AST-to-ALT ratio and coronary artery lesions among patients with Kawasaki disease
2022-01-12LeiCaoYunJiaTangMiaoGangJinMaWeiGuoQianQiuQinXuHaiTaoLv
Lei Cao · Yun-Jia Tang · Miao Gang · Jin Ma 2 · Wei-Guo Qian · Qiu-Qin Xu · Hai-Tao Lv
Abstract
Keywords Alanine aminotransferase · Aspartate aminotransferase · Coronary artery lesions · Kawasaki disease
Introduction
Kawasaki disease (KD), also known as mucocutaneous lymph node syndrome, is a common form of vasculitis in children and shows a predilection to form coronary artery lesions (CALs) [ 1]. It has recently replaced rheumatic fever as the main cause of acquired heart diseases in developed countries [ 1]. Although the mechanisms underlying KD remain unclear, intravenous immunoglobulin (IVIG) is widely recommended as the first-line therapy and is used as soon as possible after diagnosis to prevent CALs, in accordance with the recommendations of the latest guideline [ 1].
Over the last two decades, increasing efforts have been made to identify the risk factors of CALs. Male sex, infantile status, delayed treatment, IVIG resistance, and incomplete KD (IKD) were widely considered as the primary risk factors [ 2- 5]. However, a considerable proportion of KD patients without these factors still show CALs. Recently, the ratio of aspartate aminotransferase (AST) and alanine aminotransferase (ALT) levels, which are generally indicative of disease severity in chronic liver diseases, was reported to be predictive of the outcomes [ 6- 8]. Moreover, adult patients with a higher baseline AST-to-ALT ratio (AST/ALT) were shown to be prone to cardiovascular diseases and mortality[ 9]. Since KD is also a risk factor for cardiovascular diseases in which the coronary arteries are easily involved, we hypothesize that AST/ALT may also be associated with the occurrence of CALs.
To date, only one study focused on the association between AST/ALT and CALs in KD [ 10]. In that study, however, the authors categorized all patients into two groups based on AST/ALT and found that patients with a lower AST/ALT showed a higher incidence of CALs on every 2-week follow-up examination in the first month of disease onset. However, since most CALs occurred during the acute stage and regressed over time [ 11, 12], the findings of that study did not clarify whether the CALs appearing during follow-up were related to CALs on admission or if the AST/ALT itself had effects on CALs appearing de novo after IVIG. Moreover, the presence of a linear relationship between AST/ALT and CALs remains unexplored. In the present study, we aimed to further investigate the associations between AST/ALT and CALs, both on admission and in the cases of de novo CALs appearing after IVIG.
Methods
Participants
We retrospectively reviewed the medical records of patients hospitalized with a main diagnosis of KD, including both complete KD and IKD, in Children’s Hospital of Soochow University between January 2019 and December 2020. The diagnosis of KD was confirmed when a patient was febrile for ≥ 5 days and showed at least four of the following characteristics: (1) rash; (2) bilateral conjunctive injection; (3) cervical lymphadenopathy; (4) changes in the extremities; and (5) oral mucosal changes. IKD was diagnosed when patients had two or three compatible clinical characteristics and other diseases with similar presentations were excluded. Patients were excluded if they (1) showed a second episode of KD, since previous CALs could have persisted as coronary complications in such patients; (2) received initial IVIG treatment at another hospital, since the laboratory variables for such patients were incomplete and occasionally unavailable;or (3) did not receive IVIG due to economic concerns or defervescence before IVIG. All patients were treated with 2 g/kg IVIG in a single dose together with 30-50 mg/kg/day aspirin. The Institutional Review Board of Children’s Hospital of Soochow University approved this study (No:2021CS086), and the requirement for informed consent was waived because of the retrospective nature of the study.
A total of 877 patients with the main diagnosis of KD were treated in our hospital during the study period. Among them, seven patients with missing AST and (or) ALT values and two with missing echocardiographic reports (both on admission and after IVIG) were excluded. Among the remaining 868 patients, 37 were excluded, including two patients who showed a second episode of KD, 23 who did not receive IVIG treatment due to economic concerns or defervescence before IVIG, 10 who received initial IVIG treatment in other hospitals prior to admission, and two who were auto-discharged (Fig. 1).
Data collection
Data for demographic, clinical, and laboratory characteristics were obtained. These variables included measurements of ALT and AST levels, outcomes of CALs on admission and CALs appearing de novo after IVIG, and other factors such as sex, age, days of illness at IVIG initiation, IKD,IVIG resistance, white blood cell (WBC) count, C-reactive protein (CRP) level, hemoglobin level, hematocrit, percentage of neutrophils, and serum concentrations of albumin,total bilirubin, cholesterol, sodium, and potassium. AST/ALT was calculated and obtained by AST divided by ALT.Blood tests were routinely performed within 24 hours of admission. Routine two-dimensional echocardiographic evaluation was performed before IVIG initiation and was repeated within 2 weeks of the disease onset. The missing numbers of data are shown in Supplementary Table 1.
