Treatment of condylar osteophyte in temporomandibular joint osteoarthritis with muscle balance occlusal splint and long-term follow-up:A case report
2022-06-23KaiWenLanJiaMinChenLiuLinJiangYiFanFengYingYan
lNTRODUCTlON
Temporomandibular joint osteoarthritis(TMJ OA)is a non-/low-inflammatory,progressive form of arthritis characterized by degenerative changes to the articular cartilage and the underlying bone,which can lead to pain,masticatory dysfunction,and maxillofacial deformity[1].Although its exact cause is still unclear,TMJ OA is usually associated with joint trauma and overload;when the stress and functional requirements of the joint area are not balanced with the normal adaptability of the host TMJ,dysfunctional remodeling can occur[2-5].The first choice of treatment for TMJ OA is usually nonsurgical,such as lifestyle/diet adjustments,splint therapy,systemic or intra-articular drug therapy,or physical therapy[1,6].Only when non-surgical treatment is ineffective and dysfunction and/or pain are moderate to severe is surgical treatment indicated[7].
Osteophytes are a dysfunctional-remodeling form of condyles in TMJ OA patients[8].Most researchers have observed that condylar osteophytes usually present as marginal angular outgrowths with sclerotic borders and a volume of usually < 1 mm
[8-11].Researchers have advocated surgical removal of condylar osteophytes.Dingman
[12]noted the recovery of bone physiological morphology in the joint area and advocated the use of arthroplasty to remove irregular osteophytes from the joint surface and remodel its shape.This case report describes a 68-year-old female TMJ OA patient with a rare osteophyte about 2 mm high on the top of the condyle.The patient refused surgical treatment and received conservative treatment with a muscle balance occlusal splint.The patient said that the pain on the left side of her face was relieved,and her ability to chew returned after treatment.The osteophytes dissolved,and the condylar cortex remained stable during long-term follow-up observations.Herein,we discuss the effect of the splint on condylar osteophytes in patients with TMJ OA and provide reference for clinical intervention into these osteophytes.
My father will then get very angry, and as the king must answer for what his fool does he will sentence him, even although he has paid his debt, either to answer three questions or to lose his life
CASE PRESENTATlON
Chief complaints
The patient was a 68-year-old woman who suffered from occlusal discomfort with left facial pain for 2 years.
History of present illness
The patient received splint treatment for left TMJ clicking 2 years ago.She complained that the clicking did not disappear,and she subsequently began to feel weakness in chewing,accompanied by left facial pain and difficulty in opening her mouth.
History of past illness
The patient had no history of systemic disease.
Personal and family history
The patient had no previous personal or familial history of TMJ OA.
The man was very sick, now. he crawled13 about, on hands and knees. He had lost everything—his blanket, his gun, and his gold. Only the wolf stayed with him hour after hour. At last he could go on no further. He fell. The wolf came close to him, but the man was ready. He got on top of the wolf and held its mouth closed. Then he bit it with his last strength. The wolf s blood streamed into his mouth. Only love of life gave him enough strength. He held the wolf with his teeth and killed it, then he fell on his back and slept.
Physical examination
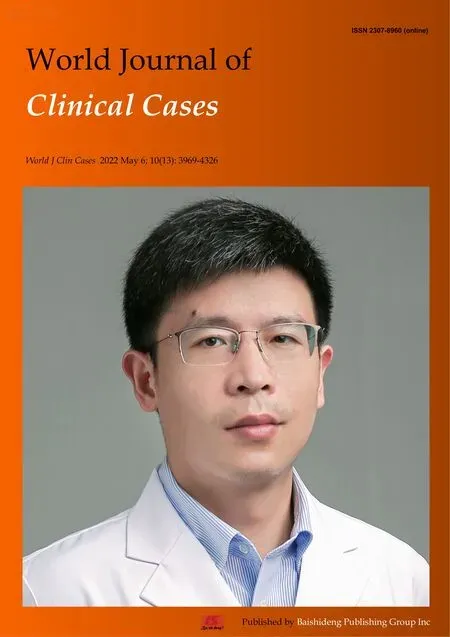
The patient was anxious and depressed.Her maxillofacial region was symmetrical.We found no tenderness on palpation of the bilateral external auditory canal and condyle region;the same was true of bilateral TMJ mobility.There was a rebound clicking sound at the left TMJ at the beginning of mouth opening and the end of mouth closing.The mandible deflected vertically when opening;the opening range was about 30 mm.There was no limitation of mandibular protrusive or lateral movement.Local pain was evoked by palpation of the left anterior and middle temporal muscles,the middle and posterior masseter muscles,the upper and middle sternocleidomastoid muscles,the trapezius muscles,and the medial pterygoid muscles.After the splint was placed in her mouth,the patient could not close her mouth while at rest.During centric occlusion,only the premolars were in point contact,and the remaining anterior and posterior teeth did not contact one another(Figure 1).
