Primary intracranial extraskeletal myxoid chondrosarcoma:A case report and review of literature
2022-06-23ZiYouZhuYuBoWangHanYiLiXinMinWu
lNTRODUCTlON
Extraskeletal myxoid chondrosarcoma(EMC)is an ultrarare type of low- to intermediate-grade malignant soft tissue tumor(STS)comprising small round monomorphic cells and has a low incidence— less than 1/1000000 people are diagnosed annually[1].It mainly occurs in deep soft tissues of the proximal lower extremities and limb girdles,especially in the thigh and popliteal fossa[1,2].Minor cases have been found in the distal extremities,thorax,enterocoelia,trunk,head and neck region,retroperitoneum and paraspinal soft tissue,and even in bone[3-5].Primary intracranial EMC is extremely rare,with only 15 cases reported in the literature.While EMC is considered to be a low-grade malignant neoplasm with a prolonged clinical course and indolent growth pattern,long-term follow-up demonstrated high local recurrence and metastasis rates after surgery(35%-50% and 25%-50%,respectively)[1].Herein,we present a case of primary intracranial EMC located in the left cavernous sinus of a 52-year-old male diagnosed through histopathological and immunohistochemical examination.To the best of our knowledge,this is the first case of primary intracranial EMC arising in the cavernous sinus.Furthermore,we collected information on the existing 15 cases and the present case,summarized the radiographic,histopathological and clinical features of this extraordinarily rare tumor,and reviewed and discussed current research on the histological origin,genetic mutations,diagnosis,treatment strategies and prognosis of primary intracranial EMC to provide greater clinical understanding of this disease.
CASE PRESENTATlON
Chief complaints
A 52-year-old male patient was admitted to our department with complaints of a moderate intermittent headache and dizziness for more than 1 mo.
History of present illness
The patient’s symptoms started from more than 1 mo with a moderate intermitted headache and dizziness,and his health status deteriorated during the last 7 d.There was no obvious nausea,vomiting,blurred vision or disturbance of consciousness.
History of past illness
The patient had a normal and healthy condition in the past;no past history of chronic heart,liver,kidney,lung diseases or infectious diseases;and no past history of head trauma or surgery.
Personal and family history
The patient had a past history of smoking and alcohol consumption for more than 30 years,had already quit smoking for 5 years and had quit drinking for 1 year.There was no special family history.
Physical examination
During the neurological examination,we found that the patient had mild abducent paralysis on his left eyeball with limited eye movement.No abnormities were found in other physical exams.
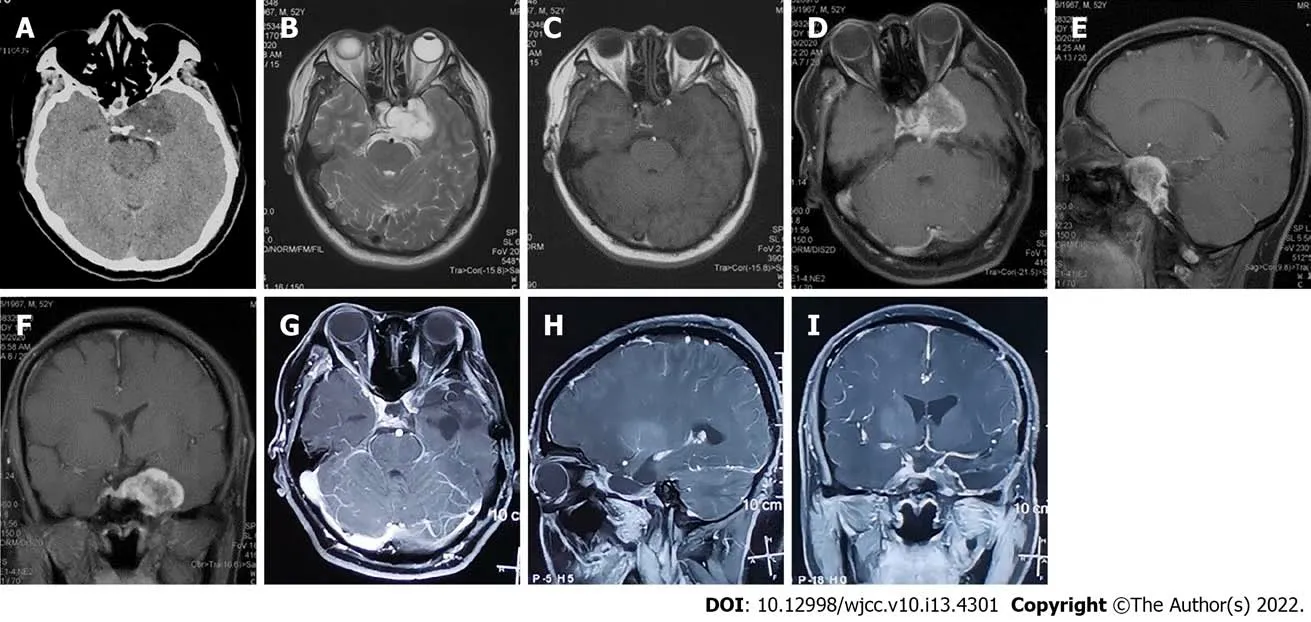
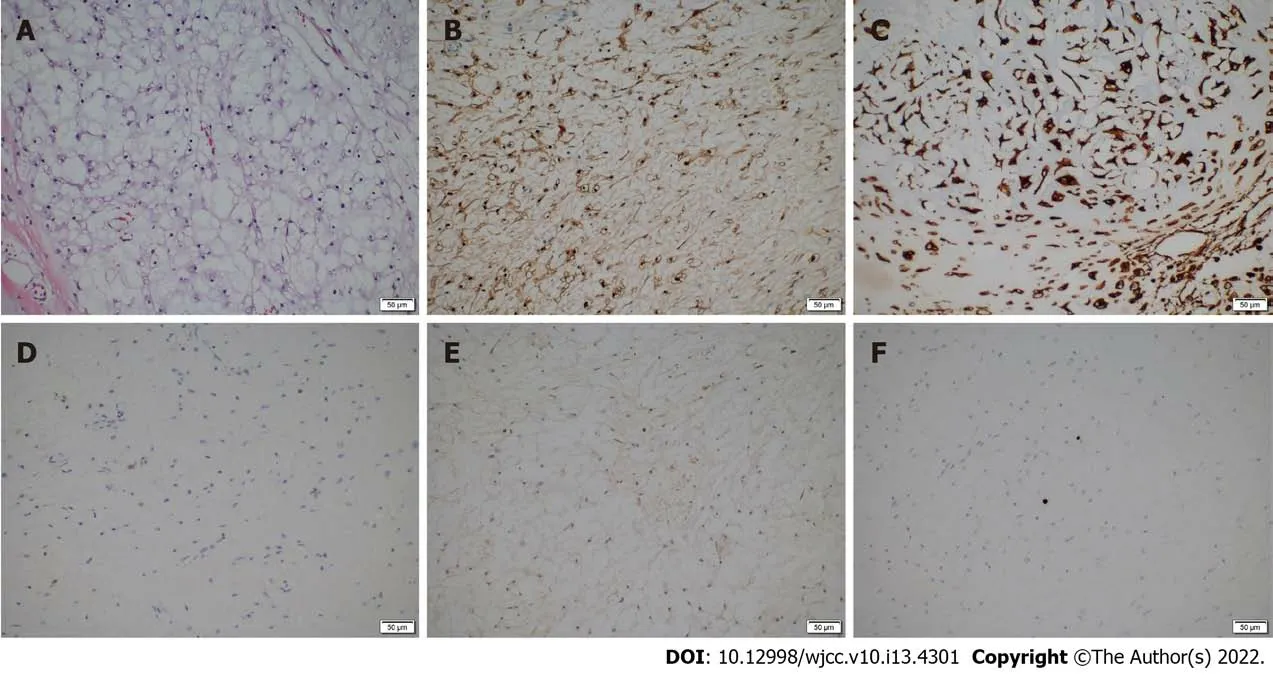
The tumor tissue was fixed in 10% formalin for histological examination.Immunohistochemical analysis was also undertaken and indicated that the tumor was positive for Vimentin,S-100 protein,and lysozyme and negative for epithelial membrane antigen(EMA),CK-pan,CK-7,CK-5,CK-19,and CK-20;the Ki-67 index was less than 1%(Figure 3A-F).According to the results of the histological and immunohistochemical analyses,the Director of Pathology Department of The First Hospital affiliated with Jilin University and her colleagues discussed the pathological features of this lesion and finally diagnosed it as primary intracranial EMC.We performed regular follow-up by phone call contact and informed patients to have regular MRI exams every 3-6 mo after surgery.To date,no radiographic evidence or clinical symptoms have indicated tumor recurrence or metastasis(Figure 1G-I).Meanwhile,the diplopia and blurred vision caused by abducent paralysis in the left eye of the patient showed good improvement.The recovery of this patient 12 mo after the operation was smooth,and the patient returned to his normal life.Regular follow-up will be continued.