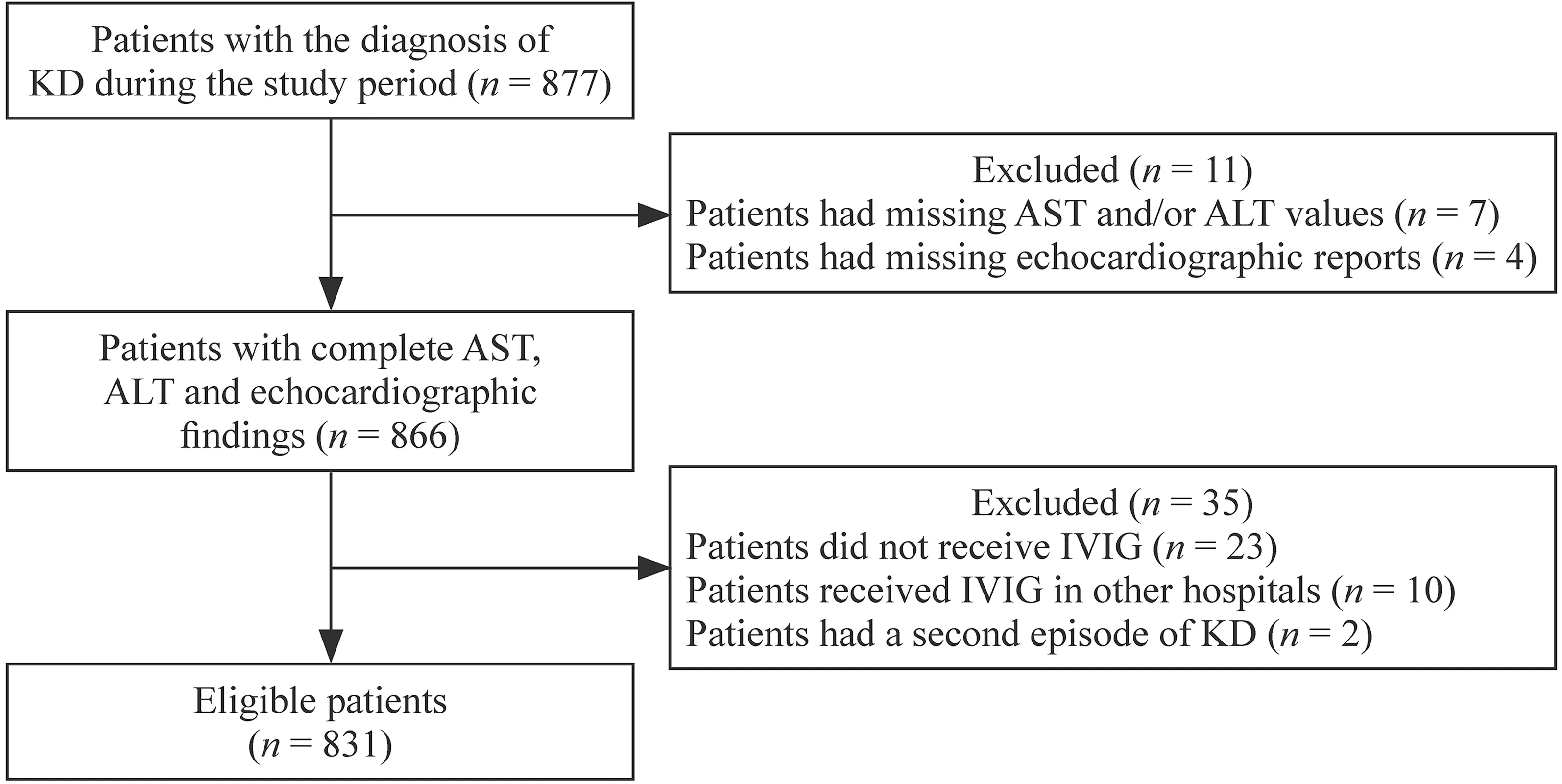
Fig. 1 Study flow diagram. KD Kawasaki disease, AST aspartate aminotransferase, ALT alanine aminotransferase, IVIG intravenous immunoglobulin
Definitions
We calculated theZscores for the left main coronary artery,left circumflex artery, left descending artery, and right coronary artery by using a previously reported method [ 13].CALs were defined by aZscore ≥ 2.5 for any coronary artery and (or) clear irregularity of the coronary lumen.IVIG resistance was considered when patients showed a persistent or recrudescent fever > 38.0 ℃ lasting for more than 36 hours after the initiation of IVIG [ 1]. Delayed IVIG treatment was termed as IVIG initiation after the 10th day of illness.
Statistical analysis
Categorical variables were expressed as numbers and percentages. Continuous variables were shown as median with mean ± standard deviation (SD) or median with quartiles. In comparisons between two groups, the Mann-WhitneyUtest or Student’sttest was used as appropriate.
