Clinical study on warm needling moxibustion plus isokinetic muscle strength training in treating knee osteoarthritis
2022-06-23CHENWei陈玮LIJing李璟LIUGuizhen刘桂珍
CHEN Wei (陈玮), LI Jing (李璟), LIU Guizhen (刘桂珍)
1 Putuo Hospital, Shanghai University of Traditional Chinese Medicine, Shanghai 200062, China
2 Yueyang Hospital of Integrated Traditional Chinese and Western Medicine, Shanghai University of Traditional Chinese Medicine,Shanghai 200437, China
Abstract
Keywords: Acupuncture Therapy; Warm Needling Therapy; Osteoarthritis, Knee; Muscle Strength; Visual Analog Scale; Pain Measurement; Coagulated Cold Due to Yang Deficiency
Knee osteoarthritis (KOA) has a high clinical incidence and mainly manifests as pain and dysfunction[1].Epidemiological studies have shown that the prevalence of KOA in China is about 21.5%[2], and it increases significantly with aging. The prevalence of KOA in people over 55 years old is about 88.0%, and the disability rate is about 53.0%[3], making it rank as the second most common disabling disease in the world[4].
KOA falls under the category of “bone Bi-Impediment” in traditional Chinese medicine. The symptoms of senile KOA are recurrent and lingering unhealed. The etiology and pathogenesis of KOA are still unclear, but mechanical, biological, and other factors are believed to play a role[5]. With the deepening of the study, the influence of mechanical factors on KOA has drawn more and more attention. Research has shown that isokinetic muscle strength training can improve the muscle function of the patients[6]. Warm needling moxibustion therapy has a certain effect on KOA. A meta-analysis showed that compared with oral Western medicine and placebo acupuncture, warm needling moxibustion had certain advantages in treating KOA[7].In this study, we observed the clinical efficacy of warm needling moxibustion, isokinetic muscle strength training, and the combination of the two treatments for senile KOA, so as to explore the optimal treatment.
1 Clinical Materials
1.1 Diagnostic criteria
This study referred to theGuidelines for Diagnosis and Treatment of Osteoarthritismade by the Orthopaedic Branch of the Chinese Medical Association in 2007[8].
1.2 Inclusion criteria
Those who met the above diagnostic criteria; met the syndrome differentiation criteria of Yang deficiency and coagulated cold syndrome in Chinese medicine[9]: pain and heaviness in the joint, with unsmooth flexionextension movement, mild during daytime and severe during the night, aggravated while got cold and eased after got warm, a pale tongue with white coating, and deep, thready, and moderate pulse as the main manifestations; Western Ontario and McMaster Universities osteoarthritis index (WOMAC)score ≤120 points[10]; visual analog scale (VAS) of the knee joint after 50 m walk was 3-8 points[11]; aged 50-75 years old; had no other therapy or relevant medication in the past one month.
1.3 Exclusion criteria
Those with severe varus or valgus deformity of the knee joint; imaging examination showed a large number of osteophytes, severe subchondral osteosclerosis;those with severe knee soft tissue adhesion; those with knee joint fractures, tendon ruptures, or open injuries.
1.4 Elimination, dropout, and discontinuation criteria
Those with poor compliance; those who voluntarily asked to withdraw; those who lost to follow-up; those who showed adverse reactions during treatment.
1.5 Statistical methods
All data were statistically analyzed by the SPSS version 20.0 statistical software. Measurement data in normal distribution were expressed as mean ± standard deviation (±s). Pairedt-test was applied to the intra-group comparisons. Analysis of variance and least significant difference (LSD)t-test was used for comparisons between multiple groups. If data did not meet the normal distribution or homogeneous variance,a non-parametric test was applied. Counting data were analyzed by Chi-square test. Inspection levelα=0.05.P<0.05 was considered to indicate a statistically significant difference.
1.6 General data
A total of 135 KOA patients were enrolled in the Rehabilitation Department of Putuo Hospital, Shanghai University of Traditional Chinese Medicine, between June 2019 and June 2021. All patients were randomly divided into a warm needling moxibustion group, an isokinetic muscle strength training group, and a combined group by the random number table method,with 45 cases in each group. During the trial, three patients in the warm needling moxibustion group dropped out, five cases in the isokinetic muscle strength training group dropped out, and five cases in the combined group dropped out. A total of 122 patients finished the study. There were no statistically significant differences in gender, age, or duration of disease among the three groups (P>0.05), indicating that the three groups were comparable (Table 1).

