Late contralateral recurrence of retinal detachment in incontinentia pigmenti:A case report
2022-06-23YouRanCaiYongLiangXinZhong
lNTRODUCTlON
Incontinentia pigmenti(IP),also known as Bloch-Sulzberger syndrome,is a rare X-linked genetic disorder(OMIM: 308,300).It occurs due to a mutation in the
gene,which is located on the Xchromosome at position q28.The prevalence of IP may vary according to sex and geographical location.It usually occurs in female individuals,as it is typically lethal at the embryonic stage in males,owing to X inactivation mosaicism,although the proportion of male patients reported to survive past birth in East Asia was higher than that in other areas[1].The incidence of IP is 0.7
100000 individuals[2].
Skin lesions are the main presentation in patients with IP.Patients usually exhibit stereotypical skin lesions during infancy and early childhood.These first present as a blistering maculopapular lesion that develops into a whorled pigmented lesion in four stages[3].IP is usually accompanied by lesions in ectodermal tissues including the skin,eyes,teeth,bones,and central nervous system.Manifestations in the central nervous system can lead to severe disability[4].
The ocular manifestations in patients with IP are diverse and involve the retina,lens,vitreous humor,optic nerve,and other structures;7%-23% of patients experience blindness in at least one eye,mainly due to retinal vascular abnormalities,retinal pigment epithelial lesions,and retinal detachment(RD)[5].Here,we present an atypical case of both eyes presenting sequentially with tractional RD in a girl with IP,as shown by an unreported code-shifting variant in East Asian populations.
CASE PRESENTATlON
Chief complaints
An 11-year-old Chinese girl presented to our outpatient clinic with sudden blurred vision in the left eye that occurred 7 d before her visit.
History of present illness
Four days before presentation at our hospital,the patient visited a local hospital with the same complaint.She was diagnosed with bilateral RD and advised to visit a higher-level hospital.The patient had no other discomfort except for blurred vision.
History of past illness
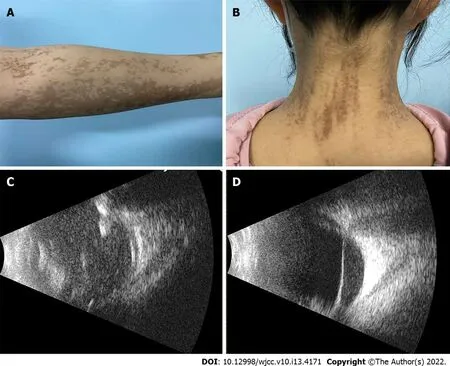
She had experienced blisters of varying dimensions on her trunk and limbs from the first postnatal week,followed by rupture and crusting of the blisters and streaks of pigmentation on the extremities(Figure 1A)and back of her neck(Figure 1B).In infancy,the patient visited a dermatologist and was diagnosed with IP.Her right eye was previously diagnosed with RD in our hospital in 2017,but the treatment window was missed.
Personal and family history
No standard recommendations for ophthalmic screening or IP follow-up are currently available.Holmstrom and Thoren proposed that examinations of the eyes should be performed as soon as possible after birth,at least once a month for 3-4 mo,and the frequency of examinations should be increased in children with ocular pathologies.If no abnormalities are found by the age of 3 years,follow-up may be discontinued.Our patient was from a rural area where financial factors and poor medical provision made it difficult for her to have regular scheduled follow-up visits.Due to the lack of previous examination data,it is difficult to determine whether retinal abnormalities were present before 3 years of age.As eye abnormalities persist throughout the life of patients with IP,those who develop retinal abnormalities are followed-up for life.In addition,for patients with retinal abnormalities in one eye,we should increase the frequency of follow-up and pay more attention to fundus changes in the other unaffected eye.
Physical examination
At initial examination,her visual acuity was assessed as no perception of light in the right eye and able to count fingers with the left eye,with no improvement with correction.Intraocular pressure in both eyes was 16 mmHg.Slit-lamp examination of the anterior chamber revealed a cloudy lens in the right eye,and vitreous turbidity,elevated retinal folds,massive proliferation of membranes,exudates,and hemorrhages in the left eye.