We examined the distribution of AST and ALT levels and found that they were strongly skewed right. Log10transformations of AST and ALT were then performed and the generated values were used in downstream analyses. Univariate logistic regression analysis was performed to explore the risk factors for CALs on admission. Multivariable-adjusted analysis was performed to evaluate the associations between AST/ALT and CALs. The covariates, when added to the model, changed the matched odds ratio (OR) by at least 10% and were selected for adjustments. IVIG resistance was added to the multivariable-adjusted analyses for CALs appearing de novo after IVIG, and IKD was added to multivariable-adjusted analyses for CALs on admission and those appearing after IVIG because they were widely considered to be a risk factor for CALs. The variance inflation factor was then used to examine the multicollinearity of the covariates, and a variance inflation factor ≥ 5 indicated multicollinearity. To examine the associations between AST/ALT and CALs, we carried out three models. Model 1 had no adjustment. Model 2 adjusted for age and sex. Model 3 adjusted for model 2 plus CRP, albumin, total bilirubin, delayed IVIG treatment after the 10th day, and IKD. We also divided AST/ALT into quintiles in multivariable-adjusted analyses.Based on logistics regression model, restricted cubic spline with four knots was used to identify the linear relationships between AST/ALT and CALs. Further, fitted curve of the presence of CALs on admission against observed AST/ALT was performed. Area under the receiver-operator characteristic (ROC) curve (AUC) was used to identify the capacity of the variables to predict CALs on admission. DeLong's test was used to compare the difference of AUC. We determined the missing data by multiple imputation methods and carried out the sensitivity analyses.
Subgroup analyses were carried out to assess the following variables: age (< 1 year vs. ≥ 1 year), sex, IVIG resistance, IKD, and days of IVIG at initiation (< 10 days vs. ≥ 10 days). All statistical analyses were performed using R for Windows (Version 4.0.4). A two-sidedP< 0.05 was considered significant.
Results
A total of 831 patients, including 473 (56.9%) males and 358 (43.1%) females, were enrolled. The characteristics of the patients are shown in Table 1. The median age was 24 months, while 152 (18.3%) children were under 12 months of age. IKD was observed in 153 patients(18.4%), while 678 (81.6%) patients showed complete KD.Ninety-eight (11.8%) patients received delayed IVIG treatment. A total of 223 patients had CALs either on admission or showed repeated CALs after IVIG. They were younger and tended to be male. They also tended to have received delayed IVIG treatment and higher incidence of IVIG resistance, showed higher WBC counts and CRP, ALT levels, and lower hematocrit, AST/ALT, and hemoglobin, albumin, cholesterol, and serum sodium levels (P< 0.05). Among these patients, 201 (24.2%) had CALs on admission while 21(2.5%) showed CALs de novo after IVIG, and one showed CALs after IVIG with missing echocardiographic reports on admission.
The results of univariate analysis of CALs are shown in Table 2. Male sex, younger age, delayed IVIG treatment,higher WBC count and CRP and ALT levels, and lower AST/ALT, hematocrit, and hemoglobin, albumin, and cholesterol levels were associated with higher incidences of CALs on admission. Models to evaluate the associations between AST/ALT and CALs on admission were evaluated with and without adjustments (Table 3). In the crude model, AST/ALT as a continuous variable was negatively associated with CALs on admission (P= 0.002). Even afteradjusting for potential confounders, the results remained the same (P= 0.007). A notably negative linear relationship was observed between AST/ALT and odds ratio of CALs after adjusting for potential confounders (Pfor nonlinear was 0.6, Fig. 2). Each unit increase in AST/ALT was related to a 22% lower risk of CALs on admission [OR = 0.78, 95%confidence interval (CI) 0.65-0.94]. Among the AST/ALT quintiles, Q2 showed a significant 40% lower risk of CALs on admission in comparison with Q1 (95% CI 0.36-0.99,P< 0.05), Q4 showed a 56% lower risk of CALs (95% CI 0.25-0.77,P< 0.01), and Q5 showed a 54% lower risk of CALs (95% CI 0.26-0.80,P< 0.01) in the fully adjusted model. The same results were also noted in ALT and CALs on admission, rather than AST and CALs on admission(Table 3). Expected presence of CALs on admission was also negatively related to AST/ALT after adjusting the other confounders (Fig. 3). We determined the missing data by multiple imputation methods and obtained the same results(Supplementary Table 2). ROC curves for prediction of CALs on admission with versus without AST/ALT are shown in Supplementary Fig. 1. The AUC of models with and without AST/ALT were 0.660 (95% CI 0.617-0.704)and 0.644 (95% CI 0.661-0.689), respectively (P= 0.023).