Laboratory examinations
To a child a hug says so many things. It tells you that the person hugging you loves you, cares for you. A hug also confirms that you are a lovable being. Months after Dad s death I realised with a jolt18 that his lack of hugs said more about him than me. My father was not a demonstrative man and I was, therefore, perhaps, a lovable being.
Imaging examinations
But I did. I was so weak my legs trembled. I could never have crossed that squirming deck if Benny hadn t supported me. The kid was stronger than he looked. He helped me down the steps and steered12 me to the bench where Dad was sitting with his head drooping13 on his chest.
When he became tired of searching for it he crept into the baking- oven, intending to lie down there and sleep till morning; but just at that moment he heard the witch calling from her bed to one of her daughters, and telling her to make some porridge for her
FlNAL DlAGNOSlS
Clinical diagnoses were:(1)TMJ disorder(TMD;masticatory-muscle dysfunction);and(2)Bilateral TMJ OA.
TREATMENT
When I was growing up I do not recall hearing the words I love you from my father. When your father never says them to you when you are a child, it gets tougher and tougher for him to say those words as he gets older. To tell the truth, I could not honestly remember when I had last said those words to him either. I decided1 to set my ego2(,) aside and make the first move. After some hesitation3, in our next phone conversation I blurted4 out the words, Dad… I love you!
OUTCOME AND FOLLOW-UP
