Distress management in cancer patients:Guideline implementation based on CAN-IMPLEMENT
2022-05-10LianFuXiaojuZhanYanHuZhnqiLuYanYanMinzhuHuanYuanyuanLiFuzhonZhuYanWanZhHuan
Lian Fu , Xiaoju Zhan , Yan Hu , Zhnqi Lu , Yan Yan , Minzhu Huan ,Yuanyuan Li , Fuzhon Zhu , Yan Wan , Zh Huan
a School of Nursing, Fudan University, Shanghai, China
b Department of Nursing, Affiliated Jinhua Hospital, Zhejiang University School of Medicine, Jinhua, China
c Department of Nursing, Fudan University Shanghai Cancer Center, Shanghai, China
d Department of Oncology, Fudan University Shanghai Cancer Center, Shanghai, China
e Department of Psychological Medicine, Zhongshan Hospital Affiliated to Fudan University, Shanghai, China
f Department of Social Work, Fudan University Shanghai Cancer Center, Shanghai, China
g Department of Integrated Therapy, Fudan University Shanghai Cancer Center, Shanghai, China
Keywords:Clinical practice guideline Distress management Guideline adherence Implementation Patient care team Neoplasms
ABSTRACT Objective: To standardize the distress management of gastric cancer patients receiving chemotherapy,the adapted Cancer-related Distress Management Guidelines were implemented in nursing practice among gastric cancer patients receiving chemotherapy based on A Guideline Adaptation and Implementation Planning Resource (CAN-IMPLEMENT).Methods: Based on the theoretical framework of CAN-IMPLEMENT, A multidisciplinary team was established, barriers and facilitators obstacles of guidelines implementation in medical oncology units were assessed, corresponding solutions were formulated, the guidelines implementation process was monitored, and implementation results were evaluated.Results: The multidisciplinary team developed review criteria, standardized work paths, assessment tools,training manuals for healthcare professionals,education manuals for patients and their caregivers.After guidelines implementation, the completion rate of the distress management record came up to 97.9%(189/193).From September 2017 to December 2018,the compliance of medical staff on most items in the audit checklist was improved, ranging from 57.1% (100/175) to 100.0% (193/193).The positive distress rate of gastric cancer patients receiving chemotherapy was decreased from 22.7% (32/141) to 9.3% (18/193) (P <0.05), and the Median (range) of the distress score declined from 2 (0-9) to 0 (0-7)(P <0.001).Conclusions: The implementation of guidelines based on CAN-IMPLEMENT promotes the establishment of a distress management system in the medical oncology units.The review standards, standardized work paths,and evaluation tools for distress in cancer patients formulated by the multidisciplinary team had clinical applicability and effectiveness.Quality control in the practice of distress management was effective.The compliance of healthcare professionals with distress management was improved.The distress of gastric cancer patients receiving chemotherapy was alleviated effectively.
What is known?
· Distress management is clarifying patients’ distress status, understanding their distress experience,and effectively alleviating their distress through corresponding management strategies.However, as the critical link to put evidence into practice successfully, guideline implementation is usually full of difficult challenges.
· A Guideline Adaptation and Implementation Planning Resource(CAN-IMPLEMENT) was developed by Harrison, M.B.and van den Hoek,J.for the Canadian Guideline Adaptation Study Group of the Canadian Partnership Against Cancer (the ‘Partnership’)based on the ADAPTE methodology using a mixed-methods,case-study design.
What is new?
· Ten translated practical audit criteria for distress management of cancer patients were developed based on the extracted recommendations from the adapted guidelines by the multidisciplinary panel of guideline implementation.
· Standard working pathway(s) and unified assessment tools for cancer patients’ distress management, training manual for healthcare professionals, education and handbook for patients and their caregivers were developed.
· The barriers and facilitators of this guideline application were systematically and comprehensively evaluated from three aspects: guidelines analysis, understanding users of guidelines and assessing of practicing context of the guideline application.At the same time,according to the barriers and facilitators of the guideline application, the solution strategies suitable for the practice situation of the research site were formulated.
· According to the Cancer-related Distress Management Guidelines adapted based on CAN-IMPLEMENT, the implementation of work plan was helpful to standardize distress management in cancer patients, and effectively alleviated distress of cancer patients.
· The guideline implementation was feasible in a hospital in China based on CAN-IMPLEMENT and guided by the Knowledge-to-Action Framework.The guideline translation for distress management in cancer patients was performed successfully.
1.Introduction
Gastric cancer is one of the top ten prevalent cancers worldwide.The new cases of gastric cancer were over 1,000,000, and the deaths was about 783,000 in 2018, making it the fifth most frequently diagnosed cancer and the third leading cause of cancer death [1].In China, there were approximately 679,100 new cases and 498,000 deaths of gastric cancer in 2015,ranking second after lung cancer among all cancer types [2].Distress is a multifactorial unpleasant experience of a psychological, social, spiritual, and/or physical nature that may interfere with the ability to cope effectively with cancer, its physical symptoms, and its treatment [3].Thus, distress management is the identification and treatment of the multifactorial unpleasant experience in cancer patients.Hong et al.reported that the prevalence of clinically significant preoperative psychological distress was 76.97% in Chinese patients with newly diagnosed gastric cancer [4].In addition, patients with clinically psychological distress were more likely to have poor quality of life and demonstrate negative coping styles [4].In the research site, the research team found that most patients with gastric cancer have a low education level and a high age.These patients are not good at expressing emotions, and their psychological care needs are easily overlooked.At the same time, all gastric cancer patients in the research site were undergoing chemotherapy or preparing for chemotherapy.Therefore, it was decided to recruit gastric cancer patients receiving chemotherapy as the research object of the guideline implementation after group discussion.
