A Scenario-Based Evaluation of COVID-19-Related Essential Clinical Resource Demands in China
2021-12-25TingZhngQingWngZhiweiLengYunYngJinYngFngyunChenMengmengJiXingxingZhngWeirnQiYunshoXuSiyChenPeixiDiLiingLuzhoFengWeizhongYng
Ting Zhng, Qing Wng, Zhiwei Leng, Yun Yng, Jin Yng, Fngyun Chen, Mengmeng Ji,Xingxing Zhng, Weirn Qi, Yunsho Xu, Siy Chen, Peixi Di, Liing M,c, Luzho Feng,*,Weizhong Yng,*
a School of Population Medicine and Public Health, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing 100730, China
b Division of Infectious Diseases, Chinese Center for Disease Control and Prevention, Beijing 102206, China
c Department of Respiratory and Critical Care Medicine, The Affiliated Hospital of Guilin Medical University, Guilin 541001, China
Keywords:COVID-19 Transmission dynamics model Clinical resource demands Vaccination
ABSTRACT The coronavirus disease 2019(COVID-19)pandemic is a global crisis,and medical systems in many countries are overwhelmed with supply shortages and increasing demands to treat patients due to the surge in cases and severe illnesses. This study aimed to assess COVID-19-related essential clinical resource demands in China, based on different scenarios involving COVID-19 spreads and interventions. We used a susceptible–exposed–infectious–hospitalized/isolated–removed (SEIHR) transmission dynamics model to estimate the number of COVID-19 infections and hospitalizations with corresponding essential healthcare resources needed.We found that,under strict non-pharmaceutical interventions(NPIs)or mass vaccination of the population,China would be able to contain community transmission and local outbreaks rapidly.However,under scenarios involving a low intensity of implemented NPIs and a small proportion of the population vaccinated, the use of a peacetime–wartime transition model would be needed for medical source stockpiles and preparations to ensure a normal functioning healthcare system.The implementation of COVID-19 vaccines and NPIs in different periods can influence the transmission of COVID-19 and subsequently affect the demand for clinical diagnosis and treatment. An increased proportion of asymptomatic infections in simulations will not reduce the demand for medical resources; however,attention must be paid to the increasing difficulty in containing COVID-19 transmission due to asymptomatic cases. This study provides evidence for emergency preparations and the adjustment of prevention and control strategies during the COVID-19 pandemic. It also provides guidance for essential healthcare investment and resource allocation.
1. Introduction
On March 11, 2020, the World Health Organization (WHO)declared the coronavirus disease 2019 (COVID-19) epidemic to be a pandemic [1]. As of January 16,2021, 92 262 621 cases had been confirmed and 1 995 037 deaths had been reported worldwide[2].In Chinese mainland,community transmission in the first wave was fully contained through the implementation of stringent interventions [3–5]. Due to multiple factors, for example, virus variations and improvement in case detection and diagnosis capacity[5], the proportion of asymptomatic infections among reported cases has increased compared with the initial epidemiological curve. Significant pressure to the healthcare system can result whenever a large-scale outbreak occurs. The current increase in the number of COVID-19 cases in the United States and the United Kingdom has posed huge challenges to their healthcare systems[6]. Moreover, the available number of essential healthcare resources is also of importance. The number of hospital beds per 1000 people in Wuhan, China and in Italy is 7.28 and 3.49 [7],respectively, which are both higher than the average global level(2.7) and higher than that of middle- (2.4) and low-income (1.2)countries [8]. During the period of exponential increase in the number of cases, with a cumulative incidence rate of 0.59% in Wuhan, China and 0.05% in Italy, the case fatality rate increased significantly because healthcare systems were overloaded [9,10].
Healthcare systems always bear the brunt in a pandemic[11,12]. Once such systems become overloaded, an increasing number of people cannot be admitted for treatment or isolation,which not only amplifies disease transmission but also leads to excess mortality[13,14].It has been estimated that,on September 6,2020,there may have been in excess of three million healthcare workers infected worldwide[15].Due to a lack of personal protective equipment(PPE),front-line healthcare workers in many countries have been at significant risk of infection.Furthermore,due to the COVID-19 pandemic, healthcare professionals have suffered psychological and physical fatigue to a significant extent, which may reduce their ability to address the ongoing challenges of COVID-19 in the future. According to reported data from the WHO, every one in six patients hospitalized with COVID-19 will suffer from severe illness and breathing difficulties, with noninvasive ventilators often needed to assist with ventilation [16].Should a patient’s condition deteriorate, an invasive ventilator may be needed to provide further assistance with ventilation.With the rapid increase in the number of severe cases of COVID-19, a worldwide shortage of ventilators has resulted in patients in many countries not receiving adequate treatment[6].The total mortality rate in Wuhan, China, increased to between 33% and 42% in the first three months of 2020 compared with the same period in 2019. In total, 61% of excess deaths were related to COVID-19. A lack of access to healthcare services might be the key reason for the increase in non-pneumonia-related deaths, especially in relation to the long-term management and monitoring of chronic diseases such as diabetes mellitus, hypertension, and ischemic heart disease, as well as the failure of some emergency services to seek timely clinical treatment, resulting in a significant increase in out-of-hospital deaths [17].
Coping with a surge in clinical demands is challenging during a pandemic[18,19].The number of hospital beds per capita in many countries such as China is lower than that in developed countries[8],but those countries have struggled to implement appropriately targeted measures to combat this severe pandemic. Additional demands on medical resources during the pandemic have involved a greater need for PPE (e.g., masks and protective coveralls), a heavier workload for healthcare workers (doctors and nurses),and a more extensive need for healthcare equipment(e.g.,hospital and intensive care unit (ICU) beds and respirators). The co-circulation of other respiratory pathogens may involve symptoms similar to COVID-19, and the use of clinical resources will also increase [20,21].
