Healthcare use among people with diabetes mellitus in Europe: a population- based cross- sectional study
2022-03-04lvaroFuentesMerlosJosAntonioQuesadaRicoRaulReinaDomingoOrozcoBeltr
Álvaro Fuentes- Merlos , José Antonio Quesada- Rico , Raul Reina , Domingo Orozco- Beltrán
ABSTRACT
INTRODUCTION
Factors contributing to the increasing incidence of diabetes include sedentary lifestyle, obesity and population ageing.1In this regard, the disease has been associated with a poorer quality of life, physical inactivity,obesity and other comorbidities, as well as to non- modifiable factors such as advanced age and male sex.2
Diabetic mellitus (DM) is a chronic disease that constitutes a considerable public health problem, negatively impacting on patients’quality of life and influencing healthcare policy.23The worldwide prevalence of diabetes and impaired glucose tolerance in adults has increased in the past few decades.245According to recent estimates by the International Diabetes Federation, in 2019, there were 463 million people living with diabetes worldwide (9.3% of adults aged between 18 years and 99 years), and this figure is set to reach 578 million (10.2%) by 2030 and 700 million (10.9%) by 2045.5Moreover, half of people with diabetes (50.1%) are undiagnosed.5This high prevalence has important social, financial and developmental repercussions, particularly in low- income and middle- income countries.6Diabetes is among the 10 leading causes of death in adults, and was responsible for an estimated 4.2 million deaths worldwide in 2019.5As a result, the impact of diabetes on healthcare systems and national economies is of increasing concern. In 2019,the global healthcare expenditure linked to diabetes was US$760 billion, and this sum is projected to reach 825 billion by 2030 and 845 billion by 2045.5
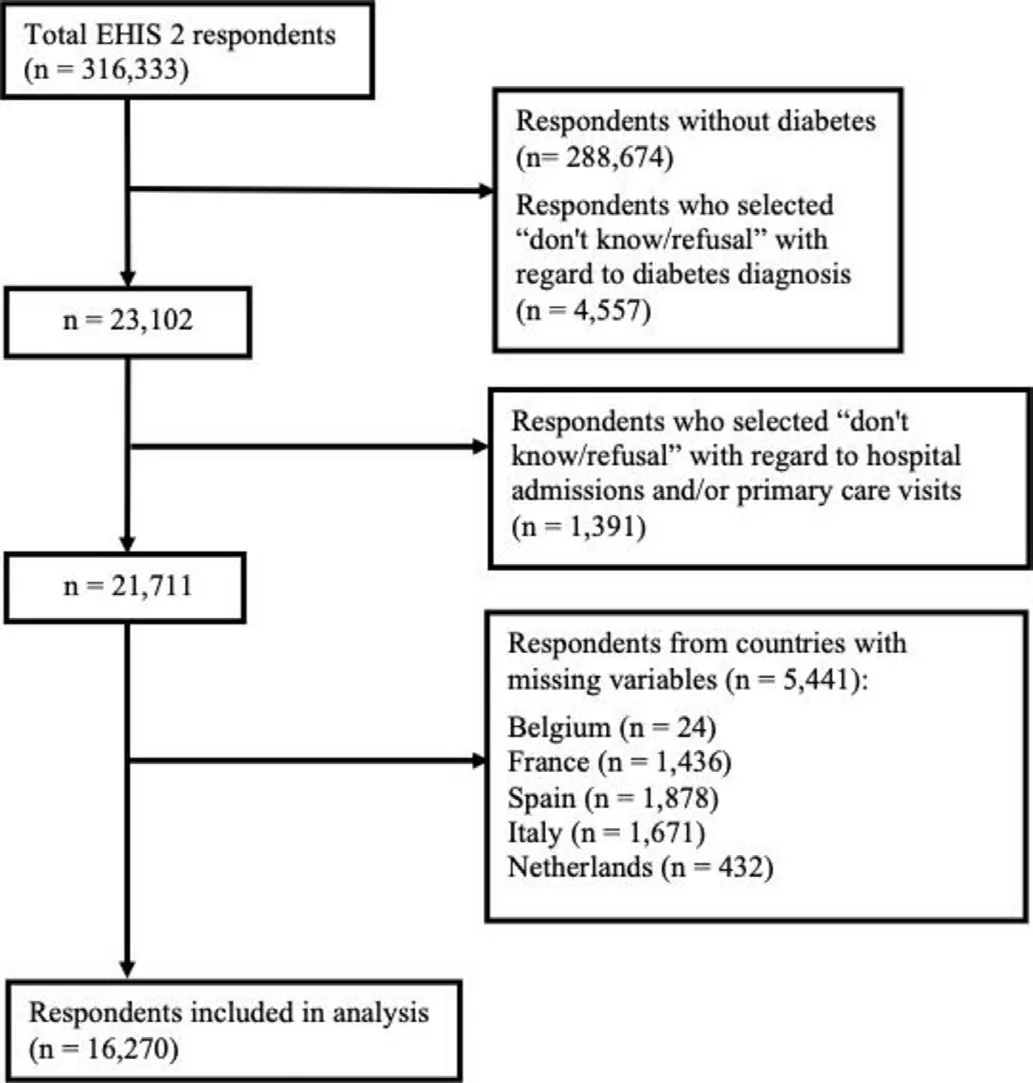
Figure 1 Inclusion of patients in the analysis. EHIS,European Health Interview Survey.