The guideline implementation is a process of changing practice in health care while utilizing the best level of evidence that is available in the published literature [5].As the critical link to put evidence into practice successfully, guideline implementation is usually full of difficult challenges[6,7].Fischer et al.indicated that the barriers to guideline implementation could be differentiated into personal factors,guideline-related factors,and external factors[8].Accordingly, the corresponding strategies were identified,including dissemination,education and training,social interaction,decision support systems and standing orders [8].Cheng et al.demonstrated that the main barriers to evidence-based nursing implementation in China were lack of knowledge and skills for nurses, followed by a lack of protocol and heavy workload for the system [9].Another study conducted in China showed that high frequency and high ranking of barriers for the guideline implementation all converged on“lack of access”,“less convenient”,“lack of applicability” and “lack of evidence from Chinese sample”, and high frequency and high ranking of enablers converged on “short formats presentation”, “utilisation of various media”, “information visualisation” and “linking to patient electronic medical records”[10].
The entire study was designed to conduct guideline adaptation and guideline implementation for distress management in gastric cancer patients receiving chemotherapy, which was based on A Guideline Adaptation and Implementation Planning Resource(CAN-IMPLEMENT) [11,12].CAN-IMPLEMENT was under the guidance of Knowledge-to-Action Framework, including knowledge creation and action cycle (application) [11,12].The knowledge creation is the same as in the Knowledge-to-Action Framework,but the action cycle (application) consists of three phases naming identification and clarification of the practice issue, solution building,and implementation,evaluation and sustainability[11,12].Identification and clarification of the practice issue, includes five steps naming call to action,guideline development plan,search and screen, assess and select, and draft, revise and endorse.Solution building is made up of three steps:align knowledge to local context practice and system, assess barriers and facilitators to knowledge use, and select and tailor implementation interventions.Implementation, evaluation and sustainability is composed of three steps: monitor knowledge use/evaluate implementation, evaluate outcomes, and nature change and sustain knowledge use.The psychological symptoms and physical symptoms were both need attention.A work plan was developed for the adaptation of Cancerrelated Distress Management Guidelines.Two clinical practice guidelines on distress management were included.The domain scores were good for the draft Cancer-related Distress Management Guidelines on AGREE II.The quality of the draft Cancer-related Distress Management Guidelines was well-accepted based on two included guidelines.The final Cancer-related Distress Management Guidelines were formed based on the revision of the draft guidelines, including 13 recommendations [13].
According to CAN-IMPLEMENT, this study consisted of three phases: 1) integrating relevant clinical practice guidelines on the distress management in cancer patients to form the Cancer-related Distress Management Guidelines (identification and clarification of the practice issue); 2) aligning the Cancer-related Distress Management Guidelines into clinical practice among gastric cancer patients receiving chemotherapy (solution building); 3) monitoring, evaluating and maintaining the implementation of Cancer-related Distress Management Guidelines in clinical practice (implementation, evaluation and sustainability).The Adaptation Part including Step 1 to 5 was previously reported[13].The Implementation Part(Phase 2 and Phase 3, from Step 6 to 11) was reported here.The Implementation Part was to align the Cancer-related Distress Management Guidelines into nursing practice in gastric cancer patients undergoing chemotherapy,and to monitor the process of guideline implementation,evaluate the effects of guideline implementation,and maintain the guideline implementation in clinical practice.The specific objectives in Implementation Part were as follows: 1) To explore the gap between the current distress management and recommendations in the adapted guidelines; 2) To analyze gaps,assessing barriers and supports of guideline implementation from guidelines,users and practice context,and developing appropriate solutions; 3) To monitor the process and evaluate the outcome of this guideline implementation; 4) To regularize the distress management among gastric cancer patients receiving chemotherapy.
2.Methods
Ethics approval for this study was provided by School of Nursing Fudan University Shanghai Cancer Centre(1710177-23) and Fudan University(IRB#2017-9-3).From May 2017 to June 2019,the study‘Guidelines Adaptation and Implementation for Distress Management in Cancer Patients’ was carried out in School of Nursing,Fudan University and three medical oncology units, Fudan University Shanghai Cancer Center, China.The primary research contents of this study were translating relevant distress management guidelines into clinical nursing practice,which was based on CANIMPLEMENT and guided by the Knowledge-to-Action Framework.The authorization was obtained from the principal investigator of the CAN-IMPLEMENT project.
2.1.Solution building: guideline alignment (phase 2)
2.1.1.Align knowledge to local context (Step 6)
A multidisciplinary panel of guideline implementation was set up.The multidisciplinary panel of guideline implementation included a professor, an associate professor, three supervisor nurses, two nurse practitioners and two nurses of oncology nursing, a chief physician of psychological medicine, a chief physician of palliative care, a chief physician, an associate chief physician and an attending doctor of oncology, an associate professor of psychological care,two social workers,a professor and an associate professor skilled with evidence-based practice methodologies,a doctoral candidate and a postgraduate student of nursing science.The recommendations in the adapted guidelines were translated to practical audit criteria considering the local practice contexts and the specific responsibilities of the professionals.A guideline implementation work plan was developed by the multidisciplinary panel of guideline implementation.