One month later,the patient reported that her left facial pain had disappeared.At 3 mo,the patient’s mouth-opening range was improved(to about 35 mm).At 6 mo,the patient reported that her weakness in chewing had reduced and the pain had significantly relieved.She could chew both soft and crisp food.
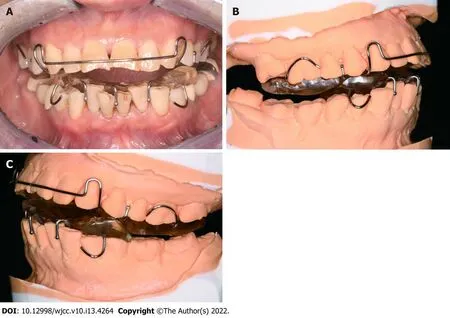
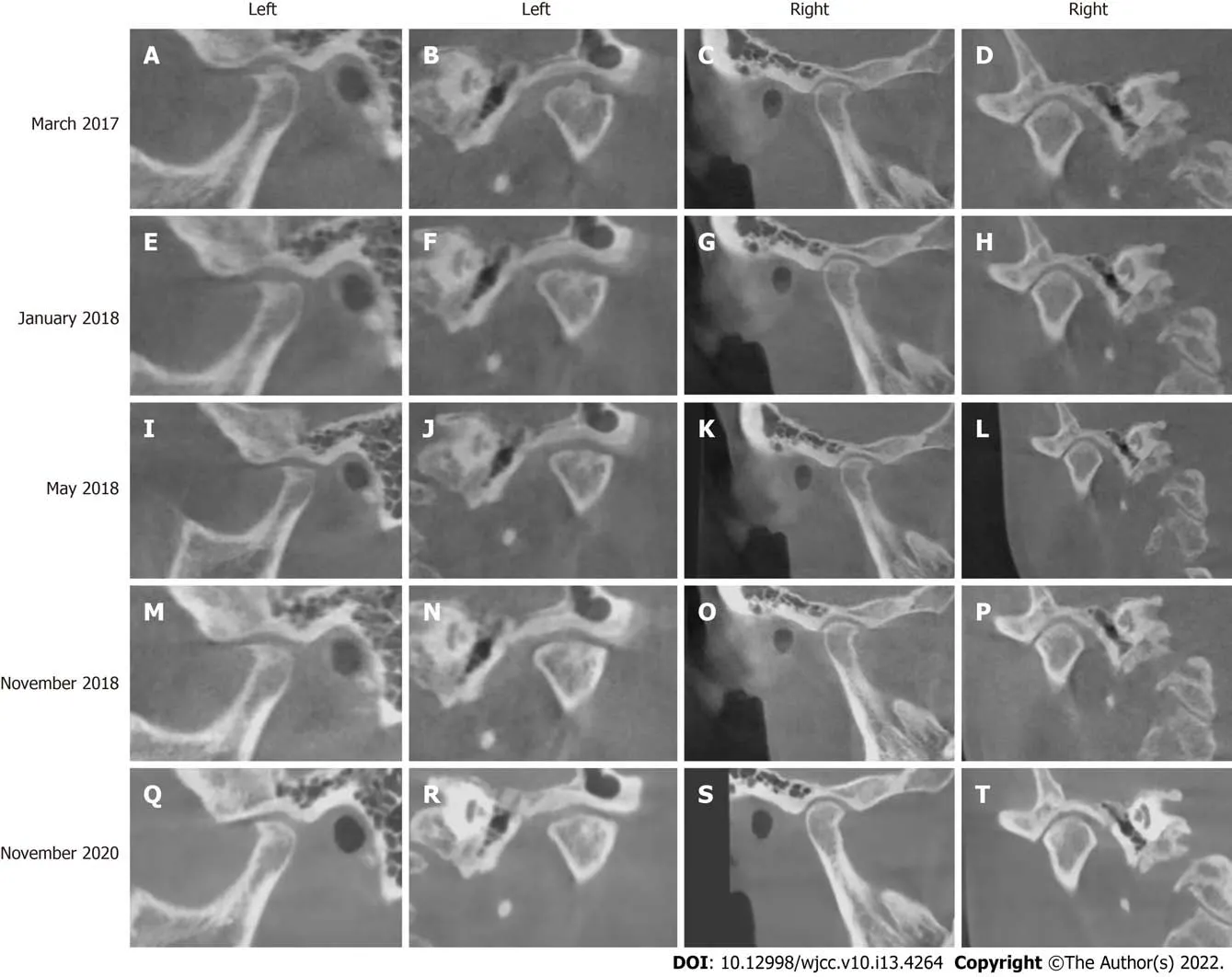
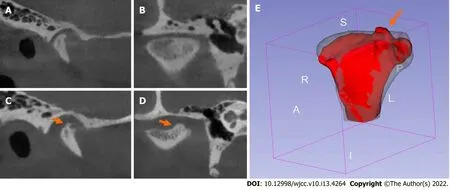
At 9 mo,the patient’s rebound clicking sound was reduced and weakened,and she had no discomfort from chewing or facial pain.CBCT re-examination of the TMJ showed that the left condylar top bone had become smooth and the cylindrical osteophyte had disappeared(Figure 4E-H).Threedimensional reconstruction and alignment of CBCT images before and after treatment can allow visualization of osteophyte dissolution(Figure 5).At 12 mo,the patient’s bilateral TMJ CBCT images(Figure 4I-L)were basically the same as those from the previous imaging session.
At 18 mo,the patient had no discomfort when chewing or speaking.Her bilateral TMJ CBCT images(Figure 4M-P)were basically the same as those from the previous imaging session.As the patient’s symptoms disappeared and the condylar cortex remained stable,we asked the patient to stop wearing the splint and be followed after 1 year.
Then a big fire was lit again, and the mother said: Just sit down there, children, and if you re tired you can sleep a bit; we re going into the forest to cut down wood, and in the evening when we re finished we ll come back to fetch you
At 3 years,the patient has not worn the splint for 1 year.We found no abnormality or discomfort in her TMJ or masticatory muscles.Bilateral TMJ CBCT showed that the bone conditions were basically the same as those from the previous imaging session(Figure 4Q-T).