Laboratory examinations
No abnormities were found in the laboratory examinations.
Imaging examinations
The sun shone; the young green leaves burst forth; the swallows built their nests; windows were opened, and the children sat once more in the garden on the roof, high above all the other rooms
“Little maiden,” said the lord-in-waiting, “I will obtain for you constant employment in the kitchen, and you shall have permission to see the emperor dine, if you will lead us to the nightingale; for she is invited for this evening to the palace.” So she went into the wood where the nightingale sang, and half the court followed her. As they went along, a cow began lowing.
FlNAL DlAGNOSlS
According to the features of CT and MRI scans of the head described above,the preoperative diagnosis was cavernous sinus hemangioma or meningioma;however,the nature and diagnosis of the lesion is hard to determine.
TREATMENT
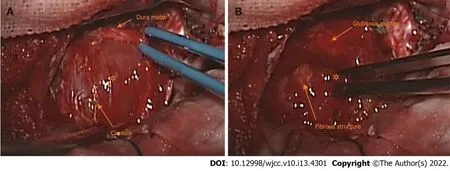
The patient underwent surgery,and the tumor was totally removed from his left cavernous sinus through a supratentorial pterion approach craniotomy and microsurgery.After the surface dura mater of the left cavernous sinus was dissected,we observed that the mass was wrapped by gray-white capsula that adhered tightly to the adjacent dura mater(Figure 2A).The tumor was gray-red in color,with a soft gelatinous texture and moderate vascularity.Notably,it contained abundant glutinous matter.Intratumor gray-white fibrous structures were also observed(Figure 2B).The tumor was grossly totally resected,yet persistent abducent paralysis existed in the patient's left eyes accompanied by diplopia and blurred vision after surgery.The patient had an uneventful recovery after surgery and was discharged 10 days later;shortly thereafter,he was transferred to the oncology department for 45Gy/15F X-ray radiotherapy.The postoperative management conformed to the multidisciplinary treatment(MDT)modality and was made by our surgeons,pathologists,radiologists and oncologists after evaluating and discussing the results of the postoperative pathological exam,the patient’s brain MRI,which was performed before discharge,and the general condition of the patient.
OUTCOME AND FOLLOW-UP
He made the youth follow him through dark secret passages, underground vaults22, and grey rocks till at last they came to an open field, which looked as if it belonged to a more beautiful world than ours
DlSCUSSlON
Primary intracranial extraskeletal myxoid chondrosarcoma(EMC)is extremely rare,and only 15 cases have been reported in the literature to date.The case presented herein is of a 52-year-old male patient with primary intracranial EMC that occurred in the left cavernous sinus.To the best of our knowledge,this is the first case of primary intracranial EMC arising in this area.We also collected information on 15 previously reported cases of primary intracranial EMC and the present case(shown in Table 1 and Table 2)[6-20]with the aim of performing a systematic review of this tumor type,and we discussed the epidemiological and radiographic features,diagnosis,treatment strategies and prognosis of this rare disease.
So she sent for the Enchanter secretly, and after making him promise that he would never turn herself and King Cloverleaf out of their kingdom, and that he would take Potentilla far away, so that never again might she set eyes upon her, she arranged the wedding for the next day but one

Our study included 16 primary intracranial EMC cases(including the present case)consisting of 6 male patients(6/16,37.5%)and 10 female patients(10/16,62.5%)with a median first-onset age of 42 years(range 12-75 years),two of which were juveniles(2/16,12.5%).The tumor size ranged from 2.0 cm to 7.0 cm(mean diameter was 3.2 cm).The sex ratio is nearly 1:1.7 for primary intracranial EMC,which is different from extracranial EMC in that the male/female ratio is nearly 2:1,with a significant predisposition for males.The median first-onset age of patients with extracranial EMC is 50-60 years[1,5].The reason for the difference in the male/female incidence rate and median first-onset age between intracranial and extracranial EMC is unclear;we suspected it might result from the scarcity of primary intracranial EMC cases due to its exceeding rarity.To determine whether epidemiological differences such as M/F incidence and median first-onset age definitely existed between primary intracranial EMCand extracranial EMC,more cases and clinical data are needed.
The locations from which primary intracranial EMCs arise are varied and include the cerebellar hemisphere(
= 2),cerebellopontine angle(
= 2),pineal area(
= 2),sellar area(
= 1),cavernous sinus(present case),ventricle system(
= 2;one in the lateral ventricle and the other in the 4th ventricle)and cerebral hemisphere(
= 6;4 in the frontal or parietal lobe and 2 in the parafalcine region).In most cases,the tumor had clear margins from the brain parenchyma and proved to be in an extra-axial lesion during surgery.Dulou
[17]reported an extra-axial case situated in the left frontal lobe in which the tumor had a less clear margin and a deep location in the brain cortex.Six cases were found to have tight adhesion with adjacent dura mater,including the falx cerebri and tentorium;2 cases were located in the ventricle system adhered to the choroid plexus;2 cases were located in the cerebellopontine angle(CPA)tightly adhered to adjacent cranial nerves;and 4 cases in the cerebrum hemisphere had no relation with either the dura mater or brain parenchyma.One case in the pineal area reported by Sorimachi
[15]adhered to the superior colliculus and connected with the thalamus by a bundle of blood vessels yet had no connection with the dura mater.In the present case,the tumor had a tight connection with the dura mater of the cavernous sinus.Two cases reported by Qin
[19]and Arpino
[16]had cranial bone involvement.According to the data,we found that all the cases,including cases in the ventricle system of primary intracranial EMC,were extra-axial lesions that occurred on the surface or shallow region of the brain cortex or in deep sites of the ventricle system,and cases with involvement in cranial bone or brain parenchyma were rare(3/16;18.8%).Tumors usually had connections with the adjacent dura mater,nerves or choroid plexus(10/16;62.5%).