From September 2017 to June 2018, a cross-sectional study was conducted to describe and analyze the gastric cancer patients’distress and the gap between the current distress management and guidelines’ recommendations.The participants were a medical oncology unit,8 doctors,20 nurses,8 mental health professionals,2 social workers,4 palliative care staff and 141 gastric cancer patients receiving chemotherapy.Inclusion criteria were as follows.1) Medical oncology unit: a medical oncology unit in a tertiary-level oncology hospital; treating gastric cancer patients with chemotherapy; approval for the study.2) Medical staff: participate in the implementation of distress management guidelines for gastric cancer patients receiving chemotherapy; practicing nurses/physicians/social workers and so on; with working experience ≥6 months;informed consent to the study.3) Gastric cancer patients receiving chemotherapy:18 years of age or older;diagnosed as gastric cancer by clinical pathology;receiving at least one chemotherapy treatment in the research site within the past three months;being able to read and answer questions correctly;informed consent to the study.
A self-designed distress management record in cancer patients was used to record whether the users of the guidelines followed the recommendations to carry out the distress management for cancer patients.A self-designed audit checklist for medical institutions’distress management aimed to judge the current situation of distress management in cancer patients at the medical institution level.There are eight items involving the norms, procedures,evaluation records, multidisciplinary cooperation team, medical staff training manual, medical staff training, patient education manual,and patient education.The options for each item are“Yes”or“No”.The self-designed audit checklist for medical staff’s distress management was performed to judge whether the clinical practice of the guideline users meet the requirements of the recommendations.The options for each item are “Yes” or “No”.The Distress Thermometer (DT) is a single-item distress self-evaluation tool with good reliability and validity, evaluating the average distress experienced by patients in the past week [14].The score ranges from 0 to 10,with 0 being no distress and 10 extremely distress.In addition, DT also includes a list of questions.The Hospital Anxiety and Depression Scale(HADS)is a 14-item scale with good reliability and validity, including two subscales for anxiety and depression[15].A four-point Likert-type scale ranging from 0(not a problem)to 3(high level of problems)is used for scoring each item.The score for each subscale is obtained by simple summation of individual items with scores in each subscale (anxiety and depression)ranging from 0 to 21.A score of seven or less indicates a nonanxiety/depression case, 8-10 a borderline case of anxiety/depression, and 11 or above a definite case of anxiety/depression.The data were analyzed by SPSS 25.0.The completion rate of the distress management record,the compliance of items on the audit checklist for medical staff’s distress management,and the positive distress rates, the distress scores, the problem reporting rates and the positive rates of anxiety and depression among gastric cancer patients receiving chemotherapy were described by frequency distributions and descriptive statistics.
2.1.2.Assess barriers and facilitators to knowledge use (Step 7)/select and tailor implementation interventions (Step 8)
The expert meeting method was used to assess the barriers/supports and develop feasible solutions for guideline implementation.Eligibility criteria of experts were as follow:Engaged in relevant work in the fields of evidence-based medicine, clinical oncology, oncology nursing, psychology, or social work; with working experience ≥5 years; research or practical experience in evidence-based medicine, clinical oncology, cancer nursing, psychology, social work and so on; informed consent to the research.Interview outlines were developed to guide the expert meeting,covering the aspects of innovation, adopters and practice environment.1) Guidelines analysis: the background of guideline implementation, feasibility, appropriateness, meaningfulness and effectiveness of recommendations and so on.For example, how important and necessary do you think the guideline application is?What are the feasibility, appropriateness, meaningfulness and effectiveness of recommendations in the adapted guidelines? 2)Understanding users of guidelines: the knowledge, attitude and skills of decision-makers, medical staff, patients and so on.For example, what is the level of knowledge, attitude and skill of medical staff on distress management in cancer patients? 3)Assessing of practicing context: rules and regulations, leadership,organizational culture, practice pattern and so on.For example,does the research site have corresponding rules and regulations on distress management in cancer patients? 4) According to the identified barriers and facilitators and the actual situation of the research site: what do you think are the corresponding solutions?Within 24 h, the researchers analyzed and summarized the barriers, facilitators and related solutions of the guideline application through repeated reading of expert meeting minutes and combining with their own professional judgment.
2.2.Implementation, evaluation and sustainability: guideline application and evaluation (phase 3)
2.2.1.Monitor knowledge use (Step 9)/evaluate outcomes (Step 10)
A historical controlled trial was conducted with the same instruments in Step 6 between July 2018 and December 2018.The subjects included a medical oncology unit, 8 doctors, 20 nurses, 8 mental health professionals,2 social workers,4 palliative care staff and 193 gastric cancer patients receiving chemotherapy.The inclusion criteria of participants were the same as those in the gap analyses.Chi-square test and Mann-Whitney U test were performed to compare the differences in the completion rate of the distress management record,the compliance of items on the audit checklist for medical staff’s distress management,and the positive distress rates, the distress scores, the problem reporting rates and the positive rates of anxiety and depression of gastric cancer patients receiving chemotherapy before and after the guideline implementation.A value of P <0.05 was considered statistically significant.
2.2.2.Nuture change and sustain knowledge use (Step 11)
From January to March 2019, the implementation of Cancerrelated Distress Management Guidelines was sustained by assessing barriers and facilitators to knowledge use, selecting and tailoring implementation interventions, monitoring process and evaluating outcomes again.For monitoring process and evaluating outcomes,another historically controlled trial was performed including a medical oncology unit, 8 doctors, 20 nurses, 8 mental health professionals, 2 social workers, 4 palliative care staff and 30 gastric cancer patients receiving chemotherapy.The inclusion criteria of participants were the same as those in the gap analyses.The instruments were the same as those used in Step 6.Chi-square test and Mann-Whitney κ test were performed to compare the differences in the completion rate of the distress management record,the compliance of items on the audit checklist for medical staff’s distress management, the positive distress rates, the distress scores, the problem reporting rates, and the positive rates of anxiety and depression of gastric cancer patients receiving chemotherapy before and after the guideline implementation maintenance.A value of P <0.05 was considered statistically significant.