A quiet pride settled over us as we sat on that play-ground bench, Ronny’s hand now in mine. I at once wept and marveled at the young boy beside me. What a powerful contribution the author of that Little Golden Book had made in the life of a disadvantaged child.


DlSCUSSlON
Large condylar osteophytes are relatively infrequent in TMJ OA patients.Alexiou
[8]studied the imaging features of 142 TMJs with OA and found that 26% of condyles had mild osteophytes < 1 mm,18% had moderate osteophytes 1 mm-2 mm,and only 12% had severe osteophytes > 2 mm.In this case,CBCT showed the formation of a 1 mm-2 mm,beak-like osteophyte at the front edge of the condyle.These imaging findings corresponded to the size of a moderate osteophyte reported in the literature[8].However,we could also observe a cylindrical osteophyte about 2 mm high at top center of the left condyle.Although Dingman
[12]have reported the existence of exostosis on the condylar surface,the location and morphology of condylar osteophytes in this situation have not been reported in the literature.
We cannot explain certain aspects of this case.The cause of osteophytic formation on top of the condyle was unclear.The patient had received treatment with a splint similar to the twin-block(TB)splint(Figure 1),but due to the lack of CBCT image comparisons before and after the splint treatment,we could not determine the relationship between such treatment and the osteophyte on top of her condyle.However,we have observed another case in which an adult patient with condylar resorption was treated with the TB splint and an osteophyte appeared on top of the condyle after treatment(Figure 6).In addition,the splint had different effects on the osteophyte in different condylar positions.Although the osteophyte on top of the condyle dissolved,the marginal osteophyte did not change significantly.Differences in stress in different areas of the joint might have caused the differences in bone remodeling.In future,the mechanical effect of the muscle balance occlusal splint on the joint should be explored in both basic and clinical research,so as to determine the effect of this splint therapy on condylar osteophytic remodeling.
The patient refused surgical treatment and began conservative treatment with a muscle balance occlusal splint(Figure 3)in June 2017.The splint was fixed to the maxillary dentition with clasps;its thickness was about 1.5 mm-2.0 mm at the central fossa of the maxillary first molar and about 3 mm-4 mm in the area of the anterior teeth.The occlusal surface of the splint was designed as a shallow concave structure that formed loose contact with the buccal and lingual cusps of the opposite teeth.The patient was asked to wear the splint all the time,except when eating,and followed every 1-3 mo for evaluation of symptoms and signs.At follow-ups,the clinician adjusted the occlusal surface of the splint so that it once again contacted both sides of the opposite dentition evenly during centric occlusion.
The effect of osteophytes on the TMJ is still controversial.According to Krisjane
[11],the establishment of marginal osteophytes enlarges and stabilizes the articular surface and helps support the loading forces.However,Lee
[13]believed that the extensive formation of osteophytes might lead to condylar deformity.Kirk
[14]analyzed the biomechanical principles of the TMJ and pointed out that osteophytes on the condylar surface and the lateral pole increase the shear force,which can damage the disc or capsule attachment.Li
[15]found that the higher the degree of osteophytic formation,the more serious the articular-cartilage destruction.We speculate that the cylindrical osteophyte in this case might have been the main disruptor of the disc-condylar relationship,thereby interfering with the mandibular functional movement.However,because we did not perform arthrography or magnetic resonance imaging(MRI)on this patient’s TMJ,we could not know the condition of the disc and capsule.
This case report suggests that the muscle balance occlusal splint could be a noninvasive means of treating condylar osteophytes in TMJ OA patients.The specific mechanism of the splint treatment on osteophytic remodeling is still unclear,and further basic and clinical research is needed.
The patient’s compliance was good,and no adverse events occurred at any point during the treatment.The patient was satisfied with the therapeutic effect of the muscle balance occlusal splint.After splint treatment began,she felt that her facial-muscle pain was gradually relieved,her masticatory function recovered,and her anxiety relieved.
