Nurses’ experiences in voluntary error reporting:An integrative literature review
2021-12-11MingWeiJeffreyWooMarkJamesAvery
Ming Wei Jeffrey Woo ,Mark James Avery
a School of Health &Social Sciences,Nanyang Polytechnic,Singapore
b Department of Health Services Management,School of Medicine,Griffith University,Brisbane,Australia
Keywords:Experience Medical errors Nurses Voluntary error reporting Patient safety
ABSTRACT Objective:This integrative review aimed to examine and understand nurses’ experiences of voluntary error reporting (VER) and elucidate factors underlying their decision to engage in VER.Method:This is an integrative review based on Whittemore &Knafl five-stage framework.A systematic search guided by the PRISMA 2020 approach was performed on four electronic databases:CINAHL,Medline (PubMed),Scopus,and Embase.Peer-reviewed articles published in the English language from January 2010 to December 2020 were retrieved and screened for relevancy.Results:Totally 31 papers were included in this review following the quality appraisal.A constant comparative approach was used to synthesize findings of eligible studies to report nurses'experiences of VER represented by three major themes:nurses' beliefs,behavior,and sentiments towards VER;nurses'perceived enabling factors of VER and nurses'perceived inhibiting factors of VER.Findings of this review revealed that nurses’ experiences of VER were less than ideal.Firstly,these negative experiences were accounted for by the interplays of factors that influenced their attitudes,perceptions,emotions,and practices.Additionally,their negative experiences were underpinned by a spectrum of system,administrative and organizational factors that focuses on attributing the error to human failure characterized by an unsupportive,blaming,and punitive approach to error management.Conclusion:Findings of this review add to the body of knowledge to inform on the areas of focus to guide nursing management perspectives to strengthen institutional efforts to improve nurses' recognition,reception,and contribution towards VER.It is recommended that nursing leaders prioritize and invest in strategies to enhance existing institutional error management approaches to establish a just and open patient safety culture that would promote positivity in nurses’ overall experiences towards VER.
What is known?
· Error reporting facilitates analysis of factors responsible for the causation of nursing error and delineates one essential step to drive robust patient safety culture and improve nursing care quality.
· Despite a plethora of safety literature had emphasized the significance of error reporting,evidence had further suggested that nurses often underreport error.
What is new?
· This review provides insights on the spectrum and interplay of issues surrounding nurses'attitudes,perceptions,practices,and emotions and their perceived enabling and inhibiting factors of error reporting that would contribute to a holistic understanding of nurses' overall experiences towards voluntary error reporting (VER).
· The findings of this review delineate the need to drive organizational reforms to achieve a more optimized patient safety culture and better institutional error management outcomes.This calls for the collaborative efforts of nursing leaders at various levels to prioritize and invest in strategies to refine existing institutional policies,practices,processes,and communication approaches to boost nurses' commitment towards VER and improve the overall error reporting systems.
1.Introduction
Medical errors denote a severe public health implication.The WHO defines a medical error as an event caused by deviations from the standard care that would result in a patient experiencing harm or risk of injury [1].To set the context of this paper,the term‘medical error’ from the nursing perspective comprises a broad spectrum of adverse clinical incidents associated with the delivery of care by nurses that fall below reasonable standards.They include but are not limited to the following:erroneous administration of medications,falls,and infections[2].Medical errors can be harmful and may lead to profound health implications for patients,such as permanent incapacitation and death [3].Such deleterious consequences may subject errant healthcare professionals to medicolegal disputes and litigation and their institutions to liabilities for compensations owing to medical negligence [4].Costs incurred by medical errors contribute to a significant drain on healthcare resources and compound the financial burden on the affected healthcare institutions and governments.This is evident in the cost of up to GBP 2 billion incurred by the National Health Services in the United Kingdom in addressing such complications[5].Likewise,the United States has also reported incurring an estimated US$ 50 billion to reduce the occurrence of medical errors [6,7].Nonetheless,studies had shown that 48%-70% of errors could be averted[8,9],for which a feasible solution is a dynamic error reporting by health practitioners [10].
Error reporting is critical,given its central role in investigating and analyzing root causes of errors,the insights from which are envisioned to mitigate recurrences due to awareness and the resultant changes that took place [11].From the organization's perspective,error reporting permits the diagnoses and identification of any underlying vulnerabilities embedded in the healthcare systems to systematically develop strategies to address any active and latent failures [12].From the individual nurse's perspective,error reporting facilitates valuable learning through retrospective investigations and reflections from past mistakes to improve their prospective clinical practices [13].Contemporary safety literature has copiously examined the aspect of preventable adverse medical incidents;given the resultant heightened awareness among healthcare professionals and patients,the need to improve the delivery of nursing care and patient safety is imperative.Establishing a robust error reporting system is fundamental to continuous quality improvement that supports a culture of safety in healthcare.
Nurses comprise the largest workforce in any healthcare organization.While highly involved in medical errors(due to actions of self or others),nurses are also pivotal to reporting and managing such errors as prominent stakeholders.Studies have argued that any practicing nurses,regardless of their level of knowledge and precision,are bound to have committed medical mistakes at one point or another in their nursing career [14,15].Consistent voluntary error reporting(VER)by healthcare professionals is integral to a robust institutional error-management system[16].Many studies have revealed that 50%-96%of medical errors were underreported by nurses [12,17,18].Given the importance of error reporting to promote a robust culture of safety,the lack of commitment among nurses would result in their losses of valuable learning opportunities to improve their nursing care.
The term voluntary error reporting(VER)indicates an individual nurse's accordance,commitment,and intention to disclose and report a medical error openly [6].Nurses' perceptions of error reporting have been shown to influence their behavior leading to actual translation to VER[19-21].The recent literature review has focused on barriers of error reporting confronted by nurses[22-24].Accordingly,this integrative review seeks to expand the scope of such existing investigation to gain a holistic understanding of nurses' experiences of VER from their perspectives with personal,professional,psychological,and organizational considerations.This review has adopted the conceptual model ‘Conceptual Model for Disclosure of Medical Errors’ by Fein et al.[25],whose definition of nurses' experiences in VER were underpinned by the interplay of factors concerning their attitudes,perceptions,feelings,and practice of error reporting,as well as various enabling and hindering factors in influencing their commitment in VER.Examining these areas makes up the totality of understanding of nurses'experiences of VER [25],and this will guide the approach of presentation of findings of this review.This integrative review aims to understand nurses' experiences in VER.Such insights would enhance professional nursing practices by informing strategies to foster a safety-centric culture and optimize error management.
2.Methods
This paper presents an integrative review that examines nurses’experiences in error reporting.The methodological approach by Whittemore and Knafl adopted in this review comprised five sequential stages:1) problem identification,2) systematic literature search,3)data evaluation,4)data analysis,and 5)presentation of findings[26].The rationales underlying this choice were twofold.Firstly,the approach enabled the amalgamation of findings from studies of different research designs and methodologies to draw conclusions on established knowledge areas and identify any research gap of the given topic.Secondly,the systematic search,appraisal,and synthesis of the body of literature add rigor to the review [27].
2.1.Problem identification
The research question underpinning this integrative review would be:What are nurses’ experiences towards VER?
2.2.Literature search
A systematic search was performed across four electronic databases:Cumulative Index to Nursing and Allied Health Literature(CINHAL) (Ebsco),Medline (PubMed),Scopus,and Embase to retrieve papers published between January 2010 to December 2020.Firstly,the rationales behind this timeline are due to a lack of studies focusing on electronic error reporting compared to paper reporting systems before 2010.Hence,this ensures the presentation of evidence that reflects contemporary practices of error reporting [28,29].Secondly,the inclusion of papers towards 2020 served to provide the production of current evidence.The three key concepts underpinning the search strategy were error,reporting,and nurses.The final search date of the databases fell on 4th January 2021.The keywords utilized were a nurse,and the subject heading “error” and “reporting” were searched separately.Search interrogation techniques were deployed with simultaneous use of the Boolean operator (AND/OR) and truncation (wildcard) (*) to merge exploded terms to broaden the search to derive a more comprehensive result.The search utilized a combination of terms such as “nurs*” OR “nurse attitude” OR “nurse experience” AND“medication error*” OR “nursing error*” OR “medical error*” AND“voluntary report*” OR “incident report*” OR “report*” OR“disclose*.”
Publications were included in this integrative review if they were peer-reviewed original research in English on nurses' perceptions,attitudes,and barriers in error reporting.Conversely,publications were excluded if the focus of error reporting was on allied healthcare professionals such as physicians,pharmacists,and nursing students (for those investigating perceptions of both nurses and other professionals,they were excluded if they had not compartmentalized the findings for nurses).The exclusion was further applied to articles that reported on the causes and classification of medical errors,incident reporting of non-sentinel events,legal and ethical perspectives of medical errors,evaluation of error-reporting systems,and nurses’perceptions of cultural safety general rather than error reporting.Lastly,publications were also excluded if they were pilot studies,literature reviews,discussion papers,opinions,editorial papers,commentaries,conference reports,and grey literature (dissertation).
