达格列净联合沙格列汀治疗二甲双胍控制不佳的2型糖尿病患者的效果观察
2022-05-10由晓丹
由晓丹

【摘要】 目的:探討达格列净联合沙格列汀治疗二甲双胍控制不佳的2型糖尿病(T2DM)患者的效果。方法:选择2019年1月-2020年12月辽阳市第二人民医院收治的84例二甲双胍控制不佳的T2DM患者,采用随机数字表法将其分为对照组与观察组,每组42例。两组均给予二甲双胍治疗,观察组加用达格列净联合沙格列汀,对照组加用格列美脲,两组均连续治疗24周。比较两组治疗前后体重、空腹血糖(FPG)、餐后2 h血糖(2 h PG)、糖化血红蛋白(HbA1c)、收缩压(SBP)、舒张压(DBP)、总胆固醇(TC)、甘油三酯(TG)、低密度脂蛋白胆固醇(LDL-C)、高密度脂蛋白胆固醇(HDL-C)、血尿酸(UA)、血肌酐(Scr)水平及不良反应发生情况。结果:观察组治疗后体重较治疗前下降,且低于对照组(P<0.05);对照组治疗前后体重比较,差异无统计学意义(P>0.05)。观察组治疗后体重减少≥5%者占比为26.19%(11/30)高于对照组的2.38%(1/30),差异有统计学意义(P<0.05)。治疗后,两组FPG、2 h PG、HbA1c均较治疗前下降,且观察组均优于对照组(P<0.05)。观察组治疗后HbA1c<7.0%者占比为59.52%(25/30)高于对照组的35.71%(15/30),差异有统计学意义(P<0.05)。治疗后,观察组TC、TG均低于治疗前,且TG低于对照组(P<0.05)。观察组治疗后SBP、DBP均低于对照组和治疗前(P<0.05)。两组不良反应发生率比较,差异无统计学意义(P>0.05)。结论:与格列美脲相比,在二甲双胍控制不佳T2DM患者中,同时添加达格列净及沙格列汀可显著改善血糖、体重及TG水平,且并未明显增加不良反应。
【关键词】 达格列净 沙格列汀 二甲双胍 2型糖尿病
Effect of Dapagliflozin Combined with Saxagliptin on Patients with Metformin Poorly Controlled Type 2 Diabetes Mellitus/YOU Xiaodan. //Medical Innovation of China, 2022, 19(10): 00-013
[Abstract] Objective: To investigate the effect of Dapagliflozin combined with Saxagliptin on patients with Metformin poorly controlled type 2 diabetes mellitus (T2DM). Method: A total of 84 patients with Metformin poorly controlled T2DM treated in Liaoyang Second Peoples Hospital from January 2019 to December 2020 were selected. They were divided into control group and observation group by random number table method, with 42 cases in each group. Both groups were treated with Metformin, the observation group was added with Dapagliflozin combined with Saxagliptin, and the control group was added with Glimepiride. Both groups were treated for 24 weeks. Body weight, fasting blood glucose (FPG) and 2 h postprandial blood glucose (2 h PG), glycosylated hemoglobin (HbA1c), systolic blood pressure (SBP), diastolic blood pressure (DBP), total cholesterol (TC), triglyceride (TG), low density lipoprotein cholesterol (LDL-C), high density lipoprotein cholesterol (HDL-C), blood uric acid (UA), blood creatinine (Scr) and the incidence of adverse reactions. Result: The body weight of observation group was lower than that of control group after treatment (P<0.05); there was no significant difference in body weight of the control group before and after treatment (P>0.05). The proportion of weight loss ≥5% in the observation group was 26.19% (11/30), which was higher than 2.38% (1/30) in the control group, and the difference was statistically significant (P<0.05). After treatment, FPG, 2 h PG and HbA1c in two groups were decreased compared with before treatment, and observation group were better than those in control group (P<0.05). After treatment, the proportion of HbA1c <7.0% in the observation group was 59.52% (25/30) higher than 35.71% (15/30) in the control group, and the difference was statistically significant (P<0.05). After treatment, TC and TG in observation group were lower than those before treatment, and TG was lower than that of control group (P<0.05). The SBP and DBP of observation group after treatment were lower than those of control group and before treatment (P<0.05). There was no significant difference in the incidence of adverse reactions between the two groups (P>0.05). Conclusion: Compared with Glimepiride, the Dapagliflozin combined with Saxagliptin significantly improved blood glucose, body weight, and TG levels in patients with Metformin poorly controlled T2DM without significantly increasing adverse reactions.
