Sparing lung tissue with virtual block method in VMAT planning for locally advanced non-small cell lung cancer
2022-06-18JiaYunChenDaQuanWangXiaoDongZhangQiFuXueNaYanKuoMenJianRongDaiNanBi
Jia-Yun Chen· Da-Quan Wang,2 · Xiao-Dong Zhang · Qi Fu ·Xue-Na Yan · Kuo Men · Jian-Rong Dai· Nan Bi
Abstract This study aimed to exploit a new virtual block method to spare normal lung tissue in VMAT planning for patients with locally advanced non-small cell lung cancer(LA-NSCLC). The previous method was used to manually restrict the angle of the beam passing through, which ignored the location and shape of large targets that varied between different slices and did not block the beamlets precisely. Unlike the previous method, this new virtual block method was used to block the beamlets when necessary by closing the multi-leaf collimator (MLC) at prerequisite angles. The algorithm for closing the MLC depended on the thickness of the beamlets passing through the lungs and avoided only the entrance radiation beamlet.Moreover, this block can be automatically contoured. A retrospective study was performed to compare the VMAT plans with and without the virtual block method for 17 LANSCLC patients,named the block plan(B-plan)/non-block plan(N-plan).All cases were selected in this study because of the large tumor size and unmet dose constraints of the lungs. In addition to the maximum dose constraint for the virtual block, B-plans adopted identical optimization parameters to N-plans for each patient. These two types of plans were compared in terms of dosimetric indices and plan scores. The results were statistically analyzed using the Wilcoxon nonparametric signed-rank test.B-plans have advantages in the following dosimetric metrics that have statistical significance (p <0.05): (1) lower V5/V10/Dmean/normal tissue complication probability (NTCP) of total lungs; (2) reductions in V5/V10 for the contralateral lung;(3) decrease in Dmean/V40 of the heart; (4) decrease in esophagus V40; (5) reductions in Dmean, V5/V10 of normal tissue. B-plans (82.51 ± 7.07) achieved higher-quality scores than N-plans(80.74 ± 7.22).The new virtual block spared the lungs as well as other normal structures in VMAT planning for LA-NSCLC. Thus, the block method may decrease the risk of radiation-related toxicity in patients.
Keywords Virtual block·VMAT·Normal tissue sparing·Lung cancer
1 Introduction
More than 30% of patients with non-small cell lung cancer(NSCLC)are diagnosed at a locally advanced stage[1]. Definitive radiotherapy (RT) combined with chemotherapy remains the standard treatment for these patients, with a 5-year overall survival (OS) of 20–30%[2, 3]. Intensity-modulated radiation therapy (IMRT) has been routinely used in the RT of patients with locally advanced NSCLC (LA-NSCLC) in the past two decades and has been confirmed to be superior to 3D-CRT in terms of retaining local control and reducing pulmonary toxicity[4]. In recent years, volumetric modulated arc therapy(VMAT), a newly advanced RT technique, has been adopted for LA-NSCLC RT. VMAT notably decreases the treatment delivery time compared with IMRT [5] because it allows beam-on when the gantry position, multi-leaf collimator (MLC) moves, and dose rate simultaneously vary [6].
However, one concern is the low irradiation dose to normal tissues using the VMAT technique, especially for LA-NSCLC patients with a large tumor size. Previous studies have demonstrated that VMAT plans can achieve higher degrees of conformity and homogeneity in the target dose than fixed-field IMRT [7–9]. Jiang et al. [7] and Zhang et al.[10]found that VMAT plans achieved a lower 20 Gy/30 Gy dose volume (V20/V30) and mean lung dose(MLD) in both lungs and contralateral lungs, but a higher 5 Gy/10 Gy dose volume (V5/V10) compared to IMRT plans.Despite the great advantage of the VMAT technique,VMAT plans result in higher lung V5and V10compared to traditional IMRT plans [7, 10], which might increase the risk of symptomatic radiation pneumonitis [11, 12]. Radiation pneumonitis(RP),caused by thoracic RT,is the main dose-limiting complication in LA-NSCLC. Ren et al.indicated that lung V5and MLD were independent predictors of RP grade ≥3 [13]. Another study reported that lung V10was an independent factor for predicting symptomatic RP among lung cancer patients who underwent VMAT as RT[14].Several reports recommend keeping V5of the total lung below 60–65%in RT plans of LA-NSCLC patients with concurrent chemotherapy [15, 16]. Thus,normal lung tissue sparing has raised great interest in VMAT planning design, especially in the low-dose range(5–10 Gy) of normal lung tissue.
The virtual block method has been used in helical tomotherapy (HT) planning (Accuray, Sunnyvale, CA) to reduce the lung dose.Makoto et al.[17]made plans with a virtual block structure in HT for 15 patients with cervical esophageal carcinoma and found that V5, V10, and V20of the lungs and MLD dose were significantly reduced in B-plans. Hong et al. [18] optimized beam angles in tomotherapy by applying directional/complete block functions for ten patients with stage IIIB NSCLC and found that the plan with virtual block had superior normal lung sparing compared to Linac-based static IMRT plans.However, to the best of our knowledge, this virtual block method has not been implemented in VMAT plans. In addition, the block currently used by Makoto [17] in HT was generated considering only the beamlet direction and the lungs, but omitting the changes in tumor targets between different computed tomography (CT) slices.Concurrently, tomotherapy provides the directional/complete block function: (1) The directional block function closes the beamlet and limits the entrance direction of beamlets when the blocked structure is proximal to the targets and (2) the complete block function blocks the beamlets from entering and exiting a certain blocked structure volume [19].