The main social repercussions of diabetes are related to use of healthcare and social resources, as the medical costs of diabetes patients are three times that of people without the disease.7–9In addition, the increase in prevalence, combined with the increase in medical cost per capita, suggests that the burden of diabetes on health systems will continue to increase.10This disease represents a public health challenge as it requires more efficient social and healthcare strategies. This justifies analysis of healthcare use among patients with diabetes, with a view to guiding health policies and ensuring appropriate allocation of healthcare resources.9
The costs traditionally associated with diabetes include medical visits, emergency care, hospitalisation and medicines,11and various studies have shown that the presence of complications and hospital admission are the main cost factors.912–14Indeed, costs associated with hospitalisation account for more than two- thirds of the total costs attributable to diabetes.814–16People with diabetes are at increased risk of hospitalisation because of macrovascular complications (eg, coronary artery, cerebrovascular and peripheral vascular disease) and microvascular complications (eg, retinopathy, nephropathy and neuropathy).1718Within this population, type 2 DM accounts for 90% of all cases of DM19and is usually managed in primary care settings, saving many of these costs. For example, a larger UK- enhanced primary care- based DM cost comparison analysis confirms significant cost savings, likely driven by economies of scale.20Hence, these benefits could be multiplied if services are implemented at a nationwide level.
Although the universal healthcare model predominates in Europe, people with diabetes show different patterns of healthcare use, depending on their level of education or economic status.2122Low socioeconomic status has been associated with a higher incidence of diabetes,7poorer healthcare, worse management of complications and greater use of healthcare services.21–23To achieve greater health equity, it is crucial to measure and interpret the socioeconomic inequalities related to health and healthcare.81622To date, however, there is a lack of published research on healthcare use in people with diabetes,24and most studies do not take into account healthcare use indirectly attributable to the disease (eg, for mental health comorbidities in the diabetic population).25
To harmonise health data and obtain common indicators, the European Union (EU) statistical office(Eurostat) decided to implement the European Health Interview Survey (EHIS). Thus far, no published studies have used EHIS data to analyse indicators of health and healthcare use in people with diabetes. This study aims to determine how health determinants, lifestyle and socioeconomic variables relate to healthcare use (primary care visits and hospital admissions) in people with diabetes in Europe.
METHODS
Sample
We performed a population- based cross- sectional study(ie, secondary analysis) to identify determinants of health, lifestyle and socioeconomic variables associated with healthcare use in people with diabetes in Europe.The data used for this purpose were obtained from the results of EHIS wave 2, provided by Eurostat.26The main goal of this health questionnaire, administered through a computer- assisted personal interview, is to obtain harmonised data on EU citizens’ health status, lifestyles and other health determinants, and on the use they make of healthcare services. In accordance with Commission Regulation (EU) No 141/2013, the survey was carried out in the following countries: Belgium and the UK in 2013;Bulgaria, Czech Republic, Estonia, Greece, Spain, France,Croatia, Italy, Cyprus, Latvia, Lithuania, Luxembourg,Hungary, Malta, Netherlands, Austria, Poland, Portugal,Romania, Slovenia, Slovakia, Finland and Sweden in 2014; and Denmark, Germany, Ireland, Italy, Iceland and Norway in 2015.27
Eligible survey respondents were non- institutionalised adults (aged 15 years or older) living in private households. The inclusion criteria for our study were being diabetic and having answered either yes or no (as opposed to ‘don’t know/refusal’) to the questions regarding primary care visits in the past month and hospital admissions in the past year. In Belgium, France, Spain, Italy and the Netherlands, some of the variables required to meet the objective of this study were missing from the administered questionnaire; as a result, all participants residing in these countries were excluded from our population.