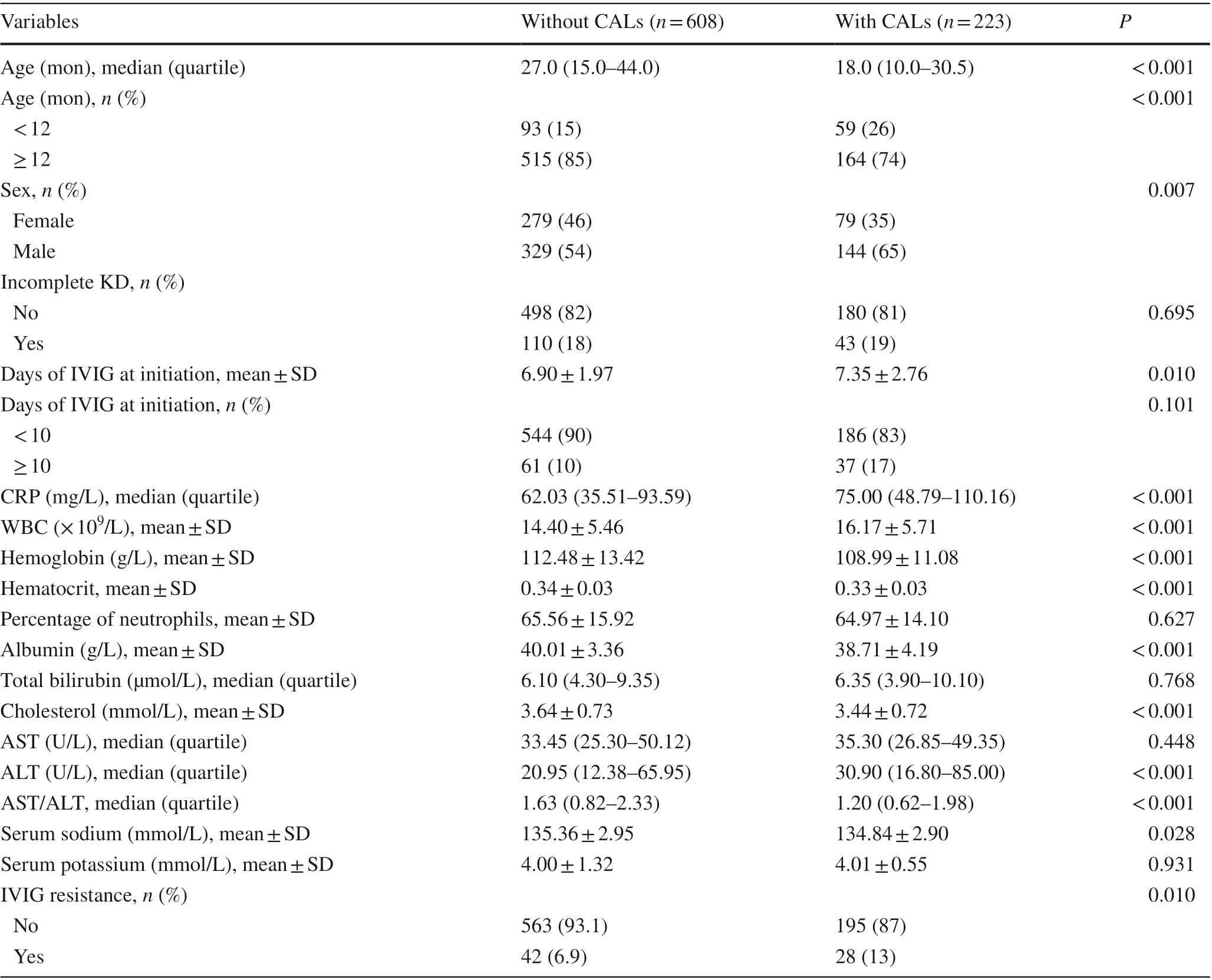
Table 1 Characteristics of all patients
Univariate analysis also identified associations of younger age and a higher total bilirubin level with CALs appearing de novo after IVIG (P< 0.05). A higher ALT level and lower AST/ALT were also associated with CALs appearing de novo after IVIG, although the differences were not significant. Notably, IVIG resistance was positively related to CALs appearing de novo after IVIG (P< 0.001, Table 2). We performed analyses to determine whether AST/ALT was a risk factor for CALsappearing de novo after IVIG (Table 4) and found that AST/ALT was not associated with CALs appearing de novo after IVIG irrespective of whether it was considered as a continuous or a categorical variable. Neither ALT nor AST was associated with CALs appearing de novo after IVIG after adjustments. These results were consistent with the findings of sensitivity analyses in Supplementary Table 2.