Currently,commercial treatment planning system(TPS)manually restricts the angle of the beam passing through the lungs in VMAT planning to reduce the low-irradiationdose volume to the lungs. For example, Eclipse (Varian Medical Systems,Palo Alto,CA)[20,21]could restrict the beam angle using arc avoidance sectors for predefined fixed arcs, whereas Pinnacle (Philips Radiation Oncology Systems, Fitchburg, WI) [22] adopted several partial arcs instead of the full arc.This method ignores the location and shape of targets that vary between different slices and does not block the beamlets precisely. Thus, we invented a new virtual block method to block the beamlets by closing the MLC at prerequisite arc angles and first introduced the block as an optimization objective in the VMAT optimization process. This new virtual block with proper optimization objectives in the VMAT planning system could provide a function like that of the directional/complete block in the HT planning system.
In the present work, we have exploited a new virtual block contouring method and optimization parameter to generate VMAT plans, taking tumor location and shape,normal lung, and beamlet direction into account. We also report the feasibility and efficacy of block objects in reducing the lung dose when making VMAT plans for LANSCLC.
2 Experimental section
2.1 Patients and characteristics
Seventeen patients with stage III NSCLC were treated between January 1, 2014, and December 31, 2015, in our cancer center.These patients were retrospectively enrolled,and their characteristics are listed in Table 1. All the tumors were located in the left lung.Two(11.8%)patients had stage IIIA disease, and 15 (88.2%) had stage IIIB disease. The median total lung volume for the 17 patients was 3595 cm3(range 2191–4693 cm3). The median planning target volume (PTV) and planning gross tumor volume (PGTV) were 467 cm3and 122 cm3, respectively.

Table 1 The clinical characteristics of patients
2.2 Immobilization and simulation
The immobilization position for the patients was supine with a chest/head-neck-shoulder mask. The CT simulation was a four-dimensional 5-mm-thickness slice CT scan.The extent of the scanned area was from the atlas to the second lumbar[23]vertebra level.The CT images were sent to the Pinnacle3version 9.10 TPS for delineation and VMAT planning (Philips Radiation Oncology System, Fitchburg,WI, USA).
2.3 The delineation of targets and organs at risk(OAR)
The targets and OAR volumes were contoured by trained radiation oncologists in reference to the guidelines of the Radiotherapy and Oncology Group (RTOG). The gross tumor volume(GTV)consisted of the primary tumor and positive lymph nodes;more details can be found in the references [23, 24]. The clinical target volume (CTV) was created as an expansion of the GTV by 0.6–0.8 cm and contained the ipsilateral hilum and involved mediastinum lymph node stations. The PTV was generated using a margin of 0.5 cm around the CTV.The PGTV was created by GTV with a 0.6-cm margin. PTV-PGTV was defined as the region remaining in the PTV after removing the PGTV plus a 0.5-cm margin.
The total lung (lung all, GTV), spinal cord, heart, and esophagus were contoured as the critical OARs for the dose constraint listed in Table 2. Planning organ-at-risk volume(PRV)was generated by a uniform 5-mm expansion of the spinal cord, named spinal cord PRV [25]. Normal tissue(NT) displayed the external contour of the patient’s body minus the PTV,as in Ref.[26],which was used to evaluate the low-dose area surrounding the PTV.
2.4 Prescribed dose and dose constraints
The prescribed doses to PGTV and PTV were 60.2 Gy and 50.4 Gy in 28 daily fractions. At least 95% of the PGTV/PTV received 95% of the prescribed dose (60.2/50.4 Gy). The planning objectives were to comply with great conformity for both targets (PGTV and PTV), while satisfying the homogeneity of PGTV and PTV-PGTV.The maximum dose (Dmax) of the spinal cord and spinal cord PRV should not exceed 40 and 45 Gy, respectively.The MLD should be less than 20 Gy. The V20/V30of the total lung should be less than 30% and 20%, respectively.The V30/V40ratio of the heart was constrained to less than 40%/30%.
2.5 Virtual block method
The virtual block method was introduced to decrease the low-dose exposure of the lung in the VMAT plans, which blocked the beamlets by closing the MLC at certain angles.The principle of closing the MLC depends on the thickness of the beamlets passing through the lungs,especially in the lateral direction, to spare the exposure of the OARs. A partial ring virtual block was determined to only avoidentrance radiation beamlets and was contoured with the scripting tool provided by Pinnacle.