An evaluation of essential clinical demand is one of the most urgent needs in terms of preparation and response for the next waves of the pandemic. Globally, many countries have faced allocation issues due to a shortage of healthcare resources since the early stage of the pandemic [6]. Moreover, very few assessments of clinical demand have been made in relation to COVID-19. In some studies,tools have been developed to assess clinical resource demands during the COVID-19 pandemic to predict the required number of hospitalizations and beds [22,23]. In published studies,estimations of clinical resources (e.g., beds and ventilators) have mainly been based on a predicted number of infections [24,25].However,there is a lack of detailed evaluations concerning clinical resource demands, in terms of the status of regular epidemic prevention and control, in relation to different parameters of prevention and control effectiveness. Based on various scenario assumptions, evaluated efficacy of the non-pharmaceutical interventions (NPIs) [3,4,26] and COVID-19 vaccines [27], and on a revised transmission dynamics model, this study aimed to assess clinical demands, using China as an example. Our results are intended to put forward a theoretical reference for emergency preparedness concerning healthcare resources and fill a lack of more effective adjustment of prevention and control strategies based various scenarios during the COVID-19 pandemic, as well as facilitating a better balance in terms of healthcare supply and demand.
2. Research methods
2.1. Concept definition
Clinical resources consist of three components: ① human resources,including doctors,nurses,and healthcare nursing workers in the hospital; ②beds and equipment, including hospital or isolation beds,ICU beds,and medical equipment(e.g.,ventilators);and ③PPE, including protective coveralls, isolation gowns, facemasks, gloves, isolation caps, face shields or goggles, and shoe covers.
An asymptomatic patient is defined as an individual infected with severe acute respiratory syndrome coronavirus 2 (SARSCoV-2)who does not exhibit symptoms during the course of infection.An inpatient refers to a symptomatic patient admitted to hospital or an asymptomatic case in centralized isolation.
2.2. Study process overview
An expanded model was built to assess the demand for healthcare resources in a Chinese city with a population of 10 million people. The epidemiological characteristics of COVID-19 were incorporated into the transmission parameters. Study results concerning the effectiveness of NPIs and an immunized population were used to parameterize the model for simulations under various scenarios. Taking the scale of a large city as an example, the initial quantitative value was determined based on qualitative scenario assumptions such as population size,transmission index,and prevention and control strategies and measures. Under different scenarios, the clinical demand was evaluated quantitatively in terms of the proportion of infections, inpatients, and resources as a result of hospitalization or isolation(Fig.1).The estimated results were then compared with actual reserves using an average per 10 million people in China [28,29] to determine whether the balance of supply and demand was met.
In Italy, COVID-19-related cases were reported later than in Wuhan, China but earlier than in other European countries, and only a few early NPIs against COVID-19 had been implemented;therefore, more accurate parameters of the natural spread of the disease, such as infectious rate after exposure (β), could be obtained through fitting data from Italy. Because of the lags between infection,illness onset,and reporting,we fitted the curve only from the start of the first reported inpatient case in Italy to the announcement of the extended lockdown(i.e.,from February 24 to March 20, 2020), during which time the number of cases did not exceed the load of the Italian healthcare system and China alerted the world of the outbreaks.Therefore,we compared the number of daily reported cases in Italy using data obtained from OurWorldIn-Data.org†† https://ourworldindata.org/coronavirus.with the number of confirmed cases estimated using the model to verify its accuracy.
2.3. Transmission dynamics model construction
2.3.1. Model assumptions
The model was constructed with the following assumptions:
(1) COVID-19 is characterized as a pandemic [1].
(2) There is no specific antiviral drug to treat COVID-19 [3].

Fig. 1. Data flow chart. PPE includes protective coveralls and surgical masks.
(3) There are uncertainties in terms of medical support from other regions and clinical demand relies solely on local preparations [12].
(4)Immunized people are age-distributed averagely throughout the whole population [6].
(5) Initial infection numbers are based on an average distribution [24].
(6) Asymptomatic infection is contagious [30].
(7)After the infectious period,patients enter a recovery period,during which they may have symptoms but no longer spread the virus [5].
(8) Hospitalized patients, due to isolation and infection control measures, are not considered as infectious [5].
(9) Once a patient has recovered, there will be no secondary infection.
(10) The total population (N) was the sum of the number of susceptible–exposed–infectious–hospitalized/isolated-removed(SEIHR) individuals, including the immunized population in some scenarios, which remained constant.
(11)Immunity,due to vaccination,is the result of the combined effect of vaccine efficacy and coverage.
(12) The COVID-19 vaccination immunity period is not considered in this study.
2.3.2. Evaluation model
The susceptible–exposed–infectious–removed (SEIR) transmission dynamics model was extended to include hospitalization and isolation and the SEIHR transmission dynamics model was developed (Fig. 1). Susceptible (S) refers to the total population,excluding the immunized population.Exposed (E) refers to people in the latent period. Symptomatic infections (I_a) refer to people who had been infected and who were infectious. Asymptomatic infections (I_b) refer to people who had been infected but had no symptoms and were infectious to a certain degree. Symptomatic hospitalizations (H_a) refer to hospitalized patients with mild-tosevere symptoms. Asymptomatic hospitalizations (H_b) refer to isolated patients without symptoms during the entire infection period. Removed (R) refers to people who had recovered or who had died(Fig.2).Different parameters of clinical demand for those hospitalized and isolated were used to differentiate between asymptomatic and symptomatic infections. Symptomatic patients who had been hospitalized required more clinical resources,whereas asymptomatic patients who were isolated required the isolation beds but fewer human resources and equipment. Many countries did not attempt to detect asymptomatic infections and did not hospitalize or isolate asymptomatic patients in centralized locations; therefore, the context of this modeling study was set in China.