IP is a rare X-linked genetic skin disease that also causes neurological,ophthalmological,hair,nail,and teeth problems.Nearly 100% of IP patients have skin lesions,30% have neurologic presentations,54%-80% have dental problems,and 25%-77% have ocular diseases[1].Although ophthalmological lesions are not the most common,ocular involvement persists in patients throughout their lifetime and affects their quality of life.The most characteristic and most serious injuries are retinal injuries.RD is often difficult to repair surgically and is the leading cause of blindness.Current reports on the ocular condition of patients with IP are mostly of infants who developed retinal changes,with few reports of patients who developed bilateral RD.In this case,the girl belonged to a rural area,and her eye examinations were conducted only intermittently after birth,owing to geographic and economic considerations.However,she did not experience any eye discomfort until she was 7 years old.She presented to a hospital with a 7-d history of vision loss.The right eye was lost to surgery at that time;fortunately,the left eye still had a chance to recover good eyesight.
Laboratory examinations
The authors declare that there are no conflicts of interest.
They all went abroad, but Little Thumb never told his brothers one syllable8 of what he knew. They went into a very thick forest, where they could not another at ten paces distance. The fagot-maker began to cut wood, and the children to gather up the sticks to make fagots. Their father and mother, seeing them busy at their work, got away from them insensibly, and ran away from them all at once, along a by-way through the winding9 bushes.
Imaging examinations
Ultrasound of the eye revealed clouded refractive media and extensive RD in the right eye(Figure 1C)and suspected RD in the left eye(Figure 1D).Dilated fundus examination revealed a patchy maculacolored exudate and hemorrhage with greenish-gray bulging of the peripheral retina in the left eye(Figure 2A).Fundus fluorescence angiography(FFA)revealed temporal and inferior temporal vascular occlusion,and retinal vascular endings and optic disc surface capillaries were dilated with enhanced permeability.An area without perfusion was observed in the left eye(Figure 2B).
Exons 4 to 10 of the
gene are a mutational hot spot,with deletions being particularly common[10].In the genomic testing of our patient's peripheral blood sample,there was a shift variant in exon 5 of
.A mutation in the
gene in intron 4 has been reported in one patient[11].However,the patient reported previously only had central nervous system,hair,and dental issues.Our patient with IP is the first case with this mutation and ocular disease.This genetic abnormality was probably the cause of the disease in the girl.However,the significance of this variant cannot be confirmed because it has been rarely reported to date.

FlNAL DlAGNOSlS
The authors have read the CARE Checklist(2016),and the manuscript was prepared and revised according to the CARE Checklist(2016).
TREATMENT
We promptly performed vitrectomy,combined with intravitreal spherical gas injection in the left eye.In addition,a laser was used in the non-perfused area.
OUTCOME AND FOLLOW-UP
Two days after surgery,the patient’s symptoms,including visual acuity,RD,and hemorrhages significantly improved.Her visual acuity improved to 20/50,and optical coherence tomography(OCT)examination revealed retinal flattening(Figure 2C).After 1 mo,FFA revealed a non-perfused zone in the retinal periphery(Figure 2E).Fundus photography showed a resorbed hemorrhage and grayish exudate(Figure 2D).Therefore,we performed supplementary laser photocoagulation in the peripheral zone of the retina.Four months after surgery,the patient visited our hospital for further testing.Her visual acuity had improved to 20/32,and FFA showed lattice-like non-perfused areas in the peripheral retina.Macular OCT revealed retinal edema and exudation(Figure 2I)and non-perfused areas with hyperfluorescence,representing neovascularization and fluorescein infiltration,visible in the upper retina on FFA(Figure 2H).Additional retinal laser photocoagulation was performed in the left eye.During the short follow-up,the patient’s vison recovered well,the retina had flattened,and no new fundus lesions were observed.Lifelong ongoing follow-up is planned.