Study variables
The independent variables included in this study are shown in online supplemental table S1, grouped into sociodemographic variables, health determinants and healthcare use. The two dependent variables were primary care visits in the past month (yes/no) and hospital admissions in the past year (yes/no).
Statistical analysis
We performed a descriptive analysis by calculating the frequencies of all qualitative variables and the minimum,maximum, mean and SD of all quantitative variables. The factors associated with primary care visits and hospital admissions were analysed using contingency tables,applying the χ2test for the categorical variables and the Student t- test for the quantitative variables. To estimate magnitudes of association, we fitted Poisson multivariate models with robust variance.28The possible overdispersion of the models was evaluated. Prevalence ratios(PRs) were calculated with the corresponding 95% CIs.We applied a stepwise variable selection process based on the Akaike information criterion, taking into account the possible multicollinearity of the variables. Goodnessof- fit indicators and the area under the receiver operating characteristic curve were also calculated. As this analysis included two dependent variables, we set the level of significance at 0.025, according to the Bonferroni method, to avoid problems related to multiplicity.
To obtain representative estimates of the European population, we took into account the complexity of the sample using as a weighting factor the raising factor of the survey divided by its mean in each country, obtaining weights centred on the means.29The statistical analyses were performed using SPSS V.26 and R V.4.0.2 (R Core Team; R Foundation for Statistical Computing, Vienna,Austria).
Ethical and data access-related issues
The legal framework for developing the EHIS is Regulation (EC) No 1338/2008 of the European Parliament and of the Council of 16 December 2008 on Community statistics on public health and health and safety at work.26This framework regulation specifies in its annexes the use of population surveys such as the EHIS to collect every 5- year statistics on health status, access and use of healthcare and health determinants. All the permissions for accessing EHIS data were managed by the Office for Responsible Research of the Miguel Hernández University of Elche.
RESULTS
The total number of respondents to EHIS 2 was 316 333.After applying the inclusion and exclusion criteria, we were left with 16 270 eligible respondents (figure 1). In this sample, which represents the adult diabetic population of 25 countries, 50.9% of respondents were women;55.5% were aged over 65 years; 11.1% had a university education; 59.3% were retired; 37.7% were overweight;36.4% had obesity; 75.9% did no recreational physical activity; and 13.6% were smokers. Regarding health status, 28.1% reported bad or very bad self- perceived health; 94.3% had a long- standing health problem;62.1% had high blood pressure; 38.7% had chronic back pain; 26.2% had chronic neck pain; 24.1% and 23.6% had a moderate or severe difficulty walking,respectively; and 24.1% and 14.7% had moderate or severe bodily pain in the past month, respectively. In total, 58.2% of respondents had seen their primary care physician in the past month, and 22.6% had been admitted to the hospital in the past year (online supplemental table S1).
The data reveal considerable variability between European countries with regard to healthcare use (figure 2).The factors associated with primary care visits and hospital admissions in the bivariate analysis are displayed in online supplemental tables S2 and S3.
The factors in the Poisson multivariate model that were significantly associated with primary care visits in the past month were being retired versus working, with a PR of 1.13 (95% CI 1.07 to 1.19); consumption of alcohol 2–3 days a month vs every day (PR 1.16, 95% CI 1.08 to 1.24); self- perceived health, with PRs increasing with worsening health, up to 1.80 (95% CI 1.51 to 2.15)for very bad vs very good self- perceived health; having a long- standing health problem (PR 1.14, 95% CI 1.04 to 1.24); high blood pressure (PR 1.06, 95% CI 1.03 to 1.10); and chronic back pain (PR 1.07, 95% CI 1.04 to 1.11) (table 1). We also found that non- response to the questions on alcohol consumption and self- perceived health had similar PRs to the worst health situation of these variables.
The factors in the Poisson multivariate model that were significantly associated with hospital admission in the past year were alcohol consumption 2–3 days a month vs every day (PR 1.18, 95% CI 1.02 to 1.36); selfperceived health, with PRs increasing with worsening health, up to 3.03 (95% CI 2.14 to 4.31) for very bad vs very good self- perceived health; having had an accident at home in the past year (PR 1.54, 95% CI 1.40 to 1.69); chronic obstructive pulmonary disease (COPD)(PR 1.34, 95% CI 1.22 to 1.47); high blood pressure (PR 1.08, 95% CI 1.01 to 1.17); chronic back pain (PR 0.91,95% CI 0.84 to 0.98); moderate difficulty walking (PR 1.33, 95% CI 1.21 to 1.45); and severe difficulty walking(PR 1.67, 95% CI 1.51 to 1.85) (table 2). Non- response to the questions on self- perceived health, accidents at home and difficulty walking had similar PRs to the worst health situation of these variables. Non- response to the question on high blood pressure showed a higher PR than having high blood pressure (PR 1.62, 95% CI 1.13 to 2.32).