The total results of four database searches were 1,276 papers.Hand-search was performed on the reference lists of included articles to retrieve additional 17 papers for screening,considering the possibility of computerized databases is yielding 50% of eligible studies due to inconsistent search terminology [26].With the support of Endnote (Clarivate Analytics) reference management software,screening of titles and abstracts of papers retrieved from database search were performed independently by both authors(MWJW and MJA),followed by assessing the full texts of each paper against the inclusion criteria.A systematic review process had resulted in the elimination of duplications and irrelevant papers against their titles and abstracts (n=1,138),hence retaining 155 studies.The suitability and relevancy of these articles were then checked by full-text reading against both the inclusion and exclusion criteria leading to the elimination of 122 papers.The final stage sees all 33 papers undergoing thorough methodological appraisal.The PRISMA 2020 guidelines underpin the study selection process(Fig.1) [30].
2.3.Data evaluation
To objectively rate the methodological quality of each paper,the Mixed Methods Appraisal Tool(MMAT)2011 by Pluye et al.[31]was used,comprising five categories of scores:very low(0%),low(25%),moderate(50%),high(75%),and very high(100%).The MMAT 2011 facilitated the quality appraisal of each paper against its stipulated assessment criteria according to the study's methodological approach;this involved converting the outcome of the assessment into a total score to consider its eligibility for inclusion [31].Calculation of the score for MMAT 2011 was based on the number of criteria met by an individual paper divided by the total number of the assessment criteria assigned for that paper's methodology[31].Leblanc et al.had recommended excluding studies with low quality(below 25%) [32].Both authors (MWJW and MJA) had independently appraised each paper to eliminate any potential biases.Any discrepancies to the assigned scores were discussed,and the consensus to the final score of each paper was reached between both authors,leading to the elimination of two papers.
2.4.Data analysis
Thematic analysis was chosen for an integrative review due to the heterogeneity of the included papers where meta-analysis would not be appropriate [26,27].Data analysis consists of four stages:data reduction,data display,comparison,conclusion drawing,and verification [26,33].Firstly,the data of each study were extracted and succinctly presented into a comprehensive review matrix(summary table of evidence)which consists of several domains.The summary tables of evidence were classified according to research design,as shown in Table 1 (quantitative studies) and Table 2 (qualitative and mixed-method studies).
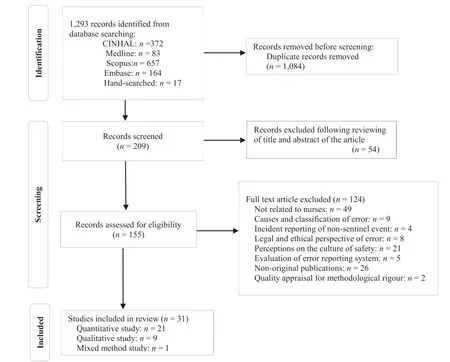
Fig.1.PRISMA flow diagram for search strategy.
The constant comparative method was used to iteratively compare,classify and identify themes,patterns,and relationships across all included studies.This is followed by assigning labels(themes) to the collected data to attach meaning that closely reflected the collection of similar findings,a process known as coding.This is to inductively construct unifying themes in preparing for narrative integration of results to answer the research question of this review [33].The first author (MWJW) performed the extraction,analysis,and coding of the data,while the second author(MJA) checked to verify its accuracy.Discussions between both authors(MWJW)and(MJA)were held to validate the conclusion by verifying from primary sources and clarifying any discrepancies to derive mutual consensus.
2.5.Presentation of findings
In the final stage of this review,findings are presented to address the research question underpinning this integrative review.
3.Results
There were 31 eligible studies included in this review.They consist of 21 quantitative studies,nine qualitative studies,and one mixed-methods study.Descriptive cross-sectional survey design underpins all quantitative papers (n=21).The sample size ranged between 71 and 1,380 nurses,with all of them used questionnaire to collect their data.Of all qualitative papers,the majority were descriptive qualitative design (n=7),while the remaining were grounded theory design (n=1) and case study design (n=1).The sample size ranged from 10 to 115 nurses in all qualitative studies.The majority (n=5) used semi-structured interviews to collect their data.A detailed description of each study can be found in both Tables 1 and 2,respectively.
3.1.Identified themes
Thematic analysis of the findings of 31 papers contributes to the emergence of three major themes:1)nurses'beliefs,behavior,and sentiments towards VER,2) nurses' perceived enabling factors of VER,and 3) nurses’ perceived inhibiting factors of VER.Except for theme 2,each theme would consist of various sub-themes(Table 3).
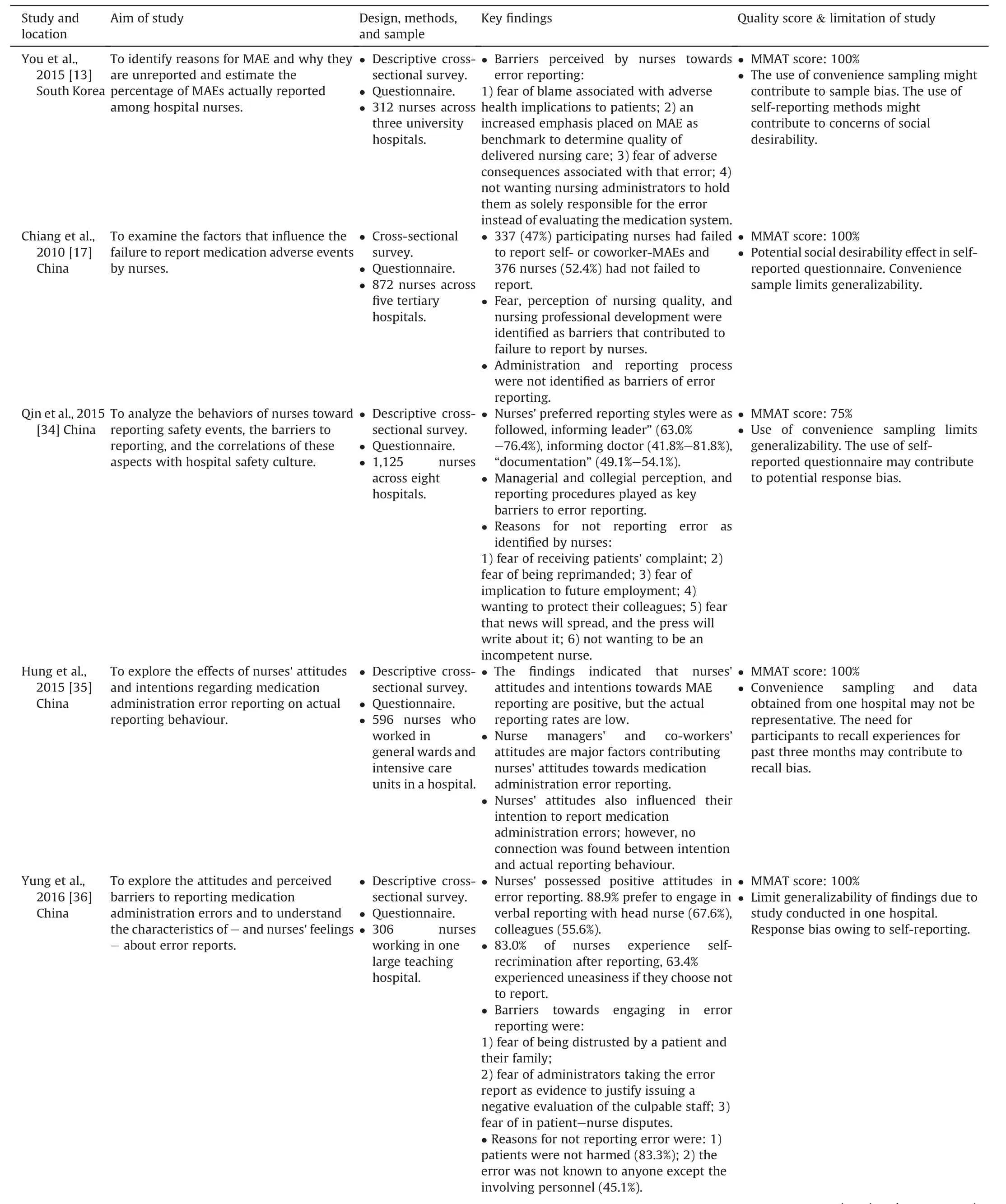
Table 1Summary table of evidence for quantitative studies (n=21).
