Role of endoscopic ultrasound in the field of hepatology:Recent advances and future trends
2021-12-06JahnviDharJayantaSamanta
Jahnvi Dhar,Jayanta Samanta
Jahnvi Dhar,Jayanta Samanta,Department of Gastroenterology,Post Graduate Institute of Medical Education and Research,Chandigarh 160012,India
Abstract The role of endoscopic ultrasound(EUS)as a diagnostic and therapeutic modality for the management of various gastrointestinal diseases has been expanding.The imaging or intervention for various liver diseases has primarily been the domain of radiologists.With the advances in EUS,the domain of endosonologists is rapidly expanding in the field of hepatology.The ability to combine endoscopy and sonography in one hybrid device is a unique property of EUS,together with the ability to bring its probe/transducer near the liver,the area of interest.Its excellent spatial resolution and ability to provide real-time images coupled with several enhancement techniques,such as contrast-enhanced(CE)EUS,have facilitated the growth of EUS.The concept of “Endo-hepatology” encompasses the wide range of diagnostic and therapeutic procedures that are now gradually becoming feasible for managing various liver diseases.Diagnostic advancements can enable a wide array of techniques from elastography and liver biopsy for liver parenchymal diseases,to CE-EUS for focal liver lesions to portal pressure measurements for managing various liver conditions.Similarly,therapeutic advancements range from EUS-guided eradication of varices,drainage of bilomas and abscesses to various EUS-guided modalities of liver tumor management.We provide a comprehensive review of all the different diagnostic and therapeutic EUS modalities available for the management of various liver diseases.A synopsis of all the technical details involving each procedure and the available data has been tabulated,and the future trends in this area have been highlighted.
Key Words:Endoscopic ultrasound;Liver disease;Elastography;Varices;Liver tumor;Liver biopsy
INTRODUCTION
The armamentarium of endoscopic ultrasound(EUS)has grown considerably in recent years,both as an investigative and a therapeutic modality.The established diagnostic tools for the study of liver diseases include trans-abdominal ultrasound(USG),computed tomography(CT)scan and magnetic resonance imaging(MRI).While in the past,interventions in liver disease have predominantly been performed by the percutaneous or vascular route,EUS is now more and more being used for both diagnostic and therapeutic purposes.The ability to combine endoscopy and sonography in one hybrid device is a unique property of EUS,together with the ability to bring its probe/transducer in close proximity to the liver,the area of interest.In addition,its excellent spatial resolution and ability to provide real-time images,along with additional techniques,such as contrast-enhanced(CE)EUS,have facilitated the growth of EUS.
Furthermore,EUS guided intervention is also used as a rescue modality when the percutaneous approach is not favorable.EUS has opened doors to a variety of other procedures which are being explored,such as portal vein(PV)sampling for cancer cells,delivery of chemotherapy in the PV,measurement of portosystemic pressure gradient,and EUS guided transjugular intrahepatic portosystemic shunt(TIPS)creation.Harnessing its use in various liver-related interventions paves the way for a new zone of specialty,“Endo-hepatology.” Herein we provide a comprehensive review on the use of EUS in the field of hepatology,both diagnostic and therapeutic,discussing the various recent advances and future trends(Figure 1).