Osteophytic remodeling is affected by mechanical factors,biochemical factors,and the synergy of their actions.The biomechanical load exerted on the TMJ affects the internal and external shapes of the joint[11].Overload is generally considered to be one of the main causes of TMJ OA[16,17].Based on the theory of quantitative bone remodeling,He G and Xinghua Z[18]simulated the formation of osteophytes and found that the change to the joint mechanical environment led to the formation of an osteophyte at the edge of the joint.Osteophytic formation is a process in which the joint adapts to the changing mechanical environment,although it can be pathological.Animal studies have shown that the biochemical factors such as inflammation and metabolic imbalance of articular chondrocytes led to the changes in the microenvironment,which promotes osteophytic formation.The use of drugs such as high-molecular-weight hyaluronic acid[15]and corticosteroids[19]has been proven to reduce osteophytic formation in experimental OA in animals.Li
[20]have published images of condylar osteophytic dissolution in patients with TMJ OA after injection of hyaluronic acid,which suggests that the formed osteophyte can still remodel after drug intervention.In this case,we used only the muscle balance occlusal splint and still observed dissolution of the osteophyte,indicating that occlusal-splint treatment might potentially affect condylar osteophytic remodeling.
Cone beam computed tomography(CBCT)performed in March 2017 showed that osteophytes had formed at the anterior margin of the bilateral condyles.A central cylindrical osteophyte 4 mm in diameter and 2 mm in height can be seen on top of the left condyle(Figure 2).
The effect of the splint on condylar osteophytes might be due to changes to the mechanical environment of the joint.An anterior repositioning splint(ARS)has been reported to promote condylar osteogenesis.The reason might be that the ARS guides mandibular advancement and joint disc repositioning;the condylar cartilage is subject to tensile stress,leading to adaptive condylar remodeling[21].The change to the bone mechanical environment is accompanied by changes to the bone structure and shape,which force the bone to adapt to the new mechanical environment[18].Previous reports on the effect of occlusal splint on TMJ OA patients’ joint bone mostly focused on treatment with this splint,which can reduce absorption of the affected condyle and promote repair and regeneration[6,22-24].The advantage of the occlusal splint(especially the stable occlusal splint)lies in the stability of occlusion and the uniform distribution of TMJ overload[25].In patients with TMJ OA,overload to the TMJ is reduced,thereby reducing bone resorption of the joint[6].However,the splint’s effect on the dissolution of condylar osteophytes has not yet been reported.
Perhaps something may come of it! At these words Catherine dried her eyes, and next morning, when she climbed the mountain, she told all she had suffered, and cried, O Destiny, my mistress, pray, I entreat you, of my Destiny that she may leave me in peace
The patient did not undergo laboratory examination.
CONCLUSlON
Surgical treatment is the traditional intervention for condylar osteophyte.Kirk
[14]pointed out that the use of arthroplasty to remove osteophyte can reduce disc-condylar relationship disorder and tissue damage in the articular cavity.Although arthroplasty may relieve symptoms,the long-term effects of surgical changes on TMJ remodeling and the function of stomatognathic system are still unclear[1].In this case,the patient refused surgical treatment.We used a muscle balance occlusal splint for noninvasive treatment.TMJ is a bilaterally linked joint and needs to be balanced bilaterally to achieve a healthy state.Muscle coordination and balance are also concerns.Clinically,the balance of the muscles in patients with masticatory muscle dysfunction is disrupted.The muscles are considered to have reached a balanced state when clinical symptoms,such as pain,disappear.The muscle balance occlusal splint treatment is designed to guarantee stability of occlusion and jaw position,to avoid restricting the jaw position without affecting muscle memory and to allow the masticatory muscle to gradually achieve a balanced state at follow-up visits.
FOOTNOTES
Yan Y,Lan KW,Chen JM,Jiang LL,and Feng YF examined the patient and collected the clinical data;Lan KW,Chen JM,Jiang LL,and Feng YF wrote the manuscript;Yan Y edited the manuscript and approved the final version.
Informed consent was obtained from the patient for publication of this report and any accompanying images.