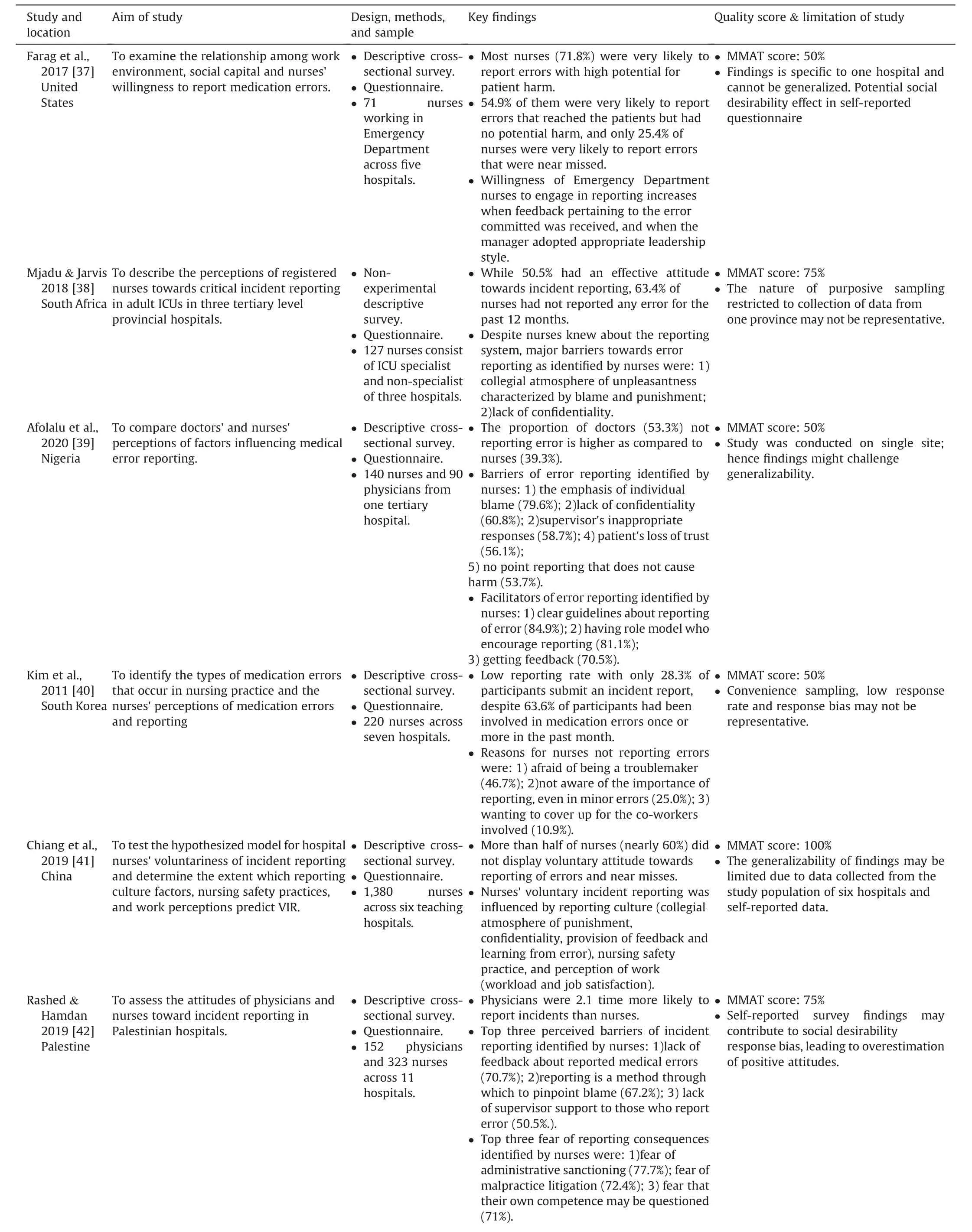
Table 1 (continued)
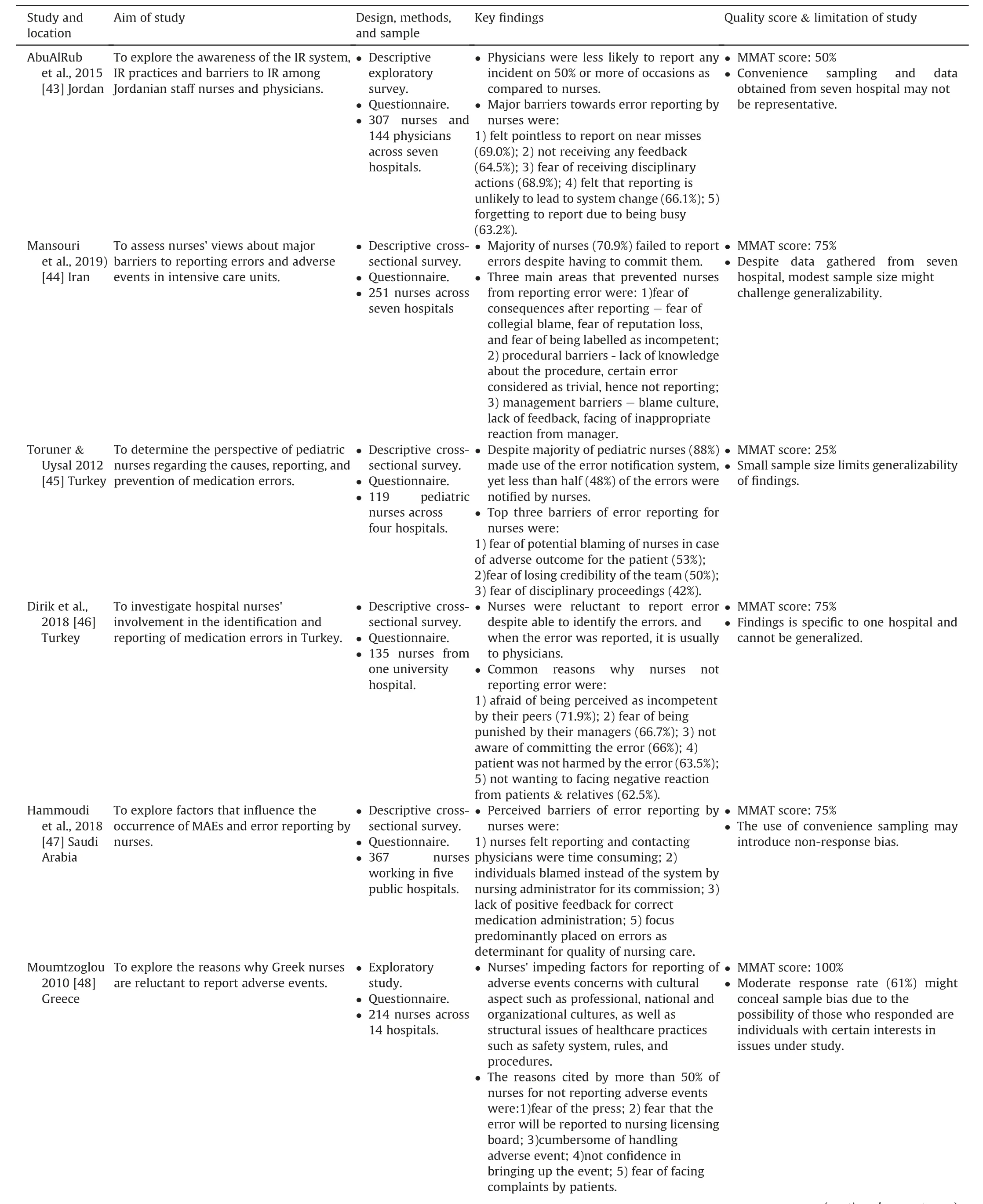
Table 1 (continued)
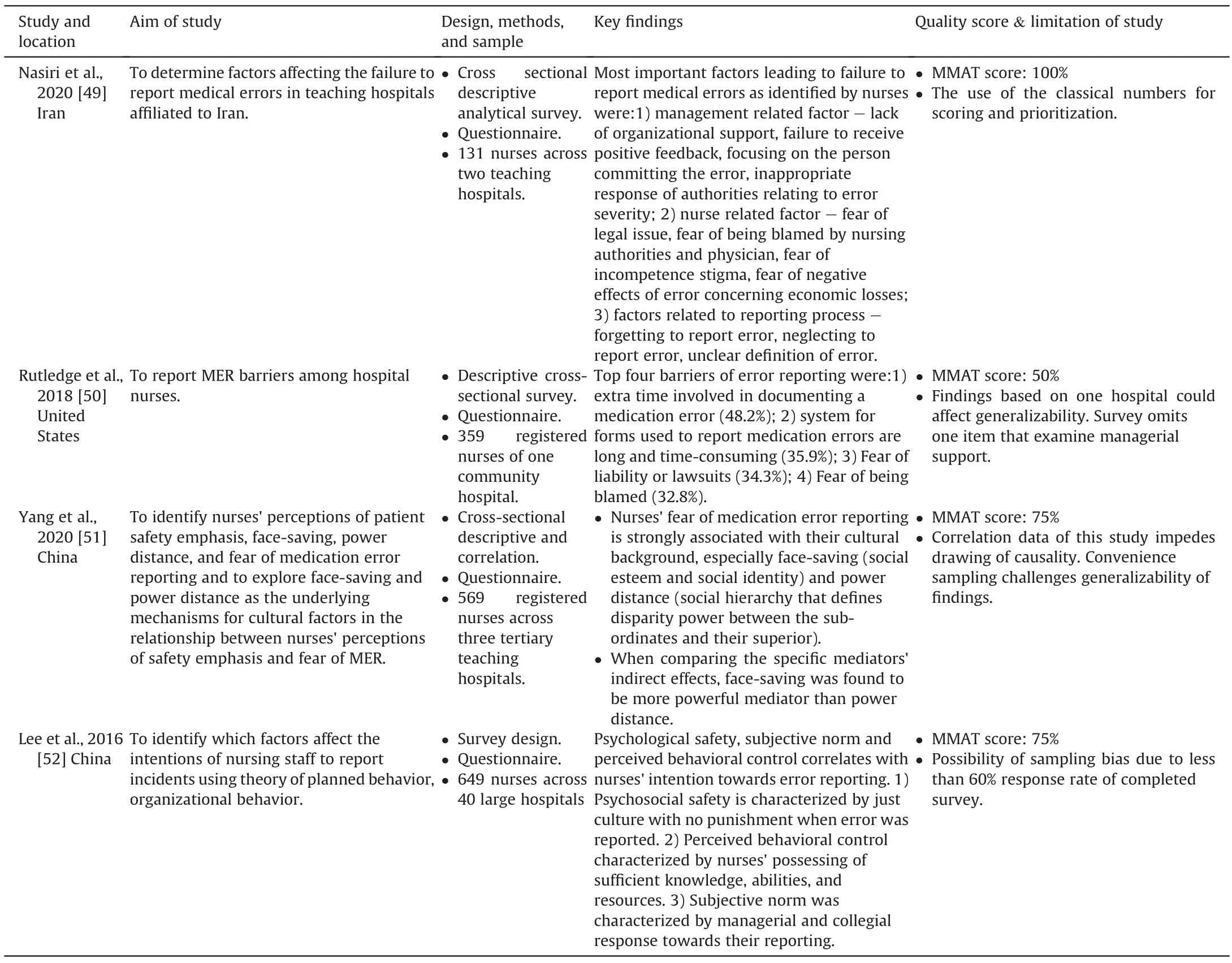
Table 1 (continued)
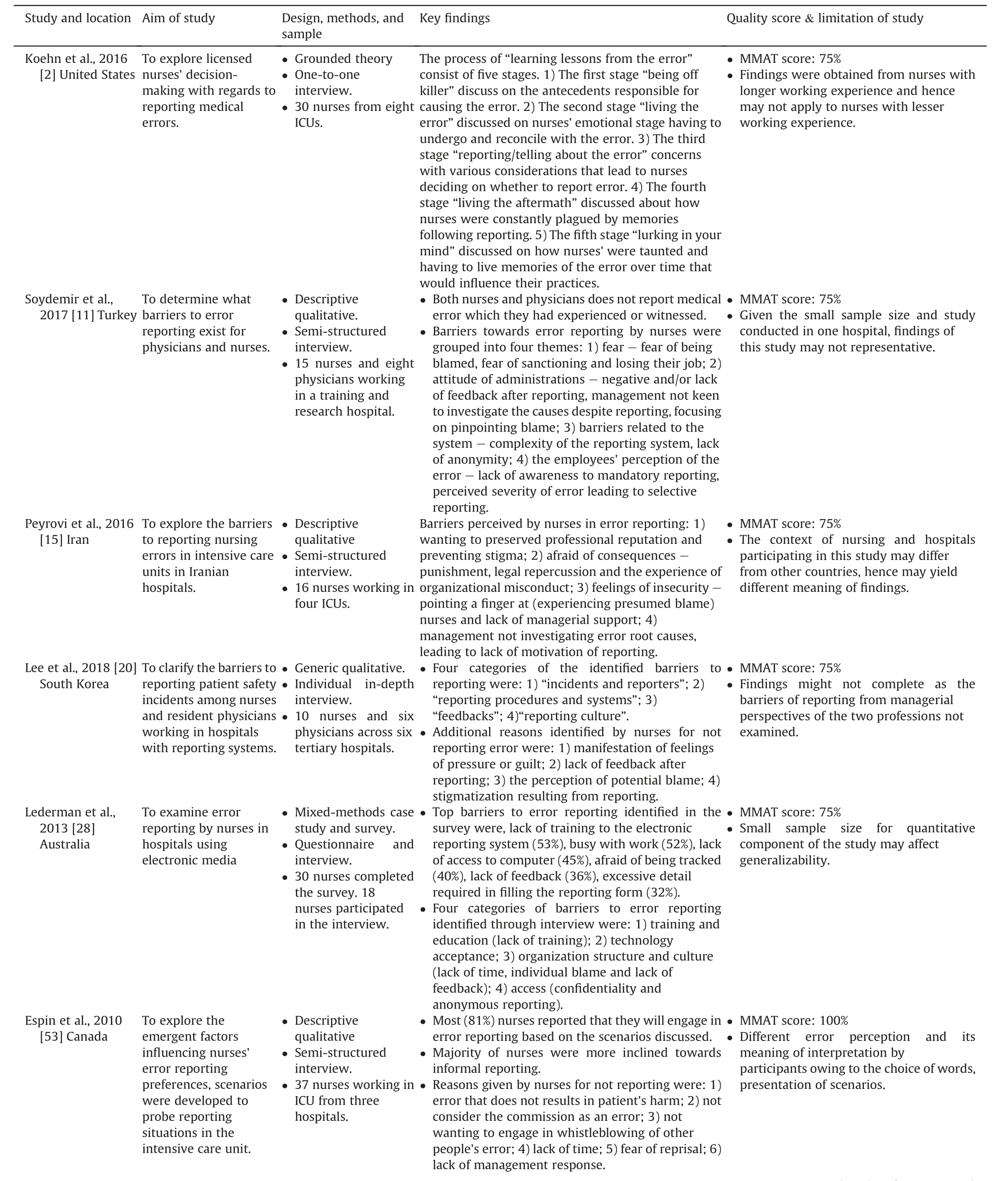