3.Results
3.1.Solution building: guideline alignment (phase 2)
3.1.1.Align knowledge to local context (Step 6)
Ten translated practical audit criteria were developed based on the extracted recommendations from the adapted guidelines(Table 1).The clinical pathways of distress management were also developed based on the translated practical audit criteria (Fig.1).The work plan of guideline implementation was presented as a protocol for a historical controlled trial.The contents of work plan included the following parts:design,participant,inclusion criteria,sample size, research site, intervention, instruments, data collection,analyses and so on.The interventions were the practical audit criteria based on the recommendations in the adapted guidelines.
Before the guideline implementation project, there were no formal audit criteria, working pathways, assessment tools, multidisciplinary panels, training manual for healthcare professionals,education and handbook for patients and their caregivers of distress management on the institutional level, as well as the related assessment tools and record forms.Therefore, the completion rate of the distress management record was zero at baseline.The general conditions of patients before the guideline implementation are presented in Table 2.The compliance rate of each item on the audit checklist for medical staff’s distress management in cancer patients was all zero (Table 3).The positive distress rate of gastric cancer patients receiving chemotherapy(DT ≥4)was 22.7%(32/141)(Table 4),and the distress score was 2(0-9).The problem report rates of gastric cancer patients receiving chemotherapy with moderate to severe distress were 0% (0/32) to 75.0% (24/32).The positive rates of anxiety and depression were both 40.0% (10/25).
3.1.2.Assess barriers and facilitators to knowledge Use(Step 7)/select and tailor implementation interventions (Step 8)
Eight experts were invited,including two supervisor nurses and two nurse practitioners of oncology nursing, a supervisor nurse of palliative care, a nurse of psychological care, a physician of psychological medicine, and a social worker.Six barriers and six supports of the guideline implementation were identified from the guidelines, the adopters and the practice environment.Ten corresponding solutions were developed, too(Table 5).
3.2.Implementation, evaluation and sustainability: guideline application and evaluation (phase 3)
3.2.1.Monitor knowledge use (Step 9)/evaluate outcomes (Step 10)
After the guideline implementation, the formal audit criteria,working pathways, assessment tools, multidisciplinary panels,training manual for healthcare professionals, education and handbook for patients and their caregivers of distress management on the institutional level were developed, as well as the related assessment tools and record forms.Except for the BMI,there was no statistically significant difference in the general conditions of the two groups of patients before and after the guideline implementation (P >0.05) (Table 2).The completion rate of the distress management record was increased from 0 to 97.9% (189/193)(P <0.001).The compliance of most items on the audit checklist for medical staff's distress management was improved, with rates ranging from 57.1%(100/175)to 100.0%(193/193),see Table 3.The positive distress rate of gastric cancer patients receiving chemotherapy decreased from 22.7%(32/141)to 9.3%(18/193)(P <0.05),see Table 4.The distress scores declined from 2 (0-9) to 0 (0-7)(P <0.001).The reporting rates for problems of gastric cancer patients receiving chemotherapy with moderate to severe distress were slightly lower,from 0% (0/18) to 61.1%(11/18) (P >0.05).The positive rates of anxiety and depression were both slightly increased to 64.7% (11/17) (P >0.05).
3.2.2.Nuture change and sustain knowledge use (Step 11)
The results of the guideline implementation maintenance were similar to those during the guideline implementation period.The formal audit criteria, working pathways, assessment tools, multidisciplinary panels, training manual for healthcare professionals,education and handbook for patients and their caregivers of distress management on the institutional level were maintained,as well as the distress management record.When compared to the results of the initial phase for gap analyses,the compliance of most items in the audit checklist for medical staff’s distress management was improved to at least 89.7% (26/29), see Table 3.The positive distress rate of gastric cancer patients receiving chemotherapy was decreased to 3.3%(1/30)(P <0.05,Table 4),and the distress scores were sustained at 0.5 (0-5) (P <0.001).