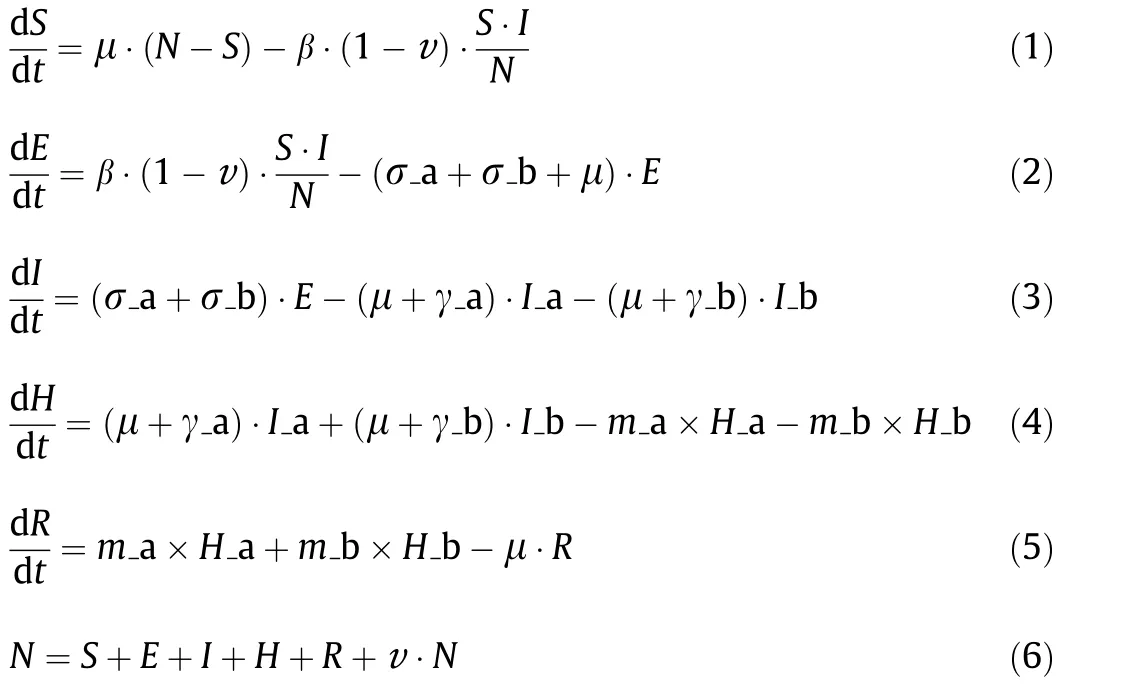
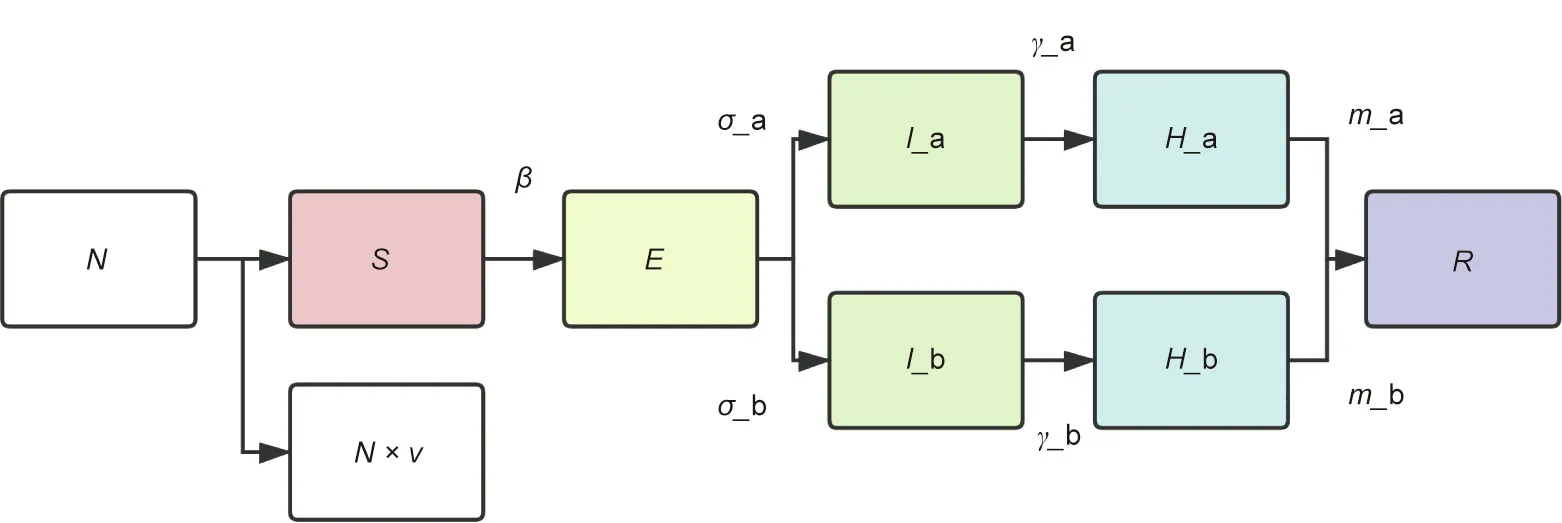
Fig.2. An illustration of the extended SEIHR transmission dynamics model.v:the proportion of immunized population(vaccinated population x vaccine effectiveness);β:the rate per unit of time at which the susceptible become infected; σ_a: rate of a latent infection progressing to a symptomatic infection; σ_b: rate of a latent infection progressing to an asymptomatic infection;γ_a: rate of a symptomatic infection progressing to inpatient admission;γ_b: rate of an asymptomatic infection progressing to inpatient admission; m_a: rate of a symptomatic inpatient progressing to recovery or death; and m_b: rate of an asymptomatic inpatient progressing to recovery or death.
The relationships of the parameters in Fig. 2 are as the above model. μ is defined as the natural mortality rate which was not considered in this calculation, t is for a particular moment, and H and I are the hospitalizations/isolations and infections,respectively.Other parameters are defined in the caption of Fig. 2.
2.3.3. Scenario construction
In this study, six scenarios were constructed based on differences in the immunized population, the effectiveness of NPIs, the percentage of asymptomatic patients, and the contact warning capability concerning cases in a city with a population size of 10 million people. Parameters regarding epidemiological characteristics and clinical resource use during the COVID-19 pandemic were obtained from previously published studies [31–34], unpublished studies, expert professional opinion, and real-world investigations as shown in Table 1 [30,34–36].
