Conservative treatment of knee osteoarthritis:A review of the literature
2022-04-06WeiBoonLimOdayAlDadah
INTRODUCTION
Traditionally,osteoarthritis is considered a degenerative disease that leads to loss of articular cartilage,bone remodelling(osteophyte formation),subchondral sclerosis and subchondral cysts.Articular cartilage is a shock-absorbent connective tissue that provides a smooth surface to minimise friction upon joint movement.The above changes lead to joint dysfunction and hence pain worsened upon activity,stiffness and loss of function.However,more recent studies[1,2]have shown that the pathogenesis is much more complex with metabolic and inflammatory aspects to it.
TREATMENT OPTIONS
The main overarching aim of conservative treatment is to provide symptomatic relief of the disease and slow its progression to avoid or forestall end-stage surgical options(total knee placement).The various conservative treatment options include exercise,weight loss,pharmacological agents and orthotics.
EXERCISE
Exercise therapy is core treatment in knee osteoarthritis(KOA)with the benefits of exercise having been linked to muscle strengthening and hypertrophy,weight management and even potential diseasemodifying effects.The 2007 Osteoarthritis Research Society International(OARSI)guidelines[3]for management of KOA stated that exercise was strongly endorsed with 21 items recommending aerobic and strengthening exercises and a further 8 items recommending water-based exercises.Currently,an exercise regime is strongly recommended as 1line treatment by international guidelines with strong evidence supporting its effectiveness[4,5].Uthman[6]concluded that it is unlikely further clinical trials comparing exercisenon-exercise will ever contradict the clear benefit of the former.Consequently,this review will focus on the effectiveness of mind-body exercises,balance exercises and general recreational physical activity(walking)that are often under-reported.
Mind body exercises
Mind-body exercises,including Tai Chi and Yoga,combine physical activity,mental focus and controlled breathing.In a single-blinded randomised controlled trial(RCT)comparing Tai Chi with standard physical therapy for KOA,Wang[7]concluded that both interventions showed improvements in Western Ontario and McMaster Universities Osteoarthritis Index(WOMAC)scores and most secondary outcomes at the post-intervention period and 52 wk follow-up.Notably,the Tai Chi group demonstrated superiority in terms of depression and the physical component in quality of life.Secondary analysis of the same trial concluded that patients begin to notice the improvements after 2-5 wk[8].Other studies have also supported the effectiveness of yoga in KOA.In a RCT of 113 patients older than 60 years with self-reported KOA,Cheung[9]reported that both yoga and the control aerobic/strengthening exercises resulted in improved pain relief and physical function.Moreover,perhaps due to the inclusion of meditation and standing-up exercises,the 8-wk yoga program was superior in terms of improving anxiety and fear of falling.As a result,the above studies show the potential of mind-body exercises over traditional standard physical therapy for a more holistic approach.
Balance training
Balance training has been shown to be effective for KOA in improving mobility and reduce pain and falls risk.Liao[10]in a RCT reported that addition of balance exercises to conventional training further improved function such as stair climbing and standing from a seated position.Balance training has also been shown to be as effective in pain reduction as strength training in a RCT by Chaipninyo[11].Holistic exercise programmes that incorporate balance exercises have also been shown to reduce falls risk in a systemic review by Sherrington[12].
Non-strenuous activities
The benefits of recreational non-strenuous activity such as walking differ based on the pre-existing severity of KOA and length of activity.In a RCT by Wallis[13]of 46 patients with severe KOA,a 12-wk walking program of 70 min per week was not effective in decreasing knee pain as compared to the control group receiving standard care.They concluded that walking may have cardiovascular benefits without relieving knee pain.However,it must be noted that the patients recruited had grade III or IV osteoarthritis and hence walking might not have significant benefits at a severe stage.In addition,excessive recreational physical activity might lead to worsening outcomes.In a clinical study assessing the dose response of walking for patients with severe KOA(Grade III and IV),Wallis[14]found that there was a higher risk of adverse events leading to worsening knee pain beyond 70 min per week of supervised walking.However,in a RCT of patients with mild to moderate KOA,Alghadir[15]concluded that a 6-wk walking program of 30 min a week resulted in greater pain relief,physical function and quadriceps muscle strength.Farrokhi[16]recommended shorter interval bouts of walking over continuous and longer sessions due to reported knee pain and undesirable knee loading when patients walk continuously for 30 min or more.Therefore,increased general activity might be more effective in mild to moderate KOA at a lower dose to prevent adverse symptoms.
They were lucky enough to escape the soldiers of King Bruin, and at last, after unheard-of fatigues3 and adventures, they found themselves in a charming green valley, through which flowed a stream clear as crystal and overshadowed by beautiful trees
However,most research trials tend to recruit patients who are physically inactive and it is questionable whether patients who are already physically fit can expect to experience the same magnitude of benefits.In the data analysis of 12796 patients in the nationwide physical exercise program for patients with KOA in Denmark,Skou[17]concluded that all patients regardless of baseline physical activity level can expect to see similar pain reduction at both post-intervention and the 12 mo mark.
Exercise regimen prescription
Prescription of an exercise regime can also be further complicated by the large number of exercises available and variable dosage in terms of frequency,sets and repetition.In addition,there have been far less research done that directly compares different exercises due to the cost and sheer number of exercises available.In a recent systematic review and network meta-analysis,Goh[18]classified exercises into aerobic,mind-body,strengthening,flexibility/skill and mixed types.Overall,mixed exercises that targeted multiple physical domains were the least effective for unknown reasons whereas other exercises were superior in some target outcomes.
In a single-blinded RCT of 78 patients with grade II or III KOA,Kabiri[19]reported that a supervised exercise program including resistance training and aerobic training resulted in significant improvements in pain relief and physical function.However,the arm ergometer group demonstrated superior reduction in Visual Analogue Scale(VAS)and change of function in the Knee injury and Osteoarthritis Outcome Score dimension while the treadmill group was superior in the timed up and go test.Therefore,this reinforces the possibility of customising exercises to better target desired outcomes in patients.Moreover,in a RCT of elderly patients with pre-radiographic KOA,Suzuki[20]concluded that a well-rounded program that targeted overall muscle strength with flexibility was more effective than targeting certain groups.