Table 2 Summary table of evidence for qualitative and mixed method studies (n=10).
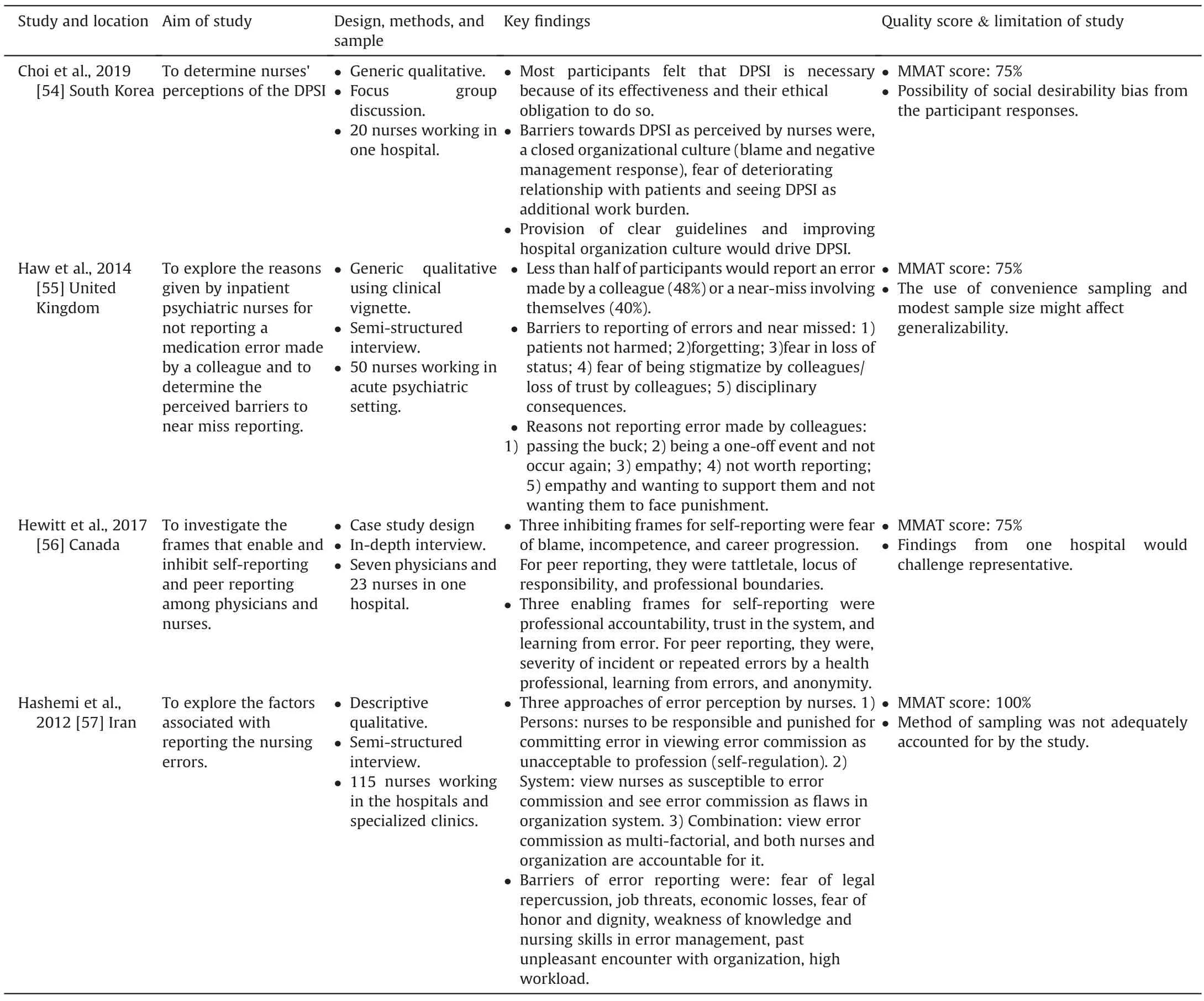
Table 2 (continued)
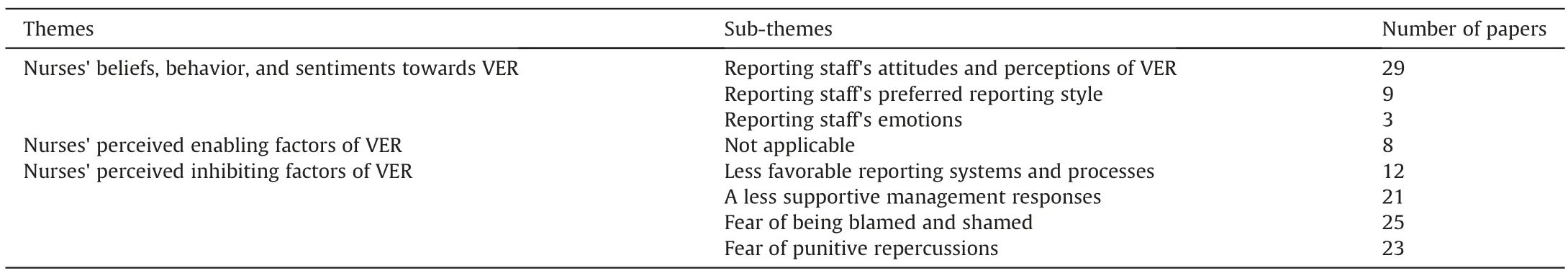
Table 3 Emerging themes and sub-themes.