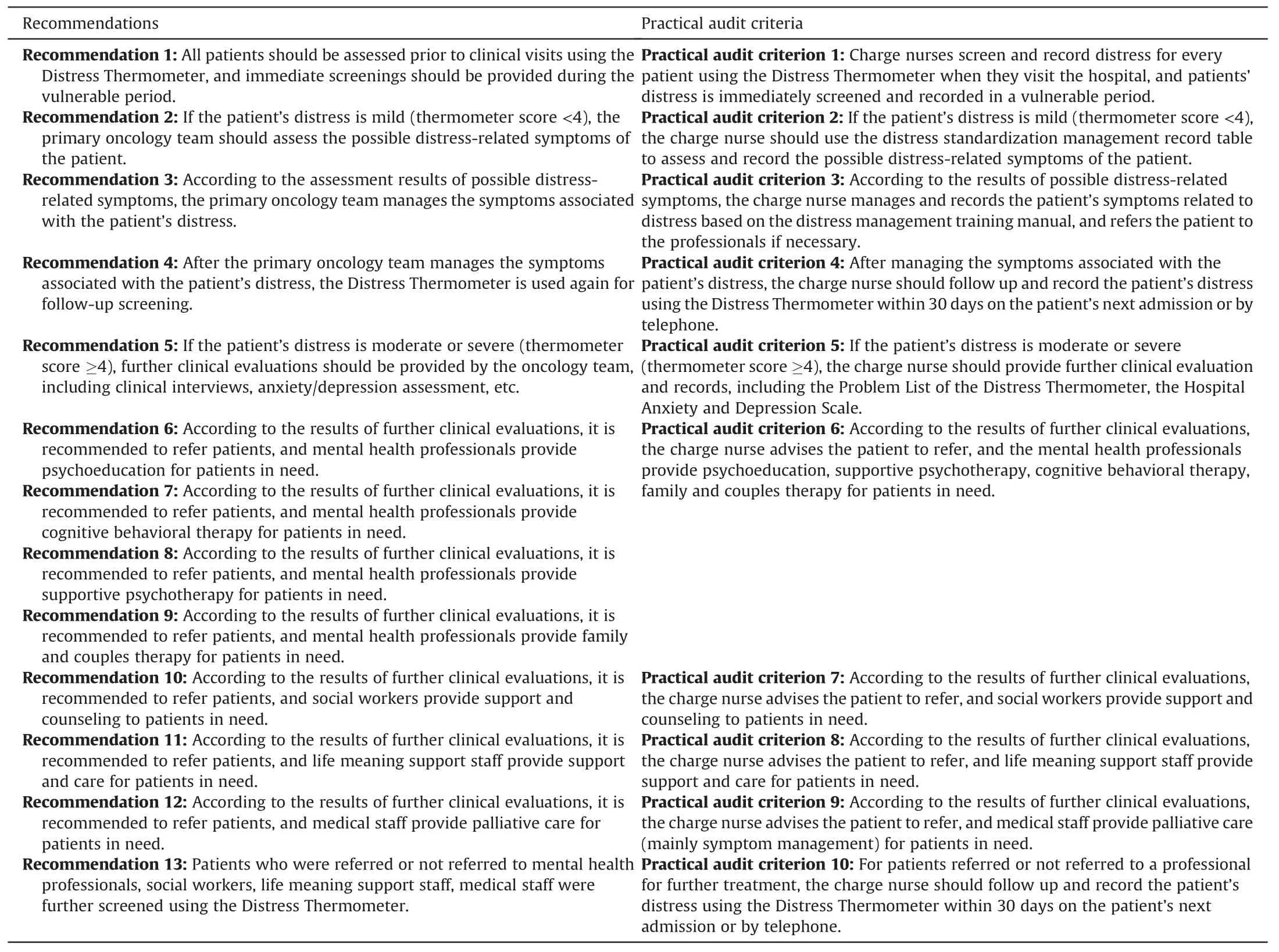
Table 1The recommendations in the adapted guidelines and the corresponding practical criteria.
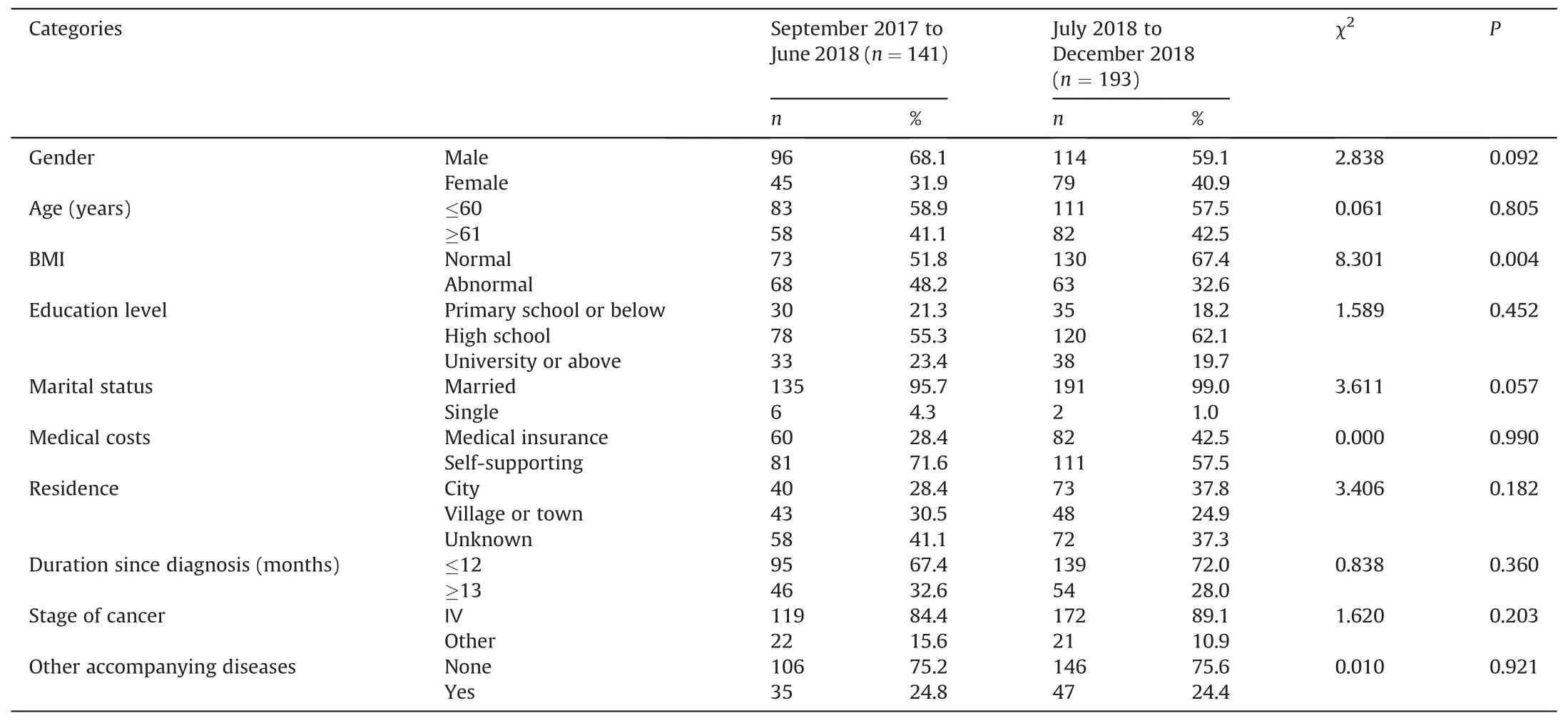
Table 2The comparison on general conditions of gastric cancer patients receiving chemotherapy before and after the guideline implementation.