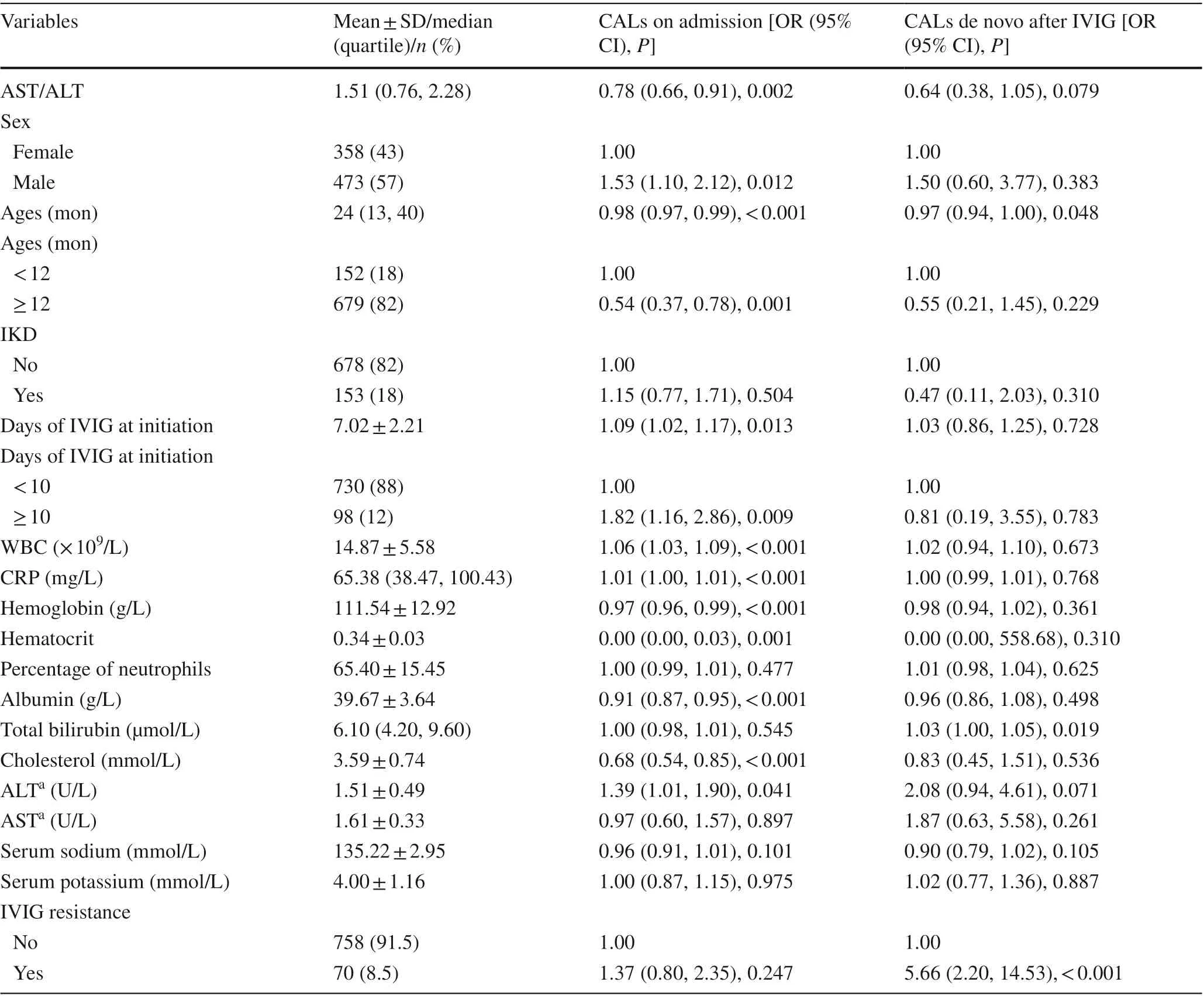
Table 2 Results of univariate analysis of coronary artery lesions on admission
Subgroup analyses were further carried out, and the results are shown in Supplementary Figs. 2 and 3. A total of 824 and 794 patients were included in these analyses,respectively. None of the variables significantly modified the association between AST/ALT and CALs on admission and CALs appearing de novo after IVIG (allP> 0.05).
Discussion
In this retrospective study, AST/ALT was associated with CALs on admission, and a linear relationship was noted between them. However, such an association was not observed between AST/ALT and CALs appearing de novo after IVIG. Besides, none of the variables such as sex, IKD,infantile patients, delayed IVIG treatment after the 10th day, and IVIG resistance modified these associations significantly. Our findings suggested that AST/ALT was a risk factor for the occurrence of CALs on admission, but not a risk factor for progressive CALs.
AST/ALT, also known as the De Ritis ratio, was first described in 1956 by De Ritis et al. [ 14] and has beenwidely studied in urological cancers [ 15- 18]. More recently, it was reported to be associated with cardiovascular diseases [ 9, 19], with a higher baseline AST/ALT being predictive of poor outcomes. In contrast, we found that a lower AST/ALT was indicative of CALs in the acute stage of KD. This divergence could be primarily attributed to differences in the study populations. ALT is liver-specific and its elevation is generally considered to indicate hepatic damage. However, older adults usually show reduced liver size and liver blood flow due to hepatic aging, which results in a lower ALT level [ 20, 21].Thus, lower ALT levels were strongly positively associated with the risk of death in older adults [ 19]. Since this phenomenon could not be observed in children, hepatic dysfunction in KD usually presented with elevations of the enzyme levels [ 6- 8].
