Learning from a rare phenomenon — spontaneous clearance of chronic hepatitis C virus post-liver transplant: A case report
2022-04-02NoreenSinghMangMaAldoMontanoLozaRahimaBhanji
Noreen Singh, Mang Ma, Aldo J Montano-Loza, Rahima A Bhanji
Noreen Singh, Mang Ma, Aldo J Montano-Loza, Rahima A Bhanji, Division of Gastroenterology and Liver Unit, University of Alberta Hospital, Edmonton T6G 2X8, Alberta, Canada
Abstract BACKGROUND Hepatitis C virus (HCV) can lead to chronic liver damage resulting in cirrhosis and hepatocellular carcinoma. Spontaneous clearance of HCV has been documented after an acute infection in 20%-45% of individuals. However,spontaneously resolved chronic hepatitis C following liver transplant (LT) is rare and has been documented only in a few case reports. The phenomenon of spontaneous clearance of chronic hepatitis C occurs together with other meaningful events, which are typically associated with significant changes in the host immunity.CASE SUMMARY We report three cases of spontaneous resolution of chronic hepatitis C following liver transplantation. These patients either failed or had no HCV treatment prior to transplant, but had spontaneous resolution of HCV post-LT as documented by undetectable polymerase chain reaction (PCR). Diagnosis of HCV was based on viremia through PCR or liver biopsy. All three patients currently undergo surveillance and have no recurrence of HCV.CONCLUSION Examining each patient’s clinical course, we learned about many viral, host and cellular-factors that may have enhanced the host’s immunity leading to spontaneous clearance of HCV. Though HCV treatment has excellent cure rates,understanding this mechanism may provide clinicians with insights regarding timing and duration of treatment.
Key Words: Spontaneous resolution of hepatitis C; Liver transplantation; Hepatitis C;Immunosuppression; Viral load; Case report
INTRODUCTION
Chronic infection with hepatitis C virus (HCV) leads to progression of liver disease, cirrhosis, hepatocellular carcinoma, and is a common indication for liver transplant (LT). Whereas spontaneous clearance of acute HCV occurs in 20%-45% of individuals[1], spontaneous resolution of chronic HCV has been documented only in case reports. The latter is rare as HCV has already successfully managed to evade immune control for a prolonged period. Spontaneous clearance of HCV following LT is unusual due to ongoing immunosuppression use. Indeed, studies have shown HCV recurrence following LT to be universal and associated with poor graft and patient survival[2]. Immunosuppression use is associated with accelerated disease with up to a third of patients developing cirrhosis at 5 years[2].
It has been hypothesized that viral, host and cellular-factors change the host’s immunity by enhancing it whereby leading to spontaneous clearance of HCV. These protective factors include HLA alleles[3], co-infection with hepatitis B[4], infection with other viruses[4], immunosuppressive therapy withdrawal[5], immune reconstitution after highly active antiretroviral therapy (HAART)[6,7],pregnancy[8] and surgery including LT and gastrectomy[9]. The mechanism by which all these factors lead to spontaneous resolution of HCV is not completely understood but likely involves alteration of the host immune response. We report three cases of patients on immunosuppression who have had spontaneous HCV clearance post-LT.
CASE PRESENTATION
Chief complaints
The chief complaints of ALL the presented case reports are HCV viremia following LT.
History of present illness
Case 1:A 57-year old Caucasian male who had been HCV positive (genotype 1a) for 9 years. Clinic notes showed that HCV viremia was diagnosed based on polymerase chain reaction (PCR). He was treated with ribavirin and pegylated interferon but did not achieve sustained virologic response (SVR).This treatment led to significant side effects including decompensation. He required an urgent LT in 2006. Unfortunately, pre-transplant HCV viral load was not available.
Case 2:Another case was a 63-year-old Caucasian male diagnosed with HCV positive (genotype 1) in 2004. He was treated for HCV but did not achieve SVR (HCV viral load 311 IU/mL in 2014).
Case 3:Our third case was a 57-year-old male with HCV (genotype 1a) as a result of a blood transfusion in 1994.