2.3.4. Clinical resource parameters
According to the model above, we predicted the distribution of current patients in hospital or in isolation (H) and its peak. Based on a previous study[36],the average length of hospitalization/isolation was 12–15 days and the proportion of critical patients was 4.7%. We assumed that healthcare workers worked one of four working shifts per day and worked six hours per day, and that the ratio of on-duty doctors to inpatients was 1:10, whereas in the ICU, this ratio was 1:1. We calculated the ratio of doctors to patients (general hospital beds, 1:2.5; ICU beds, 1:1), the number of nurses per patient(inpatients,1:3;ICU,2:1),healthcare workers per patient(inpatients,1:10;ICU,1:2),and the demand for clinical resources such as ICU beds,hospital beds, isolation beds, and ventilators. Similarly, the model also calculated the peak demand for human resources. Calculations concerning protective material were determined according to the peak in medical staff and concerning personal protection standards [26,36].
When he had read it the governor was certainly a little astonished; but he was told in the letter to ask no questions, and he knew how to obey orders
2.4. Model validation
The SEIHR transmission dynamics model was tested using inpatient data obtained during the first epidemic wave in Italy, which ran from February 14, 2020 to July 31, 2020. The daily number of hospitalized cases was collected to distinguish between the results calculated using the model and real-world results(Fig.3).In Fig.3,the data from Italy refer to currently hospitalized patients,whereas‘‘H” in the SEIHR model refers to currently hospitalized or isolated patients as predicted using the model. The shadow represents the difference between the data. We concluded from the results that the fitting degree was high at the initial stage of the epidemic.However, the peak value of the actual epidemic curve was lower and the arrival time was later,which may be related to fewer early interventions and an increase in prevention and control measureslater on. Therefore, we concluded that the fitting effect of the model was superior at a later course in time rather than earlier on.
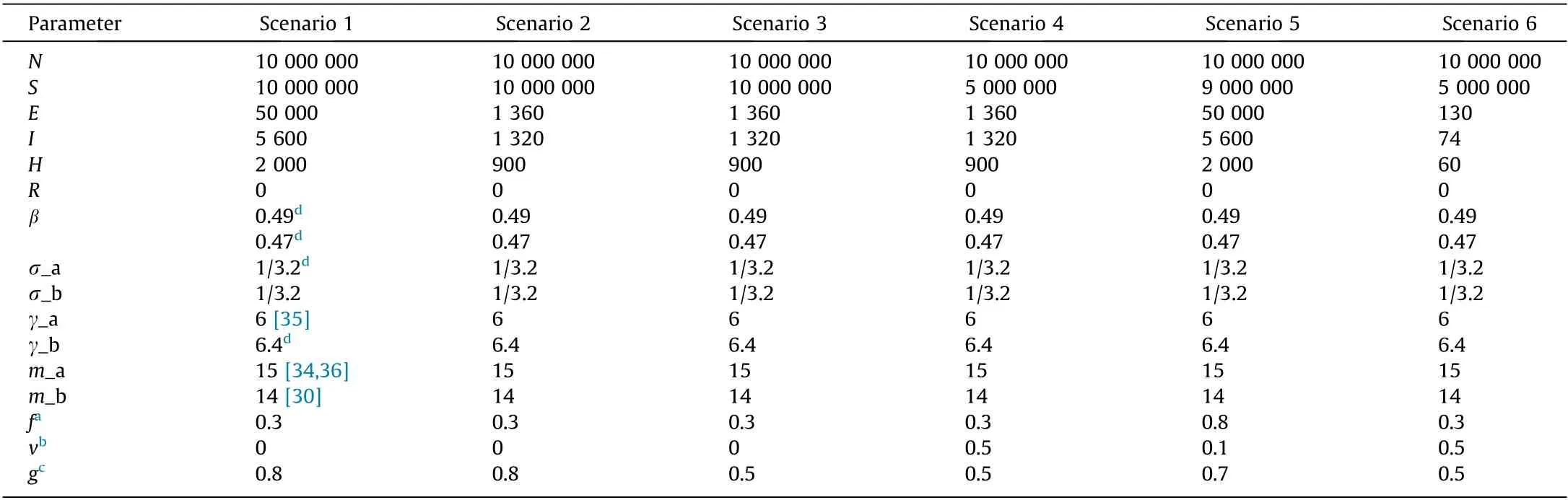
Table 1 Parameters for clinical demand evaluation in six scenarios concerning the COVID-19 pandemic.
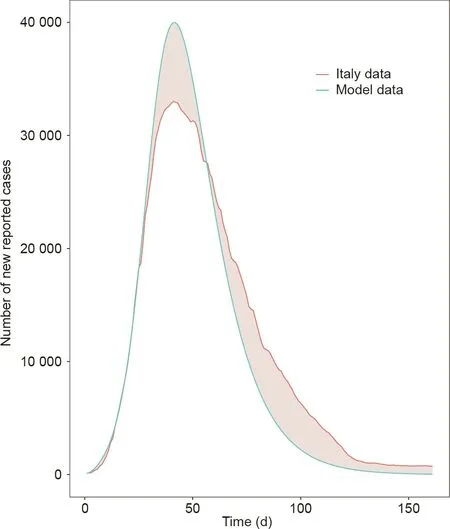
Fig. 3. The reliability of the model was tested through comparing evaluation data with real-world results in Italy. The pink shadow indicates the gap between the model evaluation and the actual number of reported cases in Italy. The smaller the gap, the more reliable the model parameters and the more accurate the results of this study, with errors in the evaluation results regarded as acceptable.
3. Results
Based on different scenarios, the symptomatic and asymptomatic was drawn from the SEIHR transmission dynamics model(Fig. 4) and the medical resources was calculated based on the number of infections.