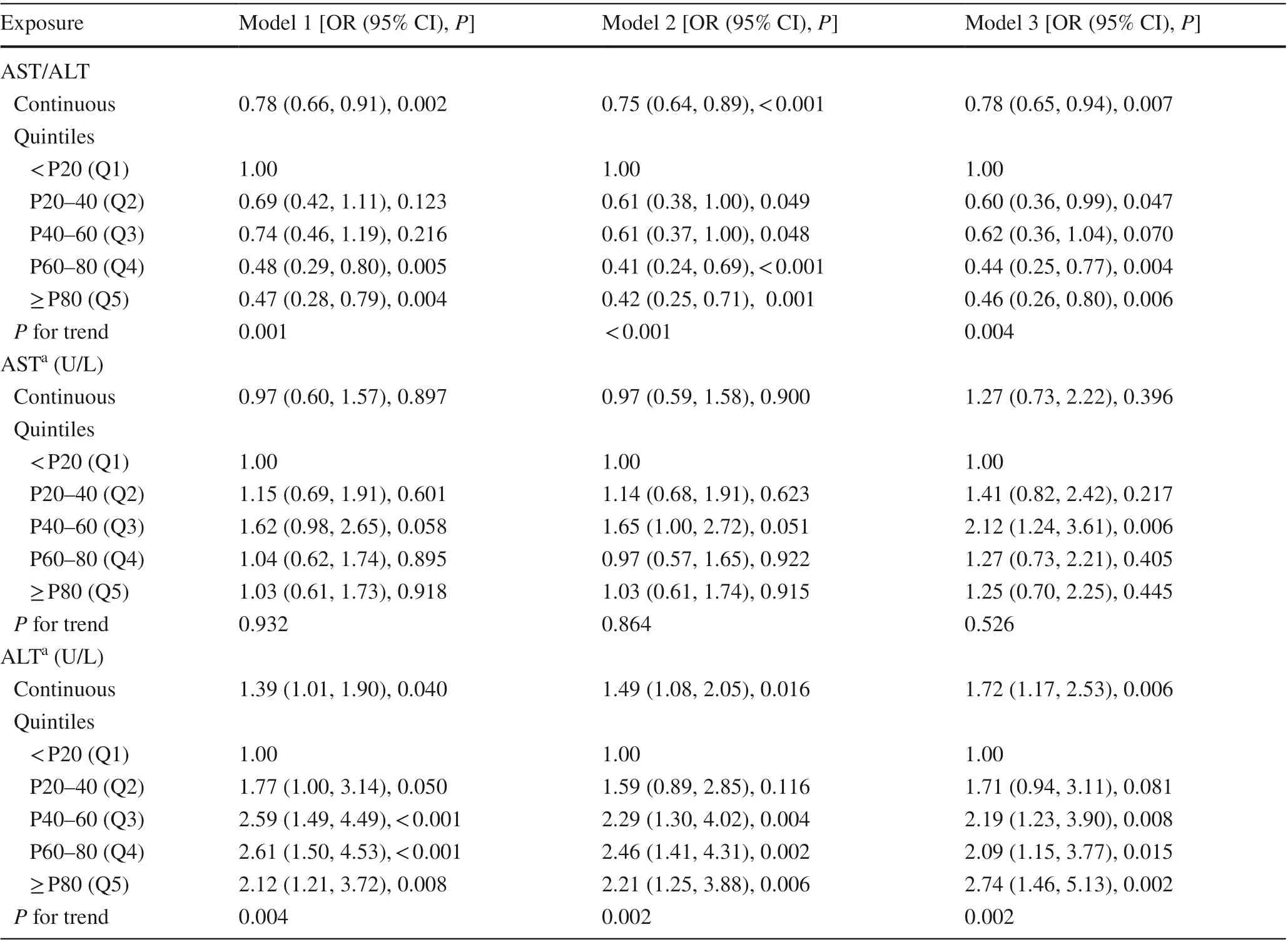
Table 3 Relationship between aspartate aminotransferase/alanine aminotransferase and coronary artery lesions on admission in different models
Wang et al. had previously enrolled 2678 patients and categorized them into two groups based on AST/ALT [ 10].They found that patients with a low AST/ALT showed a higher incidence of CALs during the first 4-week followup based on the absolute diameters of the coronary arteries. Although our findings showed a negative relationship between AST/ALT and CALs on admission when AST/ALT was handled as a continuous variable and a categorical variable (bothP< 0.05), we further identified that AST/ALT was not associated with CALs appearing de novo after IVIG. Since most CALs improved over time[ 11, 12], we speculated that CALs during the follow-up were largely attributed to unimproved CALs on admission in their study. Thus, AST/ALT could serve as a predictive risk factor for CALs, but not as a risk factor for progressive CALs.