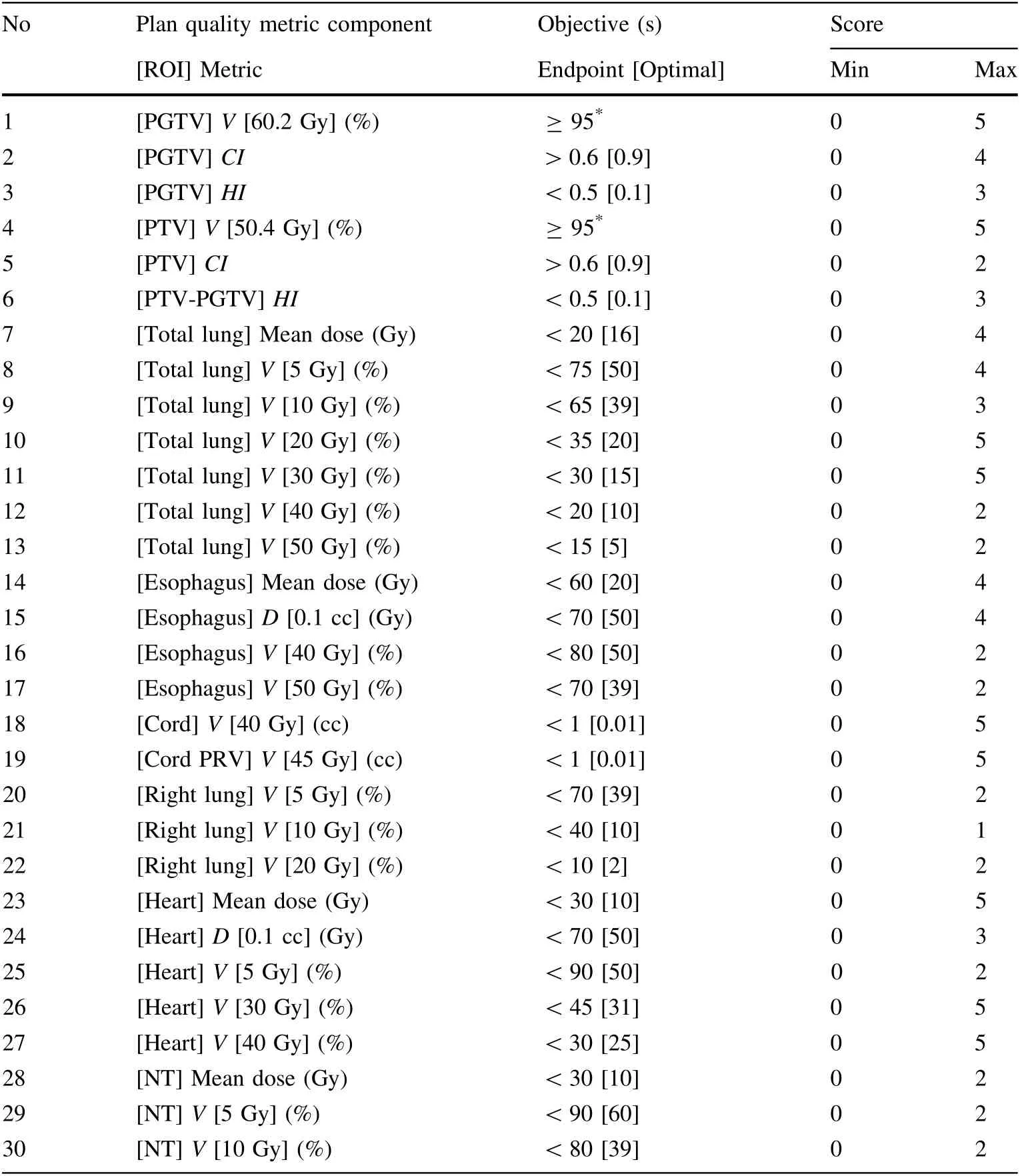
Table 2 Description of plan quality metrics (PQM)
This type of block has several advantages. First, the PTV shape with large variances between the slices was considered. Unlike the previous method, which shielded beamlets by reducing the beam angles, this new virtual block was determined by the following principles: (1) the proximity of the MLC depended on the thickness of the beamlets passing through the lungs; (2) avoiding only entrance radiation beamlets; (3) maintaining a minimum distance of 8 cm away from the PTV in the left and right directions,which avoided beam interference;(4)adding the maximum dose constraint for the virtual block in VMAT optimization; and (5) the virtual block could be contoured automatically.
The contouring algorithm and process are illustrated in Fig. 1 as follows: (1) a supporting structure, denoted as PTV-extend, was created by adding an 8-cm margin to the PTV in the left–right direction and a 20-cm margin in the anterior–posterior direction. The PTV-extension is represented by the solid dark blue line in Fig. 1a–3a. The expansion direction is indicated by the light blue arrow in Fig. 1a–3a, and these expansion distances were based on our clinical experience. (2) A supporting structure, called Outline, was the external sketch of the patient’s body and only in the body where PTV was presented.(3)Thereafter,a structure was created by contracting outline with 1 cm.This structure is denoted as a ring-outline and is shown as a hollow bright yellow line in Fig. 1b–3b. (4) Finally, a partial ring was generated by removing the ring outline part in the PTV-extension. This partial ring is named the ring
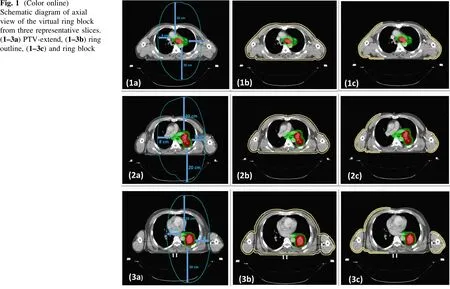
Fig. 1 (Color online)Schematic diagram of axial view of the virtual ring block from three representative slices.(1-3a) PTV-extend, (1-3b) ring outline, (1-3c) and ring block
block (hereafter, ‘‘block’’). A ring block is present in the hollow bright yellow area in Fig. 1c–3c.
2.6 Plan method
Two VMAT plans were designed for each patient,including a non-block plan (N-plan) and a block plan (Bplan).The N-plan was designed with optimized parameters using the mdaccAutoPlan system [27]. The mdaccAuto-Plan system was modified based on our clinical planning strategy, under the guidance of the developer’s team. The initial objective functions were loaded into the Pinnacle3TPS, as listed in Table 3. The mdaccAutoPlan system was used to achieve optimal PTV coverage.Then,the weight of the OAR (such as the total lungs, spinal cord, esophagus,and heart) constraint in the objective function was increased, and the plan was reoptimized to generate improved OAR sparing. Finally, two-to-three rounds of optimization were performed to eliminate hot/cold spots after adding an objective of automatically generating contours of hot/cold spots. More details of the mdaccAutoPlan algorithm can be found in the references [27, 28].