3.1. Scenario 1
When the number of inpatients reached 2000, strict NPIs such as lockdown could effectively control the epidemic within approximately three months. We set the effectiveness of NPIs at 80% in this scenario and asymptomatic infections at 30%. The peak numbers of symptomatic infections, symptomatic inpatients, asymptomatic infections, and asymptomatic inpatients were 21 374,29 889,9569,and 12 361,respectively(Fig.4(a)).In terms of numbers, doctor demand was 20 307 (Fig. 5(a)), nurse demand was 23 548 (Fig. 5(b)), and healthcare nursing worker demand was 13 085(Fig.5(c)).Hospital bed demand was 9367(Fig.6(a)),isolation bed demand was 31 388(Fig.6(b)),ICU bed demand was 1494(Fig. 6(c)), ventilator demand was > 2750 (Fig. 6(d)), and oxygen machine demand was 5679 (Fig. 6(e)).
3.2. Scenario 2
On the basis of scenario 1, when strict NPIs such as lockdown were implemented earlier,we assumed that the maximum number of cases would not exceed 2000. We also assumed that 30% of infections were asymptomatic.The peak numbers of symptomatic infections, symptomatic inpatients, asymptomatic infections, and asymptomatic inpatients were 1027, 1560, 526, and 740, respectively (Fig. 4(b)). Doctor demand was 1118 (Fig. 5(a)), nurse demand was 1286 (Fig. 5(b)), and healthcare nursing worker demand was 700 (Fig. 5(c)). The hospital bed demand was 501(Fig. 6(a)), isolation bed demand was 1758 (Fig. 6(b)), ICU bed demand was 80 (Fig. 6(c)), ventilator demand was 147 (Fig. 6(d)),and oxygen machine demand was 304 (Fig. 6(e)). Compared with scenario 1, the clinical demand was lower.
3.3. Scenario 3
Compared with scenario 1, we assumed that fewer NPIs would lead to more serious consequences. We set the effectiveness of NPIs at 50%in this particular scenario.The peak numbers of symptomatic infections, symptomatic inpatients, asymptomatic infections, and asymptomatic inpatients were 263 232, 607 006,127 515, and 258 857, respectively (Fig. 4(c)). Compared with scenario 1, there was a 12–20 times increase in the infection or inpatient rates. Doctor demand was 414 724 (Fig. 5(a)), nurse demand was 480 099 (Fig. 5(b)), and healthcare nursing worker demand was 265 747 (Fig. 5(c)). Hospital bed demand was 190 236(Fig. 6(a)), isolation bed demand was 643 627 (Fig. 6(b)), ICU bed demand was 30 350 (Fig. 6(c)), ventilator demand was 55 844(Fig. 6(d)), and oxygen machine demand was 115 331 (Fig. 6(e)).Without strict NPIs,the maximum number of cases could approach one million.
3.4. Scenario 4
On the basis of scenario 3,we assumed that the proportion of the immunized population had reached 50%. The peak numbers of symptomatic infections, symptomatic inpatients, asymptomatic infections, and asymptomatic inpatients were 1057, 1784, 542,and 830, respectively (Fig. 4(d)). Doctor demand was 1249(Fig. 5(a)), nurse demand was 1436 (Fig. 5(b)), and healthcare nursing worker demand was 781 (Fig. 5(c)). Hospital bed demand was 559(Fig.6(a)),isolation bed demand was 1965(Fig.6(b)),ICU bed demand was 89 (Fig. 6(c)), ventilator demand was 164(Fig.6(d)),and oxygen machine demand was 339(Fig.6(e)).When an immunized population reaches 50%, the degree of NPIs can be appropriately reduced to alleviate the serious socioeconomic effects of implementing NPIs and promote social and economic recovery.
3.5. Scenario 5
Compared with scenario 1, we assumed 80% of those with a positive nucleic acid test were asymptomatic, and that the total number of cases would not change significantly. However, when the proportion of asymptomatic infections reaches 80%, the cost of medical supplies is likely to be extremely high. The peak numbers of symptomatic infections, symptomatic inpatients, asymptomatic infections, and asymptomatic inpatients were 6401,10 583,27 015,and 41 123,respectively(Fig.4(e)).Doctor demand was 21 889 (Fig. 5(a)), nurse demand was 20 587 (Fig. 5(b)), and healthcare nursing worker demand was 4633 (Fig. 5(c)). Hospital bed demand was 3317 (Fig. 6(a)), isolation bed demand was 47 860 (Fig. 6(b)), ICU bed demand was 529 (Fig. 6(c)), ventilator demand was 974 (Fig. 6(d)), and oxygen machine demand was 2011 (Fig. 6(e)).