Group n Gender (case) Average age(Male Female images/BZ_7_1311_2835_1350_2881.png±s, year)Average duration(images/BZ_7_1311_2835_1350_2881.png±s, month)Warm needling moxibustion 42 9 33 62.6±6.3 42.0±19.5 Isokinetic muscle strength training 40 8 32 60.8±6.3 41.8±20.8 Combined 40 10 30 62.8±6.7 42.2±20.7
2 Treatment Methods
2.1 Warm needling moxibustion group
Points: Neixiyan (EX-LE4), Dubi (ST35), Xuehai(SP10), Liangqiu (ST34), Yanglingquan (GB34), Zusanli(ST36), and Ashi points[12].
Methods:The patient took a sitting position. The physician perpendicularly or obliquely punctured the points by 20-25 mm in depth with disposable sterile acupuncture needles of 0.40 mm in diameter and 40 mm in length. After the arrival of Qi (Deqi), even reinforcing-reducing manipulation was performed. Then,the physician put a moxa stick (about 17 mm in diameter and 20 mm in length) on the end of the needle handle at Neixiyan (EX-LE4), Dubi (ST35), Xuehai(SP10), Liangqiu (ST34), and Zusanli (ST36), and ignited it. Replaced with a new moxa stick after the old one burnt out, three moxa sticks for each point each time.The treatment was performed 3 times a week, 12 times as a course of treatment, for 2 courses in total.
2.2 Isokinetic muscle strength training group
Patients in this group were treated with isokinetic muscle strength training using the American BIODEX850-000 multi-joint isokinetic testing and training system.
Methods:The patient took a sitting position, with the knee flexed, and the waist, chest, thigh, and calf fixed to avoid movement of the body and compensation of other muscle groups during the training. Multi-angular velocity isokinetic centripetal strength training was performed within the maximum tolerable flexion and extension ranges of the patient’s knee joint. Each angular velocity isokinetic flexion and extension took 10 times as a group, and the training was repeated for three groups each time. A total of 10 angular velocities were performed.
2.3 Combined group
The combined group was treated with warm needling moxibustion plus isokinetic muscle strength training.The warm needling moxibustion was performed first.After 5-10 min rest of the lower limbs, the isokinetic muscle strength training was then performed. The methods and points used were the same as those in the above two groups.
3 Efficacy Observation
3.1 Observation items
3.1.1 WOMAC score
The knee joint function of the patients was evaluated from three aspects: pain, stiffness, and joint function.There are 24 sub-items, making a total score of 240 points. The higher the score, the more serious the condition.
3.1.2 VAS score
VAS score was used to evaluate the degree of pain.The highest score of VAS is 10 points, and the lowest score is 0 point. The higher the score, the severer the pain.
3.1.3 Peak torque (PT), total work (TW) and average power (AP) of quadriceps femoris
The PT, TW, and AP of the quadriceps femoris of the affected knee were measured by the American BIODEX850-000 multi-joint isokinetic testing and training system to evaluate the muscle strength of the quadriceps femoris.
3.2 Criteria of clinical efficacy
The criteria of clinical efficacy in this study were established according to theGuiding Principles for Clinical Study of New Chinese Medicines[13].
Clinically controlled: Clinical symptoms disappeared,and the joint movements were normal.
Markedly effective: Clinical symptoms disappeared or significantly improved, and the joint movement was not limited.
Effective: Clinical symptoms basically disappeared,and the joint movement was slightly limited.
Invalid: Clinical symptoms and activities were not significantly improved.
3.3 Results
3.3.1 Comparison of the curative efficacy
After treatment, the differences in the curative efficacy among the three groups were statistically significant (P<0.05). The curative effect of the combined group was the best, followed by the warm needling moxibustion group, and the isokinetic muscle strength training group was relatively poor (Table 2).
3.3.2 Comparison of the WOMAC score
After treatment, the WOMAC scores of pain, stiffness,and function and the total score in the three groups all decreased, and the intra-group differences were statistically significant (P<0.05). There were statistical differences in the scores among the three groups(P<0.05). The total WOMAC score and the score of stiffness in the combined group were lower than those in the warm needling moxibustion group and the isokinetic muscle strength training group (P<0.05), and these two scores in the warm needling moxibustion group were lower than those in the isokinetic muscle strength training group (P<0.05). After treatment, there was no statistical difference in the WOMAC score of pain between the warm needling moxibustion group and the combined group (P>0.05), while the pain scores in the warm needling moxibustion group and the combined group were lower than that in the isokinetic muscle strength training group (P<0.05). The WOMAC score of function in the combined group was lower than that in the warm needling moxibustion group and the isokinetic muscle strength training group (P<0.05), while there was no statistical difference in the score between the warm needling moxibustion group and the isokinetic muscle strength training group (P>0.05),(Table 3).