Soft tissue sarcoma(STS)is a rare mesenchymal neoplasm that,nevertheless,contains more than 70 subtypes,and the management and prognosis of patients can vary significantly between different subtypes[36,37].Only relying on preoperative radiographic exams and empirical diagnosis sometimes causes misdiagnosis[38].Pathological examination is the gold standard of diagnosis of STS and is an indispensable method that accurately indicates the pathological natures of intracranial lesions,such as neoplastic or nonneoplastic,benign or malignant,degree of malignancy,progression,pathological subtype and molecular features,and is also the core method that provides crucial and valuable guidance for surgeons,radiologists and oncologists to make proper and beneficial treatments of STS.Thus,accurate diagnosis with the basis of pathological examination is critical for the management of STS and should be diagnosed by expert pathologists due to the various and complicated pathological features of STS[37,39].Meanwhile,management should be discussed and performed by a multidisciplinary tumor board(MTB)once the lesion is preoperatively suspected to be STS[37,39,40].Thus,all of the deep and superficial lesions in soft tissue that have diameters over 5 cm should undergo preoperative biopsy and pathological examination,and biopsy is also considered mandatory before treatment[37,39,41].With regard to intracranial lesions,especially to suspected malignancies,stereotactic frame-based or frameless brain biopsy is recommended to increase the accuracy of preoperative diagnosis and provide guidance for appropriate treatments,including lesion resection,adjuvant radiotherapy and chemotherapy[42,43].With the guidance of CT,MRI and positron emission tomography(PET)technologies,stereotactic brain biopsy is considered to be a safe,less aggressive and effective means to obtain tissue from intracranial lesions and is generally suitable for patients with the following conditions:(1)Multiple intracranial lesions;(2)The lesion is in the deep locations of the brain,such as the brainstem,thalamus,callosum and basal ganglia,or functional cortical or subcortical areas;(3)The tumor cannot be totally removed by open microsurgery;(4)The general condition of patients is not tolerant to anesthesia,open craniotomy and microsurgery;(5)Patients who have risk factors such as advanced age,systematic disease,severe cardiac disease,
;and(6)Based on radiological and clinical manifestations,the preoperative diagnosis of lesions is intricate,ambiguous and unclear[38,42,44,45].Therefore,if one intracranial lesion is an extra-axial neoplasm and suspected to be STS based on radiographic features,clinical manifestations,history of disease,
,preoperative biopsy is necessary.In our present case,because the lesion was located in the left cavernous sinus and adjoined the internal carotid artery and cranial nerves,the risks of operating stereotactic brain biopsy in this area were evaluated to be high by surgeons.Thus,we performed open craniotomy and tumor resection on the patient and obtained the whole lesion tissue for further pathological exams.
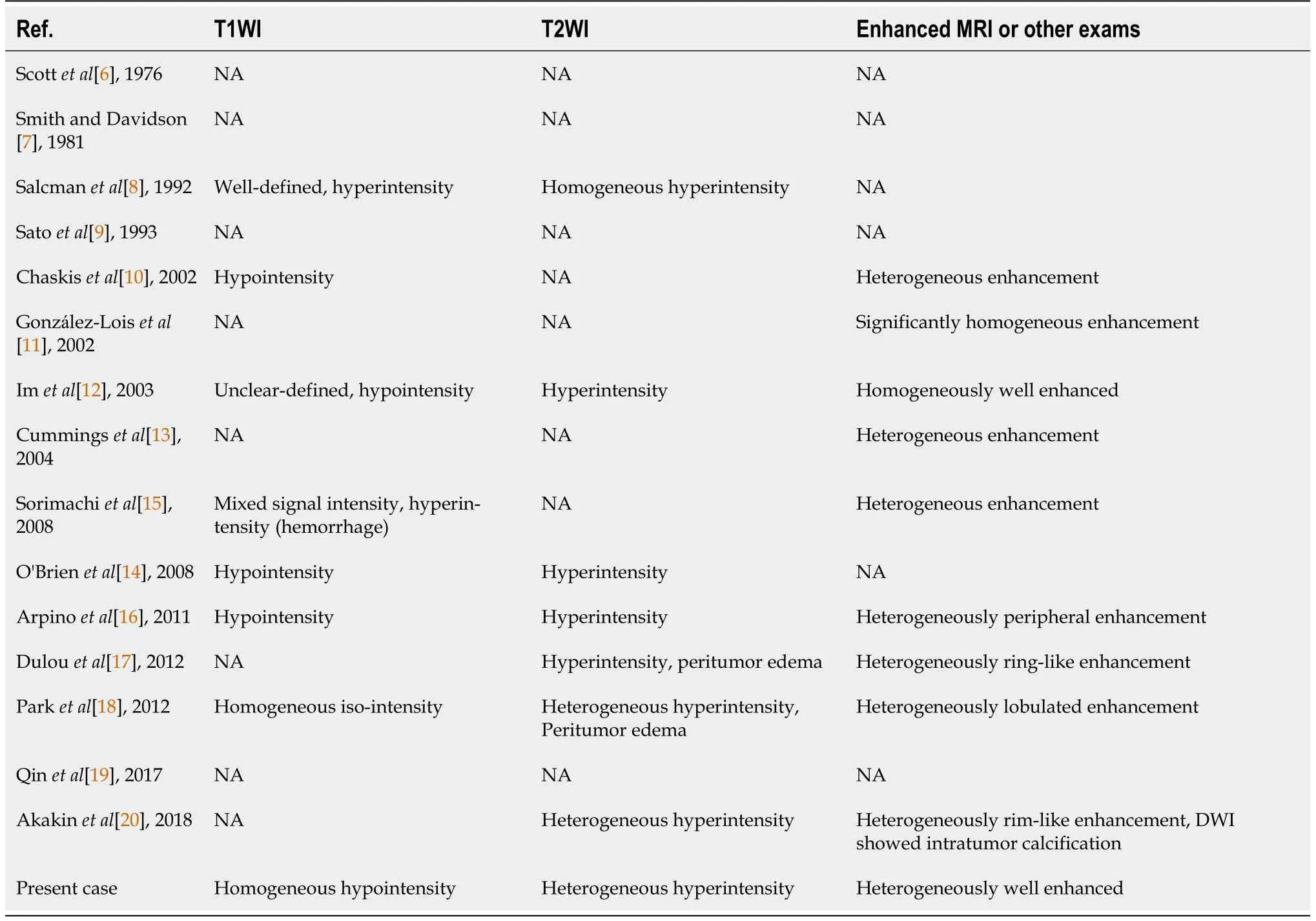
The main examination modalities adopted for diagnosing primary intracranial EMC include CT of the head and brain MRI.The manifestations of primary intracranial EMC in CT exams vary;although tumors typically show iso/Low density,in some cases with intratumor hemorrhage or calcification,the density could be high or mixed.Intratumor hemorrhage and peritumor edema can be observed,yet calcification is rare(2/16,12.5%)[6,20],which is different from previous studies reporting that calcification could be seen in more than 50% of cases of extracranial EMC and most cases of intracranial EMC[14,18].On contrast CT,tumors usually show heterogeneous enhancement,while some could be homogeneous or not well enhanced.The manifestations of primary intracranial EMC in MRI exams are more consistent,as shown in Table 2.Tumors usually exhibit homogeneous hypointensity in T1WI,but the signal can be heterogeneous in cases with intratumor hemorrhage.Tumors commonly show heterogeneous hyperintensity on T2WI,and homogeneous signals can be observed in a few cases.In gadolinium injection-enhanced MRI,most cases were heterogeneously well enhanced,and in some cases,the enhancement pattern can be lobulated or rim/ring-like.Few cases show homogeneous enhancement.
Listen the next time when someone asks you something and you aGREe, because when you could simply say yes, instead you will say absolutely or without doubt or Oh, yeah, unquestionably - absolutely without doubt
The clinical manifestations of primary intracranial EMC are diverse and nonspecific,including tumorrelated increases in intracranial pressure and the associated symptoms of headache,nausea,and vomiting as well as nervous system dysfunction,which manifest as epilepsy[11,14],vision or hearing disturbances,behavioral changes,limb weakness and difficulty walking and speaking.Tumors located in the ventricle system or near the brain stem could also cause hydrocephalus[9,14,18].In the present case,the patient suffered from abducent paralysis in the left eye,which was due to tumor compression of the abduct nerve in the cavernous sinus.