3.2.Nurses’ beliefs,behavior,and sentiments towards VER
This first theme,“nurses' beliefs,behavior,and sentiments towards VER,” investigates nurses' perspectives and their practice and feelings surrounding error reporting that underpinned their experiences towards VER.Three sub-themes represent this theme:reporting staff's attitudes and perceptions of VER,reporting staff's preferred reporting style,reporting staff's emotions.
3.2.1.Reporting staff's attitudes and perceptions of VER
A plethora of studies (n=12) that examined nurses' attitudes towards VER had yielded mixed findings.Eight studies had revealed that nurses possess a positive attitude towards VER[34-39,53,54],while four studies had reported otherwise[40-42,55].Consistent with this finding,of the four studies comparing nurses'frequency of error reporting to other healthcare professionals such as physicians,three studies revealed that nurses generally had a higher error reporting rate than the physicians[39,43,56].In contrast,one has reported otherwise [42].Despite this positive finding,approximately half of the quantitative studies(n=9) found that more than 50% of nurses did not report errors[34,35,38,40-42,44-46,55].This delineates the incongruity between nurses’ attitude and their actual action of VER.
Five studies have examined how nurses’ positive attitudes towards VER were centered around their commitment to professional accountabilities.A strong ethical obligation towards VER has been demonstrated by nurses,who considered error reporting part of their responsibility[42,54,56,57].The underlying impetus has been reported to be their upholding of patient safety,accountability,and the provision of quality nursing care as part of their profession[42,57].Nonetheless,such professional commitment could be a source of frustration to nurses.The interplay between nurses and other healthcare professionals could be frustrating when they identified that physicians might not hold themselves to similar standards in accountability for error reporting [42].Conversely,studies(n=2)revealed how nurses tended to display less favorable attitudes and were less inclined to report errors committed by other professionals,given that their accountability for their actions did not fall within the locus of nursing responsibilities [15,56].
Nurses' unfavorable attitude towards VER owing to their limitations was also observed.The need to shoulder substantial work commitments had led to nurses placing lesser emphasis on VER.This was demonstrated by nine studies that nurses were burdened by greater responsibilities such as not only high patient acuity and volume,but also administrative duties,with the expectation that they had to complete them within their working hours had led them to view VER as subservient to these competing tasks[20,28,39,43,45,47,48,53].Given their competing nursing duties,three studies also revealed how this led to nurses perceiving the need for VER to be of lesser priority,resulting in them subsequently forgetting VER due to procrastination [43,49,55].Concomitantly,the relationship between nurses'deficiency in knowledge and VER was also examined.Four studies have revealed how nurses'attitude concerning the unintentional omission of error reporting was due to their lack of knowledge to perceive and recognize events that constituted errors [44,46,49,55].Likewise,it was reported that some nurses have not engaged in VER because of their perception of specific errors as trivialities [2,43,44] or because of their ignorance of the occurrence of the errors [2,46,55].Lastly,nurses’ less favorable attitude towards VER was also reported because of their perception of not wanting to be seen by their colleagues for being a troublemaker for causing the error and instigating error reporting[40].
Four other findings were noteworthy.Firstly,nurses'perception of error severity was noted to influence their attitude and actions towards VER,as identified across the studies (n=7).They were likelier to report more severe errors inflicting more severe harm on their patients[34,37,39,44,46,50,57].Nurses had reasoned that less severe errors needed no reporting,given their perceived relative innocuousness [2,11,36,46,55,57].Secondly,errors were also noted to affect nurses’ reporting attitude,as identified across the studies(n=6).They were less likely to report near-miss events than actual errors,justifying this on the timely interception of the near-miss events and the absence of actual harm to patients[11,20,37,43,44,55].Thirdly,nurses were also less likely to commit to reporting when the errors were known exclusively to themselves[36,50].
Additionally,negative perceptions among nurses leading to their inaction in VER were also reported by five studies.These perceptions were illustrated by their lack of realization of the significance of reporting.The resultant view that it would infringe upon the quality time for patient care also contributes to their negative attitude towards and hence their actual action of VER[11,17,20,40,55].
3.2.2.Reporting staff's preferred reporting style
Investigating nurses'preferred methods in error reporting in the studies(n=9)has revealed the critical roles of the mode of reporting and hierarchy.On the reporting mode,nurses have expressed their tendency to engage in informal error reporting,i.e.,orally reporting to their colleagues and immediate supervisors in preference to formal writing[2,28,36,45,46,53].The reasons were twofold.Firstly,nurses wished to seek their colleagues'and supervisor's clarification on the definition of an error and their support to resolve it [2,53].Secondly,they feared leaving any documentary evidence that would incriminate them to the errors[20,28,36].
Similarly,two studies from Asia disclosed how nurses were more inclined to verbally inform their management,such as shift leaders,nurse managers,or head nurses who would finalize whether formal reporting be required [34,36].On hierarchy,two other studies have revealed how nurses were expected to seek the approval of their nursing leaders before decisions on reporting and consult them in vetting incident reports before final submission[20,51].Underlying this observation were traditional Asiatic values inherent to the hierarchical chain of command,which had to be obeyed by junior nurses by abiding by their senior nurses' instructions and respecting their decision-making capacity [36,51].Yang et al.coined the term ‘power distance’,implying the nurses'need to show respect to their higher authority in the hierarchical structure in nursing owing to the disparity of power [51].These findings thus suggested that hierarchy could profoundly influence nurses' effort towards VER.
3.2.3.Reporting staff's emotions
Three studies have investigated nurses’experiences during and after error reporting.Yung et al.[36]revealed that,when deciding on the appropriateness of their error-reporting,nurses were confronted by negative emotions such as regret,fear,and restlessness:the majority expressed self-recrimination following their decision to do so,whereas others said anxiety following their decision of not to report.Lee et al.collaboratively reported how nurses would experience constant self-reproach and guilt following error reporting [20].
In their grounded theory study,Koehn et al.used themes to insightfully delineate the trajectory of feelings faced by nurses surrounding their decision to report their errors [2].Under the theme of‘living the error,’nurses revealed their astonishment upon being informed that their actions had led to errors [2].With their further clarification of the error causation,their initial fear and distress were soon followed by anger,self-blame,and selfdegrading of their worth in their profession that could last for days[2].This would be followed by the following theme,‘reporting or telling the error,’ which implied that nurses would perform the action of VER based on their chosen decisions,regardless of whether reporting was made,upon considering the benefits and repercussions of consequences of their activities of error reporting[2].Under the next theme,‘living the aftermath,’ nurses lamented being constantly tormented by the aftermath of the error reporting.Such ruminations served as a painful lesson to mitigate future recurrences [2].Under the final theme of ‘lurking in your mind,’nurses reported how negative memories of their lapses would linger throughout their nursing career and serve as an impetus to influence their practice[2].