3.3.3 Comparison of the VAS score
After treatment, VAS scores in the three groups all decreased, and the intra-group differences were statistically significant (P<0.05). There were statistical differences in the VAS score among the three groups(P<0.05). The VAS scores in both the warm needling moxibustion group and the combined group were lower than that in the isokinetic muscle strength training group (P<0.05). There was no statistical difference between the warm needling moxibustion group and the combined group (P>0.05), (Table 4).
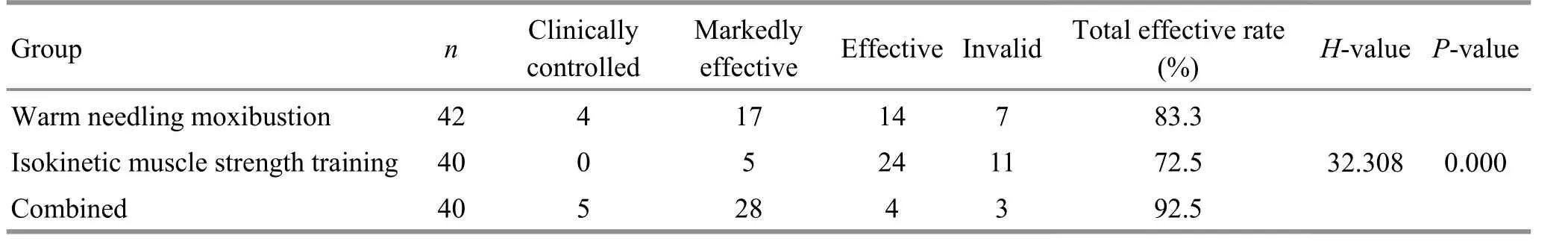
Total effective rate(%) H-value P-value 83.3 72.5 92.5 32.308 0.000

Group n Time Pain Stiffness Function Total score Warm needling moxibustion 42 Before treatment 19.29±6.52 7.90±2.99 55.74±11.11 83.00±18.10 After treatment 8.29±3.901)2) 3.67±1.881)2) 31.02±12.791) 42.93±17.171)2)Isokinetic muscle strength training 40 Before treatment 19.43±6.14 8.65±3.13 56.18±11.33 84.35±18.26 After treatment 14.20±5.411) 5.70±2.221) 34.18±9.301) 54.08±14.881)Combined 40 Before treatment 20.55±5.13 7.88±3.20 54.80±9.38 83.23±16.04 After treatment 8.00±4.091)2) 2.40±1.461)2)3) 23.15±9.991)2)3) 33.55±13.281)2)3)

Group n Before treatment After treatment Warm needling moxibustion 42 5.07±1.22 2.05±1.061)2)Isokinetic muscle strength training 40 5.08±1.33 2.95±1.451)Combined 40 4.98±1.27 1.65±1.051)2)
3.3.4 Comparison of PT, TW, and AP
After treatment, PT, TW, and AP in the three groups were all improved, and the intra-group differences were statistically significant (P<0.05). There were statistical differences among the three groups (P<0.05). PT, TW,and AP in the combined group were higher than those in both the warm needling moxibustion group and the isokinetic muscle strength training group (P<0.05), and those in the isokinetic muscle strength training group were higher than those in the warm needling moxibustion group (P<0.05), (Table 5).