After some years Jack and his wife went to visit his father, but the farmer did not recognize him, and declared he had no son; he had had one, but that one was born with bristles like a hedgehog, and had gone off into the wide world
The prevalent methods for diagnosing primary intracranial EMC rely on histopathology and immunohistochemistry analyses.EMC shows distinctive histological features: under light microscopy with hematoxylin-eosin(H/E)staining,the tumor has a multilobulated pattern with fibrous septa extending into the deep part of the tumor,and the tumor is composed of uniformly shaped small,oval,spindle or round-like cells that have eosinophilic cytoplasm and small round nuclei and are immersed in abundant myxoid extracellular stroma.The formation of mature hyaline cartilage is rare.Tumor cells commonly interconnect and arrange in cords or nests.Small clusters and complex trabecular or cribriform arrays have also been observed in some cases,and the mitotic activity is usually low.However,features such as high mitotic activity,cellular density,dedifferentiated rhabdoid or pleomorphic epithelioid tumor cells have been observed in some postoperative recurrent cases,indicating a more aggressive and higher grade of recurrent neoplasm.The main differential diagnosis of EMC includes sarcomas,which have morphological or histological features similar to those of EMC in histopathological exams,such as epithelioid leiomyosarcoma,epithelioid angiosarcoma,chordoma,parachordoma,myoepithelioma and rhabdoid tumor[5,26-28].Relying only on histological examination for diagnosis can be challenging due to the wide histological spectrum and diverse morphological characteristics of EMC;thus,immunohistochemistry should also be employed to further diagnose and differentiate sarcomas that have histological features similar to those of EMC[25,29].
The immunohistochemistry results of primary intracranial EMC have indicated that the cases are positive for vimentin,with some cases expressing EMA and S-100 protein,and negative for CK series such as CK-5/6,CK-7,CK-19,CK-20,CK-pan,and GFAP.Synaptophysin(3/3,100%)and NSE(2/2,100%)negativity was found in 3 and 2 intracranial cases,respectively[11,14,15,20],yet they have been reported to be positive in some extracranial EMC cases and have been thought to reflect the neuroendocrine origin of EMC[21,23,24,30].In addition,tumors were reported to be negative for chromogranin(2/2,100%)in two cases[15,20]yet positive in some extracranial EMC cases and have been thought to be related to neuroendocrine origin[23,31].
And the little love lump felt all the Wumpalump s health and wholeness and as he touched the little lumps who thought they lacked... they were made whole. And as he touched the little lumps who thought they were hungry... they were filled.
Currently,the standard and crucial treatment modality for soft tissue sarcoma is multidisciplinary treatment(MDT),including surgery,adjuvant radiotherapy and systematic chemotherapy[39,46,47].Surgery is considered to be the basic and standard treatment for local lesions of STS.Wide tumor resection with negative margins is recommended on the contrast that positive margins can cause increasing recurrence and metastasis rates and impact the progression-free survival(PFS)and distant metastasis-free survival(DMFS)of patients[37,39,47,48].Adjuvant radiotherapy is recommended to improve local control and reduce the recurrence of STS[37,39,41,47].EMSO suggests that postoperative radiotherapy should be applied in patients who have a deep tumor,a tumor size over 5 cm or a high degree of malignancy(grades 2-3)[39,49].In advanced disease,stereotactic radiotherapy or stereotactic surgery is adoptable for patients who lose the chance for surgery or are in poor condition and cannot tolerate the operation[39].Given the occurrence of distant metastasis of STS,systematic chemotherapy is also recommended,although the efficacy is still debatable,and the primary first-line chemotherapeutic agents are anthracyclines such as doxorubicin,ifosfamide and gemcitabine[37,39,41].Other novel treatments,such as targeted therapy,immunotherapy,and antiangiogenic agents,such as pazopanib,are promising,and further research is needed[37,50].
The origin and differentiation of primary intracranial EMC remain unclear and controversial[21].According to recent studies,EMC contains unique and special
chimeric gene mutations induced by different chromosomal translocations and has been reconsidered as a new entity that is different from any other sarcoma.It was also categorized as a mesenchymal tumor with uncertain differentiation in the most recent version of the World Health Organization(WHO)classification of soft tissue and bone tumors[22].Some researchers have pointed out that a neuroendocrine origin might be possible[21,23-25].Different ideas about the origin of primary intracranial EMC have also been proposed by researchers.The main speculation is that primary intracranial EMC may originate from multifunctional mesenchymal cells situated in the dura mater,pia-arachnoid,choroid plexus,leptomeninges sheaths around blood vessels and walls of vessels in sulci[6,10,17].In the present case,we presume that the tumor arose from multifunctional mesenchymal cells in the cavernous sinus.
Because the pathological features of EMC are diverse and varied,making a precise diagnosis by pathology can be difficult in some cases[25].In 1995,Stenman
[32]found a unique
-related gene rearrangement mutation that existed only in EMC;subsequently,Noguchi
[33]developed and proposed the use of
and
probes for fluorescence
hybridization to detect whether tumor cells contain
gene rearrangement mutations to diagnose EMC more accurately.The most common type of genetic mutation in EMC is the
gene(over 70%),which is caused by reciprocal chromosomal translocation—t(9;22)(q31.1;q12.2);second,the
gene(approximately 20%)and rare variants of NR4A3 fusion partners(less than 5%),including
,
,
and
[1,34].Other potential diagnostic markers,such as NMB and INSM-1,have also been reported[25,29].Genetic mutation detection is considered to be the most precise method for diagnosing EMC and distinguishing EMC from other tumors with similar histopathological features[35].However,it has been limited in its application in regular clinics and hospitals due to its expense and need for high levels of clinical expertise[29];therefore,of the 16 cases of primary intracranial EMC(including the present case),only 1 patient underwent molecular detection and was found to be positive for
gene mutation[13].In the present case,the patient and his family refused molecular testing due to its cost.Thus,identifying and developing cheaper,more available and precise diagnostic approaches are necessary.The effects of molecular tests on diagnosing primary intracranial EMC still need more data and research for verification.
Due to the extreme rarity of primary intracranial EMC,standard and optimal treatment strategies for this disease remain undefined.In our research of the 16 primary intracranial EMC cases available in the literature,3 did not have any information on the prognosis of patients,and in 2 cases,the patients died from non-EMC-related factors after surgery.Of the remaining 11 cases,9 patients underwent gross total resection(GTR),1 underwent partial resection(PR),and the last underwent subtotal resection(STR).Four of the 9 patients who underwent GTR also underwent postoperative RT,and the remaining 5 patients underwent GTR only without postoperative RT.The recurrence rate of the single GTR surgery group was 80%(
= 4,4/5),and the median progression-free survival(PFS)was 10 mo,yet that in the GTR combined with RT group was 25%(
= 1,1/4),and the PFS was 36 mo.No case in which GTR was accepted reported metastasis.Only 1 out of the 11 patients who underwent PR died from local recurrence and spinal metastasis of primary intracranial EMC at 36 mo after surgery[9].Interestingly,metastasis occurred through cerebrospinal fluid(CSF)circulation.One of the 11 patients underwent STR and postoperative proton therapy,and no recurrence or metastasis was found after surgery[14].According to these data,patients who undergo GTR with postoperative RT seem to have a lower recurrence rate and longer PFS than those who undergo surgery only.Due to the scarcity of data,cases and long-term follow-up,further studies are needed to verify whether GTR combined with RT is better for reducing the recurrence rate and prolonging PFS than single surgery therapy.