The quality might vary widely if the plans were made by different planners [30]; thus, the application of an automated planning system could effectively reduce the interoperator variability [31] and ensure the high quality of VMAT plans for our study [28]. The B-plan adopted identical optimization parameters to the N-plan for each patient, in addition to the new optimization parameters for the virtual block structure:Dmax<5 Gy.Our optimization goal of B-plans was to increase the volume of normal lung tissue without compromising the homogeneity and conformity of the targets (PTV and PGTV). The primary optimization weight for the ring block was initially set to 10 and could be adjusted to 20 (maximum weight value)step-by-step according to the composite object values in the Pinnacle. For some lung cancer patients, the values of total lung V5could easily meet the clinical goal, as we added the ring-block constraint. However, the total lung V20/V30increased slightly. Stricter constraints of the total lung V20/V30were added in the B-plan to achieve the clinical goal.
In our study, 6-MV photons were used to calculate the VMAT plans,and 600 MU/min remained as the maximum variable dose rate. The same isocenter was shared by double coplanar partial arcs of 340°–180°, with two opposite clockwise and counterclockwise rotations being applied.Two arcs with rotated collimators of 10°and 350°were used to avoid tongue and groove effects,respectively.The rotation time for each arc was limited to 120 s to ensure that the leaf could travel rapidly. The gantry anglespacing was set at 4°. The calculated voxel size of all the plans was isotopically 4 mm.

Table 3 Initial objectives of mdaccAutoPlan which loaded into the Pinnacle inverse optimization planning system for locally advanced nonsmall cell lung cancer

Table 3 continued
2.7 Comparison of B-plans and N-plans
Both PGTV and PTV dose coverage were evaluated using the following metrics:(1)Vpis the volume receiving at least the prescribed dose; (2) conformity index (CI) is defined as follows: CI = (TVRITVRI)/(TVVRI), where TV is the target volume, TVRIis the target volume irradiated by the 95%prescribed dose,and VRIis the area covered by the 95%prescribed isodose line[32].The CI ranged from 0 to 1,and the best target conformity was obtained when the CI value was 1. (3) The homogeneity index (HI) was defined as follows:HI = (D2%–D98%)/D95%,where Dv%is the dose at V% of the target [33]. Better dose homogeneity was achieved when the HI was close to 0.OARs were evaluated using the following parameters: (1) lungs: MLD and lungs V5–V50; (2) esophagus: Dmeanand D0.1cc(dose at 0.1 cc),V40/V50; (3) heart: Dmeanand D0.1cc, V5, V30, and V40; (4)right lung: V5, V10, and V20; (5) spinal cord: volume receiving 40 Gy (V40); (6) spinal cord PRV: volume receiving 45 Gy (V45); (7) NT: Dmean, V5, and V10.
The plan scores launched by the ESTRO QUASIMODO group [34] were used to estimate the quality of plans. A multicenter study executed by Nelms BE confirmed the accuracy and objectivity of this scoring system [31].Because more predefined structures were included in this study than those in the references [23, 26], dosimetric metrics were extracted from the collected plans and used to compare the corresponding dose objectives listed in Table 2.To evaluate the achievement of specific plan goals in the references[25,26],30 components were included in the PQM from PlanIQTMsoftware (Sun Nuclear, Melbourne,FL,USA),with a full score of 100.The objectives were used to calculate the point value for every metric,and the descriptions are presented in Table 4.For example, for the total lung V5, the plan quality score was zero with V5≥75%and four with V5≤50%.If the value of V5was 65%, the plan quality score was calculated as follows:(75–65%)/(75–50%) × 4 = 1.6.
We also calculated the radiation pneumonitis probability for each plan using the NTCP model, which originated from the Lyman–Kutcher–Burman model.NTCP is defined by the following equation [35]:

where Deffis the equivalent uniform dose that will result in the same NTCP as the actual nonuniform dose distribution if delivered uniformly to the entire volume.The TD50is the uniform dose delivered to the organ,leading to a 50%risk of complications. n is the magnitude of the volume effect and viis the volume related to the dose voxel Di. m is the slope of the curve,represented by the integral of the normal distribution.The Pinnacle system defined the following for the lungs: TD50= 24.5 Gy, m = 0.18, and n = 0.87 [36].
2.8 Statistical analysis
Plan quality scores and dosimetric metrics are presented as the average ± standard deviation. Comparisons of dosimetric metrics between the two plans were performed using the Wilcoxon nonparametric signed-rank test. Statistical significance was set at P <0.05.Statistical analysis was performed using the SPSS software of SPSS version 22.0; IBM, USA).

Table 4 Comparison of dosimetric metrics between B-plans and N-plans
3 Results and discussion
Totally, 34 plans were designed according to the protocol. Figure 2 shows the transverse sections of both the N-plan (a1-d1 panel of Fig. 2) and B-plan (a2-d2 panel of Fig. 2) with irradiation dose curves for one patient. As displayed in the left and right panels of Fig. 2, V5and V10of the total lungs in B-plan were apparently smaller than those in the N-plan. The conformity of the 95% isodose line of the PGTV (60.2 Gy) and PTV (50.4 Gy) in the B-plan was as good as that in the N-plan. A few hot spots(66 Gy)were observed in the B-plan,whereas invisible hot spots were observed in the N-plan.
Representative VMAT plans for a patient with dosevolume histograms(DVHs)of targets and OARs from both the N-plans (solid line) and B-plans (dashed line) are shown in Fig. 3. PGTV and PTV achieved 95% of the prescribed doses in both plans. N-plan produced a steeper DVH of PGTV than B-plan in the 102–107% range of the prescribed dose, yet the area of PGTV receiving 110% of the prescription dose was quite small. Regarding the selected OARs, the normalized percentage volume of the total lung in the B-plan was smaller than that in the N-plan at doses below 20 Gy. A similar numerical trend was observed in the DVH of the right lung. The V20Gyof the heart in the B-plan was notably lower than that in the N-plan. Interestingly, the tracheal area receiving a <50 Gy dose in the B-plan was less than that in the N-plan. Although the near-maximum-absorbed dose of the cord was comparable between the block and N-plans, the percentage volume of the cord receiving doses of 10–30 Gy in the B-plan was higher than that in the N-plan.The volume of the left lung receiving a dose of 20–30 Gy in the B-plan was slightly higher than that in the N-plan.