We had a family. A name and address from the church, we knew the situation, dad s been out of work, the baby s been sick, mom didn t want to put up a Christmas tree because she didn t want the children to be disappointed when Santa didn t come. The Power Company had shut the gas off once, but the church had paid the bill.
Aquatic exercises
Intra-articular corticosteroids(IACs)are frequently-used as an adjunctive treatment for pain control in KOA due to its anti-inflammatory effect.Recommendation for use of IACs in treatment of KOA is variable.While the American Academy of Orthopaedic Surgeons[79]found it inconclusive,other organisations such as NICE[43],OARSI[80]and American College of Rheumatology[5]have recommended or conditionally recommended its use.
Mode of delivery of exercises
Despite the proven benefits of exercise therapy in KOA,several studies have noted low compliance rates.An important factor affecting compliance is mode of delivery which can include supervised or internet or home based.In a randomised clinical trial comparing internetsupervised based sessions,Allen[22]identified baseline body mass index(BMI)and symptom duration as factors that affected the effectiveness of the program.Data analysis from the study showed that patients with low BMI had greater improvements through internet-based exercise sessions while those with high BMI and longer history of symptoms benefitted more from physical therapy.In another RCT comparing a month of supervised exercise in the clinicunsupervised sessions at home for KOA,Deyle[23]reported that both were effective but the supervised sessions was twice as effective in terms of pain,stiffness and function.Therefore,it might be more appropriate to use supervised sessions when KOA is more severe or patient has greater co-morbidities or low compliance.Another mode to consider would be groupindividual therapy.In a single-blinded randomised clinical trial comparing groupindividual approach,Allen[24]found that 12 wk of both approaches were effective in improving WOMAC and physical performance without significant difference between them.
Integration of exercise and patient education
ESCAPE-knee pain rehabilitation program is a community-based exercise rehabilitation program that combines exercise and patient-education to encourage self-management of osteoarthritis and patient empowerment.The program is supported by National Health Service England and widely available across the United Kingdom.In a RCT by Hurley[25]concluded that the ESCAPE program was effective,cost-efficient and resulted in better functional outcomes over conventional primary care.The clinical and cost benefits persisted 30 mo after completion of the rehabilitation program.The program was also equally effective regardless of being implemented on an individual or collective group basis.An RCT by Jessep[26]also supported the economic efficiency of the program over outpatient physiotherapy.While both methods had similar clinical benefits,the ESCAPE program had a lower cost per person and healthcare utilisation cost.Qualitative interviews by Hurley[27]concluded that the ESCAPE program enables patients to have greater confidence in the safety,effectiveness and applicability of exercising to improve their condition.Hence,it is evident that a holistic exercise program is able to achieve both physiological improvements and psychosocial benefits that fosters health beliefs and behaviours.
WEIGHT LOSS IN KNEE OSTEOARTHRITIS
The OARSI guidelines[28]for KOA noted that 13 international guidelines recommended weight loss as a core treatment.High BMI is a risk factor for developing KOA and has been associated with worse outcomes following knee replacement surgery.
Many studies have shown the effectiveness of weight management.In a randomised trial of 80 obese patients with KOA,Christensen[29]found that a low energy diet was significantly superior over the control education group in improving physical function over 8 wk.In addition,they concluded that body fat reduction was significantly associated with increase in function and a 10% bodyweight reduction would result in a 28% increase in function.In another clinical study by Coriolano[30]they found that weight loss of 16.5% in bodyweight through a diet program resulted in significant pain and function improvement.The benefits of the diet program were sufficient for patients to postpone their need for total knee replacement surgery.In addition,in the long-term Osteoarthritis Initiative cohort study,Gersing[31]reported that weight loss was associated with slower cartilage deterioration especially in the medial compartment.It should be noted that the benefits for cartilage loss was only seen in groups that had lost weight through dieting as opposed to exercise.Hence,it is evident that weight loss is effective in treating KOA,both short-term and long-term.
Then he smeared22 the dirty water all over the rabbit s face and paws, so that it might look as if it were he who had been disobeying Big Lion s orders
Weight loss is often promoted in tandem with exercise therapy and the combination of both interventions has been shown to be more effective.In a single-blinded RCT of 316 patients with symptomatic KOA,Messier[34]compared the effectiveness of exercise and weight reduction measured in primary(WOMAC function index)and secondary(functional tests,pain and stiffness score,joint space width)outcomes.The clinical study concluded that a combination of both interventions was superior over either intervention alone in self-reported pain and function,and physical performance.The benefits were maintained for 12 additional months.Moreover,in the Osteoarthritis Initiative,it was noted that slower cartilage loss was seen in the diet and diet plus exercise group,but not in the exercise only group[31].Therefore,this highlights the increased effectiveness in combining both weight loss and exercise intervention.
However,there have been doubts about the viability of weight loss programs in the long run due to the possibility of regaining weight or potentially negative side-effects of weight cycling.Weight cycling refers to periods of weight loss followed by weight gain which can lead to adverse events such as increased metabolic risk.However,in a randomised trial comparing intermittent weight cycling through low-energy dietsteady weight loss through daily meal replacements over 3 years,Christensen[35]concluded that both strategies with dietary counselling were equally viable and effective with a good safety profile.Firstly,both structured diet programs were effective in maintaining weight loss without rebounding.In addition,the benefits of weight loss on symptom relief and cardiovascular disease risks were maintained over 3 years.Hence,this emphasises the effectiveness of weight loss as long as a structured program is in place to ensure patient compliance.