3.3.Nurses’ perceived enabling factors of VER
The second theme on“nurses'perceived enabling factors of VER”will examine various facilitating factors that would incentivize nurses to commit to VER.Eight studies have examined the factors that would motivate nurses to engage in VER.Lee et al.[52] have posited that nurses'positive attitude and their actual action of VER were governed by the multifactorial considerations underpinned by the theory of planned behavior(TPB).Under the first domain of‘perceived behavioral control’of the TPB,the authors delineated the need for nurses to possess adequate knowledge,abilities,and resources to drive their commitment to VER [52].The second domain of ‘subjective norms’revealed that nurses desired and valued receiving their supervisors'support and the opportunity to open discussion of errors [52].The third domain of‘psychological safety’highlighted their need for their organizations to foster a safe working environment in tandem with a just and open culture,under which they could report errors without fears of repercussions[52].This concurred with Choi et al.[54],who revealed how clear institutional guidelines and positive organizational culture facilitate VER by nurses.
Other factors have also been elucidated.Hewitt et al.have identified three factors that would enhance nurses' receptiveness to VER [56].This receptiveness was centered upon three beliefs:firstly,one in need for professional accountability for their actions;secondly,trust in their organizations' commitment to a nonblaming policy and,thirdly,reporting would drive their constructive learning of the errors [56].Hashemi et al.[57] have corroboratively expanded the list of motivators to include the call for a supportive work environment where physicians and authority would not evade their responsibility and thus leave nurses alone to deal with errors.Afolalu et al.[39]revealed positive organizational factors,such as clarity in defining errors,clear guidelines on reporting,and their leaders as role models that would incentivize nurses to commit to VER.Lastly,the provision of feedback[37,39,42] and supervisory support [38] in positively influencing nurses’ commitment to VER have also been affirmed.
3.4.Nurses’ perceived inhibiting factors of VER
This third theme,“nurses' perceived inhibiting factors in VER,”will examine various hindering factors that would impede nurses'action in VER.This theme is represented by four sub-themes:less favorable reporting systems and processes;less supportive management responses;fear of being blamed and shamed;and fear of punitive repercussions.
3.4.1.Less favorable reporting systems and processes
Studies (n=10) have revealed how nurses’ attitude and commitment to VER could be dictated by processes and policies underpinning the organizational error-reporting system.Nurses perceived error reporting as time-consuming owing to the tedium of lodging incident reports that would add to their existing heavy workload [11,20,28,48,50,55,57].Nurses perceived the error reporting process to be cumbersome,and this was hereby explained in three instances.Firstly,nurses highlighted that significant efforts were warranted in the aftermath of error reporting:they would be overwhelmed by the need to coordinate with other healthcare professionals and manage the clinical sequelae arising from that error [2,47].Secondly,they underlined the difficulty in locating hardcopy forms for incident reporting [28,55].Thirdly,they emphasized the difficulty in navigating the complex platform[11,28,39].Lederman et al.further revealed how nurses who had trouble coping with technology acceptance had attributed their heightened challenge to lack of support by their institution to organize relevant training initiatives to enhance their familiarity in electronic error reporting systems[28].
The lack of reassurance for reporting staff's anonymity has been found as a limitation of the institutional error-reporting system,as identified across five studies.Firstly,Lee et al.highlighted nurses'concern with identity exposure in error reporting,undermining their willingness to engage in VER in the future[20].Echoing these,four other studies have further revealed how nurses would yearn for the opportunity to engage in anonymous reporting.This would lessen their burden of responsibility and drive their commitment to VER [28,38,56,57].
3.4.2.A less supportive management responses
Studies (n=21) have examined the relationship between nurses'past experiences and the management's responses to their attitude of error reporting and their commitment to VER in the future.Such undesirable responses were characterized the lack of feedback by their nursing supervisors [2,11,20,28,42-44,46,48,50],or,if given,the mostly negative nature of such feedback[11,39,46,47,49].The significance of feedback provision to nurses'intention in VER was further affirmed by Chiang et al.[41].Nurses further asserted how they would value receiving constructive feedback on enhancing patient safety because this would enable them to learn from past mistakes to improve their future practices[38,42,56].
Conversely,nurses' commitment to VER in the future could be undermined by their organizations' nonchalance:the lack of commitment to investigating root causes of errors after error reporting [15,53],and the lack of action to address flaws in the existing system [15,43].Additionally,an overemphasis on error occurrence as a critical quality indicator to appraise nurses’ performance further demotivated them towards VER for fear of repercussions [11,13,17,47].Five studies have also revealed how nurses faced immense negative responses from their nursing leaders that are incommensurate with the severity of their errors following their reporting.This had further discouraged them from engaging in future VER [39,44,49,54,57].
3.4.3.Fear of being blamed and shamed
The consensus was unanimous among studies (n=20) that emphasizing individual blame for error causation would serve as a barrier to VER by nurses.Nurses highlighted fear of blame by their colleagues,and/or physicians for being responsible of causing the error following VER [2,11,13,15,20,28,36,38,39,42,44-47,57],and this would also negatively influence their attitude towards VER[35].Nurses asserted that the disapproving outlook by the middle and senior management towards the occurrence of errors:such an outlook meant that the post-incident focus was on assigning blame and holding them entirely responsible,instead of acknowledging limitations and fallacies of existing work processes that might have caused the errors [2,11,13,39,46,47,49,56].Additionally,the literature revealed how the intensity of blame would be heightened if any patients’ mishaps resulted from the error [13,15,45,47].Two implications have been reported to follow such a blaming culture.Firstly,Hashemi et al.cautioned how the fear of consequences might lead to silence among nurses,encroaching on their honesty and responsibility in VER [57].Secondly,this might drive nurses into feelings of worthlessness,guilt,and regret due to self-blaming,eroding their confidence and motivation to continue their chosen profession[2,20,36,38].
Studies (n=14) have also affirmed how assigning and focusing on individual blame following error reporting could result in nurses experiencing shame.The shaming culture denoted an implicit endorsement of an administrative sanction on any implicated nurses,degrading their worth and pride following reporting.The nurses’concerns were manifold.Nine studies reported how nurses experienced fear of losing their professional credibility due to their colleagues and supervisors devaluing their competency and considering them as underperforming by associating their errors with poor quality of nursing care [15,17,36,42,44,45,49,55,57].Additionally,nurses also felt distressed with the loss of honor and dignity should their mistakes were reported and exposed,to the extent of questioning their proficiencies in their chosen profession[2,15,20,42].
Furthermore,the fear of shame on error reporting was also documented in two studies from China.From the oriental perspective,nurses perceived the notion of VER as having to admitting their misdeeds which would lead to chastisement by coworkers and supervisors;hence,their disinclination towards VER to uphold social esteem and dignity [34,51].Lastly,nurses also feared media publicity on their errors following reporting[34,36,42,48,49].They were concerned that this would tarnish their reputation and bring their profession into disrepute due to their disinclination towards VER [15,44,51].
3.4.4.Fear of punitive repercussions
An organization condoning a punitive culture for reporting error make it less appealing for nurses to commit in VER [17,41].An institutionalized punitive culture has been demonstrated across some studies(n=17)to discourage nurses from reporting errors for fear of punishments for having committed them.In some instances,nursing leaders' disapproval was reflected in the various punitive sanctioning:poor ratings in performance appraisals,economic loss due to wage deduction and settlement of monetary fines,and termination of employment [2,11,15,20,36,38,41-44,49,55,57].Thus,the perceived threat to their existing employment stability and future career prospects induced the nurses' inaction for VER[34,44,56].It is noteworthy that the fear of disciplinary repercussions has led nurses to conceal their errors and others'[11,15,17,46,53].Such unwillingness prevailed lest they be jointly implicated in their co-workers’ errors that subject them to punishments due to collective team-based responsibility [15].
Additionally,the fear of professional liabilities has been demonstrated across some studies (n=7),leading to nurses'reluctance to report errors.Nurses associated any errors with professional negligence,the reporting of which would subject them to consequences such as institutional disciplinary proceedings,suspension or revocation of nursing licenses by nursing regulatory boards,and litigation on the grounds of malpractice[11,15,36,42,45,48,50].The reluctance among nurses towards VER for fear of nurse-patient disputes was further identified in 10 studies.The underlying reasons included the erosion of confidence of patients and family members in their profession,complaints,lawsuits,and even aggression [34,36,39,44-49,54].Again,it is noteworthy in some studies (n=5) that nurses would avoid reporting their co-workers’ errors for two reasons:their unwillingness to subject their co-workers to disciplinary actions[17,34,40,55],and their preference to avoid compromising the social convention between them that could potentially jeopardize amicable collegial working relationship [56].