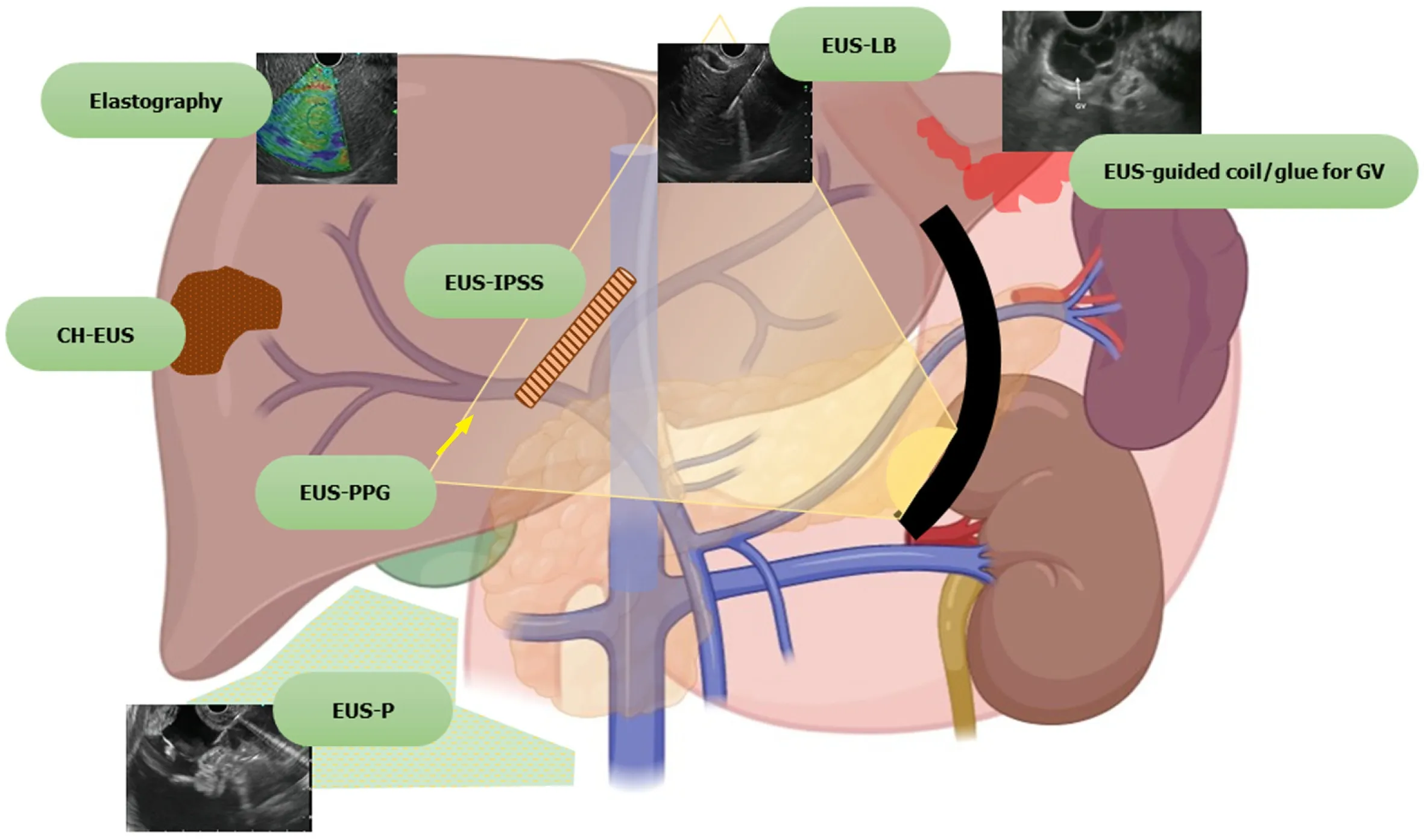
Figure 1 Spectrum of endoscopic ultrasound in hepatology.EUS:Endoscopic ultrasound;CH-EUS:Contrast harmonic endoscopic ultrasound;EUSIPSS:Endoscopic ultrasound guided intrahepatic portosystemic shunt;EUS-LB:Endoscopic ultrasound guided liver biopsy;EUS-PPG:Endoscopic ultrasound guided portal pressure gradient;EUS-P:Endoscopic ultrasound guided paracentesis;GV:Gastric varices.
LITERATURE SEARCH
A search was performed in PubMed and Embase and the search strategy is outlined in Supplementary Doc 1.All studies such as case reports,series,clinical studies,animal models and reviews regarding EUS applications in liver disorders,including portal hypertension(PHTN),were reviewed.Non-English language literature was not included in the review.EUS applications for extrahepatic bile duct obstruction,gallbladder,etc.,including their interventions,are beyond the scope of this review and have been excluded.
EUS FOR LIVER PARENCHYMA ASSOCIATED DISEASES
EUS can be used for the diagnosis,assessment and therapeutic management of ascites,liver parenchymal pathologies,space-occupying lesions(SOLs),liver biopsy,drainage of liver abscesses,bilomas and the management of hepatic tumors.