PHARMACOLOGICAL MANAGEMENT IN OSTEOARTHRITIS
Originally,the World Health Organisation(WHO)analgesic pain ladder was established for treatment of cancer pain in 1986.The WHO ladder consisted of the following steps:Step I with non-opioid analgesics[acetaminophen or nonsteroidal anti-inflammatory drug(NSAIDs)],Step II with weak opioids and step III with strong opioids.This approach has been extrapolated to pain management for osteoarthritis and involves going to the next step if the current step was inadequate for pain relief.However,such an approach has now been questioned due to the multiple pain modalities present in KOA.
Acetaminophen/paracetamol
Even though acetaminophen is often recommended as first-line analgesia,its effectiveness is questionable and it was not recommended in the most recent OARSI guidelines[4]for KOA.In a double-blinded RCT involving 779 patients with KOA,Miceli-Richard[36]concluded that acetaminophen at 4 g/day taken over 6 wk did not demonstrate statistically superior results over placebo in terms of knee pain intensity and assessment of their condition.The use of acetaminophen was well-tolerated with a good safety profile.In a separate double-blinded RCT by Case[37],acetaminophen similarly did not demonstrate statistically or clinically meaningful results over placebo as assessed by the WOMAC index.Although other trials by Prior[38]and Altman[39]do support the effectiveness of acetaminophen,the Cochrane systematic review for paracetamol in KOA concludes that the benefits for pain and physical function are small and are clinically unimportant[40].Therefore,recommendation of acetaminophen as first-line analgesic medication should be reconsidered.
However,acetaminophen might be valuable for its advantageous synergistic effect when combined with other analgesics for pain relief.Pareek[41]in a randomised multicentre study demonstrated that the combination of aceclofenac and acetaminophen was superior over monotherapy in rapid pain relief for osteoarthritic flare-ups.However,Doherty[42]in a randomised double-blinded study concluded that while the combination of paracetamol and ibuprofen was superior for pain relief over paracetamol alone,it was not significantly superior over ibuprofen alone.In addition,patients taking two ibuprofen/paracetamol tablets were found to be at greater risk of reduction in haemoglobin levels due to gastrointestinal(GI)blood loss than either monotherapy alone.This suggests a synergistic interaction between paracetamol and ibuprofen in causing GI complications.
NSAIDs
NSAIDs work by inhibiting cyclo-oxygenase enzymes,and in turn reducing prostaglandin levels.Hence,this leads to a reduction in pain and inflammation.NSAIDs can be classified into non-selective or selective COX-2 inhibitors,as well as topical and oral formulations.The National Institute for Health and Care Excellence(NICE)[43]recommends topical NSAIDs before systemic analgesics(oral NSAIDs,COX-2 inhibitors and opioids)for KOA.The OARSI guidelines[44]also consider topical NSAIDs to be safer and better tolerated than oral NSAIDs.
Comparison of selective and non-selective NSAIDs
Head-to-head trials have shown both classes to have comparable effectiveness.In a 6-wk RCT comparing efficacy of celecoxib(COX-2 selective NSAID)ibuprofen(non-selective NSAID)for KOA,Gordo[45]concluded that both were similarly effective and well-tolerated.Pooled results from two placebo-controlled trials[46]showed that both Naproxen(non-selective NSAID)and Celecoxib(COX-2 selective NSAID)resulted in early significant pain relief based on WOMAC score by the second day of treatment and analgesic effect was maintained for 12 wk.However,while both treatments were statistically superior over placebo at week 6 based on the OMERACT-OARSI response,Naproxen remained superior at week 12 but Celecoxib was not.
Instead,the bigger difference would be tolerability and safety profile.COX-2 selective inhibitors have been thought to cause fewer GI side-effects as the inhibition of COX-1 is responsible for the associated GI toxicity.In the CONDOR randomised trial,Chan[47]reported that the risk of GI complications was lower in the patient group taking COX-2 selective NSAIDs than in patients taking non-selective NSAIDs with a proton pump inhibitor.There is an increased risk of GI complications with prolonged intake and in patients over 70 years of age.
In terms of cardiovascular risks,both classes appear to have similar risks.Two population-based analysis studies in Taiwan and Finland reported that use of all NSAIDs increase the risks of cardiovascular events[48,49].A meta-analysis[50]concluded that naproxen,out of all the NSAIDs,is associated with the least vascular risks.Overall,NSAIDs have varying safety profiles and prescription of the most appropriate drug should be done based on the balance of benefitsrisks to the individual patient.In a network meta-analysis[51],Naproxen was ranked as the most effective conservative treatment of KOA,coupled with its good relative safety and low cost to improve pain and function.
Oral vs topical NSAIDs
Despite oral NSAIDs being a step-up in pharmacological pain management,oral NSAIDs are not shown to be superior in studies.Tugwell[52]in a RCT reported that oral and topical preparations of diclofenac were equivalent in symptomatic relief of KOA.While the topical form resulted in minor local skin irritation,the oral form had significantly greater systemic side-effects and abnormal laboratory tests(liver function tests,haemoglobin and creatinine clearance).In the TOIB RCT comparing topical and oral ibuprofen for chronic knee pain,Underwood[53]reinforced that both formulations were similar in effectiveness but oral NSAIDs produced more instances of minor adverse side-effects.However,neither resulted in significant improvements in WOMAC scores from baseline to follow-up at one year,hence this shows that neither preparation is particularly effective in some patients.
Clegg[122]in a large RCT of 1583 patients concluded that neither glucosamine nor chondroitin sulfate taken alone or together reduced pain effectively and was not significantly better than placebo.Part of the centres of the above GAIT trial also participated in an ancillary study whereby Swaitzke[123]reported that neither glucosamine nor chondroitin sulfate alone or in combination had a predefined clinically important difference on progress of joint width space narrowing.However,they did note that patients with Kellgren-Lawrencegrade II KOA showed the greatest potential for diseasemodifying effect by these treatments.In a more recent RCT by Fransen[124]the study similarly reinforced the ineffectiveness of glucosamine and chondroitin for symptomatic benefit over placebo.However,patients taking the glucosamine-chondroitin combination had a statistically significant reduction in progress of joint space narrowing at 24 mo.This could be due to the lower percentage of patients with moderate to severe KOA compared to the GAIT trial.