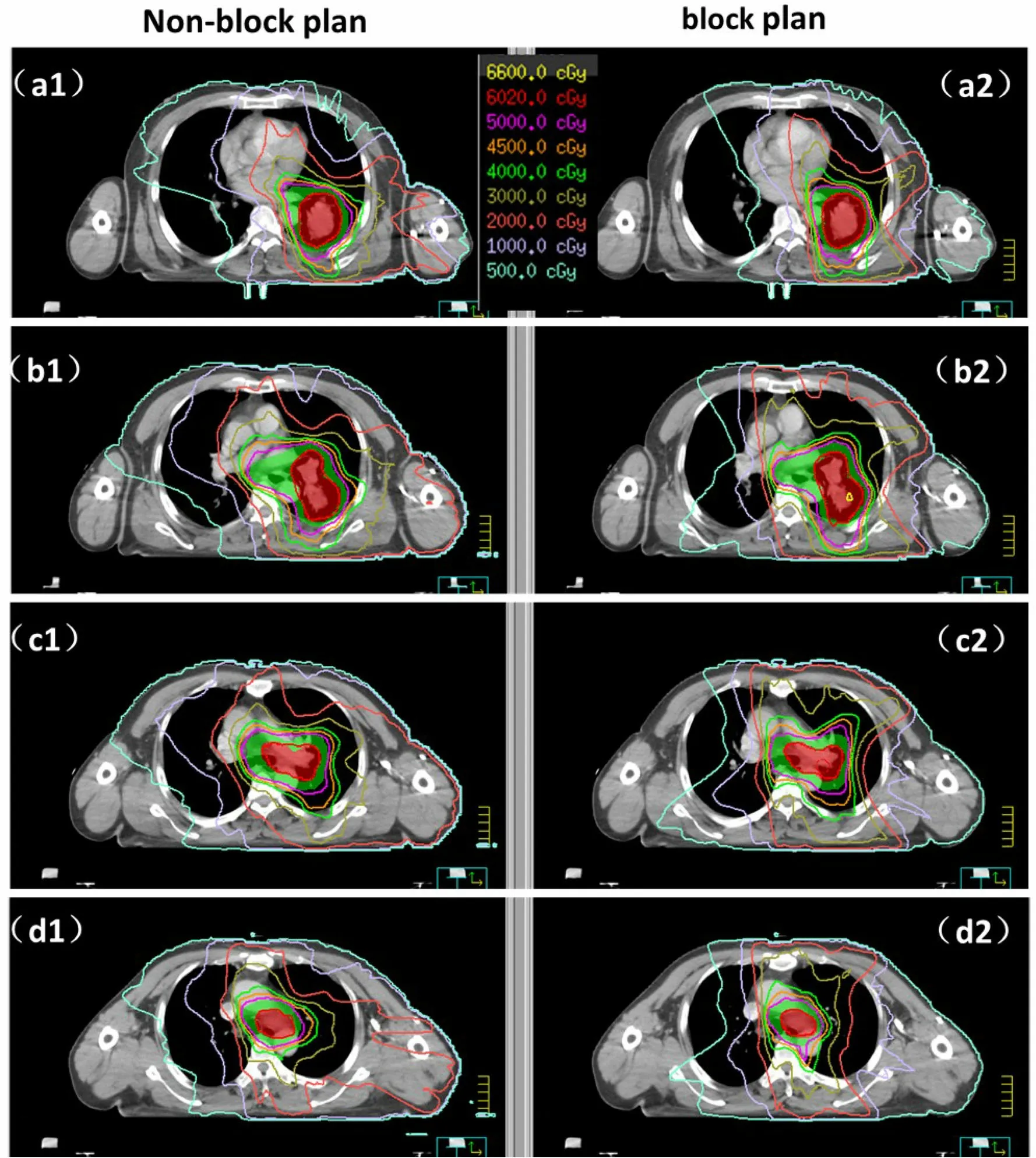
Fig. 2 (Color online) Transverse sections of the representative N-plans(left four panel)and B-plans(right four panel)of one patient with isodose lines. The dose distributions show planning target volume (PGTV and PTV) prescribed to 60.20 Gy (red line) and 50.40 Gy (purple line). The yellow, orange, green, bronze, pink,lavender, and indigo blue lines represent the dose curve of 66 Gy,45 Gy, 40 Gy, 30 Gy, 20 Gy, 10 Gy, and 5 Gy, respectively
3.1 Dose coverage of PGTV and PTV
Both B-plans and N-plans achieved sufficient dose coverage in the target volume.The mean V60.2of PGTV for N-plans and B-plans were 96.04 ± 0.64% and 96.21 ± 0.89% (P = 0.227), respectively. For PTV, the mean Vpwere 99.28 ± 0.56% and 98.56 ± 1.16%(P = 0.004), respectively. N-plans and B-plans showed similar conformity of the target volume, with a CI of 0.77 ± 0.05 and 0.76 ± 0.05 (P = 0.193) for PGTV, as well as 0.74 ± 0.05 and 0.74 ± 0.062 (P = 0.981) for PTV.N-plans achieved lower HI values in both targets than B-plans for PGTV (0.09 vs. 0.1, P = 0.003) and PTVPGTV (0.16 vs. 0.18, P = 0.003).