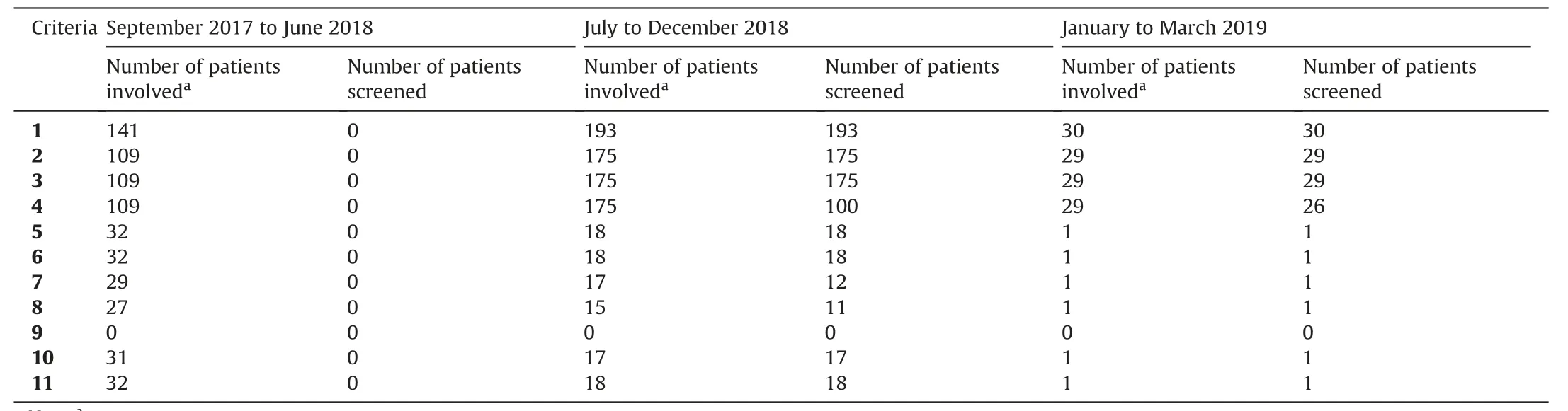
Table 3The comparison on completion rate of distress management on the audit checklist for medical staff during different stage after the guideline implementation.
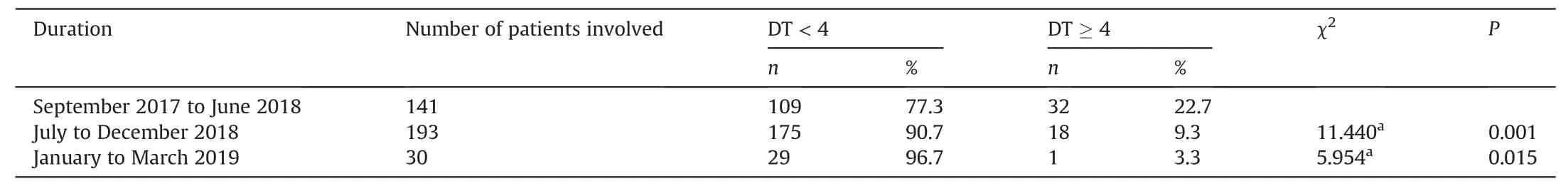
Table 4The comparison on distress screen positive rate of gastric cancer patients receiving chemotherapy before and after the guideline implementation.