Evidence regarding the safety and effectiveness of opioids are still contradictory based on current literature with mixed recommendations from guidelines.The latest OARSI guidelines[4]strongly recommends against opioid use due to the risk of potential dependency,be it transdermal or oral form.However,the latest American College of Rheumatology guidelines[5]conditionally recommends Tramadol over non-Tramadol opioids if opioids are considered.Non-tramadol opioids are only recommended if alternatives are exhausted and should be used at the lowest possible dose for the shortest possible time.
Opioids can generally be classified as weak or strong(Table 1).
But in a few minutes a maid saw him, and said to her master, I pray you, sir, to drive away that beggar who is sitting on the steps, or he will fill the whole house with his dirt
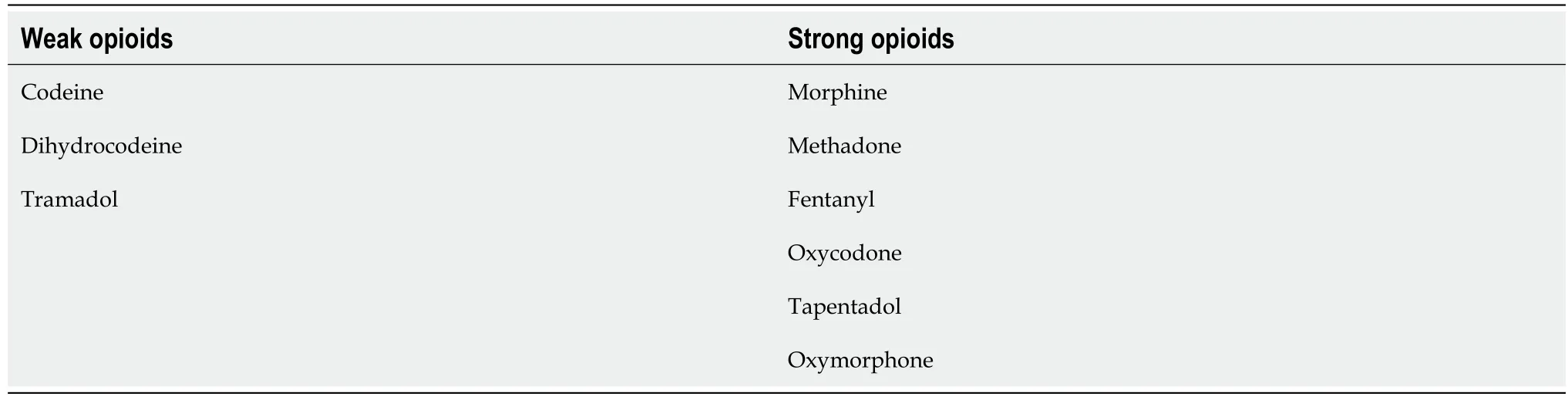
Research has generally supported the effectiveness of weak and strong opioids over placebo for pain relief.Peloso[54]in a RCT reported that controlled release codeine was statistically superior over placebo in improving pain,stiffness and physical function based on the WOMAC subscales.Also,in a non-inferiority trial,Conaghan[55]concluded that buprenorphine patches with oral paracetamol and co-codamol tablets were effective in significantly reducing patients’ pain over 7 d of treatment.However,over 80% of patients in both groups reported adverse events and the study was limited by its high withdrawal rate in both groups.
Tramadol’s mechanism of action is unique as it is not only a weak opioid receptor agonist,but also modulates norepinephrine and serotonin levels.Current clinical trials have shown tramadol to have mixed effectiveness.In a RCT of 1020 adults with osteoarthritis of the knees or hips,Gana[56]reported that tramadol at 200-300 mg once daily was statistically superior over placebo for improvements on pain,physical functioning but did not reach significance for subject global assessment of disease activity.Post-hoc data analysis by Kosinski[57]revealed tramadol also improved sleep quality and decreased pain-related sleep disturbance.However,in another RCT by DeLemos[58],the 100 mg and 200 mg dosages were not superior over placebo in any of the primary end-points.As for the 300 mg dose,significant improvements were achieved in patient global assessment of disease activity but not in WOMAC pain and physical function scores.Addition of tramadol at 200 mg per day has also been shown to allow significant naproxen dose reduction in patients taking them based on a placebo-controlled study by Schnitzer[59].
Due to the mixed effectiveness shown,the paper looked towards systematic reviews to ascertain effectiveness of tramadol.In the latest Cochrane review for tramadol[60],tramadol alone or combined with acetaminophen is not likely to be clinically important in improving pain or function in patients,but an additional 5% of patients do report a clinically important improvement of 20% or more in pain relief compared to placebo.
Head to head trials have also shown tramadol to be comparable to other opioids.In a randomised parallel trial comparing tramadol and dihydrocodeine,Wilder-Smith[61]reported that strong osteoarthritic pain insufficiently controlled by NSAIDs alone was controlled by both medication by the second day.While tramadol was superior for analgesia at rest and interfered less with GI function,it resulted in greater sedation and drowsiness as compared to dihydrocodeine.Karlsson[62]in a randomised non-inferiority trial of patients with chronic osteoarthritis pain reported that tramadol tablets were comparable to buprenorphine patches.
IACs have shown a good safety profile but long-term safety profile of IACs has been inconclusive.Raynauld[88]in a RCT comparing intra-articular injections of steroids against saline,concluded that long-term IACs was safe and did not negatively affect the knee joint.However,McAlindon[87]concluded that IACs resulted in significantly greater loss of cartilage volume compared to intra-articular injection of saline.In the recent Osteoarthritis Initiative observation study[89],IACs and especially repeated IACs may be associated with greater risk of radiographic KOA progression.