[Key words] Dapagliflozin Saxagliptin Metformin Type 2 diabetes mellitus
First-authors address: Liaoyang Second Peoples Hospital, Liaoning Province, Liaoyang 111000, China
doi:10.3969/j.issn.1674-4985.2022.10.003
根据治疗指南的建议,大多数2型糖尿病(T2DM)患者使用二甲双胍作为一线降糖单药治疗[1]。然而,对于接受二甲双胍单药治疗效果不佳的患者通常需要添加一种或多种其他降糖药,以在疾病进展过程中实现并维持血糖控制[2-3]。磺脲类药物因其作为抗高血糖药物的良好疗效和低成本而被广泛用作T2DM的二线治疗。然而,其缺点包括低血糖风险增加、体重增加和治疗效果持久性差[4-5]。新型口服抗糖尿病药物,钠-葡萄糖共转运蛋白2(SGLT2)抑制剂和二肽基肽酶4(DPP-4)抑制剂是国际指南推荐的与二甲双胍联合使用的降血糖药物[6]。研究表明,在二甲双胍治疗基础上,SGLT2抑制剂和DPP-4抑制剂的联合用药效果优于单加其中任何一种药物[7-9]。本文就SGLT2抑制剂达格列净联合DPP-4抑制剂沙格列汀治疗二甲双胍控制不佳的T2DM患者的效果进行研究,现报道如下。
1 资料与方法
1.1 一般资料 选取2019年1月-2020年12月于辽阳市第二人民医院治疗的84例二甲双胍控制不佳的T2DM患者作为研究对象。纳入标准:(1)符合T2DM诊断标准[1];(2)目前使用二甲双胍治疗,剂量≥1 500 mg/d稳定治疗3个月以上;(3)随机空腹血糖(FPG)≤15 mmol/L,糖化血红蛋白(HbA1c)7.5%~10.5%。排除标准:(1)入组前3个月内发生过心血管事件;(2)存在本研究所用药物禁忌证;(3)严重心、肝、肾功能障碍,估算肾小球濾过率(eGFR)<60 mL/min,存在不稳定、急性或严重充血性心力衰竭或左心室射血分数≤40%或相关病史。采用随机数字表法将患者分为对照组与观察组,每组42例。患者知情同意并签署知情同意书,本研究经伦理委员会批准同意。
1.2 方法 两组均给予二甲双胍(生产厂家:中美上海施贵宝制药有限公司,批准文号:国药准字H20023370,规格:0.5 g)治疗,1 g/次,2次/d,
早晚餐时服用。观察组加用达格列净(生产厂家:阿斯利康制药有限公司,批准文号:国药准字J20170040,规格:10 mg)10 mg/次,1次/d,晨服,沙格列汀(生产厂家:阿斯利康制药有限公司;批准文号:国药准字HJ20160090,规格:5 mg)5 mg/次,1次/d,早餐前服用。对照组加用格列美脲[生产厂家:赛诺菲(北京)制药有限公司,批准文号:国药准字H20057672,规格:2 mg]口服,1次/d,剂量以1 mg/d开始,根据血糖控制情况逐步增加剂量至最佳维持剂量,每2周调整一次,每次增加1 mg,最大剂量不超过6 mg/d。两组均连续治疗24周。
1.3 观察指标 记录两组体重、血糖、血压、血脂指标和血尿酸(UA)、血肌酐(Scr)水平及不良反应发生情况。体重指标:治疗前后体重及治疗后体重减少≥5%者占比;血糖指标:治疗前后FPG,餐后2 h血糖(2 h PG),HbA1c及治疗后HbA1c<7.0%者占比;血压指标:治疗前后收缩压(SBP)与舒张压(DBP);血脂指标:治疗前后总胆固醇(TC)、甘油三酯(TG)、低密度脂蛋白胆固醇(LDL-C)、高密度脂蛋白胆固醇(HDL-C);不良反应:胃肠道不良反应、上呼吸道感染、尿路感染、头痛、低血糖、酮症酸中毒。