All authors own a patent(No.ZL 202120549626.3,CN)describing the design of the muscle balance occlusal splint,as well as its treatment application for temporomandibular joint disorder and bruxism.The patent is licensed to Hospital of Stomatology,Sun Yat-sen University.
The authors have read the CARE Checklist(2016),and the manuscript was prepared and revised according to the CARE Checklist(2016).
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial(CC BYNC 4.0)license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
China
Kai-Wen Lan 0000-0002-2239-4130;Jia-Min Chen 0000-0001-6059-4881;Liu-Lin Jiang 0000-0001-9570-995X;Yi-Fan Feng 0000-0003-3070-1492;Ying Yan 0000-0002-3134-2463.
Xing YX
Wang TQ
Xing YX
1 Renapurkar SK.Surgical Versus Nonsurgical Management of Degenerative Joint Disease.
2018;30: 291-297[PMID: 30008342 DOI: 10.1016/j.coms.2018.04.005]
2 Tanaka E,Detamore MS,Mercuri LG.Degenerative disorders of the temporomandibular joint: etiology,diagnosis,and treatment.
2008;87: 296-307[PMID: 18362309 DOI: 10.1177/154405910808700406]
3 Milam SB.Pathogenesis of degenerative temporomandibular joint arthritides.
2005;93: 7-15[PMID:16170470 DOI: 10.1007/s10266-005-0056-7]
4 Arnett GW,Milam SB,Gottesman L.Progressive mandibular retrusion--idiopathic condylar resorption.Part I.
1996;110: 8-15[PMID: 8686682 DOI: 10.1016/S0889-5406(96)70081-1]
5 Arnett GW,Milam SB,Gottesman L.Progressive mandibular retrusion-idiopathic condylar resorption.Part II.
1996;110: 117-127[PMID: 8760837 DOI: 10.1016/S0889-5406(96)70099-9]
6 Ok S,Jeong S,Ahn Y,Kim Y.Effect of stabilization splint therapy on glenoid fossa remodeling in temporomandibular joint osteoarthritis.
2016;60: 301-307[PMID: 27026211 DOI: 10.1016/j.jpor.2016.03.001]
7 Bouloux G,Koslin MG,Ness G,Shafer D.Temporomandibular Joint Surgery.
2017;75: e195-e223[PMID: 28728730 DOI: 10.1016/j.joms.2017.04.027]
8 Alexiou K,Stamatakis H,Tsiklakis K.Evaluation of the severity of temporomandibular joint osteoarthritic changes related to age using cone beam computed tomography.
2009;38: 141-147[PMID: 19225084 DOI:10.1259/dmfr/59263880]
9 Massilla Mani F,Sivasubramanian SS.A study of temporomandibular joint osteoarthritis using computed tomographic imaging.
2016;39: 201-206[PMID: 27621122 DOI: 10.1016/j.bj.2016.06.003]
10 Lim MJ,Lee JY.Computed tomographic study of the patterns of oesteoarthritic change which occur on the mandibular condyle.
2014;42: 1897-1902[PMID: 25240743 DOI: 10.1016/j.jcms.2014.07.009]
11 Krisjane Z,Urtane I,Krumina G,Neimane L,Ragovska I.The prevalence of TMJ osteoarthritis in asymptomatic patients with dentofacial deformities: a cone-beam CT study.
2012;41: 690-695[PMID: 22464854 DOI: 10.1016/j.ijom.2012.03.006]
12 Dingman RO,Grabb WC.Intra-capsular temporomandibular joint arthroplasty.
1966;38: 179-185[PMID: 5919600 DOI: 10.1097/00006534-196609000-00001]
13 Lee PP,Stanton AR,Hollender LG.Greater mandibular horizontal condylar angle is associated with temporomandibular joint osteoarthritis.
2017;123: 502-507[PMID: 28189528 DOI:10.1016/j.oooo.2016.12.008]
14 Kirk WS Jr,Kirk BS.A biomechanical basis for primary arthroplasty of the temporomandibular joint.
2006;18: 345-368,vi[PMID: 18088837 DOI: 10.1016/j.coms.2006.03.006]
15 Li P,Raitcheva D,Hawes M,Moran N,Yu X,Wang F,Matthews GL.Hylan G-F 20 maintains cartilage integrity and decreases osteophyte formation in osteoarthritis through both anabolic and anti-catabolic mechanisms.