Despite opioids being recommended as a last pharmacological resort when all alternatives fail,their use has not been shown to be superior over non-opioid in non-inferiority trials.In the SPACE trial comparing non-opioids and opioids for moderate to severe chronic osteoarthritis,Krebs[66]concluded that opioid therapy should not be initiated as they were not superior for pain relief,function and quality of life.Instead,the opioid group had significantly more medication-related sideeffects and higher pain intensity over 12 mo.Beaulieu[67]also reported that tramadol and diclofenac were equally effective in pain relief and functional improvement.In another systematicreview comparing pain reduction,Smith[68]reported that NSAIDs,strong and weak opioids all have similar analgesic.Therefore,the lack of a demonstrable difference between strong and weak opioids suggests the need for more comparative trials in chronic non-cancer pain.Elderly patients prescribed opioids as opposed to NSAIDs also have a significantly greater risk of falls and fractures by 4.1 times[69].
Despite lack of evidence for clinical superiority over placebo,meta-regression in systematic reviews[70,71]have shown them to have small or no clinical impact on pain relief and functional improvements.Their effectiveness is also compromised by their high incidence of adverse events and side-effects as demonstrated by the high withdrawal rates in clinical studies although this can be partially mitigated by titration as many clinical studies often start with a non-titrated dose.Side-effects include GI adverse events(constipation,nausea,vomiting);central nervous system events(sedation,dizziness);dermatological events(pruritus,rashes)[72].
Opioid use also leads to poor long-term outcomes and result in both peri-operative and postoperative complications.In terms of post-operative complications,pre-operative opioid use has been linked to a greater likelihood of chronic opioid use following surgery[73];greater risk of adverse outcomes that includes peri-prosthetic joint infection[74],higher hospital readmission rates[75]and post-operative pain[76].The higher risk of complications would further obfuscate management as patients would need to wean or reduce their opioid use for several months prior to the surgery[77].In terms of peri-operative complications,long-term opioid use can result in hyperalgesia and tolerance[78].This would make it more difficult to provide adequate peri-operative and post-operative analgesia in patients undergoing knee replacement(or any form of)surgery.
It has been proposed that aquatic exercises have certain advantages over land-based ones such as pain reduction and reduced joint loading due to the buoyancy of the water.However,in a single-blinded randomised trial comparing land basedwater based exercise,Wang[21]concluded that both types of exercises demonstrate benefits in pain relief,physical function and quality of life without significant differences between them.Instead,they recommended that choice should be based on the patient’s preference and convenience.
Clinical studies have affirmed the effectiveness of IACs as an adjunctive therapy for short-term pain relief and the effectiveness of IACs in the literature has varied from 4 wk up to 26 wk.A network metaanalysis of conservative treatments[51]concluded that IACs provided the greatest short-term pain relief from 4 to 6 wk.In a RCT comparing a single intra-articular injection of hyaluronic acid and triamcinolone acetonide,Tammachote[81]concluded that IACs resulted in improved pain,function and knee range of motion without any serious adverse events that was present in the 1week and lasted for 6 mo.However,Yavuz[82]reported in a prospective study that all three IACs(methylprednisolone,betamethasone and triamcinolone)were effective but their benefits declined at week 12.Regarding the choice of corticosteroid administered,the literature has been mixed.Lomonte[83]supported that both methylprednisolone and triamcinolone were equally effective for sustained improvement in pain and function up to 24 wk whereas Yavuz[82],reported that Methylprednisolone also provided better analgesia until the 6week.The effectiveness of IACs is also independent of the injection site.In a RCT of 60 patients with KOA receiving IACs,Parrilla[84]concluded that corticosteroids resulted in a clinically significant pain improvement regardless of the injection site.
However,IACs have not shown synergistic benefits when combined with other conservative treatments.A RCT by Henrikson[85]concluded that addition of IACs to physical therapy provided no further benefits.Another RCT by Deyle[86]also showed that physical therapy was superior over IACs in the long-term with less pain and functional disability.
Furthermore,the effectiveness of repeated IACs has been shown to be variable.In a randomised placebo-controlled trial,McAlindon[87]concluded that repeated IACs every 3 mo did not result in superior knee pain control over saline injections.However,intra-articular injections of triamcinolone acetonide at the same dose resulted in significant improvement in knee pain and stiffness over 2 years in a RCT by Raynauld[88].
In a randomised controlled study by Matsumoto[63],oxymorphone resulted in superior pain relief and functional improvements over placebo in patients with osteoarthritic pain uncontrolled by other non-opioid analgesia.However,83% of patients reported at least one adverse event which were mild to moderate and was the biggest reason for patient withdrawal.Conversely,Caldwell[64]in an RCT reported that morphine sulphate only resulted in statistically significant pain relief but not physical function.While opioids have been shown to maintain their analgesic effect in the long-term for open-label extension studies,Bialas[65]concluded that such studies are limited due to the low-quality evidence and high dropout rates.
Hyaluronic acid is a glycosaminoglycan naturally found within the knee joint that decreases with the progression of osteoarthritis.Its anti-arthritic effects have been hypothesised to be due to multiple mechanisms of action including chondroprotection,joint lubrication,shock absorption,anti-inflammation and immune cells modulation.Intra-articular hyaluronic acid(IAHA)is an alternative to IACs but recommendation among national and international guidelines for its use in KOA remains inconclusive.The OARSI guidelines[4]state that IAHA treatment is conditionally recommended for longer term treatment effects in patients with KOA whereas NICE guidelines[43]do not recommend it.
29.The Master Cat: The original French is Le maitre chat. Perrault uses the French familiar term maitre, which referred to someone whose social standing was not very high. At the same time, he is playing with the word and using it in the sense of a teacher as master who instructs a young man and determines the events in the story. (Zipes 2001, 397).Return to place in story.