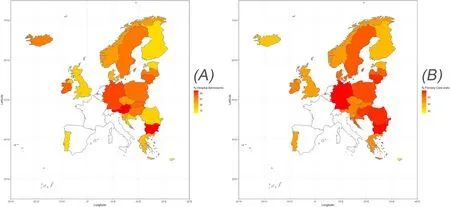
Figure 2 Proportion by country of primary care visits in the past month and hospital admissions in the past year.
DISCUSSION
This study, based on a large and representative sample of the European population, shows high healthcare use among people with diabetes in Europe, with 58.2%consulting their primary care physician in the past month and 22.6% being admitted to the hospital in the past year. The factors associated with primary care visits were labour status, alcohol consumption, self- perceived health,long- standing health problems, high blood pressure and chronic back pain. The factors associated with hospital admission were alcohol consumption, self- perceived health, having an accident at home in the past year,COPD, high blood pressure, chronic back pain and difficulty walking.
These findings are in line with other studies, which have shown that healthcare use and cost in people with diabetes are two to three times greater than in people without diabetes.9103031In our sample, 72% of patients who had seen their primary care physician in the past month had also been admitted to the hospital in the past year, and, inversely, 28% of those who had been admitted to the hospital in the past year had visited their primary care physician in the past month. The high proportion of healthcare use among people with diabetes is reflected in high costs for European healthcare systems. In this regard, one previous study showed that 70% of healthcare costs associated with diabetes resulted from hospital admissions.9Another study performed in the USA estimated the total cost of diabetes at US$327 billion, of which US$237 billion (73%) represented healthcare costs directly attributable to diabetes, and US$90 billion (27%)represented loss of productivity due to absenteeism, loss of productivity at work and at home, unemployment due to chronic disability and premature death.30
Regarding factors associated with primary care visits,our findings show greater healthcare use in retired versus working people. The relationship of socioeconomic status and older age with use of healthcare services among people with diabetes has been well defined in other studies.13–519In addition, ageing is known to influence the risk of developing type 2 diabetes, which accounts for 90% of diabetes cases worldwide.6
In contrast, we found an inverse relationship between alcohol consumption and healthcare use. Lower diabetes risk has been associated with varying levels of alcohol consumption in previous studies, possibly owing to differences between the different study populations in terms of age, race and geography, as well as differences in follow- up time and/or adjustment variables.32
In our sample, respondents who had visited their primary care physician in the past month were more likely to have very poor self- perceived health, a longstanding health problem, high blood pressure and chronic back pain. In this regard, a previous longitudinal study showed that self- perceived health is a subjective measure that can predict healthcare use.33Other studies have found that poor self- reported health is related to higher rates of mortality, hospitalisation and use of outpatient services.34