History of past illness
Case 1:He had a past medical history of schizophrenia, dyslipidemia, and diabetes.
Case 2:His past medical history included osteoarthritis and hepatocellular carcinoma diagnosed in December 2012. He had transarterial chemoembolization as well as selective internal radioembolization(SIRT) in April 2013. Unfortunately, he developed decompensated liver cirrhosis and required LT in July 2015.
Case 3:His past medical history included a kidney transplant in 2001 for IgA nephropathy that failed in 2007. He also had HCV liver cirrhosis, requiring LT in 2012. Due to his kidney transplant, his medications included mycophenolate mofetil 750 mg twice daily, tacrolimus 0.5 mg twice daily,pantoprazole 40 mg daily and amlodipine 5 mg daily.
Personal and family history
They have no special personal and family history.
Further diagnostic work-up (including relevant labs)
Case 1:Post-LT immunosuppression included prednisone, sirolimus, and mycophenolate mofetil.Immediately after LT, he had a mild episode of cellular rejection that was treated with oral prednisone.One-year post-LT, he had a second episode of mild cellular rejection with liver biopsy showing a superimposed recurrent HCV (Metavir A1, F2). HCV viral load was positive in 2007 (unknown viral load). A liver biopsy was done in February 2007 showing mild acute cellular rejection with superimposed recurrent Hepatitis C (Metavir Grade 3, Fibrotic Stage 2).
Case 2:He had HCV viral load of less than 12 IU/mL following LT, consistent with untreated HCV.Post-LT immunosuppression included tacrolimus and mycophenolate mofetil. The donor’s liver was hepatitis B core antibody-positive and the patient was started on Entecavir. His post-transplant course was remarkable for cytomegalovirus (CMV) viremia in 2016 with a peak of 1376 IU/mL, which cleared without antiviral therapy; subsequent CMV viral load testing was negative.
Case 3:He was never treated for HCV; liver biopsy done in 2007 showing stage 4 fibrosis and he had a positive HCV viral load in 2008 (viral load unknown). Unfortunately, HCV viral load was not available pre-transplant. His post-transplant course was complicated by biliary anastomotic strictures requiring ERCP stent placement.
FINAL DIAGNOSIS
Cases 1-3
Recurrent HCV following liver transplant.
TREATMENT
Case 1
Unfortunately, at the time, he was not considered for re-treatment due to the potential for adverse psychiatric side-effects of using Interferon-regimens especially in the setting of paranoid schizophrenia.In June 2007, he developed CMV viremia from which he recovered. A repeat liver biopsy was done in January 2009 showing chronic hepatitis, consistent with recurrent Hepatitis C (Metavir Grade A1, Stage F1).
Case 2
No treatment for HCV was provided.
Case 3
No HCV treatment was provided following LT.
OUTCOME AND FOLLOW-UP
Case 1
Despite no additional treatment for his recurrent hepatitis C, repeat HCV PCR in 2013, 2015, 2016 and 2017 all showed undetectable viral load consistent with spontaneous clearance of HCV. Presently, he undergoes surveillance for cirrhosis and has normal serum liver tests.
Case 2
Subsequent HCV viral load testing in October 2015 and January 2016 were negative thereby suggesting spontaneous resolution of HCV following liver transplant. Presently, he has normal serum liver test and is on tacrolimus for immunosuppression.
Case 3
Repeat testing for HCV viral load in 2013, 2014, and 2015 were negative, consistent with spontaneous clearance following LT. Presently, he has normal serum liver tests while being on tacrolimus and mycophenolate mofetil.
DISCUSSION
Spontaneous clearance of chronic HCV following LT is a rare phenomenon that is poorly understood.Only a small number of cases exist, which makes it difficult to understand host and viral factors influencing chronicity or to identify predictors of spontaneous clearance. Nevertheless, certain viral and host factors seem to be associated with clearance. Scottet al[10] completed a prospective study in Alaskan natives and found the rate of spontaneous HCV clearance among patients with chronic disease to be 1.15 cases per 100 persons per year. A low viral load and young age at onset of disease were associated with spontaneous clearance.