Research studies have shown IAHA and IACs to have comparable efficacy with IACs providing greater pain relief in the short-term while IAHA provide greater pain relief in the long-term.In a randomised non-inferiority study by Tammachote[81],they concluded that both groups had similar symptomatic improvement by the end of six months.However,IACs resulted in better pain relief in the first week and greater functional improvement in the second week.In a multi-centre prospective study,Leighton[90]reported that IACs and IAHA were comparable throughout the first 12 wk but IAHA was superior for pain,stiffness and function from the 12to 26week.Bannuru[80]in a systematic review concluded that current evidence suggests corticosteroids to be more effective in the short term up to 4 wk,whereas hyaluronic acid is more effective beyond the 4week.Therefore,the differing therapeutic trajectory plays a key role in clinical prescription based on the patients’ symptoms and expectations.A randomised study by Ozturk[91]reported that the combination of IAHA and IACs was superior over hyaluronic acid alone,resulting in more rapid pain relief and to a lower level.This shows the potential of synergistic effects of combining both therapies.However,it should also be noted that available research trials have been criticised for publication bias and risk of selective reporting of outcomes in an analysis of randomised trials[92].
Repeated use of hyaluronic acid has also been shown to be effective with a good safety profile.In the AMELIA randomised controlled study,Navarro-Sarabia[93]found that patient responsiveness increased throughout the 40-mo study with repeated injections.In terms of symptom improvement,IAHA not only improve symptoms in-between injections but also had a carry-over effect that lasted for at least 1 year after the last injection.As for safety,incidence of adverse events did not differ from that of placebo’s and there were no serious adverse events.Neustadt[94]also reported that five injections of hyaluronic acid at weekly intervals up to 26 wk was associated with an excellent safety profile and only had minor local adverse reactions.Follow-up at 24 mo still supported the excellent safety profile of the injection.
Overall,the current literature suggests that hyaluronic is an effective alternative to corticosteroid injections with an excellent safety profile.
Capsaicin has been recommended by NICE[43]for adjunctive pain management in KOA.Its mechanism of action isselective depression of type-C nociceptive fibres.
Initial research regarding its effectiveness dates back to 1991 where Deal[95]reported that topical application four times daily resulted in significant pain relief compared to placebo.This was supported by subsequent research trials.In a double-blinded RCT,Kosuwon[96]further reported that 0.0125%capsaicin gel was effective for improving stiffness and function in patients with grade II and III Kellgren-Lawrence KOA.In a long-term extension trial of a RCT by Schnitzer[97]concluded that capsaicin cream was effective in all three primary end-points for patients with mild to moderate KOA who were already taking NSAID or COX-2 inhibitors.The efficacy was also maintained up to a year of continuous use.McCleane[98]has also highlighted the potential of combining capsaicin with glyceryl nitrate which resulted in reduced localised burning sensation and superior analgesic effects even in patients with osteoarthritis uncontrolled by other pharmacological treatments.However,the study did include patients with osteoarthritis in other joints besides knees which would affect the generalisability of its results.
Capsaicin also has a good safety profile due to its lack of systemic absorption.The main side-effect is a localised burning sensation but withdrawals due to this has been low in the afore mentioned research trials.
As a result,topical capsaicin is effective for mild to moderate KOA.More research would need to be done for patients with severe KOA or other co-morbidities as they are excluded in afore mentioned trials.
But, but, said the Prince, in his most impatient tone, old people should not be so long-winded! Tell me what country I have got into, and nothing else
Andwhen one looked at the fields, how beautifully the corn stood andhow green it shone, without comparison! and there was a twittering and a fluttering of all the little birds, as if the day were a greatfestival; and so it was, for it was Sunday
Flexiseq gel is marketed as an adjunctive analgesia that contains phospholipid vesicles that passes into the knee synovial joint where it provides lubrication to minimise friction between cartilage and hence reduces pain.In a RCT of 1395 patients with osteoarthritic knee pain,Conaghan[99]reported that Flexiseq gel was superior to oral placebo with comparable efficacy to oral celecoxib in pain reduction and functional improvement.There have also been an additional three clinical studies that used Flexiseq gel as a treatment arm[99-102].However,these clinical studies have shown low quality of evidence.All three of these clinical studies also involve Flexiseq gel as the topical placebo arm and there has been no comparison of Flexiseq gel against a true inactive topical gel to date to account for placebo effects.Furthermore,all the trials have the potential to introduce funding bias as they are sponsored by pharmaceutical companies.There is also limited evidence base for the analgesic mode of action as stated in NICE guidelines[103].
TRANSCUTANEOUS ELECTRICAL NERVE STIMULATION
Transcutaneous electrical nerve stimulation(TENS)therapy involves passing of electrical currents through electrodes placed on the targeted area to stimulate peripheral nerves for pain control.Delivery of the electrical currents can be of varying frequencies and intensity.Clinical studies examining the effectiveness of TENS therapy have shown that it is mostly ineffective with little clinical benefits for patients.
In a double-blinded RCT of 203 patients with KOA by Atamaz[104],application of TENS therapy did not result in a statistically significant or superior results in pain intensity or physical functioning over placebo treatments.While it was suggested that the lower intake of paracetamol in treatment groups suggested pain relief,lower intake was only present in the first 3 mo for the TENS group and did not persist to the end of the study.In addition,it would be difficult to attribute the improvements in assessment parameters to application of physical agents as every group also had a structured exercise and education program.In another RCT by Cheing[105],the combination of TENS and exercise training resulted in the best overall improvements in physical outcomes but this was not significantly superior over placebo stimulation.Another randomised placebo-controlled study by Fary[106]similarly showed that 26 wk of pulsed electrical stimulation was not more effective than placebo.Hence,the current literature does show that TENS therapy at best has small benefits that are not likely to be clinically meaningful.
KNEE BRACING
Knee bracing is often recommended as an adjunctive treatment in KOA.Proposed mechanisms of action for knee bracing include unloading of the medial compartment,or through general biomechanical and neuromuscular effects that lead to improved proprioception and joint stability.