4.Discussion
Identifying and reporting errors are vital steps to foster a safe working environment in healthcare.While eradicating medical errors is impractical[58],strategies to manage and reduce them are instrumental,and VER delineates one crucial initiative to improve patient safety.As frontline healthcare providers involved in direct patient care,nurses should be committed to VER.The impacts of errors on patient safety can be accurately evaluated,and preventive actions can thus correspondingly be meted.Apart from being a professional calling,this has also been seen as a legal and ethical obligation underpinning responsible nursing care [48].Quality assurance and patient safety in healthcare institutions can be affirmed when nursing leaders drive efforts and prioritize error reporting [59].
A review of the literature (n=31) revealed that the findings were more inclined towards highlighting nurses' less favorable opinions of the factors influencing their attitude and commitment towards VER,signifying that their experiences of VER were less than ideal.It is plausible that such negative experiences could lead to a slippery slope of patient safety culture.This review examined and will discuss the complexity and interplays of the issues concerning the relationship between nurses' attitude,perception,emotion,and practice in error reporting and various underlying factors that would underpin their experiences towards VER.This would produce a synergistic effect that leads to a better understanding of nurses’ overall experiences in VER.
4.1.Nurses’ attitude,perception,emotion,and practice of VER
This review first reported the attitude of nurses in VER were more inclined towards positive as evidenced by the number of studies (n=8) supporting this finding and as well as of those(n=3)who revealed a higher rate of VER among them as compared to other health professionals.Inherent to the principle of sound risk management is the unmistakable ability to recognize and embrace error reporting.This commitment further reflects nurses as a disciplined workforce that displays integrity and dedication towards a culture of safety and quality.Nonetheless,studies (n=9)included in this review had also revealed that nurses failed to report an error,and this further signifies a gap between their idealistic professional views and realistic practice of VER.Because of this,studies postulated that VER was a rational behavior in which nurses exercised their rational decision-making after considering the consequences to choose and plan their actions and then engage in that desired behavior[17,60].Ajzen and Fishbein's[61]theory of planned behavior (TPB) has offered insights into this view by deducing that attitudes and perceptions of an individual (nurse)would form the primary determinant to influence their rational behavior,i.e.,their commitment towards VER.According to the TPB,attitudinal beliefs (the first domain) posited how the behavior(VER) of an individual (nurse) and the intention to act on that behavior rested with their consideration;in other words,this would depend on whether the individual had a favorable or unfavorable evaluation of that behavior.This explanation echoed with the findings of this review,where nurses would consider various positive and negative consequences to underpin their attitude and their eventual decision to commit to VER.This would also influence their underlying feelings and emotional coping concerning that decision they had made.
Using the TPB as an approach [61],Redding et al.[62] further explained how two considerations would underpin attitudinal beliefs of nurses towards VER:firstly,their expectation of the outcome for engaging in that behavior and secondly,the extent to which they value the result[62].As reported in this review,nurses’practice of selective reporting and their perception of reporting as insignificant would reflect on a spectrum of their negative attitude towards VER;this would align with both considerations by Redding et al.[62].Echoing this review,Chiang et al.[17]argued that,since most errors did not seriously harm patients,most nurses would consider them careless lapses and hence had perceived reporting as redundant.These identified issues would therefore signify their complacency and further undermined their professional credibility.
Additionally,this review also revealed nurses' disinclination in reporting their co-workers’ errors.One plausible explanation was that nurses had perceived whistleblowing as an act of sabotage that breached professional etiquette.Given the insights from attitudinal beliefs of the TPB[61],nurses viewed that whistleblowing and the punitive follow-up actions on those implicated would jeopardize amiable collegial relationships and possibly even inter-professional collaboration,which explained their less favorable attitude and commitment in VER.This explanation was in line with Espin et al.[53] and Hewitt et al.[56],further supporting the two considerations of attitudinal beliefs as discussed earlier by Redding et al.[62].Nonetheless,nurses must realize that they also owe a duty of care to their patients:the two principles of beneficence -‘doing good’ and non-maleficence -‘above all,not harm’ -implies that nurses are accountable for not only their actions but also others'that might endanger the patients' safety [63].Commitment to the disclosure of errors of self and others would support this principle.
Ajzen and Fishbein[61]also postulated that in addition to their attitudinal belief,commitment to an intended behavior(VER)by an individual also rested with their perceived behavioral control.This was associated with control beliefs,the second domain of the TPB.In other words,Chang [64] contended that nurses' attitude and commitment in VER would also depend on their perceived capabilities and proficiencies to drive their intention.This concurred with this review where nurses attributed not committing to VER due to forgetfulness and knowledge deficits.These fallibilities further reflected the limitations of nurses’ capabilities and challenged their ability to engage in VER.Such findings further resonated with Garrett &Reeves [65] and Brubacher et al.[66].Addressing from the perspectives of attitudinal and control beliefs of the TPB,two important recommendations would arise from these findings of this review.Firstly,this calls for nursing leaders to drive professional education programs to inform and convince nurses on the importance of VER and their crucial role and responsibilities in contributing to patient safety culture.Secondly,it is also imperative for nursing leaders and the broader organization to advocate necessary support mechanisms to provide emotional comfort to nurses affected by their decision of VER.This will cultivate a positive mindset and enhance receptiveness among nurses to VER [57,67,68].
4.2.Nurses’ perceived enabling and inhibiting factors of VER
A review of both facilitating and inhibiting factors had demonstrated that the efforts to drive nurses’ commitment to VER stemming from various considerations of organizational supports needed improvement.Resonated with the view of Afolalu et al.[39],nurses in this review also posited that their attitude and commitment to VER would be strengthened by addressing various systemic,organizational,and administrative factors.While this review had shown that nurses would value multiple initiatives to drive their positive attitude and commitment to VER,by the same token,having to deprive them of these incentives would further discourage them from doing so.This further points to the limitation of the organization to advocate a just and open patient safety culture that is conducive to supporting VER.
Addressing the inadequacies of reporting systems exemplified by their perceived complexity and redundancy of existing errorreporting systems in underlying nurses' unwillingness to report errors is one pressing concern.They also represented another situation of control belief,the second domain of Ajzen and Fishbein's TPB [61] as discussed earlier,where Chang [64] further asserted how their perceived lack of supportive resources and opportunities would also act as predictors to hinder their commitment to VER.Nursing leaders need to acknowledge such logistical barriers and strive to simplify and streamline them to encourage reporting.Resonating with the views of Chen et al.[10],this review has also found it critical for nursing leaders to obtain feedbacks from nurses as frontline users to review and improve the reporting process.Considering technological advancement,it is also imperative that the nursing leaders work with information technology designers to establish more user-friendly electronic error-reporting systems.Such supportive steps serve as initiatives that contribute as the enabling factors for VER,but actively involving nurses in the change process is envisioned to drive their positive experiences and dedication to VER.
Ajzen and Fishbein[61]further argued how nurses'attitude and commitment in VER could be shaped by their normative belief,the third domain of TPB.In this instance,Sheeran &Orbell [69]explained that the normative idea concerned the extent to which an individual (nurse) perceived and valued the opinions and attitudes of other people(subjective norm)to perform in that intended action.This review has further highlighted the significance of two aspects of normative beliefs:the nature of the reporting process and responses from nursing leaders following error reporting.Firstly,the bureaucratic and centralized nature of seeking a supervisor's endorsement before engaging in formal error reporting would encroach on nurses'autonomy to abide by their professional accountability to undertake mandatory reporting.Additionally,when nursing leaders practiced selective reporting,and their actions were incongruent with institutional guidelines of compulsory reporting,Lee et al.cautioned that this might cause nurses to experience dissonance and unknowingly endorse and imitate this flawed practice [20].This would further undermine the organizational efforts to drive a safe and just culture.In this regard,Covell and Ritchie have asserted that individuals tended to follow ‘the culture of the floor,’implying that the departmental culture would shape VER practices among nurses [70].Thus,this reflected the need for nursing leaders to stay objective and exhibit exemplary behaviors of error reporting to drive this positive influence among nurses.Secondly,the issues concerning negative and absence of feedback aftermath VER could impede learning for nurses,who would have only an incomplete understanding of the incident and its factors.In this regard,Hoffmann and Rohe contended that,following error reporting,nursing leaders would have to openly convey the investigation outcomes alongside constructive feedback to the nurses involved to support their learning from mistakes[71].Accordingly,Hillen et al.[72]and Wong,Cummings,and Ducharme[73] had recommended for nursing leaders to adopt the appropriate leadership style,such as transformational leadership,to model clinical governance stewardship to advocate a conducive working culture desirable for error reporting for nurses,further contributing as an enabling factor to drive their positive experiences in VER.