Theold man who was driving the oxen told them that in the lifetime of hisfather the horses had many a hard battle with the wild beasts thatwere now exterminated
DlSCUSSlON
I held out the chain. She took it in both her hands, reached forward, and secured the simple clasp at the back of my neck. She stepped back then as if to see that all was well. I looked down at the shiny piece of glass and the tarnished13 golden chain, then back at the giver. I meant it when I whispered, Oh, Maria, it is so beautiful. She would have loved it. Neither of us could stop the tears. She stumbled into my arms and we wept together. And for that brief moment I became her mother, for she had given me the greatest gift of all: herself.
The brothers were at once set at liberty, while Sir Red, for his wickedness, was hanged on the highest tree that could be found, and so he got the reward he deserved
IP is a genetic disease associated with many lesions at various sites,especially in the eyes.O'Doherty
[6]believed that ocular changes can be divided into four stages.The most severe outcome is RD.It is important to establish early treatment to prevent RD.Therefore,most current studies have been conducted on infants.Several studies have suggested that the prevention of RD is the most important aspect of ocular pathology in patients with IP.Early laser treatment is required when retinal neovascularization and areas of ischemia are present[7].The incidence of RD is approximately 20% and the functional prognosis is extremely poor[1,8].RD can be treated with vitrectomy or scleral buckling.For advanced lesions,it is difficult to achieve a good outcome even with surgical treatment[9].Our patient presented with RD;therefore,we performed vitrectomy combined with laser photocoagulation on her left eye with localized RD.The outcome,including visual acuity and fundus examination findings,was acceptable.This might be related to the fact that the patient visited the clinic at the very first appearance of eye symptoms.
Tracing her family history,her parents and her younger brother had no history of skin or ocular disease and were all born at full term.
There were soft rugs and cushions of all the colours of the rainbow, and beautiful carpets that looked like the finest moss5, and flowers and trees with curiously6 crooked7 branches, both green and yellow, white and red, and there were also little fountains which sprang up from the most beautiful snail-shells, and fell into bright mussel-shells, and at the same time made a most delightful music, which filled the whole palace
It is not as dear, said the old man, as the glove-cleaner, or life-cleaner, as I sometimes call it. No. That is five thousand dollars, never a penny less. One has to be older than you are, to indulge in that sort of thing. One has to save up for it.
CONCLUSlON
Asymmetric retinal changes in both eyes are typical ocular abnormalities in patients with IP.Surgery combined with laser therapy is an effective treatment for patients who develop early RD.This case highlights that,in patients who present with retinal abnormalities in one eye,more attention should be paid to potential abnormal changes in the other eye.In addition,genetic testing should be performed in patients with IP to learn more about the association of mutations with disease-related changes.
FOOTNOTES
Cai YR collected the case data and wrote the report;Liang Y treated the patient;Zhong X reviewed the literature and performed the preliminary revision of the article;all authors read and approved the final version to be published.
The participant in this study provided written informed consent prior to study enrollment.
Genome sequencing revealed a heterozygous shift in the
gene in the patient,a rare shift mutation in exon 5(c.519-3_519dup:p?)at chrX: 153,788,619-153,788,622.
A diagnosis of bilateral RD related to IP was confirmed based on the medical history,clinical signs,examinations,and intraoperative findings.
50. Iron door: Superstition90 has long credited iron with the power of driving away witches and evil spirits (Waring 1978). Locking the witch behind the oven s iron door perhaps prevents her from escaping. Return to place in story.
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial(CC BYNC 4.0)license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
China
And so it began on Wednesday some fifteen years ago: I bought a card and gave it to Patricia. There was no special occasion. The card was just an expression of how much I loved her and How much I was thinking about her. I picked Wednesday for no special reason other than it was the middle of the week.
You-Ran Cai 0000-0001-9326-1003;Yong Liang 0000-0002-7229-1578;Xin Zhong 0000-0002-5684-1816.