However,clinical studies do not support the theoretical benefit of knee braces.In a RCT of 117 patients with unicompartmental KOA,Brouwer[107]found that benefits in using the brace was small and compliance was low due to ineffectiveness and skin irritation.In a separate 52 wk observation study of 204 patients with KOA,Yu[108]found that that neither patellofemoral or tibiofemoral customised bracing resulted in a significant difference in overall pain and functional improvements compared to the control unbraced group.Rather,a multidisciplinary program with a multidisciplinary approach was effective and sufficient for symptomatic improvements.However,limitations of this study included high dropout rate with less than 60% participating in the final assessment and potential recall bias.Survey results by Squyer[109]also indicated low compliance use of knee brace in patients which is 28% after the first year and 25% after the second year.No patient or radiographic factors were identified in the survey to predict usage or discontinuation of the knee brace.
Due to the lack of research supporting its efficacy and poor-quality evidence,the OARSI guidelines[4]now recommended against knee bracing.
FOOT ORTHOSES
Laterally-wedged insoles have also been recommended in the treatment of medial KOA because of their potential to reduce the knee adduction moment(KAM)(medial-to-lateral knee loading).Research has shown that an increased external knee adduction moment(EKAM)causes an increase in risk of structural deterioration over time of the medial knee compartment.Therefore,insoles might have the potential to minimise the rate of deterioration and help relieve symptoms.
However,several clinical studies have shown that laterally-wedged insoles might not confer any beneficial biomechanical effect and symptom relief.In a secondary analysis of data from a RCT study,Duivenvoorden[110]concluded that neither valgus brace nor laterally wedged insoles resulted in clinically relevant biomechanical alterations.Unloading of the medial compartment was only present in laterally wedged insoles at baseline and did not persist beyond six weeks.However,the unloading effect at baseline was small and might not be clinically relevant.Another randomised study assessing the relationship between KAM and knee pain in 70 patients with medial KOA by Jones[111]concluded that lateral wedges did reduce the average EKAM but changes in EKAM had no clear-cut relationship with knee pain reduction.Instead,some subjects experience paradoxical pain reduction even though EKAM increased.This finding was further supported by a three-month RCT by Lewinson[112]Their study concluded that the magnitude of KAM reduction was not associated with the same magnitude of change in pain.
The benefits of weight loss might be linked to reduce joint loading.In a secondary analysis of data from the CAROT trial,Aaboe[32]found that every kilogram lost in bodyweight resulted in 2.2 kg reduction in the peak knee joint loading.Weight loss has also been linked to inflammatory and interstitial turnover changes.Loeser[33]in a RCT of 429 patients with symptomatic KOA found that weight loss through diet decreased biomechanical markers of interstitial matrix inflammation and turnover(IL-6,C1M,C3M and CRPM).However,the limitation of this study was that the biochemical results do not show a relationship with change in physical function or radiographic progression of osteoarthritis.
Several studies have shown little difference between laterally wedged insoles and neutral insoles.In a 6 mo prospective RCT of 156 patients with symptomatic medial KOA,Pham[113]concluded that lateral wedged insoles was not superior over neutral insoles in terms of pain,stiffness and physical functioning with the exception of decrease NSAIDs consumption.Neither neutral nor lateral wedged insoles demonstrated disease-modifying effects.Bennell[114]double-blinded RCT of 200 subjects with mild to moderately severe medial KOA also similarly reported that lateral wedge insoles demonstrated no additional benefit over flat insoles in symptom improvement or disease modifying effect.
Effectiveness of insoles also depends on patient factors.Shimda[115]in a prospective study analyzing the gait of 42 patients reported that laterally wedged insoles were most effective in reducing KAM in patients with early and mild osteoarthritis.Toda[116]concluded that insoles are more effective for younger patients and those with higher lean body mass.Conversely,use of insoles are less effective for older patients with sarcopenia.
The thoughtfulness, empathy and love of this convenience store manager demonstrates vividly5 that people remember more how much an employer cares than how much the employer pays. An important lesson for the price of a Little League baseball glove.
Evidence to support use of thermotherapy has been inconclusive.An early RCT by Clarke[117]in 1974 reported that use of ice packs for three weeks did not result in statistically significant or clinically important pain relief compared to the control group.Subsequently,Hecht[118]found that ten treatment sessions of cold pack application resulted in oedema reduction while hot packs did not.However,the clinical importance of oedema reduction was unclear.Yurtkuran[119]reported that ice massage for 20 min at 5 sessions per week was clinically superior over control in increasing quadriceps strength.No difference was seen for function,joint range of motion or knee oedema.In a recent RCT,Aciksoz[120]concluded that both hot and cold applications in addition to standard treatment resulted in mild improvements for pain,function and quality of life.However,the improvement was not sufficient to be statistically superior over the control group.
THERMOTHERAPY
Thermotherapy involves superficial application of heat or cold to improve symptoms.Cryotherapy is thought to help in pain management by vasoconstriction of blood vessels and blocking of nerve impulses in the joint.This would be useful in reduction of inflammation,oedema of the joint and pain.Alternatively,heat therapy has been proposed to help by relaxing muscles and increasing blood circulation to the applied area.This would then result in pain and stiffness reduction,as well as improving mobility.
Overall,insoles and knee bracing have similar effectiveness.However,insoles do have an advantage because of higher compliance,lower cost and ease of use.Therefore,clinicians and allied health professionals should take this into consideration if they wish to recommend foot orthoses as an adjunctive treatment.
Overall,the current literature has been inconclusive with contradicting results.However,given that the thermotherapy is easily implemented and relatively safe,there is no harm in its recommendation as an adjunctive therapy.The decision on heat or cold application would heavily depend on patient’s preference as Denegar[121]in a randomised trial reported greater improvements in pain and function when patients used their preferred treatment.
But do not men sometimes act quite as cruelly towards theirown fellow-men? Was not the knight Sir Bugge murdered by wickedpeople? And though he was well spoken of, did he not also wish to kill the architect who built the castle for him, with its thick walls andtower, at the point where the Skjaerumaa falls into the bay? Jurgenand his parents now stood there; the wall and the ramparts stillremained, and red crumbling fragments lay scattered around
ORAL SUPPLEMENTS
Glucosamine and chondroitin are two of the most popular dietary supplements marketed for effective management of symptoms of osteoarthritis and improvement of joint health.