1.4 统计学处理 采用SPSS 23.0软件对所得数据进行统计分析,计量资料用(x±s)表示,组间比较采用独立样本t检验,组内比较采用配对t检验;计数资料以率(%)表示,比较采用字2检验,不良反应发生情况比较采用Fisher确切概率法。以P<0.05为差异有统计学意义。
2 结果
2.1 两组一般资料比较 观察组男22例,女20例;年龄34~65岁,平均(53.82±7.39)岁;病程6~20个月,平均(11.34±3.28)个月。对照组男23例,女19例;年龄33~66岁,平均(54.27±7.58)岁;病程6~19个月,平均(10.98±3.12)个月。两组一般资料比较,差异均无统计学意义(P>0.05),具有可比性。
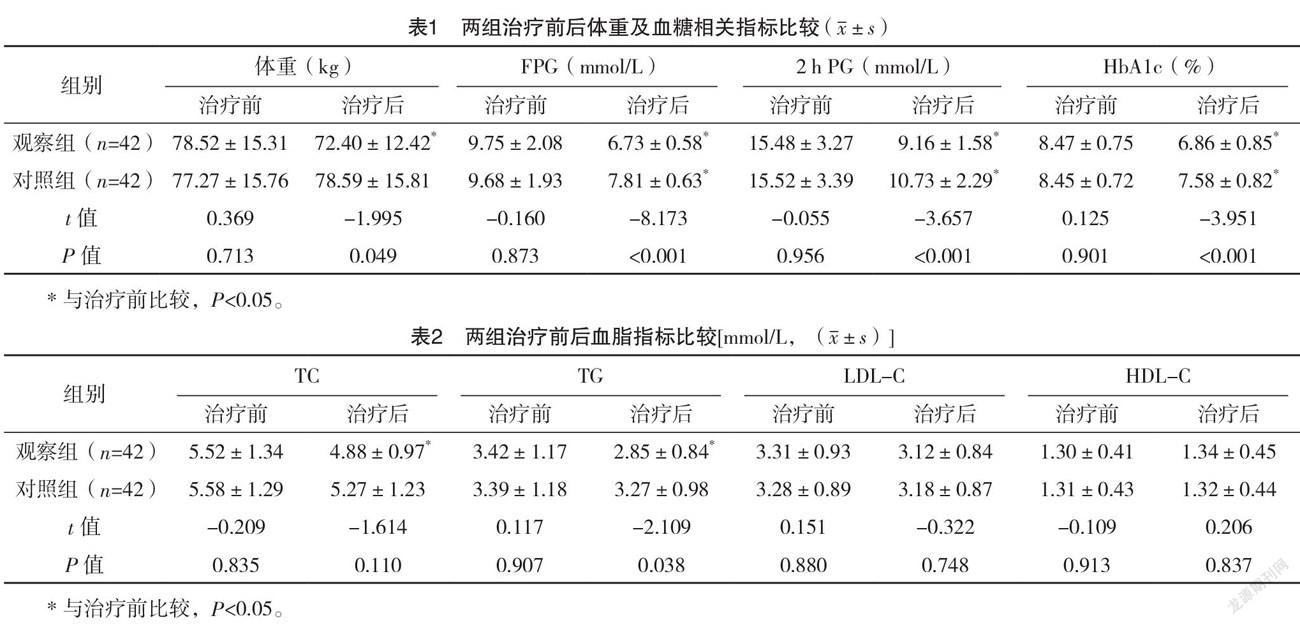
2.2 两组治疗前后体重及血糖相关指标比较 两组治疗前体重、FPG、2 h PG、HbA1c比较,差异均无统计学意义(P>0.05)。观察组治疗后体重较治疗前下降且低于对照组(P<0.05);对照组治疗前后体重比较,差异无统计学意义(P>0.05)。观察组治疗后体重减少≥5%者占比为26.19%(11/42)高于对照组的2.38%(1/42),差异有统计学意义(字2=9.722,P=0.002)。治疗后,两组FPG、2 h PG、HbA1c均较治疗前下降,且观察组均优于对照组(P<0.05)。观察组治疗后HbA1c<7.0%者占比为59.52%(25/42)高于对照组的35.71%(15/42),差异有统计学意义(字2=4.289,P=0.038)。见表1。
2.3 两组治疗前后血脂指标比较 两组治疗前各血脂指标比较,差异均无统计学意义(P>0.05)。对照组治疗前后各血脂指标比较,差异均无统计学意义(P>0.05)。观察组治疗后TC、TG均低于治疗前,且TG低于对照组(P<0.05)。观察组治疗后LDL-C及HDL-C与对照组和治疗前比较,差异均无统计学意义(P>0.05)。见表2。
2.4 兩组治疗前后血压、UA、Scr比较 两组治疗前SBP、DBP、UA、Scr比较,差异均无统计学意义(P>0.05)。对照组治疗前后SBP、DBP、UA、Scr比较,差异均无统计学意义(P>0.05)。观察组治疗后SBP、DBP均低于对照组和治疗前(P<0.05);观察组治疗后UA、SCR与对照组和治疗前比较,差异均无统计学意义(P>0.05)。见表3。
2.5 两组不良反应发生情况比较 两组均无严重不良反应发生。两组不良反应发生率比较,差异无统计学意义(P>0.05),见表4。
3 讨论
近年来针对T2DM患者的降糖药物逐渐增多,在药物选择方面不仅要考虑其控制血糖的效果,对患者体重、心血管危险因素的影响也成为降糖药物选择的重要参考指标[10]。二甲双胍是T2DM初始治疗的基石药物,对改善血糖及体重均有效,对于二甲双胍治疗血糖控制不佳的患者常需联合用药,如磺脲类、噻唑烷二酮类、DPP-4抑制剂、SGLT2抑制剂、胰高血糖素样肽1(GLP-1)受体激动剂或基础胰岛素[11]。SGLT2抑制剂通过抑制肾脏葡萄糖重吸收促进尿中多余葡萄糖的排泄,并独立于胰岛素发挥作用,而DPP-4增强葡萄糖依赖性胰岛素分泌并抑制胰高血糖素分泌[12-13]。一项比较荟萃分析表明,初始治疗中加入的每一类药物通常都会使HbA1c降低0.9%~1.1%,因此,将DPP-4抑制剂与SGLT2抑制剂联合使用有可能降低HbA1c[11-14]。已有研究表明,SGLT2抑制剂达格列净联合DPP-4抑制剂沙格列汀治疗T2DM效果显著,且较单独添加任何一种药物都能够更好地改善血糖控制[8-9,15-16]。
