSS (version 24.0, IBM, New York, United States).Normally distributed continuous data are presented as mean ± SD. Categorical data are presented as frequency or rate. Age, height, weight, BMI, course of the disease, HbA1c (%), and fasting blood glucose were compared using one-way ANOVA. The ASA scores, gender, and control of blood glucose were the Chi-square test or Fisher exact test. The GV
unit body weight and peripheral capillary blood glucose were examined with the repeated measures analysis of variance. The Bonferroni method was applied for pairwise comparisons in the repeated measures analysis of variance. All statistical analyses were two-sided tests. A
< 0.05 indicated a statistically significant difference.
RESULTS
Patient characteristics
A total of 78 patients with T2D were randomly allocated to 4 groups, with the control group receiving 0 mL, group 1 receiving 100 mL, group 2 receiving 200 mL, and group 4 receiving 300 mL carbohydrate drink. All groups were well balanced for characteristics, including gender, age, BMI, height, weight,ASA grade, disease course, HbA1c, fasting blood glucose level, and control of blood glucose (Table 1).
Analysis of GV
Preoperative carbohydrate loading < 300 mL 2 h before anesthesia induction in patients with T2D did not affect GV or increase the risk of reflux and aspiration. Blood glucose level did not significantly change with preoperative carbohydrate loading of < 200 mL. However, 300 mL carbohydrate loading may increase blood glucose levels in patients with T2D before anesthesia induction. In conclusion, it is safe for patients with T2D to drink 200 mL 14.2% carbohydrate 2 h before surgery. In the future, we will study whether preoperative consumption of 200 mL of 14.2% carbohydrate can reduce postoperative insulin resistance and promote recovery of patients.
Analysis of blood glucose levels
药品管理指的是针对药房当中一部分容易让人产生依赖性的药品进行分类管理工作,这些容易上瘾的药品包括有阿片和阿片的衍生物,同时也包含有一些吗啡、可卡因以及大麻的代用品等药品。对于医学来说,这一类药品的使用是一把双刃剑,在能够帮助缓解患者疼痛的同时,如果使用过量还会影响患者的健康水平,因此为了防止药物的滥用,需要在药方加强药品管理。
Boosting算法也是一种基于数据集重抽样算法,与Bagging算法主要区别在于需要动态调整训练样本中各数据权重,每一次迭代增加不能正确学习样本权重,降低能正确学习样本权重,从而提升在整个训练样本数据集上的学习正确率。基本算法如下。
DlSCUSSlON
Preoperative carbohydrate loading improves glycemic control and postoperative recovery in nondiabetic patients[3,4]. However, the practice of carbohydrate loading in patients with T2D is controversial because of reflux and aspiration concerns due to increased GV and delayed emptying. In our study, no difference was found in GV/W between T0 and T2 in all groups. This finding indicates that GV does not increase with a carbohydrate loading of < 300 mL. Our results are in line with those of previous studies, which reported no delay in gastric emptying in patients with T2D compared with healthy control subjects[20]. Our patients drank 14.2% liquid carbohydrates with low osmotic pressure.Delayed gastric emptying seems to affect solids rather than liquids in patients with diabetes, which can possibly explain the similar GV between T0 and T2 in our study[10,21]. Furthermore, in our study, the preoperative fasting blood glucose level was controlled less than 10 mmol/L, which may reduce the incidence of delayed gastric emptying in T2D. Previous studies have shown that severe acute hyperglycemia may lead to delayed gastric emptying[22]. In summary, carbohydrate loading of < 300 mL 2 h before anesthesia induction does not significantly affect GV in patients with T2D.