We performed a retrospective review of patients who underwent a liver transplant at the University of Alberta Hospital, Edmonton, Canada from 2000 to 2015 to identify cases of spontaneous HCV clearance. Among the 191 patients transplanted for HCV, we only found the three cases described above(1.5%). We also performed a literature review to identify additional cases of spontaneous HCV resolution post-LT to better understand factors associated with this phenomenon. We used a similar strategy as Tamakiet al[11], but did not exclude patients on HAART, interferon or ribavirin. We completed a systematic review using PubMed from August 2015 to January 2020 by including keywords of LT and spontaneous clearance of HCV. No additional case reports were found. We have presented all the case reports since 2000 (Table 1) and reviewed the literature to consolidate the protective factors that may be associated with spontaneous clearance of HCV.
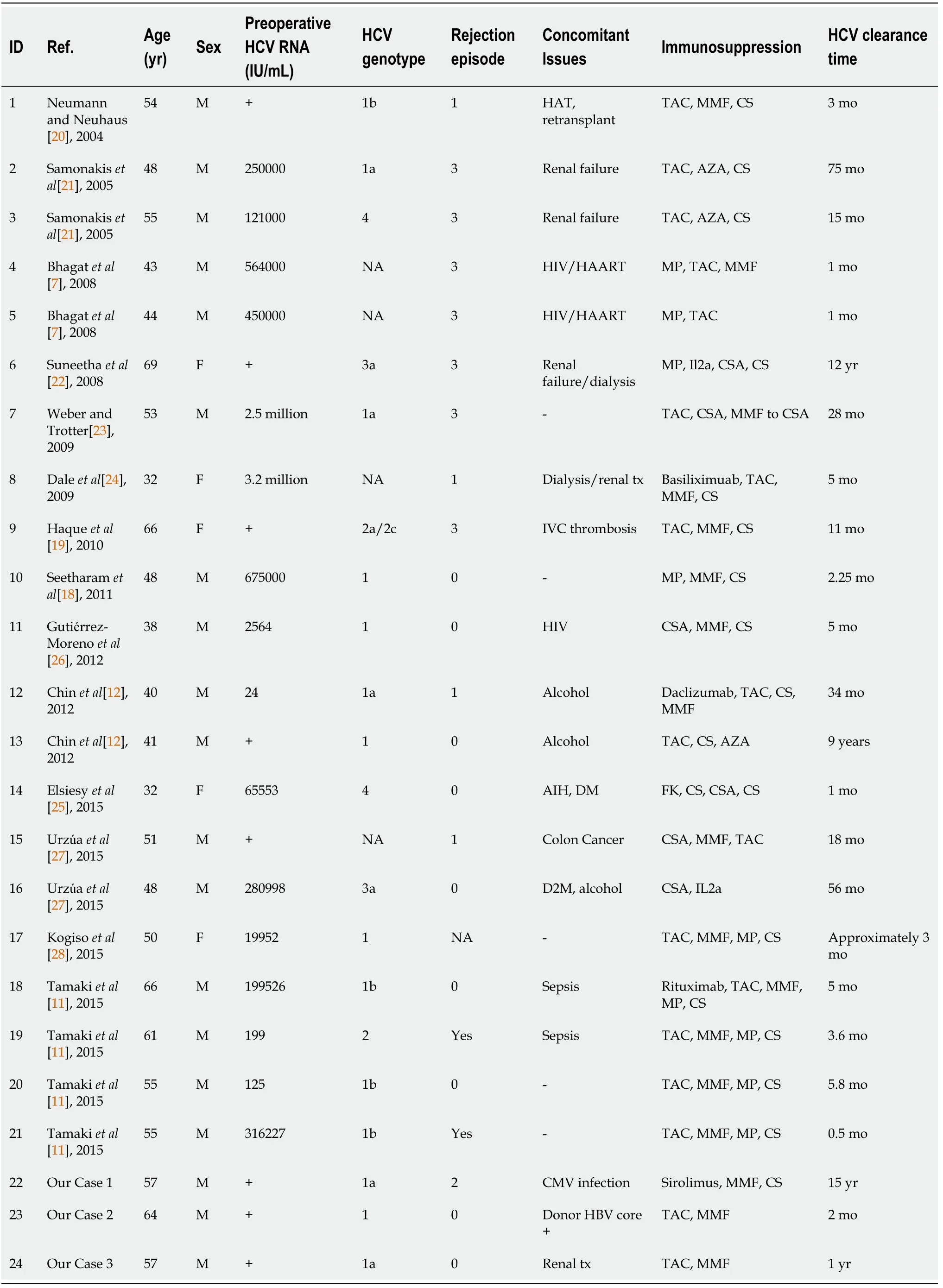
Table 1 Summary of cases of spontaneous hepatitis C clearance post-liver transplant
Host factors
Female sex and younger age have been associated with spontaneous clearance[10] (Table 2). Younger age may be protective due to lower likelihood of advanced fibrosis. It may also mean a more robust immune system. Though it is unclear what benefit these factors have in the post-LT setting. The mean age of cases included was 49 years (SD 9.95 years) and the majority were men (75%). The beneficial effect of female sex may be related to gender-based differences in immunity. For instance,polymorphisms of interleukin-28B gene (IL28B), specifically IL28B-CC genotype associated with spontaneous clearance of chronic HCV have a much greater effect in females. These polymorphisms are also associated with response to treatment with pegylated interferon (PEG-IFN), simeprevir, sofosbuvir,and ribavirin[12]. Interestingly, two of the patients with spontaneous resolution of HCV had donors with IL28B-CC genotype; it was felt this altered host immune response to HCV and led to spontaneous clearance[12]. Host HLA class II genotype plays an important role in host susceptibility. In a recent meta-analysis by Gauthiezet al[3], HLA alleles DQB1*03, DQB1*03:01, DQB1*11 and DRB1*11:01 were thought to be protective due to effective presentation of HCV epitopes to CD4+ T lymphocytes. On the other hand, HLA allele DQB1*02 was associated with failure to spontaneously clear HCV[3].