3.6. Scenario 6
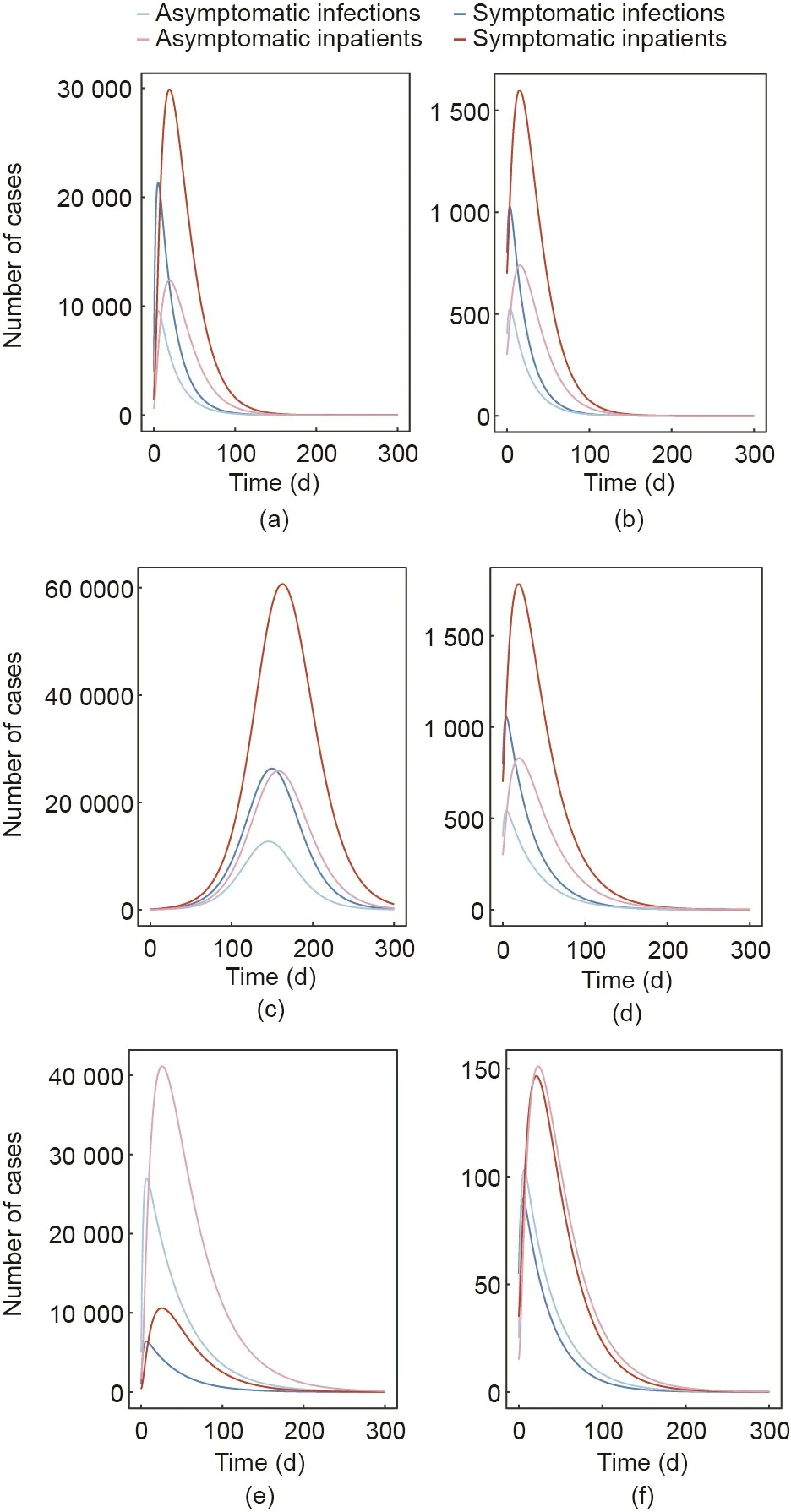
Fig. 4. The number of infections and inpatients under six scenarios. Panels (a–f)correspond to the number of asymptomatic and symptomatic infections and inpatients that coincided with the duration of the epidemic under scenarios 1–6.
As well as evaluating the numbers of healthcare workers and equipment resources needed, we also evaluated the total demand of PPE under six scenarios.The overall demand for PPE was related to the medical staff in different scenarios (Fig. 7; Table 2).
4. Discussion

Fig.5. Healthcare worker demand under the six scenarios,represented as different colored panels: (a) doctors; (b) nurses; and (c) nursing workers.
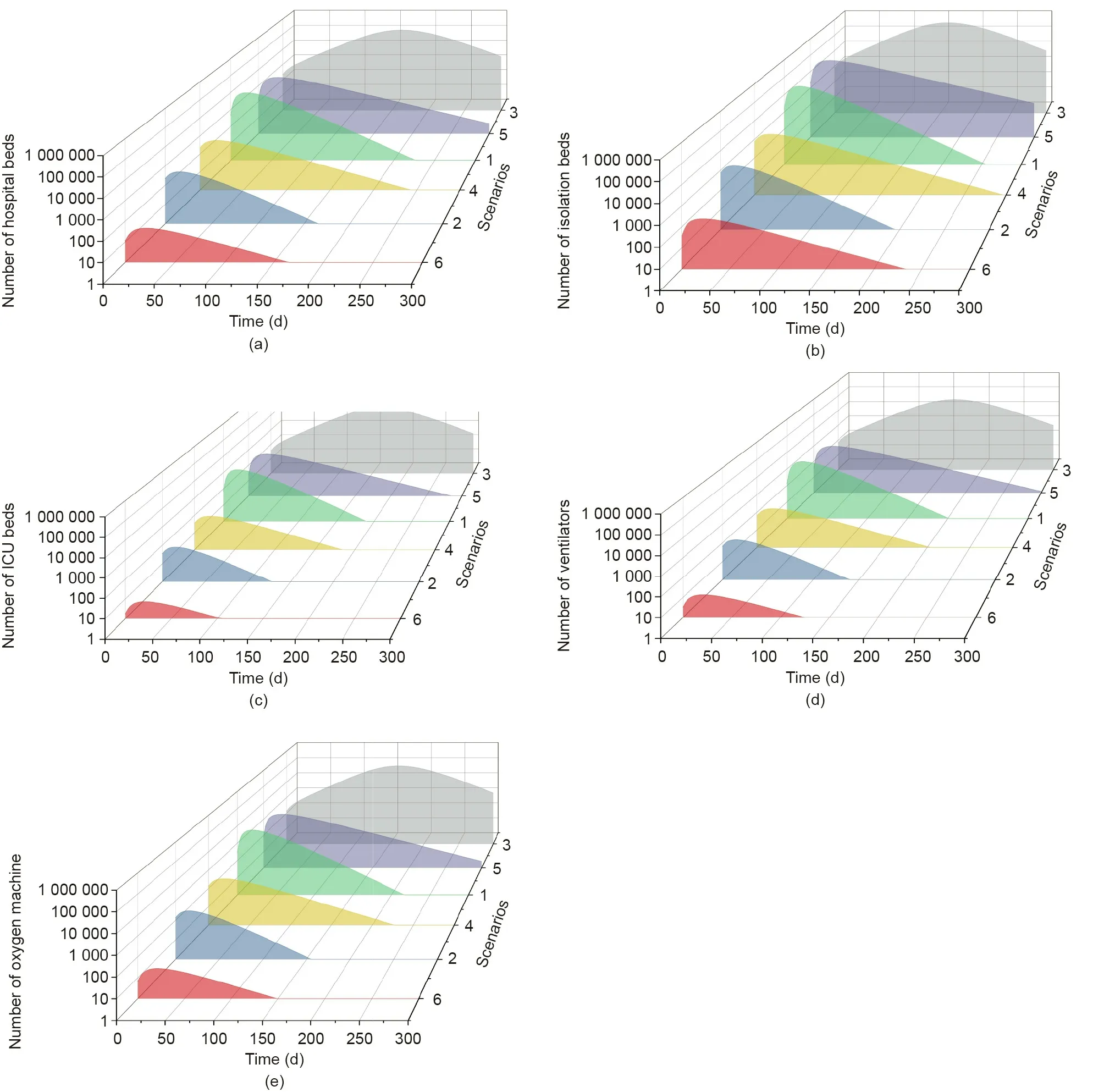
Fig. 6. Equipment demand (a) hospital beds, (b) isolation beds, (c) ICU beds, (d) ventilators, and (e) oxygen machines under six scenarios, represented as different colored panels.