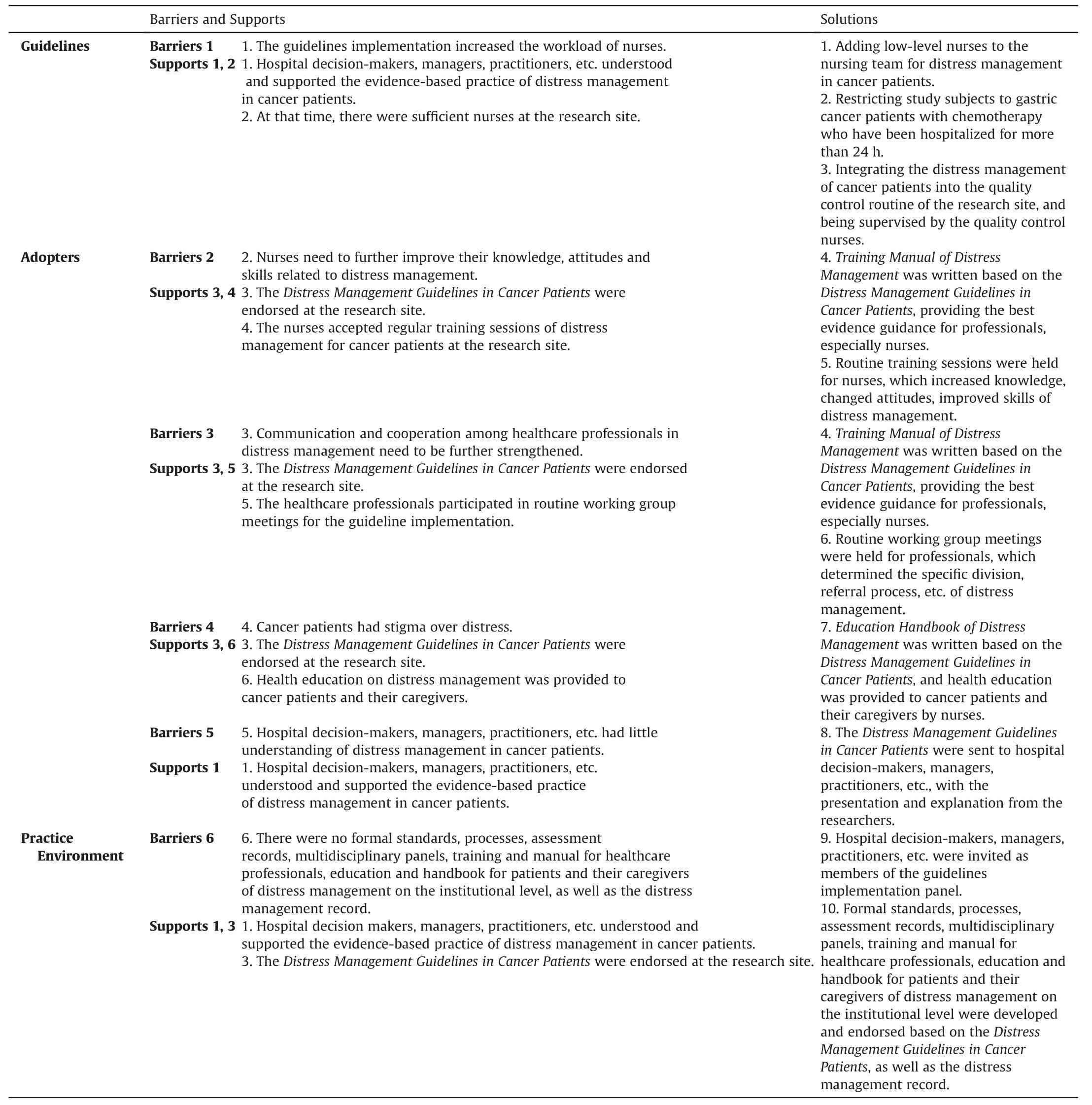
Table 5The barriers, supports and solutions of guideline implementation.
4.Discussion
The members in the multidisciplinary panel of guideline implementation included different roles,such as hospital decision-makers, department managers, frontline medical staff, patients,and university researchers.They can provide support in terms of policies,resources,practice,and management.Some core members of the guideline adaptation panel were also members of the guideline implementation panel, which can better ensure the consistency and continuity of the guideline translation, so as to smoothly advance the guideline implementation.The work plan of guideline implementation was formulated by coordinating resources related to nursing,psychological medicine,social work,and medical treatment under the leading of the guideline implementation panel.The guideline implementation working group convened a meeting.Based on the Cancer-related Distress Management Guidelines, combined with the actual context of the research site, each recommendation in the guidelines was transformed into operable practice norms one by one, a process for distress management among cancer patients was formed, and relevant evaluation recording tools were developed.In this guideline implementation work plan, the distress management was led by responsible nurses,and a multidisciplinary team participated in the screening, evaluation, nursing, referral,and treatment.
In the gap analyses,the difference between distress management practice in the research site and recommendations in the adapted guidelines was quite big.There was no distress management system at the institutional level before the guideline implementation project,and healthcare professionals almost did not provide services on distress management for cancer patients.Meanwhile,the distress status of gastric cancer patients receiving chemotherapy was not optimistic.Distress has a large negative impact on patients’quality of life [4].Therefore, it is necessary to carry out distress management[16-18].In this study, distress management was conducted via assessing barriers and supports, formulating solutions, establishing relevant norms and procedures and training medical staff.The barriers and supports of this guideline implementation were identified from the guidelines, the adopters and the practice environment[11,12].Grifford and her colleagues reported that barriers included lack of evidence,inadequate knowledge in evidence-based practice,and patients’inability to understand new evidence,while leadership support and network information services were factors that promote evidence-based practice[19].The results in this study were similar to the results of her study.Meanwhile,the solutions corresponding to the above barriers and supports were formulated, including education and training, communication and exchange, review and feedback, patient-related measures, organization-level intervention and so on.Many strategies were formulated in current studies, such as practice protocol development and implementation, multifaceted,audit and feedback, organization structure change, quality control team, training program, multidisciplinary team collaboration,educational materials and so on.Based on the evaluated obstacles and facilitating factors, combined with the actual situation of the research site,the corresponding solutions formulated were similar to the above research, involving nurse human resource allocation,quality control nurse supervision, nurse training meetings, establishing a multidisciplinary cooperative team and so on.