To date,the most effective approach for treating EMC is surgery,and wide local resection with a negative microscopic margin is considered to be the standard method and recommended for patients with local lesions,since inadequate initial surgery has been reported by Satoshi Kawaguchi[51]to be a significant risk factor for local recurrence[23,24,52,53].However,even if patients undergo wide resection,the postoperative recurrence rate still reaches 35%-50% at 5 years,and the metastasis rate is also 25%-50% after radical surgery.Bishop[54]pointed out that indolent biological characteristics and low-grade histological classification might cause combined modality therapy(CMT),such as surgery and radiotherapy(RT),to not be widely used in patients with local EMC,which could result in a high recurrence and metastasis rate.They performed a retrospective study of 41 patients with local EMC and found that patients treated with surgery combined with RT had better local control than those treated with surgery alone(100% and 63%,respectively,local control rate in 10 years).They also found that local recurrence was the only risk factor that led to a high metastasis rate and worse distant metastasisfree survival(DMFS).According to previous research,surgery combined with radiotherapy is beneficial to patients;thus,they recommend CMT for EMC to reduce local recurrence and distal metastasis.Another retrospective study of 87 patients with EMC also reported that surgery with RT combined with CMT could obtain better local control than surgery alone[55].Data from the Surveillance,Epidemiology and End Result(SEER)database were used to perform a population-based analysis of 156 patients with local EMC,and the results revealed that surgery combined with RT could be considered for patients with local lesions,especially large tumors[56].
Informed written consent was obtained from the patient for publication of this report and any accompanying images.
EMC is a low- to intermediate-grade malignant soft tissue sarcoma with indolent biological characteristics,but it has high potential for postoperative recurrence and metastasis even if patients undergo wide resection.However,EMC is considered to have a favorable prognosis due to its protracted clinical course and long survival period,even when local recurrence or distal metastasis occurs[26].Many studies have investigated the prognostic factors of EMC related to recurrence and metastasis.A large tumor size,older age,proximal location,refusal of postoperative RT,histological characteristics such as high mitotic activity,high Ki-67 index,atypia including anaplasia or rhabdoid cell features,high cellularity and metastasis occurrence have been found to be significantly associated with poor prognosis[1,5,23].Moreover,different types of
translocation events could affect the prognosis of EMC.Patients carrying an
chimeric gene showed a better prognosis with longer disease-free survival(DFS)and distal metastasis-free survival(DMFS)than those carrying
and other variant
-related chimeric genes[51,65].Due to the high propensity of recurrence and metastasis of EMC accompanied by a protracted clinical course,long-term follow-up is absolutely indispensable for these patients.
CONCLUSlON
Primary intracranial extraskeletal myxoid chondrosarcoma is an extremely rare disease.To the best of our knowledge,only 15 cases have been reported to date.We herein report the case of a 52-year-old male patient with EMC and review the literature.We believe that our report can enrich the clinical data on primary intracranial EMC and provide a better understanding for clinicians and radiologists who diagnose and manage this rare disease.
Now as I slid the evening meal into the oven, I realized it had been nearly three weeks since we d even heard mention of Susan s name. I missed her warm smile and eager-to-please ways.
ACKNOWLEDGEMENTS
The author would like to thank to all the specialists who providing available help for this article,and thank to the patient and his family provide medical history.
A plain computed tomography(CT)scan of the head revealed a homogeneous low-density and round shape-occupying lesion in his left cavernous sinus.No hemorrhage,calcification or bone destructive lesions were noted on CT(Figure 1A).The magnetic resonance imaging(MRI)scan of the head revealed a 3.4 × 3.0 cm sized,well-defined mass with an irregularly round shape located in the left cavernous sinus and simultaneously involving the sellar region and right cavernous sinus.The tumor was homogeneously hypointense on T1-weighted imaging(T1WI)and heterogeneously hyperintense on T2-weighted imaging(T2WI)with septal or stripe-like iso-hypointensity in the central area and significant hyperintensity in the paracentral area(Figure 1B and C).A gadolinium injection-enhanced MRI scan of the head also revealed a well-defined and heterogeneous well-enhanced tumor with an irregular round shape that was mainly located in the left cavernous sinus and involved the sellar area and right cavernous sinus.In addition,the tumor was not or slightly enhanced in the central part but was significantly enhanced in the remaining part(Figure 1D-F).No abnormities were found in plain chest and abdominal CT scans.
FOOTNOTES
Zhu ZY,Wang YB and Li HY contributed equally to this work;Wu XM,Wang YB were the surgeons that performed the surgery;Wu XM designed the study,Zhu ZY and Wang YB made data collection,data analysis and interpretation,and made contribution to interpreting of the imaging findings,reviewing the literatures,and writing the manuscript;Li HY and Zhu ZY contributed to the translation work,made terms and grammar corrections;Wu XM,Zhu ZY and Wang YB contributed to the revision work;All authors contributed to the article and issued the final approval for the version to be submitted.
In addition to surgery and RT for local lesions,systematic therapy and antiangiogenic therapy have also been investigated.In recent studies,EMCs were found to be more sensitive to anthracycline-based agents than previously expected,and trabectedin could be a suitable alternative for patients with metastatic EMC who are unsensitive or intolerable to anthracycline-based agents[57,58].Antiangiogenic agents such as sunitinib and pazopanib also showed certain positive effects on EMC[59-61].Because a special
rearrangement mutation exists in EMC and studies have shown that the products of
-associated fusion genes play an important role in the growth and differentiation of tumor cells and might be related to tumorigenesis,progression and metastasis[62-64],revealing the precise functions and mechanism of these mutations in the pathogenesis and progression of EMC might help us discover potential therapeutic targets for targeted treatment and biomarkers for diagnosis.In addition,the influence of the blood-brain barrier(BBB)on permeability and the effects of chemotherapeutic,antiangiogenic and targeted drugs should also be taken into account when treating primary intracranial EMC.More research on pharmacotherapies for primary intracranial EMC treatment is still needed.In summary,we believe that a radical resection approach,such as GTR combined with RT,is the most beneficial treatment strategy for patients with primary intracranial EMC,but the effects of chemotherapy and antiangiogenic therapy still need to be verified by further research due to the scarcity of data and limited number of studies.
The authors declare that they have no conflict of interest.
The authors have read the CARE Checklist(2016),and the manuscript was prepared and revised according to the CARE Checklist(2016).
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial(CC BYNC 4.0)license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
The child does not know, when we fly through the room, that we smile with joy at his good conduct, for we can count one year less of our three hundred years
China
Zi-You Zhu 0000-0003-3582-0618;Yu-Bo Wang 0000-0002-3404-0225;Han-Yi Li 0000-0001-9587-7531;Xin-Min Wu 0000-0001-8933-5744.
Gong ZM
Ah, yes, you are always so polite, said mamma, with a smile; andKaela silently pressed his hand, all soiled as it was with the clay.Then he unfolded to them both the beauties of Nature, in all herworks; he pointed26 out to them how, in the scale of creation, inanimatematter was inferior to animate27 nature; the plant above the mineral,the animal above the plant, and man above them all. He strove toshow them how the beauty of the mind could be displayed in the outward form, and that it was the sculptor s task to seize upon that beauty of expression, and produce it in his works. Kaela stood silent, but nodded in approbation28 of what he said, while mamma-in-law made the following confession:-
A
Gong ZM
1 Stacchiotti S,Baldi GG,Morosi C,Gronchi A,Maestro R.Extraskeletal Myxoid Chondrosarcoma: State of the Art and Current Research on Biology and Clinical Management.
2020;12[PMID: 32967265 DOI:10.3390/cancers12092703]
2 Enzinger FM,Shiraki M.Extraskeletal myxoid chondrosarcoma.An analysis of 34 cases.
1972;3: 421-435[PMID: 4261659 DOI: 10.1016/s0046-8177(72)80042-x]
3 Fukuda T,Ishikawa H,Ohnishi Y,Tachikawa S,Onizuka S,Sakashita I.Extraskeletal myxoid chondrosarcoma arising from the retroperitoneum.
1986;85: 514-519[PMID: 3953507 DOI: 10.1093/ajcp/85.4.514]
4 Demicco EG,Wang WL,Madewell JE,Huang D,Bui MM,Bridge JA,Meis JM.Osseous myxochondroid sarcoma:A detailed study of 5 cases of extraskeletal myxoid chondrosarcoma of the bone.