Regarding comorbidities, previous publications have associated physical inactivity, obesity, high blood pressure and chronic back pain with healthcare use in the diabetic population.335–38Our results are consistent with those of other authors,2–4in that they show a greater tendency to inactivity (75.9%) and a high prevalence of overweight(37.7%) and obesity (36.4%), all of which are frequently associated with high blood pressure and chronic back pain.3738

TabIe 1 PRs of primary care visits in the past month, estimated through Poisson multivariate models
As regards factors associated with hospital admission in the past year, we found an inverse relationship between alcohol consumption and healthcare use, with the most frequent users in the group who drank two to three drinks a month. Other associated factors are having very poor self- perceived health and comorbidities such as COPD and high blood pressure. Hospital admissions in the diabetic population were also linked to greater risk of accidents at home in the past year and moderate or severe difficulty walking. In our study population, 28.7% and 26.8% of participants were aged over 64 years and over 74 years, respectively. Our findings therefore confirm the relationship between ageing and physiological and functional decline that can increase disability, fragility and risk of falls.39In contrast, the prevalence of chronic back pain was relatively low in people who had been admitted tothe hospital in the past year, which may be attributable to the medical supervision received and control of their analgesic regimen during the hospital stay.40
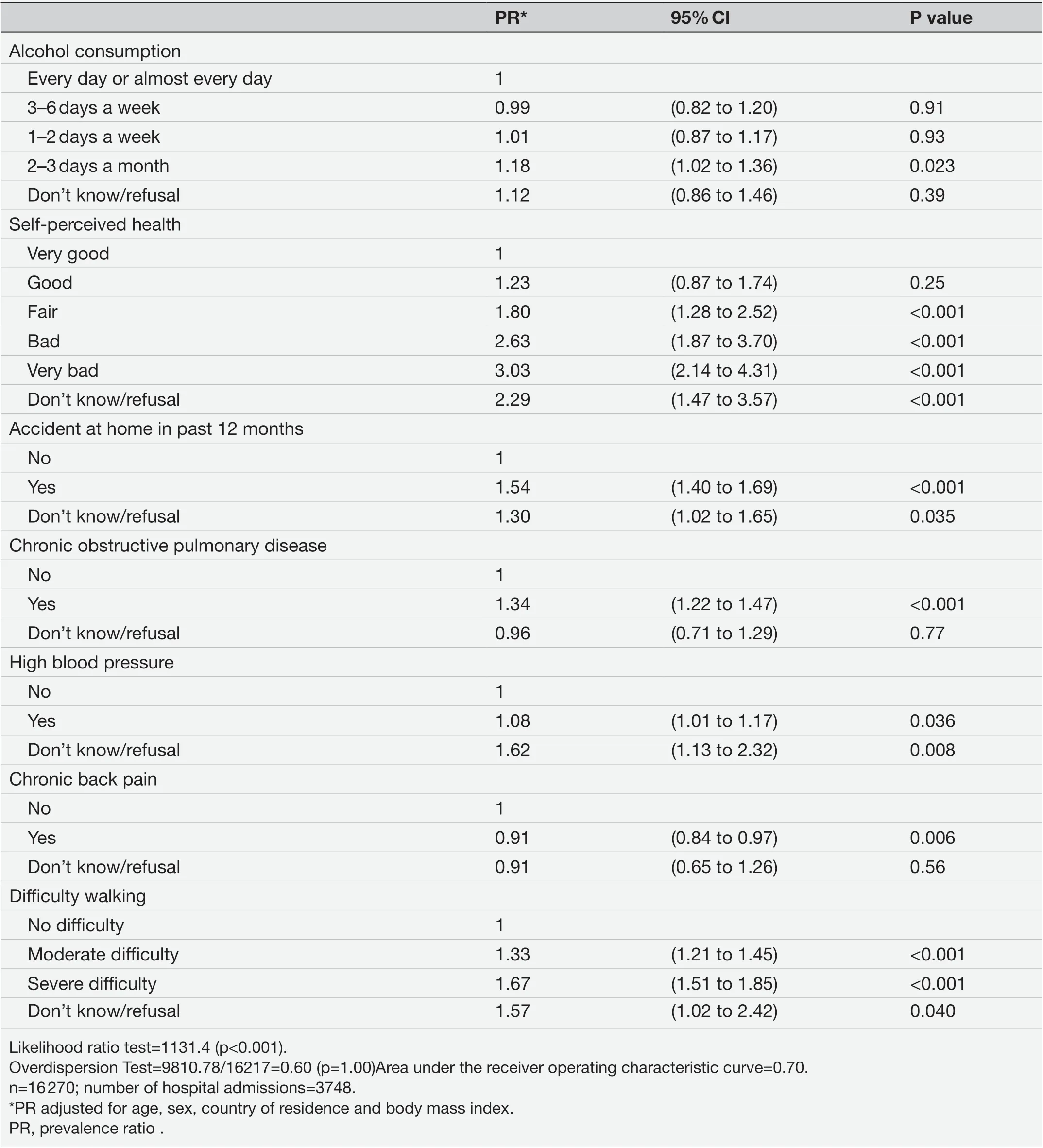
TabIe 2 PRs of hospital admissions in the past year, estimated through Poisson multivariate models
The main driver of diabetes costs is the treatment of associated complications. Our results suggest that lifestyledirected interventions (eg, educational self- management workshops or promotion of physical activity and weight loss) focused on specific sectors of the population (eg,people who are retired or who have comorbidities) could be associated with an improvement in the quality of life of people with diabetes and encourage a more efficient use of health services in Europe. In view of the ageing populations and increasing socioeconomic and demographic diversity in multinational and multicultural regions like Europe, effective prevention of diabetes requires multidimensional public health programmes that incorporate patients’ perspectives (ie, physical, emotional and social functioning), lifestyles and socioeconomic status(education, income and healthcare costs). This innovative approach—based on improving life expectancy and socioeconomic indicators by taking into account the experience of an increasingly demanding population—should focus on promoting healthy lifestyles and providing chronic disease self- management education,with the aim of reducing hospital admissions and thus reducing diabetes- related healthcare costs. In this regard,the holistic and preventive approach to primary care presents itself as the best setting to assess the nature of this impact. Future studies could assess the impact of this approach on diabetes care, which represents a considerable financial burden on healthcare systems.