One recurring finding in this review is fear,identified by nurses as a predominant factor for their evasion from VER.Echoed with the view of Heard et al.[74],the notions of blame,shame,and punishment as highlighted by this review represented different facets of collegial,managerial,and organizational disapproval(normative beliefs) of nurses' erroneous actions and were responsible for their strong and negative evaluation towards VER.This review would discuss nurses’fear from two perspectives,1)blame at the management and collegial levels and 2) blame at the personal level and its related consequences.
At the management and collegial levels,nurses'fear of punitive actions and disapproval by their nursing leaders and colleagues has led to their unwillingness to report errors.Two implications could follow.Firstly,Kagan and Barnoy have found that this could lead to nurses deliberately concealing future errors to absolve them from accountability [59].Secondly,Chen et al.have posited that fear would further demotivate nurses -the frontline users -to voice their insights into problems underlying errors [10].While nurses are not to be absolved from professional accountability,nursing leaders should be mindful that honest errors are part of human fallibility.Therefore,the focus should be on instilling the belief that error reporting seeks to enhance nurses’ learning and improve existing flaws of work processes:such a belief could improve their receptiveness to VER.
At the personal level,the fear of punishments following error reporting drove nurses to strive for perfection in their performance,potentially unknowingly subjecting them to undue pressure.When unmet,such unrealistic perfectionistic expectations might turn into self-blame [75,76].Reproach by others,coupled with selfcondemnation,could further result in more fear and ill feelings towards VER.Thus,the two perspectives have called for nursing leaders at all levels to work with other healthcare stakeholders to drive a non-destructive culture of reporting,serving as an incentive to promote nurses’ positive experience toward VER.
4.3.Limitations and strengths
Some limitations are of note.Firstly,while the literature search has involved four databases,the use of more databases might have ensured a more comprehensive retrieval of papers because of the heterogeneous terminology about errors.Secondly,potential publication bias arose from the inclusion of solely peer-reviewed papers in English,as this step could have meant excluding relevant materials from other sources and in other languages.Nonetheless,one of the strengths of this review is that our findings are not confined to one cultural context,and this breadth provides comprehensive insights into nurses’error-reporting behaviors from a global perspective.Secondly,the methodological strength of this review was the adoption of integrative review methods that drives systematic and rigorous screening and reporting of evidence to attenuate potential bias and errors [26,27].
4.4.Implications for nursing management and recommendations
4.4.1.Strategies to enhance nurses’ positive attitude,perception,and practice of VER
Following the discussion above on how various factors would profoundly influence VER by nurses,several recommendations are suggested.Firstly,the issues concerning nurses'negative attitude in VER underpinned by their cognitive fallibilities,their negative perceptions towards VER,and their preference towards oral reporting call for the necessity for further attention.Such human approaches to error management posit to attribute an adverse incident to human failures [39,57].Human failures undermine an organization's effort and ability to build and sustain an effective error-management system.To promote a strong patient-safety culture,three areas of improvement involving continuous learning are warranted.Firstly,undergraduate curricula should instill among nursing students the significance and benefits of error reporting to equip them with sufficient knowledge and correct mindsets to prepare them for practice.Secondly,healthcare institutions should invest time and resources in reviewing and,if necessary,revising existing training initiatives to improve nurses'proficiency in safety management.Internal workshops on patient safety,risk management,and incident reporting should be incorporated into new nurses' orientation programs to acquaint them with institutional error-management protocols and be organized periodically for existing staff to teach their correct beliefs and adherence to proper practices in VER.Thirdly,identifying the learning needs of nursing staff should also be prioritized to tailor appropriate ‘refresher’ training to drive their positive attitudes,perceptions,and professional accountability towards VER.Additionally,training opportunities for both senior and middle nurse leaders may be considered to improve their understanding of the significance of their roles through leading by example and role modeling by consistently adhering to institutional error-reporting guidelines.This was exemplified by discouraging the notion of oral reporting and encouraging and affirming their support for nurses' decision to lodge errors through formal incident report systems.
4.4.2.Strategies to support nurses’ emotions and to promote their commitment to VER
Nonetheless,the literature on safety has contended that a given adverse incident usually does not originate from a single event caused by an individual(human failure)but rather from a series of events.This view reflects the complexity of the interplay between multiple factors [3,77,78].Such a systematic approach to error management posits attributing an adverse incident to system failures [57,68,77,78].Despite advocacy for deemphasizing individual blame by healthcare institutions to promote a supportive culture of reporting [2,56],this review has found that nurses' resistance towards VER was partly due to the entrenched organizational culture characterized by nursing leaders' disapproval of nurses' errors.As such,nurses would view VER as a mechanism that reflected their failures and subjected them to disciplinary actions,which might cause nurses to lose trust in the organization when they perceived a mismatch between idealistic and realistic practice.Consistent with the view of Smeulers et al.[79],this calls for nursing leaders to consider openly encouraging and rewarding nurses for their efforts in disclosing their errors and others,with a focus on root cause analysis and improving the system rather than blame.Additionally,to ease their perceived burden of reporting,nurse leaders could consider incentives,such as allocating protected time within nurses' working hours to meet their daily requirement of completing their necessary administrative duties,or where it is not feasible,to replace with overtime pay if error reporting take place outside work time.Undertaking this recommendation will affirm an organization's commitment to an open and just safety culture and cement nurses' trust in VER.
Lastly,this calls for collaborative efforts among nursing leaders to introduce organizational reforms to promote shared values on error reporting.Firstly,as change sponsors,nursing executives are instrumental in espousing this commitment and legitimizing change in a twofold manner:enacting and conforming to institutional policies that explicitly enforce zero-tolerance to nonreporting behaviors mandating feedback collective contextual learning in the aftermath of error reporting.Secondly,they should ensure supportive protocols and initiatives to manage the emotional needs of distressed nurses due to errors.Thirdly,they could consider organizing corporate team-building events such as staff retreats where frontline nurses are invited and empowered to voice their opinions and concerns.They should also work together with senior and middle nursing leaders to collectively formulate practical solutions to improve error-reporting initiatives.Alternatively,the anonymous employee-engagement survey may be deployed as a platform for nurses who wish to remain anonymous but are keen to share their concerns;this will provide insights into their perspectives on VER barriers and develop strategies to address them.Nurse managers should critically drive departmental changes by disseminating institutional expectations and error reporting guidelines to all nursing staff to reinforce their adherence.Nurse managers are also instrumental in establishing a positive departmental culture that forms the norm for encouraging error reporting and dealing with errors.This can be done by managing nurses’ expectations on error reporting through proper supervision,monitoring and regulating collegial attitudes,and acting as role models for acceptable behaviors by reacting to a mistake saying congruent with the system approach to error management.These initiatives entail an open and supportive risk management system.
5.Conclusions
To the best of our knowledge,this is the first integrative review to integrate findings that examine nurses' attitudes,practices,and emotions,and various enabling and inhibiting factors from gaining comprehensive insights into nurses' experiences in VER from a holistic approach.This review concludes that nurses'experiences in VER have been less than ideal,underlining a thorny problem that would deserve further attention.The connection between nurses'attitude and perception of VER and how various enabling and inhibiting factors perceived by them influence their commitment to VER is evident.This implies that existing organizational initiatives to establish an effective error management system needed improvement.This warrants more outstanding efforts by organizations to formulate and invest in strategies to manage various aspects of human failure and system failure to drive positivity of their overall experiences and devotion in VER.A strong corporate responsibility is needed to establish a safe and just working culture.To display the organization's commitment to driving this cultural shift,nursing leaders should prioritize mass communication of these strategies to raise nurses' awareness of its availability and understanding of their organization's intention to drive patient safety culture to ensure its practicability.Future research should investigate nurses' perspectives on these strategies initiated by their healthcare organizations to evaluate the effectiveness of supporting nurses' learning and emotional well-being after error reporting and promoting their commitment to VER.
Declaration of competing interest
The authors have declared no conflict of interest.
Funding
Nothing to declare.
Data availability statement
Authors declare the absence of shared data in the present study.
CRediT authorship contribution statement
Ming Wei Jeffrey Woo:Conceptualization,Methodology,Formal analysis,Writing -original draft.Mark James Avery:Supervision,Methodology,Formal analysis,Writing -review &editing.
Acknowledgments
This article is the revised version of Jeffrey Woo's Master dissertation as part of his study for the Master of Health Services Management programme at School of Medicine,Griffith University.The authors would like to acknowledge the support of School of Medicine,Griffith University for their support in this study.
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2021.07.004.
杂志排行
International Journal of Nursing Sciences的其它文章
- A study of the relationship between nurses’ experience,structural empowerment,and attitudes toward computer use
- Self-care:A concept analysis
- Exploring the employment readiness and return to work status of breast cancer patients and related factors
- Resilience of nurses at the epicenter of the COVID-19 pandemic in Lebanon
- Mobile health applications for the care of patients with breast cancer:A scoping review
- Nursing students’ attitudes toward mobile learning:An integrative review