碲标准溶液A: 称取0.1000 g单体碲(光谱纯99.9%)于100 mL烧杯中,加入10 mL硝酸,低温溶解,加4 mL硫酸(1+1)低温加热至恰好冒三氧化硫白烟,取下冷却,加硫酸(1+8)溶解,移入500 mL容量瓶中,用硫酸(1+8)定容。含碲为200 μg/mL。碲标准溶液B:吸取25 mL碲标准溶液A于100 mL容量瓶中,用硫酸(1+8)定容,此溶液含碲50 μg/mL;硫酸(1+1);盐酸(1+1);氢溴酸(1+1)-溴化钾(饱和):用氢溴酸(1+1)配制溴化钾的饱和溶液;亚铁氰化钾溶液:20 g/L。
Change in blood glucose level was another focus of our study. In the control group, group 1 and group 2, blood glucose level increased by < 2 mmol/L after carbohydrate loading. However, in patients receiving 300 mL of the carbohydrate drink (group 3), blood glucose levels increased by 3.4 mmol/L after 2 h. Studies have shown that a change in blood glucose level of < 2 mmol/L after carbohydrate loading does not increase perioperative complications[12,27,28]. Therefore, our results support a preoperative carbohydrate loading of < 200 mL in patients with T2D, although the optimal time for preoperative carbohydrate loading remains unaddressed. Carbohydrate loading 3 h before surgery does not pose a risk for hyperglycemia or aspiration in diabetic patients[12,20]. However, some researchers do not recommend the 2-h interval between carbohydrate loading and surgery due to concerns of delayed gastric emptying[29]. In our study, carbohydrate loading 2 h before anesthesia induction did not affect GV or increase the risk of reflux and aspiration. Future studies are warranted to confirm our results.
Our study has certain limitations. First, the blood glucose level of the enrolled patients was well controlled, and their preoperative FPG was < 10 mmol/L. Further stratified analysis must be performed in patients with different levels of blood glucose and HbA1c. Second, data about primary diseases in our patients were lacking. Because primary diseases may affect GV and gastric emptying, the lack of suchdata could have introduced a bias in result interpretation. Finally, single-center study design and insufficient data limit further application of our results. Prospective, large-scale, randomized, and multicentered studies are needed to further validate our results.


CONCLUSlON
GV was assessed at 3 different time points as described above. Gastric content was first evaluated using the Perlas A scale. No difference was observed in patients with Perlas grade II at T0 and T2 among the groups (
> 0.05). GV/W was increased significantly at T1 in groups 1, 2, and 3. At T2, GV/W decreased significantly, with no statistical difference observed between T0 and T2 in all the groups (
> 0.05)(Figure 3). Moreover, the number of patients with GV/W > 1.5 mL/kg was similar among the groups (
> 0.05) (Figure 3).
ARTlCLE HlGHLlGHTS

FOOTNOTES
2.3 NDM酶 NDM属于B类金属酶类,多见于ST14型的肺炎克雷伯菌携带。2008年从一名在印度接受治疗的瑞典患者的样本中检出,此后NDM在全球范围内迅速传播,目前发现的NDM亚型共16种,以NDM-1流行最为广泛。
Natural Science Foundation of Fujian Province, No. 2019J01587.
The present study was approved by the Ethics Committee of Putian College Affiliated Hospital, No. 201936.
This study is registered at the Chinese Clinical trial registry, No.ChiCTR1900028529.
The risk of reflux and aspiration was further evaluated using Perlas grading determined by ultrasonography. Patients with Perlas grade I had < 100 mL gastric content, whereas those with grade II had obvious gastric content in both supine and RLD positions[23]. Moreover, GV/W > 1.5 mL/kg helps determine the risk of reflux and aspiration[24-26]. In our study, the number of patients with Perlas grade II and GV/W > 1.5 mL/kg did not differ among the groups. This finding further confirms that preoperative carbohydrate loading does not increase the risk of reflux and aspiration in patients with T2D. However, it should be noted that all our groups had patients with Perlas grade II and GV/W > 1.5 mL/kg. This indicates the importance of performing routine preoperative GV ultrasonography in patients with diabetes.
All study participants or their legal guardian provided informed written consent about personal and medical data collection prior to study enrolment.
The authors declare that they have no competing interests.