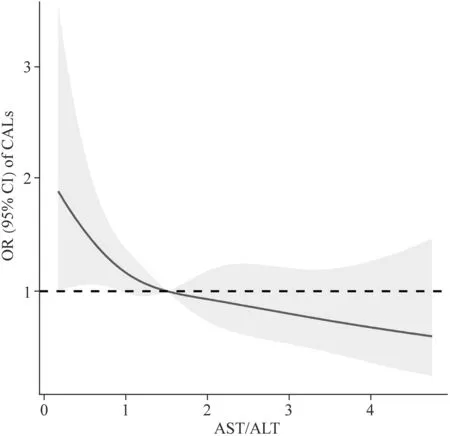
Fig. 2 The adjusted odds ratio (OR) for AST/ALT and CALs on admission. The black solid line indicates OR. The shaded area represents the 95% confidence interval (CI). AST aspartate aminotransferase, ALT alanine aminotransferase, CALs coronary artery lesions
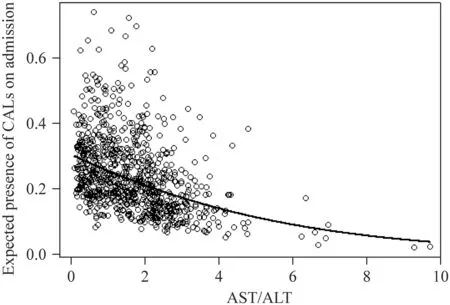
Fig. 3 AST/ALT and expected presence of CALs on admission. The black hollow circles indicate AST/ALT and the expected presence of CALs on admission ofindividuals. The black line indicates the expected presence of CALs on admission based on observed AST/ALT and on the mean values of the confounding variables used to fit Model 3. AST aspartate aminotransferase, ALT alanine aminotransferase, CALs coronary artery lesions
Previously, a lot of studies were focused on the risk factors of CALs [ 2- 5], including both initial and repeated CALs during the acute stage of the disease. Herein, we also identified elevated total bilirubin and IVIG resistance as independent risk factors for CALs de novo after IVIG. Hyperbilirubinemia was frequently seen in KD which was caused by the lysis of hepatocytes and was indicative of intensive inflammatory response [ 22, 23]. Interestingly, it was related to CALs de novo after IVIG rather than CALs on admission, indicating a correlation with a remote expression of CALs. IVIG resistance was an important indicator of severe inflammatory vasculitis so that great efforts had been made to identify the risk factors[ 24- 26]. Not surprisingly, it was positively related to CALs de novo after IVIG. Thus, applying prediction models to screen out these patients would intensively improve the outcomes.
We further identified a linear relationship between AST/ALT and CALs on admission, indicating that a lower AST/ALT was associated with a higher incidence of CALs. ALT is mainly located in the liver, with small amounts present in the skeletal muscle. In contrast, AST is located widely in the liver, skeletal muscle, myocardium, kidney, etc. As the most important enzymes of the liver, both of them have been reported to be associated with IVIG resistance in several prediction systems for KD[ 25- 27], which was generally indicative of more severe inflammation. However, only ALT was associated with CALs on admission in our present study. AST is one of the cardiac markers, and elevated AST levels may indicate a hypoperfusion state due to cardiac dysfunction [ 28].Although KD was one of the most common cardiovasculitis in children, it was reported that no difference in AST was noted in patients with CALs versus those without[ 29]. Therefore, we speculated that an increase in the ALT level was more unfavorable to some extent, and thus led to a lower AST/ALT in these patients.
Anjani et al. recently reported a case involving a boy who died of fulminant acute liver failure in the disease course of KD. The post-mortem liver biopsy showed fibrinoid necrosis of the small-sized artery, which suggested hepatic vasculitis [ 30]. Amano et al. reported hepatic vasculitis in 13 of all 17 autopsied patients, all of whom showed complicating coronary artery aneurysms, indicating a high incidence of hepatic vasculitis in patients with CALs [ 31]. Although hepatitis was much frequently seen during the acute stage, other organ dysfunctions have also been reported [ 32- 34]. Considering the wide distribution of AST and the high liver specificity of ALT, AST/ALT could partly reflect vasculitides other than hepatic vasculitis.
Our study should be viewed in light of certain limitations. First, we primarily investigated CALs in the acute stage of KD because most CALs occurred during the early stage of the disease, because most CALs occurred during the early stage of the disease and regressed over time [ 11, 12]. Second, we did not analyze troponin or brain natriuretic peptide, which are more sensitive in cardiac dysfunction and myocardial damage, because theywere not routinely tested and different assays had been used to assess troponin. Third, selection biases existed due to the retrospective nature of the study. Forth, since that AST/ALT was only a predictor of initial CALs on admission and was not a predictor of progressive CALs,a decreased AST/ALT could not be an indicator of more aggressive therapy. Lastly, we were unable to conclude that AST/ALT was useful in the diagnosis of KD because there were no such febrile controls in the present study,although maybe AST/ALT truly was. Further prospective studies to include long-term follow-up and febrile controls are needed in the future. Overall, the results of the study were robust for a relatively large number of participants and were strengthened by sensitivity analyses.