Li X
Webster JR
Li X
1 Swinney CC,Han DP,Karth PA.Incontinentia pigmenti:A Comprehensive Review and Update.
2015;46: 650-657[PMID: 26114846 DOI: 10.3928/23258160-20150610-09]
2 Cammarata-Scalisi F,Fusco F,Ursini MV.Incontinentia Pigmenti.
2019;110: 273-278[PMID: 30660327 DOI: 10.1016/j.ad.2018.10.004]
3 Landy SJ,Donnai D.Incontinentia pigmenti(Bloch-Sulzberger syndrome).
1993;30: 53-59[PMID:8423608 DOI: 10.1136/jmg.30.1.53]
4 Greene-Roethke C.Incontinentia pigmenti:A Summary Review of This Rare Ectodermal Dysplasia With Neurologic Manifestations,Including Treatment Protocols.
2017;31: e45-e52[PMID: 28870493 DOI:10.1016/j.pedhc.2017.07.003]
5 Poziomczyk CS,Recuero JK,Bringhenti L,Maria FD,Campos CW,Travi GM,Freitas AM,Maahs MA,Zen PR,Fiegenbaum M,Almeida ST,Bonamigo RR,Bau AE.Incontinentia pigmenti.
2014;89: 26-36[PMID:24626645 DOI: 10.1590/abd1806-4841.20142584]
6 O'Doherty M,Mc Creery K,Green AJ,Tuwir I,Brosnahan D.Incontinentia pigmenti--ophthalmological observation of a series of cases and review of the literature.
2011;95: 11-16[PMID: 20829317 DOI:10.1136/bjo.2009.164434]
7 Michel S,Reynaud C,Daruich A,Hadj-Rabia S,Bremond-Gignac D,Bodemer C,Robert MP.Early management of sight threatening retinopathy in incontinentia pigmenti.
2020;15: 223[PMID: 32854719 DOI:10.1186/s13023-020-01509-2]
8 Chen CJ,Han IC,Tian J,Muñoz B,Goldberg MF.Extended Follow-up of Treated and Untreated Retinopathy in Incontinentia pigmenti:Analysis of Peripheral Vascular Changes and Incidence of Retinal Detachment.
2015;133: 542-548[PMID: 25695859 DOI: 10.1001/jamaophthalmol.2015.22]
9 Wald KJ,Mehta MC,Katsumi O,Sabates NR,Hirose T.Retinal detachments in incontinentia pigmenti.
1993;111: 614-617[PMID: 8489439 DOI: 10.1001/archopht.1993.01090050048026]
10 Hsiao PF,Lin SP,Chiang SS,Wu YH,Chen HC,Lin YC.NEMO gene mutations in Chinese patients with incontinentia pigmenti.
2010;109: 192-200[PMID: 20434027 DOI: 10.1016/S0929-6646(10)60042-3]
11 Conte MI,Pescatore A,Paciolla M,Esposito E,Miano MG,Lioi MB,McAleer MA,Giardino G,Pignata C,Irvine AD,Scheuerle AE,Royer G,Hadj-Rabia S,Bodemer C,Bonnefont JP,Munnich A,Smahi A,Steffann J,Fusco F,Ursini MV.Insight into IKBKG/NEMO locus: report of new mutations and complex genomic rearrangements leading to incontinentia pigmenti disease.
2014;35: 165-177[PMID: 24339369 DOI: 10.1002/humu.22483]
杂志排行
World Journal of Clinical Cases的其它文章
- Capillary leak syndrome:A rare cause of acute respiratory distress syndrome
- lmproving outcomes in geriatric surgery:ls there more to the equation?
- Mass brain tissue lost after decompressive craniectomy:A case report
- Primary intracranial extraskeletal myxoid chondrosarcoma:A case report and review of literature
- Spinal canal decompression for hypertrophic neuropathy of the cauda equina with chronic inflammatory demyelinating polyradiculoneuropathy:A case report
- Enigmatic rapid organization of subdural hematoma in a patient with epilepsy:A case report