不断加强与气象部门的会商和信息共享工作,国土资源部门向气象部门提供隐患点名称及区域分布、群测群防体系通讯录等相关资料,气象部门向我们提供全年气候趋势预测、重要天气消息、专题气象汇报、降水实况、区域站点降水统计、一周天气预报、每日天气预报等较详尽的气象资料,为强降雨期间指挥、调度全市地质灾害防范工作了提供科学的依据。有的县市还通过“村村响”喇叭或自行编制风险预警短信发送至各乡镇、村及各隐患点监测员,通知各级及时开展防范工作,从而切实打通地质灾害风险预警最后一公里的问题。2.2.4制度建设是保障
The datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
The authors have read the CONSORT 2010 Statement, and the manuscript was prepared and revised according to the CONSORT 2010 Statement.
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
本研究采用 UPLC-MS/MS 法同时测定慢性不可预见性温和应激模型大鼠脑脊液样品中 5-羟色胺和 5-HIAA 的浓度,该方法简单、快速,可用于脑脊液中 5-羟色胺和 5-HIAA 的含量测定。
China
步骤3:考察属性aj中的每一个候选断点Caj的存在性,即把原始决策表中与Caj相邻的2个属性值中的较小值改成较大值。如果此时的决策表不会产生冲突,那么把Caj从断点集中去除;否则,还原已修改的属性值。
Xin-Qiang Lin 0000-0001-6568-9433; Yu-Ren Chen 0000-0002-5074-4329; Xiao Chen 0000-0001-8220-0599; Yu-Ping Cai 0000-0001-6254-3332; Jian-Xin Lin 0000-0002-1699-6418; De-Ming Xu 0000-0002-6531-6124; Xiao-Chun Zheng 0000-0002-6213-0789.
Fan JR
A
Fan JR
1 Amer MA, Smith MD, Herbison GP, Plank LD, McCall JL. Network meta-analysis of the effect of preoperative carbohydrate loading on recovery after elective surgery.
2017 ; 104 : 187 -197 [PMID: 28000931 DOI:10 .1002 /bjs.10408 ]
2 Ljungqvist O, de Boer HD, Balfour A, Fawcett WJ, Lobo DN, Nelson G, Scott MJ, Wainwright TW, Demartines N.Opportunities and Challenges for the Next Phase of Enhanced Recovery After Surgery: A Review.
2021 ; 156 :775 -784 [PMID: 33881466 DOI: 10 .1001 /jamasurg.2021 .0586 ]
3 Wang S, Gao PF, Guo X, Xu Q, Zhang YF, Wang GQ, Lin JY. Effect of low-concentration carbohydrate on patientcentered quality of recovery in patients undergoing thyroidectomy: a prospective randomized trial.
2021 ;21 : 103 [PMID: 33823815 DOI: 10 .1186 /s12871 -021 -01323 -8 ]
4 Li L, Wang Z, Ying X, Tian J, Sun T, Yi K, Zhang P, Jing Z, Yang K. Preoperative carbohydrate loading for elective surgery: a systematic review and meta-analysis.
2012 ; 42 : 613 -624 [PMID: 22581289 DOI:10 .1007 /s00595 -012 -0188 -7 ]
5 Tsutsumi R, Kakuta N, Kadota T, Oyama T, Kume K, Hamaguchi E, Niki N, Tanaka K, Tsutsumi YM. Effects of oral carbohydrate with amino acid solution on the metabolic status of patients in the preoperative period: a randomized,prospective clinical trial.
2016 ; 30 : 842 -849 [PMID: 27438627 DOI: 10 .1007 /s00540 -016 -2217 -y]
6 Bi Y, Xu Y, Ning G. Prevalence of diabetes in Chinese adults--reply. JAMA 2014 ; 311 : 200 -201 [PMID: 24399563 DOI:10 .1001 /jama.2013 .283143 ]
7 Albalawi Z, Laffin M, Gramlich L, Senior P, McAlister FA. Enhanced Recovery After Surgery (ERAS
) in Individuals with Diabetes: A Systematic Review.
2017 ; 41 : 1927 -1934 [PMID: 28321553 DOI:10 .1007 /s00268 -017 -3982 -y]
8 Darwiche G, Almér LO, Björgell O, Cederholm C, Nilsson P. Delayed gastric emptying rate in Type 1 diabetics with cardiac autonomic neuropathy.