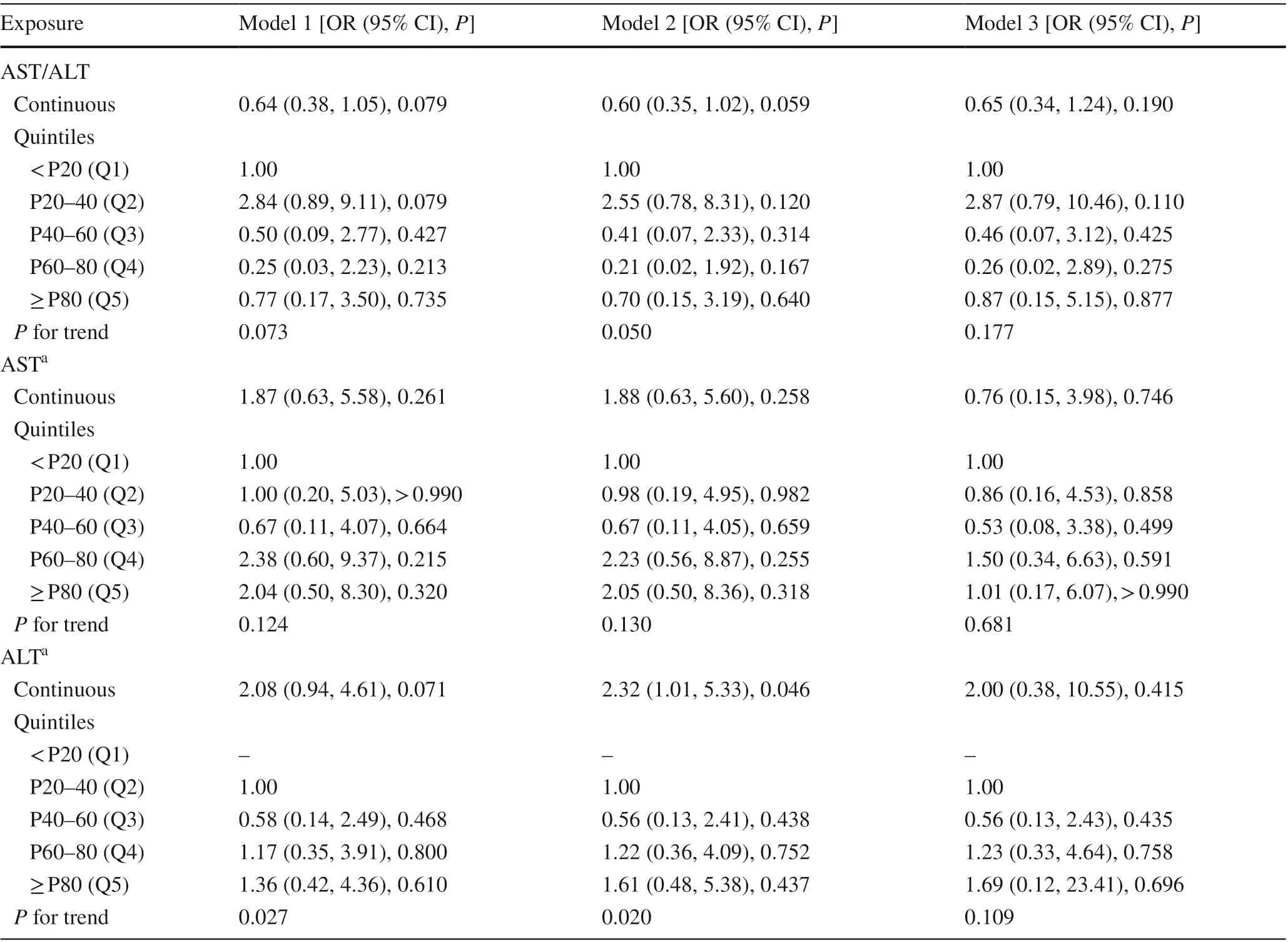
Table 4 Relationship between aspartate aminotransferase/alanine aminotransferase and coronary artery lesions de novo after intravenous immunoglobulin treatment in different models
Supplementary Information The online version contains supplementary material available at https:// doi. org/ 10. 1007/ s12519- 021- 00479-0.
Author contributions CL and TYJ contributed equally to this study as first co-authors. CL contributed to investigation, methodology and writing original draft. TYJ contributed to conceptualization, data curation, funding acquisition, reviewing, and editing. GM contributed to investigation and methodology. QWG, MJ, and XQQ contributed to investigation, and project administration. LHT contributed to conceptualization, funding acquisition and supervision. All authors read and approved the final manuscript.
Funding This work was financially supported by the National Natural Science Foundation of China (Nos. 81870365, 81700439,and 81801559), Gusu Health Personnel Training Project (Nos.GSWS2019048 and 2020054), Suzhou Science and Technology Development Plan Project (Nos. SYS2019084 and SS202066),and Jiangsu Province Key Medical Young Talents (No. QNRC 2016765).
Data availability The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Compliance with ethical standards
Ethical approval The Institutional Review Board of Children’s Hospital of Soochow University approved this study (No. 2021CS086).
Conflict of interest No financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article. The authors have no conflict of interest to declare.
杂志排行
World Journal of Pediatrics的其它文章
- Muscle strength and its association with cardiometabolic variables in adolescents: does the expression of muscle strength values matter?
- Vestibular function of pediatric patients with sudden sensorineural hearing loss: based on vertigo symptom and vestibular function testing
- Evaluation of a new frequency-volume chart for children with primary monosymptomatic nocturnal enuresis: a prospective, comparative study
- Consensus statement on the epidemiology, diagnosis, prevention,and management of cow's milk protein allergy in the Middle East:a modified Delphi-based study
- Treatment of pediatric mild persistent asthma with low-dose budesonide inhalation suspension vs. montelukast in China
- Haploidentical hematopoietic stem cell transplantation for pediatric patients with chronic active Epstein-Barr virus infection:a retrospective analysis of a single center