Table 2 Factors associated with spontaneous hepatitis C virus clearance
Host immune response:HCV infection causes an immediate induction of interferons and cytokins[13].The outcome of HCV infection is determined by the quality of the adaptive and humoral immune response[14]. Firstly, innate immunity consists of activation of T-cells by natural killer (NK) cells leading to interferon-gamma production and cytotoxic killing of hepatocytes that are infected[13]. Chronic HCV leads to a decline in NK cells thereby promoting persistent infection of hepatocytes[13]. Secondly, the humoral immunity consists of a T-cell response that develops between 5 wk to 12 wk after infection[13].Studies in humans and chimpanzees suggest that control of HCV viremia is observed after emergence of a robust CD4+T-cell proliferation[13-15]. Indeed, in cases where anti-CD4+antibody treatment was used HCV immune evasion was seen with persistent infection[14]. Additionally, CD8+T-cells are thought to be important in controlling viremia but require simultaneous CD4+T-cells to maintain response.Therefore, HCV persistence is hypothesized to be caused by CD4+exhaustion followed by CD8+phenotypic exhaustion. A study by Smyk-Pearsonet al[14] found that there is a quantitative T-cell threshold that exists by which spontaneous HCV occurs. Hence, a robust T-cell activation is needed for a spontaneous HCV clearance.
Other factors
The spontaneous clearance of HCV post-LT is unique as patients are on immunosuppression. Segevet al[16] performed a meta-analysis and meta-regression comparing steroid-free and steroid-based immunosuppression and found corticosteroids increased the ability of HCV to enter cells and led to a dramatic increase in spread of infection. Lower rates of HCV recurrence were seen when using steroidfree regimes, which was also corroborated by Fafi-Kremeret al[17]. Of note, half (15/30) of the cases with spontaneous HCV clearance had experienced rejection following transplant. This observation is in contrast to the findings of Segevet al[16] as corticosteroids are used for the management of rejection.One theory may be that rejection leads to stimulation of the immune system, which alters the host’s immune response to HCV eventually leading to spontaneous clearance.