Fig. 3 (Color online) The DVH comparison between N-plan (solid lines)and B-plans(dashed lines)for one patient include the following selected ROIs:PTV(green),PGTV(red),total lungs(dark green),left lung (violet), right lung (dark blue), esophagus (yellow green), heart(brown), trachea (sky blue), and spinal cord (beige)
3.2 Plan quality score
B-plans had higher plan quality scores comparing with N-plans (mean: 82.51 ± 7.07 vs. 80.74 ± 7.22,P <0.001). This indicates that the quality of the plan was improved with the addition of a virtual block. The number of plans (23.5%) that scored above 90 in the block group was higher than that in the non-block group (11.8%),although the difference was not statistically significant.
3.3 Pulmonary dose
As listed in Table 4 and presented in Fig. 4, some dosimetric metrics of the total lungs have significantly statistically reduced as follows: (1) V5decreased from 63.3 ± 7.36% in N-plans to 59.26 ± 7.84% in B-plans(P <0.001), with a median numeric decreased proportion of 5.1% (0.1–18.8%); (2) V10decreased from 44.41 ± 7.49% in N-plans to 40.68 ± 6.58% in B-plans(P <0.001), with a median numeric decreased proportion of 8.0% (4.0–15.1%); (3) Dmeanwas 13.68 ± 1.86 Gy in N-plans and 13.28 ± 1.78 Gy in B-plans(P = 0.001),with a median numeric decreased proportion of 2.3%(- 0.8–6.2%). (4) NTCP was significantly lower for B-plans compared to N-plans (mean: 1.60 ± 1.39 vs.1.76 ± 1.6, P = 0.015). Similar dosimetric metrics were observed in the right lung: significant reductions in V5(60.41 ± 10.31%vs.53.46 ± 11.58%,P <0.001)and V10(34.69 ± 11.65% vs. 28.38 ± 10.25%, P <0.001) were observed for B-plans, with a median decrease of 10.1%(0.4–36.7%) and 18.4% (7.0–44.2%), respectively. Other dosimetric parameters, including V20/V30/V40/V50of the total lungs and right lung V20,were equivalent between the B-plans and N-plans.
3.4 Heart dose
B-plans achieved a slight decrease in the Dmeanof heart,from 11.01 ± 4.53 Gy to 10.73 ± 4.54 Gy (with statistically significant P = 0.01). The median decreased proportion was 3.29% (range - 2.35–10.33%). B-plans also achieved a reduced heart V40compared with N-plans(4.60 ± 2.98% vs. 4.34 ± 2.98%, P = 0.015), with a median decreased proportion of 1.1% (range- 4.81–19.89%).
3.5 Esophagus dose
A statistically significant decrease in esophageal V40(46.86 ± 13.23% vs. 47.41 ± 13.7%, P = 0.039) was observed in B-plans compared with N-plans,with a median decrease of 0.6%. However, the D0.1ccwas increased in B-plans than in N-plans (61.62 ± 4.31 Gy vs.60.95 ± 3.9 Gy, P = 0.044), with a median numeric decreased proportion of 0.8%.
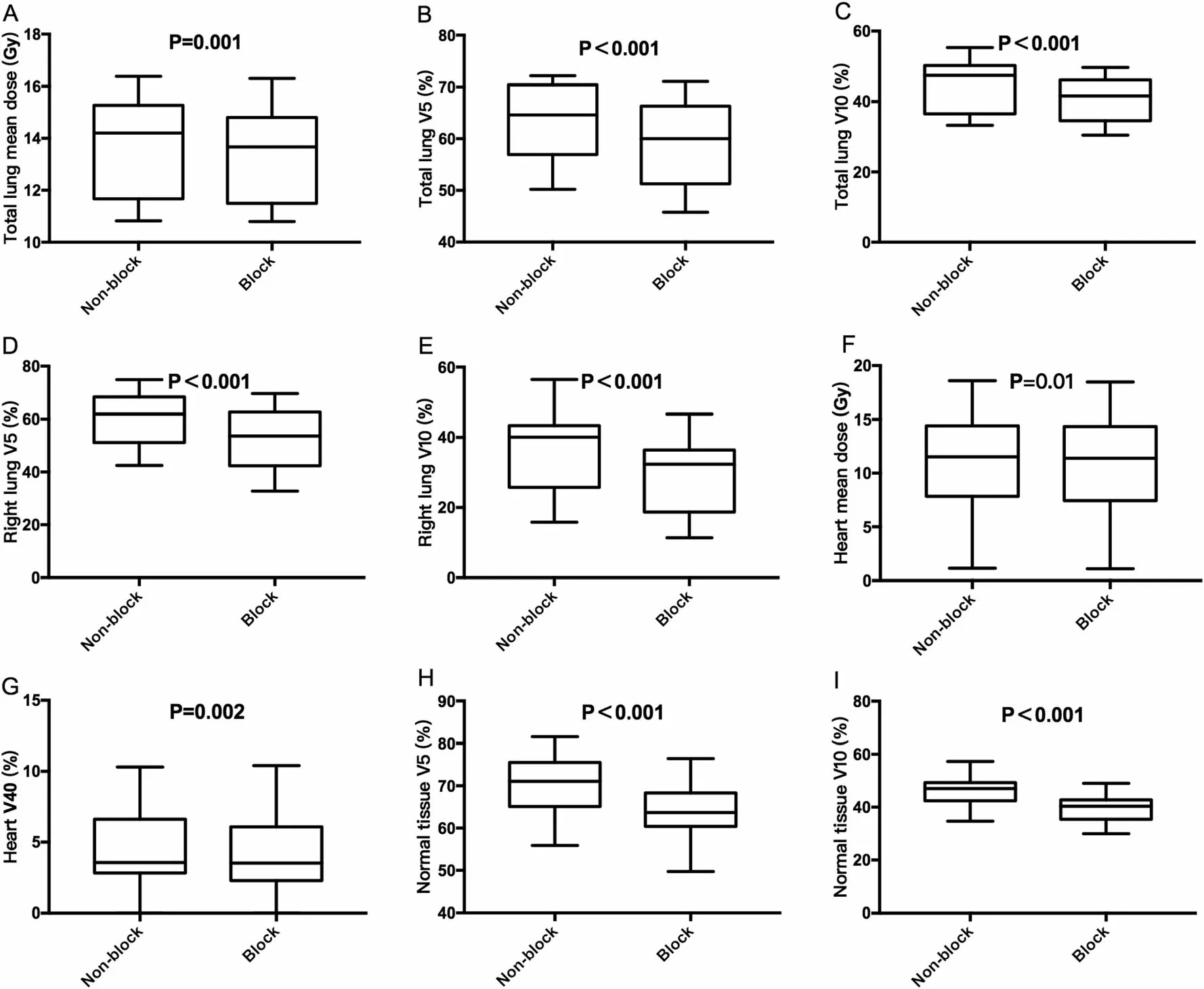
3.6 NT
B-plans obtained significant reductions in Dmean(11.68 ± 1.39 Gy, vs. 12.26 ± 1.42 Gy, P <0.001), V5(63.58 ± 6.69% vs. 70.20 ± 7.49%, P <0.001), and V10(39.84 ± 5.37% vs. 46.08 ± 6.27%, P <0.001) of NT compared to N-plans, with median decreased proportions of 3.6% (- 1.0–14.1%), 8.2% (4.6–17.0%), and 13.3%(0.4–26.8%).
4 Discussion
In recent years, the VMAT technique has been applied for the treatment of LA-NSCLC. Although several retrospective studies have confirmed the efficacy and safety of VMAT plans [37, 38], there are still concerns about pulmonary toxicity caused by increased low-dose volumes.Therefore,for the first time,we used a virtual block method in VMAT planning for LA-NSCLC cases.The N-plan used all beamlets of the set gantry angles in the optimization process. In contrast, the B-plan prevents some of the beamlets from crossing the predefined block. The results indicated that B-plans were effective in reducing lung and heart doses.