2001 ; 15 : 128 -134 [PMID: 11358681 DOI:10 .1016 /s1056 -8727 (00 )00143 -4 ]
9 Watson LE, Phillips LK, Wu T, Bound MJ, Jones KL, Horowitz M, Rayner CK. Longitudinal evaluation of gastric emptying in type 2 diabetes. Diabetes Res Clin Pract 2019 ; 154 : 27 -34 [PMID: 31238060 DOI:10 .1016 /j.diabres.2019 .06 .010 ]
10 Horowitz M, O'Donovan D, Jones KL, Feinle C, Rayner CK, Samsom M. Gastric emptying in diabetes: clinical significance and treatment.
2002 ; 19 : 177 -194 [PMID: 11918620 DOI: 10 .1046 /j.1464 -5491 .2002 .00658 .x]
11 Horváth VJ, Izbéki F, Lengyel C, Kempler P, Várkonyi T. Diabetic gastroparesis: functional/morphologic background,diagnosis, and treatment options.
2014 ; 14 : 527 [PMID: 25005121 DOI: 10 .1007 /s11892 -014 -0527 -8 ]
12 Laffin MR, Li S, Brisebois R, Senior PA, Wang H. The Use of a Pre-operative Carbohydrate Drink in Patients with Diabetes Mellitus: A Prospective, Non-inferiority, Cohort Study.
2018 ; 42 : 1965 -1970 [PMID: 29282506 DOI: 10 .1007 /s00268 -017 -4413 -9 ]
13 Sabry R, Hasanin A, Refaat S, Abdel Raouf S, Abdallah AS, Helmy N. Evaluation of gastric residual volume in fasting diabetic patients using gastric ultrasound.
2019 ; 63 : 615 -619 [PMID: 30609007 DOI:10 .1111 /aas.13315 ]
14 Perlas A, Davis L, Khan M, Mitsakakis N, Chan VW. Gastric sonography in the fasted surgical patient: a prospective descriptive study.
2011 ; 113 : 93 -97 [PMID: 21596885 DOI: 10 .1213 /ANE.0 b013 e31821 b98 c0 ]
15 Van de Putte P, Perlas A. Ultrasound assessment of gastric content and volume. Br J Anaesth 2014 ; 113 : 12 -22 [PMID:24893784 DOI: 10 .1093 /bja/aeu151 ]
16 Tacken MCT, van Leest TAJ, van de Putte P, Keijzer C, Perlas A. Ultrasound assessment of gastric volumes of thick fluids: Validating a prediction model.
2021 ; 38 : 1223 -1229 [PMID: 33606419 DOI:10 .1097 /EJA.0000000000001465 ]
17 Kruisselbrink R, Arzola C, Jackson T, Okrainec A, Chan V, Perlas A. Ultrasound assessment of gastric volume in severely obese individuals: a validation study.
2017 ; 118 : 77 -82 [PMID: 28039244 DOI: 10 .1093 /bja/aew400 ]
18 Practice Guidelines for Preoperative Fasting and the Use of Pharmacologic Agents to Reduce the Risk of Pulmonary Aspiration: Application to Healthy Patients Undergoing Elective Procedures: An Updated Report by the American Society of Anesthesiologists Task Force on Preoperative Fasting and the Use of Pharmacologic Agents to Reduce the Risk of Pulmonary Aspiration.
2017 ; 126 : 376 -393 [PMID: 28045707 DOI: 10 .1097 /ALN.0000000000001452 ]
19 Smith I, Kranke P, Murat I, Smith A, O'Sullivan G, Søreide E, Spies C, in't Veld B; European Society of Anaesthesiology.Perioperative fasting in adults and children: guidelines from the European Society of Anaesthesiology.
2011 ; 28 : 556 -569 [PMID: 21712716 DOI: 10 .1097 /EJA.0 b013 e3283495 ba1 ]
20 Gustafsson UO, Nygren J, Thorell A, Soop M, Hellström PM, Ljungqvist O, Hagström-Toft E. Pre-operative carbohydrate loading may be used in type 2 diabetes patients. Acta Anaesthesiol Scand 2008 ; 52 : 946 -951 [PMID: 18331374 DOI:10 .1111 /j.1399 -6576 .2008 .01599 .x]
21 He XD, Guo YM, Goyal RK. Effect of Hyperglycemia on Purinergic and Nitrergic Inhibitory Neuromuscular Transmission in the Antrum of the Stomach: Implications for Fast Gastric Emptying.