Our six scenarios showed some important results.First,healthcare systems are clearly prone to overload during an emerging pandemic.In scenarios 2,4,and 6,our results showed no pressure on clinical demand. In scenarios 1 and 5, our findings indicated that the healthcare system would not collapse when improving monitoring and early warning capabilities and when implementing of NPIs similar to those used in Wuhan,accompanied with a specific coverage of the immunized population.However,in scenario 5,there would be unmet demand for clinical resources and the healthcare system would likely become paralyzed. Second,a more sensitive early-warning system can provide additional time to prepare for emergency management.Strict NPIs may be implemented only when 2000 people have been hospitalized or isolated.However, if these measures were adopted when only 900 people had been hospitalized or isolated, clinical resources in terms of bed occupancy may be reduced more than ten times. Care would be needed when the level of prevention and control is decreased or when the capacity to manage cases is insufficient.This situation would lead to many infected people not being hospitalized or isolated,and essential clinical resource demands would likely exceed those in scenarios 1 and 5. Third,strict NPIs are crucial in keeping clinical demand at a low level.When the effectiveness of NPIs was reduced from 0.8 to 0.5, doctor demand increased > 100 times.Fourth, vaccination can reduce the necessity for strict NPIs while maintaining a low level of clinical resource demand, which aids in resuming standard services during COVID-19. Transmission can also be stopped with a population immunized at a coverage rate of 50%and with less strict NPIs(50%effectiveness).Fifth,challenges concerning asymptomatic infections and clinical resources arise in relation to the number of asymptomatic cases and delays in their identification, which reduces the effectiveness of NPIs.Because patients who are asymptomatic remain infectious and need to be isolated, an increase in the proportion of those who are asymptomatic does not significantly reduce the demand for clinical resources. However, due to the occult nature of asymptomatic infections, NPIs only needs to maintain low levels of effectiveness.

Fig. 7. The six scenarios of epidemiological resource demand. Panels (a–f) refer to scenarios 1–6.
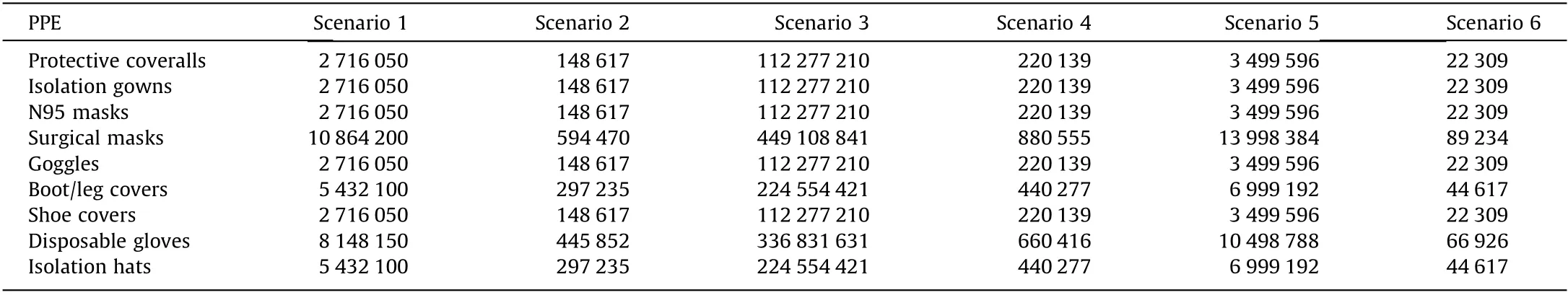
Table 2 PPE demand in six scenarios.
Our results highlight some points of concern.Two main factors can cause the collapse of a healthcare system due to COVID-19.First,a sharp increase in the number of cases within a short period of time results in a high concentration of hospital personnel,which leads to a high incidence of nosocomial infections. The equipment and facilities available in other departments cannot meet the required professional needs and hospitals may not be able to treat severe cases effectively.For every 10 million people,the number of registered doctors in hospitals in China in 2019 was 14 487.When comparing certain cities with populations of approximately 10 million in China, the total number of registered doctors and nurses was reported to be 43 100 and 57 700 in Wuhan [29],38 519 and 44 273 in Shenzhen [37], and 19 736 and 238 942 in Shijiazhuang[38],respectively.The numbers of Wuhan could meet the needs of scenario 3,even when differences in departments are not considered. The average number of registered doctors and nurses in an infectious disease hospital is 111 and 186, respectively, per 10 million in China, whereas in Shijiazhuang, the average number of registered doctors and nurses has been reported to be 225 and 328, respectively [28]. Neither in infectious disease hospitals in China generally, nor in Shijiazhuang, would the needs be met as outlined in the first five scenarios.In summary,different scenarios require a different subset of preparations. Scenario 1 requires infectious disease professionals, stockpiles of protective equipment, and the capacity to provide for early warnings. The most important requirements in scenarios 2 and 3 are to find alternative measures that are not overly detrimental to the economy.Scenarios 4–6 require increased attention to vaccine capacity and application.