Vasilissa was so frightened to see how the old witch ground her teeth that she almost told her of the little doll; but she bethought herself just in time, and answered: The blessing of my dead mother helps me.
However,the preparation of the supplements does impact the effectiveness.In the CONCEPT trial,Reginster[125]concluded that pharmaceutical-grade chondroitin at 800 mg/day over 6 mo was superior to placebo and similar to celecoxib in pain reduction and improvement in function.Similarly,Hochberg[126]in a randomised double-blinded study reported that a combination of prescriptiongrade chondroitin and glucosamine had comparable efficacy to oral celecoxib in symptomatic relief for KOA after six months of use.However,this study does have several limitations.The study compared the supplementation against oral celecoxib which did not demonstrate superior results over placebo in the GAIT trial.Furthermore,sponsorship of this study by a pharmaceutical company could have introduced bias.
One day while shopping in a small town in southern California, it was my misfortune to be approached by a clerk whose personality clashed with mine. He seemed most unfriendly and not at all concerned about my intended purchase. I bought nothing, and marched angrily out of the store. My antagonism3, toward that clerk and the entire establishment mounted with each step.
In terms of safety profile,the above research trials show both glucosamine and chondroitin to have a good safety profile.In fact,a recent prospective cohort study across the United Kingdom reported that glucosamine supplements might even be beneficial and associated with lower cardiovascular disease risks[127].However,follow-up analysis of the osteoarthritis initiative reported that long-term data showed that chondroitin sulfate and glucosamine supplementation could be associated with higher risks of radiographic osteoarthritis and subsequent knee replacements[128].
So one Sunday the White Bear came and said that they could now set out to see her father and mother, and they journeyed thither5, she sitting on his back, and they went a long, long way, and it took a long, long time; but at last they came to a large white farmhouse6, and her brothers and sisters were running about outside it, playing, and it was so pretty that it was a pleasure to look at it
Overall,glucosamine and chondroitin have shown promise for potential of disease progression and symptomatic relief.However,efficacy would depend on the preparation of the supplements and severity of the disease.More research would also need to be done regarding the long-term safety profile of the supplements.Several meta-analysis and systematic reviews have also criticised that trials supporting large symptomatic benefits often have poor quality,publication bias and small samples while more robust methodologically sound studies have found small to no benefits.
DRY NEEDLING
Dry needling involves the use of fine needles to penetrate the skin and deactivate myofascial trigger points.The mechanism of action has been linked to activation of descending pain pathways that inhibit nociceptive processing[129].
Studies by Ceballos-Laita[130]and Itoh[131]have shown dry needling to be effective in improving function and pain intensity for osteoarthritis in the short term when compared to patients receiving control sham treatment.However,limitations of the above studies include low number of dry needling treatments and lack of long-term follow ups to examine the long-term benefits.
Moreover,the effectiveness of dry needling as part of a multidisciplinary approach remains questionable.Romero[132,133]examined the benefits of adding dry needling to a structured exercise program in KOA in two separate RCTs from a short-term and long-term perspective.However,dry needling failed to show improvements in function and pain intensity in the treatment group for both studies at the 3-mo and one-year mark respectively.The correlation between trigger points and intensity of KOA pain has also shown to be poor based on a secondary analysis by Romero[134].Overall,more studies,especially with longer term results,are required to support the effectiveness of dry needling as part of a multidisciplinary approach.
CONCLUSION
Based on the current literature available to date,a multidisciplinary and a multimodal approach with a key focus on exercise,weight loss and pharmacological pain management would be the most appropriate.Out of the multiple pharmacological options available,chronic pain management through topical NSAIDs with intermittent intra-articular injections of corticosteroids or hyaluronic acid provides a reasonable balance between benefit and risk.Topical capsaicin can also be effective in mild to moderate KOA.Acetaminophen has not been shown to be an effective analgesic.Opioids,preferably tramadol,would have to be evaluated on a case-by-case basis due to their potent side-effects which are sufficiently detrimental to negate their benefits.While the post-operative negative impact is clear,more research is needed around the optimal adjunctive peri-operative analgesia and the effect of opioid tolerance on patients undergoing surgery.
There are numerous types of effective exercise therapy available,including a well-structured physical therapy program.Alternate interventions such as thermotherapy,leg orthoses or TENS have shown conflicting results and perhaps only conditionally recommended on an individual basis.Further research is required regarding the effectiveness of chondroitin and glucosamine.
FOOTNOTES
Lim WB contributed to the literature reviewing,writing and editing of the manuscript;Al-Dadah O conceived the original idea and design of the study and extensively revising the manuscript critically for important intellectual content.All of the authors reviewed and approved the final manuscript as submitted.
The Captain stopped his mules in front of Ali Baba s house, and said to Ali Baba, who was sitting outside for coolness: I have brought some oil from a distance to sell at to-morrow s market, but it is now so late that I know not where to pass the night, unless you will do me the favor to take me in
The authors declare no conflict of interests.
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial(CC BYNC 4.0)license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See:http://creativecommons.org/Licenses/by-nc/4.0/
United Kingdom
Wei Boon Lim 0000-0002-7125-066X;Oday Al-Dadah 0000-0002-1940-836X.
Zhang H
A
Zhang H
杂志排行
World Journal of Orthopedics的其它文章
- Impact of enhanced recovery pathways on safety and efficacy of hip and knee arthroplasty:A systematic review and meta-analysis
- Surgical treatment of femoral deformities in polyostotic fibrous dysplasia and McCune-Albright syndrome:A literature review
- Plate vs reverse shoulder arthroplasty for proximal humeral fractures:The psychological health influence the choice of device?
- Diagnostic role of Xpert-MTB RIF assay in osteoarticular tuberculosis:A retrospective study
- Comparative study of intertrochanteric fracture fixation using proximal femoral nail with and without distal interlocking screws
- Ilizarov bone transport combined with the Masquelet technique for bone defects of various etiologies(preliminary results)