2013;37: 752-762[PMID:23588370 DOI: 10.1097/PAS.0b013e3182796e46]
5 Meis-Kindblom JM,Bergh P,Gunterberg B,Kindblom LG.Extraskeletal myxoid chondrosarcoma:A reappraisal of its morphologic spectrum and prognostic factors based on 117 cases.
1999;23: 636-650[PMID: 10366145 DOI: 10.1097/00000478-199906000-00002]
6 Scott RM,Dickersin R,Wolpert SM,Twitchell T.Myxochondrosarcoma of the fourth ventricle.Case report.
1976;44: 386-389[PMID: 1249620 DOI: 10.3171/jns.1976.44.3.0386]
7 Smith TW,Davidson RI.Primary meningeal myxochondrosarcoma presenting as a cerebellar mass: case report.
1981;8: 577-581[PMID: 7266799 DOI: 10.1227/00006123-198105000-00012]
8 Salcman M,Scholtz H,Kristt D,Numaguchi Y.Extraskeletal myxoid chondrosarcoma of the falx.
1992;31:344-348[PMID: 1513440 DOI: 10.1227/00006123-199208000-00021]
9 Sato K,Kubota T,Yoshida K,Murata H.Intracranial extraskeletal myxoid chondrosarcoma with special reference to lamellar inclusions in the rough endoplasmic reticulum.
1993;86: 525-528[PMID: 8310804 DOI:10.1007/bf00228591]
10 Chaskis C,Michotte A,Goossens A,Stadnik T,Koerts G,D'Haens J.Primary intracerebral myxoid chondrosarcoma.Case illustration.
2002;97: 228[PMID: 12134922 DOI: 10.3171/jns.2002.97.1.0228]
11 González-Lois C,Cuevas C,Abdullah O,Ricoy JR.Intracranial extraskeletal myxoid chondrosarcoma: case report and review of the literature.
2002;144: 735-740[PMID: 12181708 DOI: 10.1007/s00701-002-0949-y]
12 Im SH,Kim DG,Park IA,Chi JG.Primary intracranial myxoid chondrosarcoma: report of a case and review of the literature.
2003;18: 301-307[PMID: 12692436 DOI: 10.3346/jkms.2003.18.2.301]
13 Cummings TJ,Bridge JA,Fukushima T.Extraskeletal myxoid chondrosarcoma of the jugular foramen.
2004;23: 232-237[PMID: 15581026]
14 O'Brien J,Thornton J,Cawley D,Farrell M,Keohane K,Kaar G,McEvoy L,O'Brien DF.Extraskeletal myxoid chondrosarcoma of the cerebellopontine angle presenting during pregnancy.
2008;22: 429-432[PMID:18568733 DOI: 10.1080/02688690701780127]
15 Sorimachi T,Sasaki O,Nakazato S,Koike T,Shibuya H.Myxoid chondrosarcoma in the pineal region.
2008;109: 904-907[PMID: 18976082 DOI: 10.3171/jns/2008/109/11/0904]
16 Arpino L,Capuano C,Gravina M,Franco A.Parasellar myxoid chondrosarcoma:A rare variant of cranial chondrosarcoma.
2011;55: 387-389[PMID: 22198591]
17 Dulou R,Chargari C,Dagain A,Teriitehau C,Goasguen O,Jeanjean O,Védrine L.Primary intracranial extraskeletal myxoid chondrosarcoma.
2012;46: 76-81[PMID: 22426765 DOI: 10.5114/ninp.2012.27176]
18 Park JH,Kim MJ,Kim CJ,Kim JH.Intracranial extraskeletal myxoid chondrosarcoma : case report and literature review.
2012;52: 246-249[PMID: 23115670 DOI: 10.3340/jkns.2012.52.3.246]
19 Qin Y,Zhang HB,Ke CS,Huang J,Wu B,Wan C,Yang CS,Yang KY.Primary extraskeletal myxoid chondrosarcoma in cerebellum: A case report with literature review.
2017;96: e8684[PMID: 29381948 DOI:10.1097/md.0000000000008684]
20 Akakın A,Urgun K,Ekşi MŞ,Yılmaz B,Yapıcıer Ö,Mestanoğlu M,Toktaş ZO,Demir MK,Kılıç T.Falcine Myxoid Chondrosarcoma:A Rare Aggressive Case.
2018;13: 68-71[PMID: 29492125 DOI:10.4103/1793-5482.181116]
21 Goh YW,Spagnolo DV,Platten M,Caterina P,Fisher C,Oliveira AM,Nascimento AG.Extraskeletal myxoid chondrosarcoma:A light microscopic,immunohistochemical,ultrastructural and immuno-ultrastructural study indicating neuroendocrine differentiation.
2001;39: 514-524[PMID: 11737310 DOI:10.1046/j.1365-2559.2001.01277.x]
22 Horvai A,Agaram N,Lucas D.Extraskeletal myxoid condrosarcoma.World Health Organization(WHO)Classification of Soft Tissue and Bone Tumours,2020: 303-305
23 Oliveira AM,Sebo TJ,McGrory JE,Gaffey TA,Rock MG,Nascimento AG.Extraskeletal myxoid chondrosarcoma:A clinicopathologic,immunohistochemical,and ploidy analysis of 23 cases.
2000;13: 900-908[PMID:10955458 DOI: 10.1038/modpathol.3880161]
24 Okamoto S,Hisaoka M,Ishida T,Imamura T,Kanda H,Shimajiri S,Hashimoto H.Extraskeletal myxoid chondrosarcoma:a clinicopathologic,immunohistochemical,and molecular analysis of 18 cases.
2001;32: 1116-1124[PMID:11679947 DOI: 10.1053/hupa.2001.28226]
25 Subramanian S,West RB,Marinelli RJ,Nielsen TO,Rubin BP,Goldblum JR,Patel RM,Zhu S,Montgomery K,Ng TL,Corless CL,Heinrich MC,van de Rijn M.The gene expression profile of extraskeletal myxoid chondrosarcoma.
2005;206: 433-444[PMID: 15920699 DOI: 10.1002/path.1792]
26 Lucas DR,Fletcher CD,Adsay NV,Zalupski MM.High-grade extraskeletal myxoid chondrosarcoma:A high-grade epithelioid malignancy.
1999;35: 201-208[PMID: 10469211 DOI: 10.1046/j.1365-2559.1999.00735.x]
27 Folpe AL,Agoff SN,Willis J,Weiss SW.Parachordoma is immunohistochemically and cytogenetically distinct from axial chordoma and extraskeletal myxoid chondrosarcoma.
1999;23: 1059-1067[PMID: 10478665 DOI:10.1097/00000478-199909000-00008]
28 Flucke U,Tops BB,Verdijk MA,van Cleef PJ,van Zwam PH,Slootweg PJ,Bovée JV,Riedl RG,Creytens DH,Suurmeijer AJ,Mentzel T.NR4A3 rearrangement reliably distinguishes between the clinicopathologically overlapping entities myoepithelial carcinoma of soft tissue and cellular extraskeletal myxoid chondrosarcoma.
2012;460: 621-628[PMID: 22569967 DOI: 10.1007/s00428-012-1240-0]
29 Yoshida A,Makise N,Wakai S,Kawai A,Hiraoka N.INSM1 expression and its diagnostic significance in extraskeletal myxoid chondrosarcoma.
2018;31: 744-752[PMID: 29327709 DOI: 10.1038/modpathol.2017.189]
30 Shao R,Lao IW,Wang L,Yu L,Wang J,Fan Q.Clinicopathologic and radiologic features of extraskeletal myxoid chondrosarcoma:A retrospective study of 40 Chinese cases with literature review.