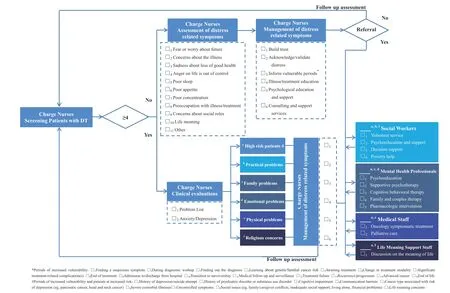
Fig.1. The clinical pathways of distress management
The completion rate of distress management records increased significantly during the guideline implementation, revealing the process quality control of the distress management practice was good.Meanwhile, the distress management record form for patients was completed by the guidelines’ users in cooperation and supervised by the quality control nurses of the research site.Therefore, the results indicate that the responsible nurses, social workers, mental health professionals, medical personnel, life meaning support personnel and quality control nurses in research sites can better perform self-monitoring and quality control monitoring of distress management process.At the institutional level, this guideline implementation promoted establishing the distress management system.The results of this study indicate that the research site approved the Cancer-related Distress Management Guidelines,formed the specific and operable clinical pathways,and formulated related assessment tools and record forms.At the same time, a multidisciplinary team for distress management in cancer patients had been established, a standardized training and education project for medical staff and patients had been formed, a training manual had been produced for medical staff training,and an educational handbook had been sent to patients and their caregivers.To the healthcare professionals, the guideline implementation improved the distress management compliance according to the recommendations in the adapted guidelines.The high compliance demonstrated the overall maturity of distress management in cancer patients and the trouble-free operation of the multidisciplinary team.At the same time, gastric cancer patients receiving chemotherapy who need distress management can receive distress management services timely, conveniently and effectively.In terms of gastric cancer patients receiving chemotherapy, the positive rate and score of distress decreased significantly after the guideline implementation, indicating that distress management practices can effectively improve the distress of gastric cancer patients receiving chemotherapy.Previous studies also showed that distress management could reduce distress in cancer patients.Millegan et al.reported that the use of iPads during chemotherapy is a potentially effective way to introduce meditation as a stress management tool for people with cancer [20].Therefore, it is recommended to provide distress management services to cancer patients as soon as possible,especially to provide evidence-based practice for distress management.
5.Limitations
This study has the following limitations.First, barriers and facilitators to knowledge use were assessed using the expert meeting method.The questionnaire survey may be more appropriate.Second, the study design of guideline evaluation was a historically controlled trial.It is recommended to use a stepped wedge trial design in future studies.Third, only gastric cancer patients receiving chemotherapy were included in the guideline implementation.Thus,the results need to be further verified in patients with other types of tumors before being popularized.
6.Conclusions
In summary, it is clear that the systematic and standardized distress management practice in cancer patients had not been carried out in the research site through the gap analysis,and there had been a big gap with the recommendations in the Cancer-related Distress Management Guidelines.The barriers and facilitators of this guideline application were systematically and comprehensively evaluated.Based on the evaluation of barriers and facilitators of the guideline application, the solution strategies suitable for the practice situation of the research site were formulated.The guideline translation for distress management in cancer patients was performed successfully,and the guideline implementation was feasible based on CAN-IMPLEMENT in a hospital in China.Guideline translation can promote the adoption and implementation of distress management for cancer patients by medical institutions,facilitate the practice of distress management, and alleviate patients’ distress effectively.It is recommended to further maintain and optimize the current distress management practice in the research site.
CRediT authorship contribution statement
Liang Fu:Conceptualization, Methodology, Investigation,Formal analysis, Writing - original draft.Xiaoju Zhang:Methodology, Resources, Writing - review &editing.Yan Hu:Conceptualization, Methodology, Supervision, Writing - review & editing.Zhenqi Lu:Methodology, Supervision, Writing - review &editing.Yang Yang:Methodology, Investigation, Resources, Writing - review&editing.Mingzhu Huang:Methodology,Resources,Writing-review&editing.Yuanyuan Li:Methodology,Resources,Writing-review&editing.Fuzhong Zhu:Methodology,Resources,Writing- review & editing.Yang Wang:Methodology, Investigation, Resources, Writing - review & editing.Zhe Huang:Methodology,Resources, Writing - review &editing
Data availability statement
The datasets used and analyzed during the current study are available from the corresponding authors on reasonable request.
Funding
This study was funded by Fudan-Fuxing Nursing Research Funds(No.FNF201701) and JBI Evidence Based Clinical Fellowship Program Funds (No.FNF201861) from Fudan University, China.No conflicts of interest exist in the study.The sponsor did not participate in the study design, data collection, interpretation of results,or presentation of the information.
Declaration of competing interest
The authors declared that they have no conflicts of interest to this work.
Acknowledgments
The authors special thanks go to Professor Margaret B.Harrison for her authorization of A Guideline Adaptation and Implementation Planning Resource (CAN-IMPLEMENT).The authors wish to thank master students from School of Nursing,Fudan University for the searching, screening, assessment, selection and drafting in the guideline adaptation.The authors express their gratitude to the professors, administrators and staffs from Joanna Briggs Institute,Department of Psychological Medicine, Zhongshan Hospital Affiliated to Fudan University and Department of Oncology,Department of Social Work, Department of Integrated Therapy, Department of Nursing, Fudan University Shanghai Cancer Center for their participation in the peer review of the adapted guidelines and the routine distress management during the guideline implementation.Finally,they wish to express their gratitude to all the patients who participated in this study.
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2022.02.006.
杂志排行
International Journal of Nursing Sciences的其它文章
- Effects of mindfulness meditation on trait mindfulness, perceived stress,emotion regulation,and quality of life in hemodialysis patients:A randomized controlled trial
- Application of rational emotive behavior therapy in patients with colorectal cancer undergoing adjuvant chemotherapy
- The effect of slow deep breathing relaxation exercise on pain levels during and post chest tube removal after coronary artery bypass graft surgery
- The association between frailty of older stroke patients during hospitalization and one-year all-cause mortality:A multicenter survey in China
- Translation and piloting of the Chinese Mandarin version of an intensive care-specific pressure injury risk assessment tool (the COMHON Index)
- Adaptation and validation of pediatric peripheral intravenous catheter insertion and care practices audit tools