This study has some limitations. First, owing to the crosssectional design, we were unable to evaluate longitudinal trends or causal relationships. Second, all the data examined in our study were collected through self- reporting,and could therefore be affected by recall bias and social desirability bias, although the EHIS was designed and validated to minimise the effects of non- response and selfreporting biases.41Third, diabetes itself is a cause of poor self- perceived health, and many of the poorest health indicators in our population could be due to the disease and not risk factors for the disease. Nonetheless, the results of our study could help to better understand the possible consequences of diabetes on health and healthcare use in a large sample of European citizens. Fourth, the questionnaire excludes gestational diabetes and does not distinguish between type 1 and type 2 diabetes. However,given the large sample size and the high prevalence of type 2 diabetes in Europe,56we can assume that the great majority of respondents in our study had type 2 diabetes.Fifth, statistical tests tend to give significant results when sample sizes are large; for this reason, we tried to evaluate clinical as well as statistical significance, taking effect size into account. Sixth, as more than half of people with diabetes are undiagnosed,5under- reporting could be an issue in our study. We assumed, however, that self- reported diabetes in the EHIS 2 was based on a previous clinical diagnosis. Seventh, the data were collected between 2013 and 2015 in the participating countries, so this fact must be considered as an additional limitation since they do not represent the same time frame. Finally, five countries(Spain, Belgium, France, Italy and the Netherlands) did not provide information on certain variables analysed in this study. Since these variables were included in the multivariate logistic model, the resulting estimates are not representative of those countries.
CONCLUSIONS
This study found that half of the people with diabetes in Europe had visited their primary care physician in the past month, and one in four had been admitted to the hospital in the past year, though these percentages varied considerably between the 25 European countries included in the study. The factors associated with primary care visits were labour status, alcohol consumption, selfperceived health, long- standing health problems, high blood pressure and chronic back pain. On the other hand, the factors associated with hospital admission were alcohol consumption, self- perceived health, having an accident at home in the past year, COPD, high blood pressure, chronic back pain and difficulties in walking.
ContributorsJAQR analysed the data. ÁF- M drafted the manuscript. DOB, RR,JAQR and ÁF- M devised the study concept and design. All authors took part in the interpretation of the results, commented on the manuscript and had final responsibility for the decision to submit for publication. All authors have read and agreed to the published version of the manuscript. ÁF- M acts as guarantor for this study.
FundingThe authors have not declared a specific grant for this research from any funding agency in the public, commercial or not- for- profit sectors.
Map disclaimerThe depiction of boundaries on this map does not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction or area or of its authorities. This map is provided without any warranty of any kind, either express or implied.
Competing interestsNone declared.
Patient consent for publicationNot applicable.
Ethics approvalNot applicable.
Provenance and peer reviewNot commissioned; externally peer reviewed.
Data availability statementData sharing not applicable as no datasets generated and/or analysed for this study. No data are available.
Supplemental materialThis content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer- reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines,terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Open accessThis is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY- NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non- commercially,and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non- commercial. See: http://creativecommons.org/licenses/by-nc/4.0/.
ORCID iDsÁlvaro Fuentes- Merlos http://orcid.org/0000-0002-1024-1620 José Antonio Quesada- Rico http://orcid.org/0000-0002-6947-7531 Raul Reina http://orcid.org/0000-0003-0279-7802
杂志排行
Family Medicine and Community Health的其它文章
- COP27 climate change conference:urgent action needed for Africa and the world
- General practitioners’ (GPs) experience,attitudes and needs on clinical genetic services: a systematic review
- Relationship of Aboriginal family wellbeing to social and cultural determinants, Central Australia: ‘Waltja tjutangku nyakunytjaku’
- Impact of COVID- 19 infection rates on admissions for ambulatory care sensitive conditions: nationwide difference- in- difference design in Japan