本研究中观察组加用达格列净及沙格列汀治疗,而对照组选择添加T2DM二线治疗药物格列美脲进行治疗。治疗后两组FPG、2 h PG、HbA1c均较治疗前下降,而观察组下降更明显,且观察组治疗后HbA1c<7.0%占比高于对照组(P<0.05),说明达格列净联合沙格列汀具有更好的控制血糖的效果,越来越多的证据也表明,对于HbA1c水平较高的患者,联合使用具有互补作用机制的抗糖尿病药物比单独添加每种药物有更好的疗效[7,15]。观察组治疗后体重、TG、SBP、DBP均较治疗前下降,且均低于对照组,治疗后体重减少≥5%者占比高于对照组(P<0.05),联合用药除降糖效果外,可同时获得减轻体重、降低血脂及血压的额外收益,有利于减少微血管及大血管并发症的发生,与文献[5,17]结论一致;DPP-4抑制剂延迟胃排空、降低食欲,SGLT2抑制剂对能量代谢途径的干预可能为体重、TG下降的原因[18],此前也已在SGLT2抑制剂治疗中观察到其降低血压的效应,并认为与药物的渗透、利钠和减肥作用有关[19]。曲建昌等[7]研究分析认为SGLT2抑制剂可降低UA水平,但对Scr无影响,可能与其增加尿糖排出同时增加尿酸排出有关,而本研究中两组治疗前后UA及Scr比较,差异均无统计学意义(P>0.05),可能与患者选择、研究时间等有关。两组不良反应发生率比较,差异无统计学意义(P>0.05),联合用药并未增加不良反应,证明了其安全性。有研究表明,与格列美脲相比,达格列净更易导致尿路及生殖器感染,可能机制为沙格列汀增强总体血糖控制,从而减少达格列净介导的糖尿从而减少感染有关[20]。
综上所述,与格列美脲相比,在二甲双胍控制不佳T2DM患者中,同时添加达格列净及沙格列汀可显著改善血糖、体重、血压及TG水平,且并未明显增加不良反应。
参考文献
[1]中华医学会糖尿病学分会.中国2型糖尿病防治指南(2017年版)[J].中华糖尿病杂志,2018,10(1):4-67.
[2] VILSB?LL T,EKHOLM E,JOHNSSON E,et al.Dapagliflozin Plus Saxagliptin Add-on Therapy Compared With Insulin in Patients With Type 2 Diabetes Poorly Controlled by Metformin With or Without Sulfonylurea Therapy:A Randomized Clinical Trial[J].Diabetes Care,2019,42(8):1464-1472.
[3] GARBER A J,ABRAHAMSON M J,BARZILAY J I,et al.
Consensus statement by the american association of clinical endocrinologists and american college of endocrinology on the comprehensive type 2 diabetes management algorithm-2017 executive summary[J].Endocr Pract,2017,23(2):207-238.