2016;23: 14-20[PMID: 27402218 DOI: 10.1016/j.anndiagpath.2016.04.004]
31 Patel SR,Burgess MA,Papadopoulos NE,Linke KA,Benjamin RS.Extraskeletal myxoid chondrosarcoma.Long-term experience with chemotherapy.
1995;18: 161-163[PMID: 7900708 DOI:10.1097/00000421-199504000-00014]
32 Stenman G,Andersson H,Mandahl N,Meis-Kindblom JM,Kindblom LG.Translocation t(9;22)(q22;q12)is a primary cytogenetic abnormality in extraskeletal myxoid chondrosarcoma.
1995;62: 398-402[PMID: 7635565 DOI:10.1002/ijc.2910620407]
33 Noguchi H,Mitsuhashi T,Seki K,Tochigi N,Tsuji M,Shimoda T,Hasegawa T.Fluorescence in situ hybridization analysis of extraskeletal myxoid chondrosarcomas using EWSR1 and NR4A3 probes.
2010;41: 336-342[PMID: 19775727 DOI: 10.1016/j.humpath.2009.04.028]
34 Urbini M,Astolfi A,Pantaleo MA,Serravalle S,Dei Tos AP,Picci P,Indio V,Sbaraglia M,Benini S,Righi A,Gambarotti M,Gronchi A,Colombo C,Dagrada GP,Pilotti S,Maestro R,Polano M,Saponara M,Tarantino G,Pession A,Biasco G,Casali PG,Stacchiotti S.HSPA8 as a novel fusion partner of NR4A3 in extraskeletal myxoid chondrosarcoma.
2017;56: 582-586[PMID: 28383167 DOI: 10.1002/gcc.22462]
35 Paioli A,Stacchiotti S,Campanacci D,Palmerini E,Frezza AM,Longhi A,Radaelli S,Donati DM,Beltrami G,Bianchi G,Barisella M,Righi A,Benini S,Fiore M,Picci P,Gronchi A.Extraskeletal Myxoid Chondrosarcoma with Molecularly Confirmed Diagnosis:A Multicenter Retrospective Study Within the Italian Sarcoma Group.
2021;28:1142-1150[PMID: 32572850 DOI: 10.1245/s10434-020-08737-7]
36 Hui JY.Epidemiology and Etiology of Sarcomas.
2016;96: 901-914[PMID: 27542634 DOI:10.1016/j.suc.2016.05.005]
37 Bourcier K,Le Cesne A,Tselikas L,Adam J,Mir O,Honore C,de Baere T.Basic Knowledge in Soft Tissue Sarcoma.
2019;42: 1255-1261[PMID: 31236647 DOI: 10.1007/s00270-019-02259-w]
38 Callovini GM,Telera S,Sherkat S,Sperduti I,Callovini T,Carapella CM.How is stereotactic brain biopsy evolving?
2018;174: 101-107[PMID: 30227295 DOI: 10.1016/j.clineuro.2018.09.020]
39 de Juan Ferré A,Álvarez Álvarez R,Casado Herráez A,Cruz Jurado J,Estival González A,Martín-Broto J,Martínez Marín V,Moreno Vega A,Sebio García A,Valverde Morales C.SEOM Clinical Guideline of management of soft-tissue sarcoma(2020).
2021;23: 922-930[PMID: 33405052 DOI: 10.1007/s12094-020-02534-0]
40 Blay JY,Soibinet P,Penel N,Bompas E,Duffaud F,Stoeckle E,Mir O,Adam J,Chevreau C,Bonvalot S,Rios M,Kerbrat P,Cupissol D,Anract P,Gouin F,Kurtz JE,Lebbe C,Isambert N,Bertucci F,Toumonde M,Thyss A,Piperno-Neumann S,Dubray-Longeras P,Meeus P,Ducimetière F,Giraud A,Coindre JM,Ray-Coquard I,Italiano A,Le Cesne A.Improved survival using specialized multidisciplinary board in sarcoma patients.
2017;28: 2852-2859[PMID: 29117335 DOI: 10.1093/annonc/mdx484]
41 Gilbert NF,Cannon CP,Lin PP,Lewis VO.Soft-tissue sarcoma.
2009;17: 40-47[PMID:19136426 DOI: 10.5435/00124635-200901000-00006]
42 Ersahin M,Karaaslan N,Gurbuz MS,Hakan T,Berkman MZ,Ekinci O,Denizli N,Aker FV.The safety and diagnostic value of frame-based and CT-guided stereotactic brain biopsy technique.
2011;21: 582-590[PMID:22194120]
43 Krieger MD,Chandrasoma PT,Zee CS,Apuzzo ML.Role of stereotactic biopsy in the diagnosis and management of brain tumors.
1998;14: 13-25[PMID: 9407627 DOI:10.1002/(sici)1098-2388(199801/02)14:1<13::aid-ssu3>3.0.co;2-5]
44 Hildebrand J.Indications for stereotactically-aided differential diagnosis: the neurologist's view.
1993;124: 23-25[PMID: 8279286 DOI: 10.1007/BF01400710]
45 Apuzzo ML,Sabshin JK.Computed tomographic guidance stereotaxis in the management of intracranial mass lesions.
1983;12: 277-285[PMID: 6341870 DOI: 10.1227/00006123-198303000-00005]
46 Andritsch E,Beishon M,Bielack S,Bonvalot S,Casali P,Crul M,Delgado Bolton R,Donati DM,Douis H,Haas R,Hogendoorn P,Kozhaeva O,Lavender V,Lovey J,Negrouk A,Pereira P,Roca P,de Lempdes GR,Saarto T,van Berck B,Vassal G,Wartenberg M,Yared W,Costa A,Naredi P.ECCO Essential Requirements for Quality Cancer Care: Soft Tissue Sarcoma in Adults and Bone Sarcoma.A critical review.
2017;110: 94-105[PMID: 28109409 DOI: 10.1016/j.critrevonc.2016.12.002]
47 Gamboa AC,Gronchi A,Cardona K.Soft-tissue sarcoma in adults: An update on the current state of histiotype-specific management in an era of personalized medicine.
2020;70: 200-229[PMID: 32275330 DOI:10.3322/caac.21605]
48 von Mehren M,Randall RL,Benjamin RS,Boles S,Bui MM,Ganjoo KN,George S,Gonzalez RJ,Heslin MJ,Kane JM,Keedy V,Kim E,Koon H,Mayerson J,McCarter M,McGarry SV,Meyer C,Morris ZS,O'Donnell RJ,Pappo AS,Paz IB,Petersen IA,Pfeifer JD,Riedel RF,Ruo B,Schuetze S,Tap WD,Wayne JD,Bergman MA,Scavone JL.Soft Tissue Sarcoma,Version 2.2018,NCCN Clinical Practice Guidelines in Oncology.
2018;16: 536-563[PMID: 29752328 DOI: 10.6004/jnccn.2018.0025]
49 Casali PG,Abecassis N,Aro HT,Bauer S,Biagini R,Bielack S,Bonvalot S,Boukovinas I,Bovee JVMG,Brodowicz T,Broto JM,Buonadonna A,De Álava E,Dei Tos AP,Del Muro XG,Dileo P,Eriksson M,Fedenko A,Ferraresi V,Ferrari A,Ferrari S,Frezza AM,Gasperoni S,Gelderblom H,Gil T,Grignani G,Gronchi A,Haas RL,Hassan B,Hohenberger P,Issels R,Joensuu H,Jones RL,Judson I,Jutte P,Kaal S,Kasper B,Kopeckova K,Krákorová DA,Le Cesne A,Lugowska I,Merimsky O,Montemurro M,Pantaleo MA,Piana R,Picci P,Piperno-Neumann S,Pousa AL,Reichardt P,Robinson MH,Rutkowski P,Safwat AA,Schöffski P,Sleijfer S,Stacchiotti S,Sundby Hall K,Unk M,Van Coevorden F,van der Graaf WTA,Whelan J,Wardelmann E,Zaikova O,Blay JY;ESMO Guidelines Committee and EURACAN.Soft tissue and visceral sarcomas: ESMO-EURACAN Clinical Practice Guidelines for diagnosis,treatment and follow-up.