According to our implementation experience, this virtual block has six advantages compared to previous methods:(1)Partial arcs over 180°are utilized in most LANSCLC VMAT cases. This ring block stands in the most direction before the beamlets pass through the lung, which is mentioned in the form of a block by Hong et al.[18];(2)this ring block considered a constant distance of 8 cm from the target. The 8-cm distance is sufficient to avoid destroying the targets’ conformity. Because the prescription dose to targets is high up to 60 Gy, the constraint to the ring block is as low as 5 Gy,a 1.5-cm distance between the block and targets used by Hong et al. [18] may not be sufficiently large; (3) this ring block could be easily implemented in a clinical routine in three steps, as shown in Fig. 1. The contouring of this ring block could be programmed by the Pinnacle scripting tool and performed automatically. Other commercially available TPS, such as Eclipse, Monaco (Elekta AB, Stockholm, Sweden), and RayStation (RaySearch Laboratories, Sweden), have their own programming modules and can accomplish the ringblock contouring process automatically. (4) Although Eclipse has arc avoidance sectors and other TPSs, such as the Pinnacle, use more than two partial arcs to limit the low-dose area to the lungs, this method of handling the beamlet entrance, which ignores the location and shape of targets, varies slices by slices and does not precisely block the beamlets. (5) Most TPSs, such as RayStation 10A,Pinnacle, Eclipse, Monaco, and RayStation, could specify avoidance for entrance and/or exit dose through specific contours, but the contours should be manually defined and drafted by planners. Nevertheless, manual contours were time-consuming and varied among different planners.This new virtual block was invented based on the principle of overcoming these problems and was easily implemented in VMAT plans for planners. (6) It should be noted that all LA-NSCLC cases were selected for this study because of the large tumor size and the unmet constraint of total lung V5, V10, and mean dose (Dmean). Although an expected value on DVHs of the lungs could also be achieved by putting a very low total lung V5/V10during the optimization in some LA-NSCLC cases, PTV coverage was sacrificed,and the prescription isodose line missed PTV in some slices. Sometimes, PTV dose coverage is critical. The optimization process will preferentially achieve a lower V5/V10if it is not guided. The virtual block method considers the relative locations of the total lungs and tumor,which could avoid this problem and close the beamlets properly.
Radiation pneumonitis(RP)is one of the most common side effects of thoracic RT in patients with LA-NSCLC.This complication has a considerable impact on patient morbidity and can even lead to death. As demonstrated earlier, RP risk is strongly correlated with the irradiation dose delivered to the lungs; Ren et al. [13] and Wu et al.[14]indicated that lung V5/V10and MLD were independent factors for predicting symptomatic RP in patients with lung cancer.The incidence rate of grade ≥3 RP was reported to be 2%in patients with V5values ≤70%,but 21%in those with values >70% (P = 0.17)[16]. Shi et al. reported that severe acute RP could be reduced from 29.2 to 5.7%if the lung V10was controlled to less than 50% [39]. As for the MLD,Barriger et al.reported that the grade ≥2 RP could be reduced from 19 to 2.2% if the MLD was controlled to be less than 18 Gy [40]. The present study demonstrated that B-plans achieved notable reductions in total lung V5/V10and MLD with median decreased proportions of 5.1%,8.0%, and 2.3%, respectively, which promoted the protection of normal lungs.Several studies have suggested that V5should optimally be less than 60–65% for patients treated with concurrent chemoradiotherapy [15, 16]. In recent years, V5has gained considerable attention for the evaluation of the quality of radiation plans. Our study observed sharp reductions in both total lung V5and contralateral lung V5in the B-plans,which improved the safety of VMAT planning in NSCLC. However, similar V20/V30/V40/V50values of the total lung were observed between the B-plans and N-plans.This indicated that the advantages of the virtual block mainly relied on the decrease in low-dose exposure, instead of high-/inter-median dose exposure.