It has been postulated that activation of Th2 cytokines may predominate in high stress situations including pregnancy, and post-gastrectomy[8,9]. Undergoing a liver transplant, also a high stress situation may lead to spontaneous clearance by restoration of the HCV-specific T-cell response.Similarly, infection of the allograft might engage the host’s immune system and lead to activation of Th-17 cells that contribute to clearance[18]. The patient in Case 1 likely had resolution as he had both episodes of rejection and CMV reactivation, which may have led to a boost in the immune system. A third of the patients (9/30) who had spontaneous resolution experienced concomitant infections (coinfection with hepatitis B or human immunodeficiency virus; CMV or sepsis) following LT.Interestingly, almost half of the patients (13/28) who had spontaneous HCV clearance had a negative HCV PCR documented within 6-months of LT.
Viral factors
A low viral load has been shown to be associated with spontaneous clearance of HCV[10]. In the cases presented, half of the patients (14/30) had low viral load defined as < 1 million IU/mL (mean ± SD,451088 ± 224854 IU/mL).
CONCLUSION
In conclusion, spontaneous resolution of chronic HCV following LT is a rare phenomenon and seems to be related to immunomodulatory effects. Though the small number of cases prevents identification of predictors of clearance some factors have emerged. Some may argue the impact of these findings is low as patients can be treated with direct-acting antivirals (DAAs). Nevertheless, these findings are beneficial in settings where there is no access to DAAs due to cost.
These findings may also help clinicians with management. Determining the presence of IL28B polymorphisms may help determine response to treatment (or presence of resistance). The viral load could be used to determine the duration of treatment with a shorter duration in those with low viral load. The median time to spontaneous HCV clearance was 11 mo (IQR 3.6, 66 mo) with almost half of the patients achieving spontaneous clearance within 6 mo (13/30). Treatment could therefore be started after 6 mo. This would provide an additional advantage of limiting drug-drug interactions early in the post-transplant setting. In patients without evidence of fibrosing cholestatic hepatitis, episodes of rejection or concomitant infections may warrant further delay in treatment; these episodes may lead to immune modulation facilitating spontaneous clearance. The number of cases of spontaneous resolution may be underestimated as we do not always get repeat HCV PCR prior to treatment. Learning from this rare event may be the first step to individualized medicine. Further studies to elucidate the mechanisms of spontaneous HCV clearance are warranted to explore new potential therapeutic strategies in this special population.
FOOTNOTES
Author contributions:All authors contributed to the writing of the manuscript, critical revision and approval of the final manuscript.
Informed consent statement:Informed written consent was obtained from the patients for publication of this report.
Conflict-of-interest statement:The authors declare that they have no conflict of interest.
CARE Checklist (2016) statement:The authors have read the CARE checklist (2016), and the manuscript was prepared and revised according to the CARE checklist (2016).
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Canada
ORCID number:Noreen Singh 0000-0002-0978-9146; Mang Ma 0000-0003-2587-1788; Aldo J Montano‐Loza 0000-0002-2511-7980; Rahima A Bhanji 0000-0001-9088-8848.
S-Editor:Gao CC
L-Editor:A
P-Editor:Gao CC
杂志排行
World Journal of Hepatology的其它文章
- COVID-19 and liver disease: Are we missing something?
- Glycogen hepatopathy in type-1 diabetes mellitus: A case report
- Step-up approach in emphysematous hepatitis: A case report
- Timing of surgical repair of bile duct injuries after laparoscopic cholecystectomy: A systematic review
- β-arrestin-2 predicts the clinical response to β-blockers in cirrhotic portal hypertension patients: A prospective study
- Modified EASL-CLIF criteria that is easier to use and perform better to prognosticate acute-on-chronic liver failure