Due to limited clinical human resources and equipment,adapting to a rapid increase in detection volumes is challenging, which then delays results in terms of diagnosis. Moreover, sufficient healthcare workers and relevant material cannot be easily provided in a short period of time. Specialist personnel, such as doctors in critical care, respiratory medicine, and infectious disease departments, become increasingly in demand and less available,and experience greater physical fatigue and psychological stress,in addition to facing the risk of infection during a pandemic,which may lead to the collapse of the medical system due to overload and poor management. Furthermore, medical systems can face other challenges such as issues in relation to nucleic acid testing and critical emergency treatment. However, when facing challenges regarding healthcare resources in short supply, such as shown in scenarios 1, 3, and 5, coping strategies from the following three perspectives could be adopted to facilitate an alternative supply of resources.First,prevention and preparation need to be the main priorities [39] in terms of ensuring vaccine reserves, vaccination coverage, and reducing the incidence rate, thereby reducing resource demands. Second, in terms of establishing a peace-time and epidemic-time convertible reserve model, healthcare workers in other departments could be trained as backup personnel in the fields of infectious diseases and respiratory medicine. Hotels and gymnasiums, for example, could be built according to Fangcang shelter hospital criteria, with the possibility of adapting them within a short period of time [6] when a pandemic occurs[14,35]. Ventilator and PPE reserves need to be considered to ensure that the surge in resource demands due to disease outbreaks can be adequately addressed [40]; therefore, due to the large demand in materials and the need to increase capacity reserves, adequate physical reserves are required. Third, improvements in technology, medical treatment, and in clinical examinations are required, for example, through providing more effective early warning systems.Big data have been used to establish a balanced allocation mechanism of clinical resources. Telemedicine should be implemented to reduce the demands on human resources, hospitalization time, and medical expenses [41]. The integration of relevant medical information can automatically generate diagnosis and treatment records, provide an informed alert,and improve the efficiency of diagnosis and treatment. The full benefits of science and technology need to be brought into play,such as using robots to complete mechanical work for basic nursing, disinfection, remote consultation, and recording information,for example, to obtain greater speed, enhanced precision, and a reduction in the demand for human resources.
This study provided theoretical support and a reference for emergency preparation of healthcare resources during the COVID-19 pandemic. The study framework not only considered the proportion of asymptomatic infections[42]in terms of healthcare resources and the effects of an immunized population, but also considered the effectiveness of NPIs. A basic SEIR model has previously been used to predict the spread of COVID-19 in the early stages [3,43]. We extended the model to a SEIHR transmission dynamics model, which was found to be methodologically robust.When considering the latency time of case reports,our method can be used to quickly and continuously assess clinical demand and provide guidance for resource input and allocation strategies in terms of prevention and control of resource production.
This study had several limitations.First,many factors affect the assessment of healthcare resource demands,such as cultural background, regional emergency response capabilities, medical support, ethical issues, and other more complex factors. Therefore,when preparing healthcare resources based on the results of this study,it would also be necessary to closely evaluate the actual situation in the assessed area. Second, our study provided no evidence concerning infectivity, the infectious period, and the proportion of asymptomatic infections that could verify the accuracy of our results, which is a limitation given these are prone to change due to the passage and mutation of the virus. Third, older adults are known to be more vulnerable to COVID-19,which might lead to a heavier disease burden and clinical resource demand for resources in a city with an aging population. As knowledge and understanding of COVID-19 increases, population age structures could be considered in the model through the use of an age-stratified model, which could be conducted in future studies.Furthermore, we did not consider the efficiency period following vaccination, which may have an effect on the range of the immunized population. Finally, the scenarios data simulated using the model cannot fully reflect a real-world situation.
5. Conclusions
Regions with differing economic development levels, population sizes,and prevention and control capabilities should estimate clinical resource demands during emergencies as soon as possible,and prepare healthcare resources in advance for possible epidemic rebounds and outbreaks. Acute respiratory infections can impose an extra load on medical systems; therefore, encouraging people to have influenza, pneumococcal, and other vaccinations can alleviate and reduce the need for healthcare resources during the COVID-19 pandemic.When responding to a situation of short supply in healthcare resources such as that occurring during the COVID-19 pandemic, use of the window period to expand healthcare resources and make timely adjustments to existing strategies is recommended.
Acknowledgements
The co-authors would extend their heartfelt thanks to Ling Yan(DAO) research technical team colleagues, Chen Chen, Changkai He,Zhichen Yang,Zhiyuan Sun,Zhengyang Sun,for their technical support.This study was supported by the following fundings:Chinese Academy of Medical Sciences (CAMS) Innovation Fund for Medical Sciences (2020-I2M-1-001, 2020-I2M-2-015, and 2016-I2M-1-014), and National Social Science Fund of China(20&ZD201).
Compliance with ethics guidelines
Ting Zhang,Qing Wang,Zhiwei Leng,Yuan Yang,Jin Yang,Fangyuan Chen, Mengmeng Jia, Xingxing Zhang, Weiran Qi, Yunshao Xu, Siya Chen, Peixi Dai, Libing Ma, Luzhao Feng, and Weizhong Yang declare that they have no conflict of interest or financial conflicts to disclose.
杂志排行
Engineering的其它文章
- COVID-19 Vaccine Allocation: Modeling Health Outcomes and Equity Implications of Alternative Strategies
- Fast Marching Method for Microseismic Source Location in Cavern-Containing Rockmass: Performance Analysis and Engineering Application
- Non-Communicable Diseases During the COVID-19 Pandemic and Beyond
- Next Steps for Efficacy Evaluation in Clinical Trials of COVID-19 Vaccines
- Facilities for Centralized Isolation and Quarantine for the Observation and Treatment of Patients with COVID-19
- Temporal Profiles of Antibody Responses, Cytokines, and Survival of COVID-19 Patients: A Retrospective Cohort