2018 ; 5 : 1 [PMID: 29410956 DOI: 10 .3389 /fmed.2018 .00001 ]
22 Halland M, Bharucha AE. Relationship Between Control of Glycemia and Gastric Emptying Disturbances in Diabetes Mellitus.
2016 ; 14 : 929 -936 [PMID: 26717862 DOI: 10 .1016 /j.cgh.2015 .11 .021 ]
23 Perlas A, Mitsakakis N, Liu L, Cino M, Haldipur N, Davis L, Cubillos J, Chan V. Validation of a mathematical model for ultrasound assessment of gastric volume by gastroscopic examination.
2013 ; 116 : 357 -363 [PMID: 23302981 DOI: 10 .1213 /ANE.0 b013 e318274 fc19 ]
24 Chang JE, Kim H, Won D, Lee JM, Jung JY, Min SW, Hwang JY. Ultrasound assessment of gastric content in fasted patients before elective laparoscopic cholecystectomy: a prospective observational single-cohort study.
2020 ; 67 : 810 -816 [PMID: 32314262 DOI: 10 .1007 /s12630 -020 -01668 -7 ]
25 Ohashi Y, Walker JC, Zhang F, Prindiville FE, Hanrahan JP, Mendelson R, Corcoran T. Preoperative gastric residual volumes in fasted patients measured by bedside ultrasound: a prospective observational study.
2018 ; 46 : 608 -613 [PMID: 30447671 DOI: 10 .1177 /0310057 X1804600612 ]
26 Van de Putte P, Vernieuwe L, Bouvet L. Gastric ultrasound as an aspiration risk assessment tool. Indian J Anaesth 2019 ;63 : 160 -161 [PMID: 30814762 DOI: 10 .4103 /ija.IJA_756 _18 ]
27 Tang X, Li S, Wang Y, Wang M, Yin Q, Mu P, Lin S, Qian X, Ye X, Chen Y. Glycemic variability evaluated by continuous glucose monitoring system is associated with the 10 -y cardiovascular risk of diabetic patients with wellcontrolled HbA1 c. Clin Chim Acta 2016 ; 461 : 146 -150 [PMID: 27502250 DOI: 10 .1016 /j.cca.2016 .08 .004 ]
28 Voss AC, Maki KC, Garvey WT, Hustead DS, Alish C, Fix B, Mustad VA. Effect of two carbohydrate-modified tubefeeding formulas on metabolic responses in patients with type 2 diabetes. Nutrition 2008 ; 24 : 990 -997 [PMID: 18718737 DOI: 10 .1016 /j.nut.2008 .06 .009 ]
29 Chen L, Chen YJ, Dong HL, Feng Y, Gu XP, Huang YG, Jiang ZW, Lou WH, Liu LX, Mi WD, Ma ZL, Min S, Peng SL,Tian XD, Wang TL, Xu ZK, Xue ZG, Yao HW, Yang YM, Zhang KC, Zhu SM. Chinese expert consensus and pathway management guide for Chinese accelerated rehabilitation surgery (2018 Edition). Zhongguo Shiyong Waike Zazhi 2018 ; 38 :1 -19 [DOI: 10 .19538 /j.cjps.issn1005 -2208 .2018 .01 .01 ]
猜你喜欢
杂志排行
World Journal of Clinical Cases的其它文章
- Diabetes mellitus susceptibility with varied diseased phenotypes and its comparison with phenome interactome networks
- Sequential chemotherapy and icotinib as first-line treatment for advanced epidermal growth factor receptor-mutated non-small cell lung cancer
- Disseminated strongyloidiasis in a patient with rheumatoid arthritis: A case report
- CYP27A1 mutation in a case of cerebrotendinous xanthomatosis: A case report
- Postoperative multiple metastasis of clear cell sarcoma-like tumor of the gastrointestinal tract in adolescent: A case report
- Efficacy and safety of adalimumab in comparison to infliximab for Crohn's disease: A systematic review and meta-analysis