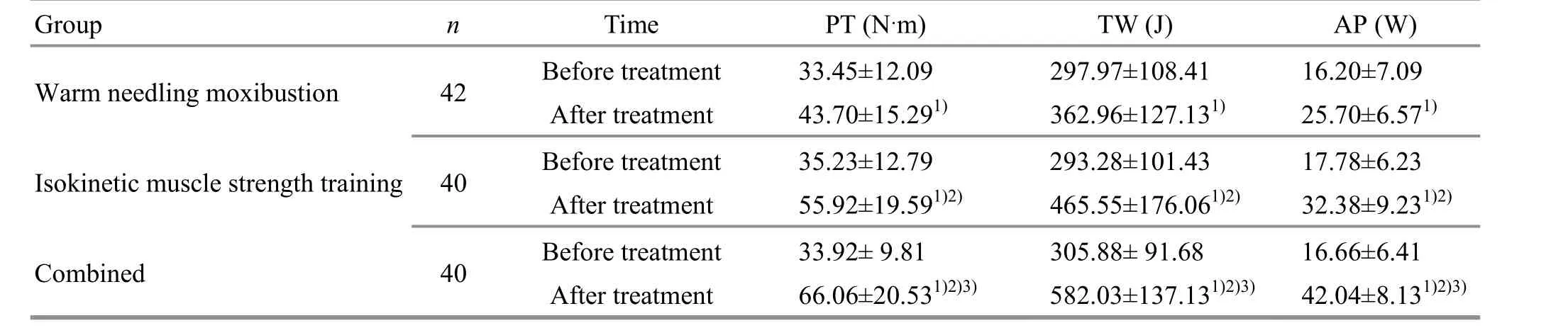
Group n Time PT (N·m) TW (J) AP (W)Warm needling moxibustion 42 Before treatment 33.45±12.09 297.97±108.41 16.20±7.09 After treatment 43.70±15.291) 362.96±127.131) 25.70±6.571)Isokinetic muscle strength training 40 Before treatment 35.23±12.79 293.28±101.43 17.78±6.23 After treatment 55.92±19.591)2) 465.55±176.061)2) 32.38±9.231)2)Combined 40 Before treatment 33.92± 9.81 305.88± 91.68 16.66±6.41 After treatment 66.06±20.531)2)3) 582.03±137.131)2)3) 42.04±8.131)2)3)
4 Discussion
Chinese medicine believes that KOA is a condition due to deficient root cause and presents with excess symptoms, and the lack of healthy Qi is the internal cause of the disease. “Liver dominates tendon, and kidney dominates bone”. Due to the gradual waning of the liver and kidney in older adults, their tendons and bones cannot get enough nutrition and thus are not strong, plus the invasion of pathogenic wind-colddampness, subsequently arising KOA[14-15]. The elderly people are insufficient in the healthy Qi and have a poor defense-exterior, which causes the stagnation of pathogenic Qi blocking the meridians, resulting in the disease lingering unhealed. Among them, the syndrome of Yang deficiency and coagulated cold is the most common syndrome[16-17].
In recent years, many studies have found that the muscle strength around the knee joint is generally weak in the elderly[18], and KOA pain is closely related to the decrease of muscle strength around the knee joint[19].There is an inseparable relationship between pain,muscle weakness, and KOA. The muscles around the joints play an important role in participating in the absorption of stress, alleviating the impact force on the knee joint during exercise, and maintaining the stability of the joint[6], especially the quadriceps femoris, which is an important structure for the stability of the knee joint. The weakness of the quadriceps femoris promotes KOA progression and is proportional to pain[20].
KOA inflammatory pain can induce muscle weakness[21]. On the one hand, pain can transmit signals through the anterior horn cells, resulting in protective inhibition. This special form of muscle inhibition is called arthrogenous muscle inhibition[22]. On the other hand, the pain will cause patients to avoid activities subjectively, and over time will cause disuse atrophy of the muscle groups[23]. The decrease of muscle strength around the knee can lead to stress imbalance on the articular surface, aggravate the wear and damage of the surrounding tissues, promote the occurrence of osteoarthritis, and aggravate KOA[24-25]. Therefore, the occurrence and development of pain-muscle weakness-KOA form a vicious cycle. These factors are related to each other and affect the course of the disease and are also the key to the recurrence of KOA[26].
KOA due to Yang deficiency and coagulated cold is mainly characterized by cold pain, heaviness, and stiffness of the joint, and unsmooth flexion-extension movement. It is often recurrent and lingering unhealed and aggravated by cold. Warm needling moxibustion combines the effect of acupuncture with the warm stimulation of moxibustion. It can not only play the effect of promoting blood circulation, unblocking collaterals, and relieving pain, but also has the effect of warming Yang and dispelling cold, and nourishing the liver and kidney. Warm needling moxibustion has the effects of improving circulation, relieving venous stasis,increasing cartilage nutrition supply, and accelerating the removal of pathological products in the local tissues around the joints. It can regulate the expression of various osteoarthritis-related inflammatory factors,inhibit inflammatory responses, regulate the metabolic balance of chondrocytes, and promote the repair of chondrocytes. It also can regulate the levels of pain mediators and exert analgesic effects[27-29]. ZHANG Y L,et al[30]found that the destruction of the articular bone of rats in the warm needling moxibustion group was better improved than that in the medication group,which indicated that warm needling moxibustion could effectively promote the repair of articular cartilage. YUE P,et al[31]found that warm needling moxibustion could effectively treat KOA in rabbits, and reduce the levels of tumor necrosis factor (TNF)-α and matrix metalloproteinase (MMP)-3 in the articular cartilage,playing an anti-inflammatory role. WANG Q,et al[32]found that warm needling moxibustion could reduce the serum C-reaction protein, TNF-α, and interleukin-1β levels. JIANG R,et al[33]held that the anti-inflammatory mechanism of warm needling moxibustion in treating KOA rats might be associated with the inhibition of the expression of a disintegrin and metalloproteinase with thrombospondin motifs-4 and MMP-3. CHEN Y D,et al[34]found that acupuncture, warm needling moxibustion, and electroacupuncture could delay cartilage degeneration in the treatment of KOA, among which warm needling moxibustion had obvious advantages. Several clinical studies have found that warm needling moxibustion has a better curative effect than acupuncture alone in the treatment of KOA[35-36].