[4] SOLA D,ROSSI L,SCHIANCA G P,et al.Sulfonylureas and their use in clinical practice[J].Arch Med Sci,2015,11(4):840-848.
[5] FRIAS J P,GONZALEZ-GALVEZ G,JOHNSSON E,et al.
Efficacy and safety of dual add-on therapy with dapagliflozin plus saxagliptin versus glimepiride in patients with poorly controlled type 2 diabetes on a stable dose of metformin:Results from a 52-week,randomized,active-controlled trial[J].Diabetes Obes Metab,2020,22(7):1083-1093.
[6] MATHIEU C,HERRERA MARMOLEJO M,GONZALEZ GONZALEZ J G,et al.Efficacy and safety of triple therapy with dapagliflozin add-on to saxagliptin plus metformin over 52 weeks in patients with type 2 diabetes[J].Diabetes Obes Metab,2016,18(11):1134-1137.
[7]曲建昌,弓月,王彤,等.达格列净联合二肽基肽酶4抑制剂和二甲双胍治疗血糖控制不佳2型糖尿病的效果分析[J].中国医药,2021,16(6):857-860.
[8]韩荣凤,李俊峰,刘英,等.SGLT-2抑制剂联合二甲双胍与DPP-4抑制剂治疗2型糖尿病的疗效观察[J].中华内分泌代谢杂志,2019,35(5):387-390.
[9] ANGWIN C,JENKINSON C,JONES A,et al.TriMaster:randomised double-blind crossover study of a DPP4 inhibitor,SGLT2 inhibitor and thiazolidinedione as second-line or third-line therapy in patients with type 2 diabetes who have suboptimal glycaemic control on metformin treatment with or without a sulfonylurea—a MASTERMIND study protocol[J/OL].BMJ Open,2020,10(12):e042784.
[10] COPPENRATH V A,HYDERY T.Dapagliflozin/Saxagliptin Fixed-Dose Tablets:A New Sodium-Glucose Cotransporter 2 and Dipeptidyl Peptidase 4 Combination for the Treatment of Type 2 Diabetes[J].Ann Pharmacother,2018,52(1):78-85.
[11] MONICA REDDY R P,INZUCCHI S E.SGLT2 inhibitors in the management of type 2 diabetes[J].Endocrine,2016,53(2):364-372.
[12] NAUCK M.Incretin therapies:highlighting common features and differences in the modes of action of glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors[J].Diabetes Obes Metab,2016,18(3):203-216.
[13] ABDUL-GHANI M.Where does combination therapy with an SGLT2 inhibitor plus a DPP-4 inhibitor fit in the management of type 2 diabetes?[J]Diabetes Care,2015,38(3):373-375.
[14]徐玉凤,吴佩丽,温伟恒,等.二甲双胍、沙格列汀、达格列净三联短期强化降糖:54例新诊断2型糖尿病的多中心前瞻性临床试验[J].南方医科大学学报,2019,39(11):1305-1311.
[15] ROSENSTOCK J,HANSEN L,ZEE P,et al.Dual add-on therapy in type 2 diabetes poorly controlled with metformin monotherapy:a randomized double-blind trial of saxagliptin plus dapagliflozin addition versus single addition of saxagliptin or dapagliflozin to metformin[J].Diabetes Care,2015,38(3):376-383.
[16] M?LLER-WIELAND D,KELLERER M,CYPRYK K,et al.
Efficacy and safety of dapagliflozin or dapagliflozin plus saxagliptin versus glimepiride as add-on to metformin in patients with type 2 diabetes[J].Diabetes Obes Metab,2018,20(11):2598-2607.
[17] R?DHOLM K, WU J H, WONG M G,et al.Effects of sodium-glucose cotransporter-2 inhibitors on cardiovascular disease,death and safety outcomes in type 2 diabetes-a systematic review[J].Diabetes Res Clin Pract,2018,140:118-128.
[18] J?STR?M C D,JOHANSSON P,PTASZYNSKA A,et al.
Dapagliflozin lowers blood pressure in hypertensive and non-hypertensive patients with type 2 diabetes[J].Diab Vasc Dis Res,2015,12(5):352-358.
[19] FADINI G P,BONORA B M,MAYUR S,et al.Dipeptidyl peptidase-4 inhibitors moderate the risk of genitourinary tract infections associated with sodium-glucose co-transporter-2 inhibitors[J].Diabetes Obes Metab,2018,20(3):740-744.
(收稿日期:2021-11-08) (本文編辑:田婧)