2018;29: iv51-iv67[PMID: 29846498 DOI: 10.1093/annonc/mdy096]
50 Linch M,Miah AB,Thway K,Judson IR,Benson C.Systemic treatment of soft-tissue sarcoma-gold standard and novel therapies.
2014;11: 187-202[PMID: 24642677 DOI: 10.1038/nrclinonc.2014.26]
51 Kawaguchi S,Wada T,Nagoya S,Ikeda T,Isu K,Yamashiro K,Kawai A,Ishii T,Araki N,Myoui A,Matsumoto S,Umeda T,Yoshikawa H,Hasegawa T;Multi-Institutional Study of 42 Cases in Japan.Extraskeletal myxoid chondrosarcoma:A Multi-Institutional Study of 42 Cases in Japan.
2003;97: 1285-1292[PMID: 12599237 DOI:10.1002/cncr.11162]
52 McGrory JE,Rock MG,Nascimento AG,Oliveira AM.Extraskeletal myxoid chondrosarcoma.
2001;185-190[PMID: 11153986 DOI: 10.1097/00003086-200101000-00025]
53 Chiusole B,Le Cesne A,Rastrelli M,Maruzzo M,Lorenzi M,Cappellesso R,Del Fiore P,Imbevaro S,Sbaraglia M,Terrier P,Ruggieri P,Dei Tos AP,Rossi CR,Zagonel V,Brunello A.Extraskeletal Myxoid Chondrosarcoma: Clinical and Molecular Characteristics and Outcomes of Patients Treated at Two Institutions.
2020;10: 828[PMID:32612944 DOI: 10.3389/fonc.2020.00828]
54 Bishop AJ,Bird JE,Conley AP,Roland CL,Moon BS,Satcher RL,Livingston JA,Patel S,Wang WL,Lazar AJ,Lewis VO,Lin PP,Guadagnolo BA.Extraskeletal Myxoid Chondrosarcomas: Combined Modality Therapy With Both Radiation and Surgery Improves Local Control.
2019;42: 744-748[PMID: 31436747 DOI:10.1097/coc.0000000000000590]
55 Drilon AD,Popat S,Bhuchar G,D'Adamo DR,Keohan ML,Fisher C,Antonescu CR,Singer S,Brennan MF,Judson I,Maki RG.Extraskeletal myxoid chondrosarcoma:A retrospective review from 2 referral centers emphasizing long-term outcomes with surgery and chemotherapy.
2008;113: 3364-3371[PMID: 18951519 DOI: 10.1002/cncr.23978]
56 Kemmerer EJ,Gleeson E,Poli J,Ownbey RT,Brady LW,Bowne WB.Benefit of Radiotherapy in Extraskeletal Myxoid Chondrosarcoma:A Propensity Score Weighted Population-based Analysis of the SEER Database.
2018;41: 674-680[PMID: 27819877 DOI: 10.1097/coc.0000000000000341]
57 Morioka H,Takahashi S,Araki N,Sugiura H,Ueda T,Takahashi M,Yonemoto T,Hiraga H,Hiruma T,Kunisada T,Matsumine A,Susa M,Nakayama R,Nishimoto K,Kikuta K,Horiuchi K,Kawai A.Results of sub-analysis of a phase 2 study on trabectedin treatment for extraskeletal myxoid chondrosarcoma and mesenchymal chondrosarcoma.
2016;16: 479[PMID: 27418251 DOI: 10.1186/s12885-016-2511-y]
58 Stacchiotti S,Dagrada GP,Sanfilippo R,Negri T,Vittimberga I,Ferrari S,Grosso F,Apice G,Tricomi M,Colombo C,Gronchi A,Dei Tos AP,Pilotti S,Casali PG.Anthracycline-based chemotherapy in extraskeletal myxoid chondrosarcoma:a retrospective study.
2013;3: 16[PMID: 24345066 DOI: 10.1186/2045-3329-3-16]
59 Stacchiotti S,Pantaleo MA,Astolfi A,Dagrada GP,Negri T,Dei Tos AP,Indio V,Morosi C,Gronchi A,Colombo C,Conca E,Toffolatti L,Tazzari M,Crippa F,Maestro R,Pilotti S,Casali PG.Activity of sunitinib in extraskeletal myxoid chondrosarcoma.
2014;50: 1657-1664[PMID: 24703573 DOI: 10.1016/j.ejca.2014.03.013]
60 Stacchiotti S,Ferrari S,Redondo A,Hindi N,Palmerini E,Vaz Salgado MA,Frezza AM,Casali PG,Gutierrez A,Lopez-Pousa A,Grignani G,Italiano A,LeCesne A,Dumont S,Blay JY,Penel N,Bernabeu D,de Alava E,Karanian M,Morosi C,Brich S,Dagrada GP,Vallacchi V,Castelli C,Brenca M,Racanelli D,Maestro R,Collini P,Cruz J,Martin-Broto J.Pazopanib for treatment of advanced extraskeletal myxoid chondrosarcoma:A multicentre,single-arm,phase 2 trial.
2019;20: 1252-1262[PMID: 31331701 DOI: 10.1016/s1470-2045(19)30319-5]
61 Stacchiotti S,Dagrada GP,Morosi C,Negri T,Romanini A,Pilotti S,Gronchi A,Casali PG.Extraskeletal myxoid chondrosarcoma: tumor response to sunitinib.
2012;2: 22[PMID: 23058004 DOI:10.1186/2045-3329-2-22]
62 Filion C,Motoi T,Olshen AB,Laé M,Emnett RJ,Gutmann DH,Perry A,Ladanyi M,Labelle Y.The EWSR1/NR4A3 fusion protein of extraskeletal myxoid chondrosarcoma activates the PPARG nuclear receptor gene.
2009;217: 83-93[PMID: 18855877 DOI: 10.1002/path.2445]
63 Brenca M,Stacchiotti S,Fassetta K,Sbaraglia M,Janjusevic M,Racanelli D,Polano M,Rossi S,Brich S,Dagrada GP,Collini P,Colombo C,Gronchi A,Astolfi A,Indio V,Pantaleo MA,Picci P,Casali PG,Dei Tos AP,Pilotti S,Maestro R.NR4A3 fusion proteins trigger an axon guidance switch that marks the difference between EWSR1 and TAF15 translocated extraskeletal myxoid chondrosarcomas.
2019;249: 90-101[PMID: 31020999 DOI: 10.1002/path.5284]
64 Filion C,Labelle Y.The oncogenic fusion protein EWS/NOR-1 induces transformation of CFK2 chondrogenic cells.
2004;297: 585-592[PMID: 15212958 DOI: 10.1016/j.yexcr.2004.03.040]
65 Agaram NP,Zhang L,Sung YS,Singer S,Antonescu CR.Extraskeletal myxoid chondrosarcoma with non-EWSR1-NR4A3 variant fusions correlate with rhabdoid phenotype and high-grade morphology.
2014;45: 1084-1091[PMID: 24746215 DOI: 10.1016/j.humpath.2014.01.007]
杂志排行
World Journal of Clinical Cases的其它文章
- Capillary leak syndrome:A rare cause of acute respiratory distress syndrome
- lmproving outcomes in geriatric surgery:ls there more to the equation?
- Mass brain tissue lost after decompressive craniectomy:A case report
- Spinal canal decompression for hypertrophic neuropathy of the cauda equina with chronic inflammatory demyelinating polyradiculoneuropathy:A case report
- Enigmatic rapid organization of subdural hematoma in a patient with epilepsy:A case report
- Multiple stress fractures of unilateral femur:A case report