2012;20: 1336-1346[PMID: 22809835 DOI: 10.1016/j.joca.2012.07.004]
16 Lin YY,Tanaka N,Ohkuma S,Iwabuchi Y,Tanne Y,Kamiya T,Kunimatsu R,Huang YC,Yoshioka M,Mitsuyoshi T,Tanimoto K,Tanaka E,Tanne K.Applying an excessive mechanical stress alters the effect of subchondral osteoblasts on chondrocytes in a co-culture system.
2010;118: 151-158[PMID: 20487004 DOI:10.1111/j.1600-0722.2010.00710.x]
17 Nishioka M,Ioi H,Matsumoto R,Goto TK,Nakata S,Nakasima A,Counts AL,Davidovitch Z.TMJ osteoarthritis/osteoarthrosis and immune system factors in a Japanese sample.
2008;78: 793-798[PMID:18298222 DOI: 10.2319/091407-438]
18 He G,Xinghua Z.The numerical simulation of osteophyte formation on the edge of the vertebral body using quantitative bone remodeling theory.
2006;73: 95-101[PMID: 16253537 DOI: 10.1016/j.jbspin.2005.03.019]
19 Pelletier JP,Martel-Pelletier J.Protective effects of corticosteroids on cartilage lesions and osteophyte formation in the Pond-Nuki dog model of osteoarthritis.
1989;32: 181-193[PMID: 2920053 DOI:10.1002/anr.1780320211]
20 Li C,Long X,Deng M,Li J,Cai H,Meng Q.Osteoarthritic changes after superior and inferior joint space injection of hyaluronic acid for the treatment of temporomandibular joint osteoarthritis with anterior disc displacement without reduction: a cone-beam computed tomographic evaluation.
2015;73: 232-244[PMID: 25579006 DOI: 10.1016/j.joms.2014.08.034]
21 Ma Z,Xie Q,Yang C,Zhang S,Shen Y,Abdelrehem A.Can anterior repositioning splint effectively treat temporomandibular joint disc displacement?
2019;9: 534[PMID: 30679602 DOI: 10.1038/s41598-018-36988-8]
22 Lei J,Yap AU,Liu MQ,Fu KY.Condylar repair and regeneration in adolescents/young adults with early-stage degenerative temporomandibular joint disease: A randomised controlled study.
2019;46: 704-714[PMID:31009097 DOI: 10.1111/joor.12805]
23 Ok S,Lee J,Kim Y,Kim K B,Jeong S.Anterior condylar remodeling observed in stabilization splint therapy for temporomandibular joint osteoarthritis.
2014;118: 363-370[PMID:25151591 DOI: 10.1016/j.oooo.2014.05.022]
24 Cuccia AM,Caradonna C.Condylar growth after non-surgical advancement in adult subject: a case report.
2009;5: 15[PMID: 19619334 DOI: 10.1186/1746-160X-5-15]
25 Hasegawa Y,Kakimoto N,Tomita S,Fujiwara M,Ishikura R,Kishimoto H,Honda K.Evaluation of the role of splint therapy in the treatment of temporomandibular joint pain on the basis of MRI evidence of altered disc position.
2017;45: 455-460[PMID: 28238557 DOI: 10.1016/j.jcms.2017.01.011]
杂志排行
World Journal of Clinical Cases的其它文章
- Capillary leak syndrome:A rare cause of acute respiratory distress syndrome
- lmproving outcomes in geriatric surgery:ls there more to the equation?
- Mass brain tissue lost after decompressive craniectomy:A case report
- Primary intracranial extraskeletal myxoid chondrosarcoma:A case report and review of literature
- Spinal canal decompression for hypertrophic neuropathy of the cauda equina with chronic inflammatory demyelinating polyradiculoneuropathy:A case report
- Enigmatic rapid organization of subdural hematoma in a patient with epilepsy:A case report