In the previous clinical practice, we found that warm needling moxibustion treatment of KOA had a good pain-relief effect, but the improvement of function was not satisfactory, which was related to the pathogenesis of this disease. In the elderly, the liver and kidney are waning, the tendons and bones are gradually getting weak, and the muscle strength is generally poor,resulting in slow functional recovery after the onset of KOA. Isokinetic muscle strength training is a new movement mode and the best muscle strength training method at present[23]. It requires specific equipment to complete. The severity of KOA is negatively correlated with knee muscle strength[37]. During the process of isokinetic muscle strength training, the blood vessels in the muscle continuously expand and contract with the contraction of the muscles, which can increase muscle nutrition, effectively prevent muscle atrophy, and improve muscle strength. Meanwhile, the agonist and antagonistic muscles are exercised at the same time,which is conducive to enhancing the stability of the joint,reducing the wear of the tissues around the joint, and reducing algogenic factors such as inflammatory responses, thereby controlling the progression of the disease. ZUO T T,et al[38]found that intra-articular injection of sodium hyaluronate combined with isokinetic muscle strength training had a synergistic effect in relieving pain, enhancing knee muscle strength,and promoting joint function recovery. CHEN D[39]pointed out in the study that the isokinetic muscle strength training combined with joint mobilization had a good effect on pain and muscle strength in KOA.Through meta-analysis, some researchers found that compared with isometric and isotonic training,isokinetic training had more significant effects on muscle strength and pain and showed advantages of safety, efficiency, and accuracy[40].
Due to the unclear mechanism of KOA, Western medications and surgery have considerable side effects and limitations and cannot effectively block the progression of the disease. Relevant guideline clearly points out that improving or restoring joint function and improving the quality of life are the ultimate goals of KOA treatment[8]. Several foreign guidelines have recommended acupuncture or muscle strength training for the treatment of KOA[41-42].
In this study, elderly patients with KOA due to Yang deficiency and coagulated cold were taken as the subjects, and it was the exploration of acupuncture and moxibustion combined with exercise in the treatment of KOA. Results of this study showed that the total effective rate of the combined group was significantly higher than that of the warm needling moxibustion group and the isokinetic muscle strength training group.The total efficacy and scores of each KOA symptom and joint function were all superior in the combined group to the single therapy group, indicating that the warm needling moxibustion and the isokinetic muscle strength training together played a synergistic effect.The combination of these two treatments can enhance muscle strength and increase the stability of the knee joint, thereby blocking the vicious cycle of KOA and controlling the process of the disease. After treatment,the daily activity function of the patients was significantly improved and the quality of life was enhanced, which was consistent with the ultimate goal of KOA treatment proposed by the Orthopaedic Branch of the Chinese Medical Association[8]. Therefore, it is worth promoting this combined treatment.
Conflict of Interest
The authors declare that there is no potential conflict of interest in this article.
Acknowledgments
This work was supported by the Three-year Development Project for Traditional Chinese Medicine of Shanghai [上海市进一步加快中医药事业发展三年行动计划项目, No. ZY(2018-2020)-FWTX-8010]; Key Clinical Specialty Construction Project in Putuo District of Shanghai (上海市普陀区中医临床重点专科建设项目,No. ptzyzk2110).
Statement of Informed Consent
Informed consent was obtained from all individual participants.
Received: 18 October 2021/Accepted: 1 December 2021
猜你喜欢
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Meta-analysis of acupuncture intervening exercise-induced fatigue
- Clinical efficacy of electroacupuncture in controlling myopia in children and its influence on retinal blood flow
- Clinical efficacy of Tuina manipulations for lumbar disc herniation and its influence on posture-associated indicators
- Clinical study of warm needling moxibustion plus intra-articular injection of sodium hyaluronate for hip involvement in ankylosing spondylitis
- Clinical study of warm needling moxibustion combined with entecavir in the treatment of compensated cirrhosis due to chronic hepatitis B
- Clinical observation on moxibustion at Baihui (GV20)plus Tuina for children with postnasal drip syndrome