Previous studies have reported that the doses to the heart are highly related to the cardiac events of LA-NSCLC.Thus, it is associated with the OS of LA-NSCLC.There is increasing recognition of the importance of sparing the heart in patients with LA-NSCLC owing to the increase in long-term survivors.The Pacific trial revealed a significant improvement in LA-NSCLC patients with consolidation immunotherapy, with a median OS of 47.5 months[41,42].According to a pooled analysis of six prospective trials, the 2-year competing risk-adjusted cardiac event rates for stage III NSCLC patients with a heart Dmean-<10 Gy/ 10–20 Gy/ ≥20 Gy were 4%, 7%, and 21%,respectively [43]. Chun et al. [44] performed a second analysis of the RTOG 0617 trial and found higher V40of the heart which resulted in worse OS among stage III NSCLC patients,with a hazard risk of 1.012.In our study,notable reductions in heart Dmean/V40were observed for B-plans,which decreased proportions by 3.29%/1.1%.The B-plans displayed effective performance in heart protection.
We applied a SIB-based dose-reduction protocol in LANSCLC patients in this study, and the dose prescriptions was 50.4 Gy to PTV, with a simultaneously 60.2 Gy to PGTV in a total fraction of 28. This dose protocol was confirmed to be effective and well-tolerated in our previous studies[45,46].All radiation plans with or without virtual blocks were made by senior medical physicists working over 5 years [24] to exclude the influence of various technical levels. Two types of plans achieved ≥95%prescription dose coverage for PGTV/PTV. The B-plans showed better quality than the N-plans did. Although B-plans obtained a higher HI in PGTV and PTV-PGTV than N-plans, the plans were still acceptable for clinical use. Furthermore, the high-dose region of targets can be reduced in several ways, such as (1) increasing the weight of the maximum dose and uniform dose to targets in objective settings of the optimization parameters; (2) the addition of appropriately angled small-weighted conformal fields; and (3) multiple arcs using an appropriately set.
It should be noted that the ring block could also be used in other tumor entities such as esophageal carcinoma and hepatocellular carcinoma. RP is also a general complication of esophageal cancer RT, which is associated with low-dose irradiation of the lung volume [17]. Hepatic radiation toxicity has been at the center of interest for hepatocellular carcinoma, and radiation delivery to targets is limited by the tolerance of the surrounding normal liver parenchyma[47].Ring-block is potentially a good solution to restrict the low-dose volume of the lungs in esophageal carcinoma and normal liver tissue in hepatocellular carcinoma.
This study has several limitations. First, because the B-plans were made, which were not used in clinical practice, verification of treatment-related toxicities was not performed. Second, the tumor locations of all enrolled patients with lung cancer in the study were retained. It should be noted that the role of the B-plan in patients with right lung tumors remains unclear. In addition, the homogeneity of the target volume for B-plans was slightly worse than that of N-plans, and the D0.1ccof the esophagus was higher in B-plans than in N-plans. This implies that the block types should be further optimized. Third, the contouring of this virtual block method was based on our clinical experience; thus, further research is required to prove this theoretically.
5 Conclusion
To reduce the risk of RP, we created a novel virtual block that can be applied in VMAT planning for patients with LA-NSCLC. The VMAT plan with the virtual block method could significantly reduce V5, V10, MLD of the lung, and V30and Dmeanof the heart, with the same conformity of targets as the VMAT plan with the virtual block method. In addition, the homogeneity of the target volume for the VMAT plan with the virtual block method was slightly worse than that for the VMAT plan with the virtual block method. Advantageous profiles obtained by VMAT planning for LA-NSCLC can be achieved using our novel virtual block.The use of a ring block at a distance of 8 cm from the targets with proper weight in the optimization parameter is recommended based on our analysis. This block is conveniently implemented routinely clinical scenarios and can promote the application of VMAT plans in LA-NSCLC patients.
Author contributions All authors discussed and conceived of the study design. Jia-Yun Chen did the initial validation of the projects and score metric development. Da-Quan Wang performed case selection and data analysis. Jia-Yun Chen and Da-Quan Wang -drafted the manuscript. Da-Quan Wang and Nan Bi contoured the targets and organs at risk of the case.Xiao-Dong Zhang provided the mdaccAutoPlan system, and Jia-Yun Chen modified mdaccAutoPlan system based on clinical planning strategy. Qi Fu and Xue-Na Yan did the treatment planning of the cases.Nan Bi evaluated all plans and provided meaningful suggestions about the plan evaluations. Kuo -Men participated in discussions about the data analysis and provided meaningful suggestions. Jian-Rong Dai guided the study preparation of the manuscript.All authors read,discussed,and approved the final manuscript.
杂志排行
Nuclear Science and Techniques的其它文章
- Development of a low-background neutron detector array
- Dication-accelerated anion transport inside micropores for the rapid decontamination of pertechnetate
- Iterative Bayesian Monte Carlo for nuclear data evaluation
- Decomposition of oil cleaning agents from nuclear power plants by supercritical water oxidation
- Signal modeling and impulse response shaping for semiconductor detectors
- Nuclear mass based on the multi-task learning neural network method