Ascites:Assessment and paracentesis
Ascites can be due to benign or malignant diseases.Although the differential diagnosis is broad,around 80%-90% of cases are attributed to underlying cirrhosis and PHTN[1].Traditionally,routine paracentesis is performed bedside and sometimes with abdominal ultrasound guidance.However,abdominal paracentesis may become difficult in the presence of multiple abdominal scars,previous puncture marks,obesity,dilated bowel loops,dilated/tortuous veins,or the presence of omental or peritoneal nodules[1-3].EUS guided paracentesis(EUS-P)is more sensitive than CT in detecting ascites[2,4].The presence of ascites not visualized on imaging(CT/USG)as well as compartmentalization of fluid(such as benign etiologies like tuberculosis or tumor implants in peritoneal carcinomatosis)makes EUS-P a very promising tool in these areas[4,5].With EUS-P,even small amounts of fluid(as little as 2.7 mL)can be aspirated and provide valuable diagnostic information[6].In addition,EUS-P can be used as a rescue procedure in the case of previously failed percutaneous paracentesis or part of diagnostic workup during diagnostic EUS(Figure 2).
Additionally,EUS guided fine needle aspiration(EUS-FNA)of suspicious nodules in the omentum/peritoneum can be performed simultaneously while performing paracentesis for targeted cytological diagnosis[7].Contrast-enhanced EUS(CE-EUS)has also been evaluated to identify enhancement patterns of peritoneal nodules or omental caking and differentiate benign or malignant causes of undiagnosed ascites[8].
The technique of EUS-P:The technique of EUS-P is detailed in Table 1.
Future trends:Since the first report of EUS-FNA of ascites and pleural fluid performed in 1995,various reports of EUS-P with/out FNA of peritoneal deposits have been published subsequently with excellent diagnostic capability and correlation with intraoperative findings[12].Some cases of development of infectious complications(attributed to traversing the contaminated gastrointestinal wall)such as self-limited fever(3.3%)and bacterial peritonitis(4%)have been reported[5,10].Recent developments include the deployment of double plastic stents in loculated ascites(benign/malignant),leading to internal drainage causing significant improvement in quality of life[13,14](Figure 3).A clinical trial is also recruiting patients for EUS guided placement of a plastic prosthesis for refractory malignant ascites[15].The various studies on EUS-P are summarized in Table 2.

Figure 2 Endoscopic ultrasound guided paracentesis.Needle is visualized in the ascitic fluid.

Table 1 Technique of endoscopic ultrasound guided paracentesis[1-3,9-11]
Thus,EUS-P is an excellent tool(sensitivity 94%,specificity 100%)to detect a small quantity of ascites[10]and therapeutic drainage where the percutaneous approach isnot amenable.Furthermore,FNA of peritoneal/omental nodules is an added advantage that can increase the diagnostic yield.
Assessment of liver parenchyma/SOLs:Anatomy of the liver,its segments and surrounding structures
The requirement for three-dimensional conceptualization of the liver parenchyma makes EUS assessment of the liver and surrounding structures different from the conventional methods of USG/CT/MRI.Depending on the position of the EUS scope,either in the stomach or duodenum,various structures can be identified(Table 3 and Figure 4)such as[17]:(1)From the gastric end:Segments I(caudate lobe),left lobe segments(II,III,IV),right lobe(V,VIII),umbilical part of the left PV and ligamentum teres,ligamentum venosum,inferior vena cava,and hilum;and(2)From the duodenal bulb:Segments VI,VII;the hepatoduodenal ligament structures and PV and hepatic artery branches,the liver hilum and the segmental divisions of the right PV and hepatic artery.

Table 2 Studies on endoscopic ultrasound guided paracentesis

Table 3 Structures visualized with endoscopic ultrasound in the liver
Although transabdominal USG or CT scan is the first-line approach for evaluation of liver parenchyma or focal lesions,EUS has additional features which can add to its diagnostic/therapeutic potential[18,19]:(1)Transducer proximity enables better identification of the structures;(2)Combination of real-time images with elastography enables semi-quantitative measurements of liver parenchymal stiffness;(3)Newer generation EUS machines with color,power and pulsed Doppler systems helps easy assessment of the vasculature;(4)CE-EUS or harmonic EUS increases the diagnostic performance of focal liver lesions;and(5)Simultaneous assessment and interventions such as management of varices and liver biopsy can be performed in a single setting.
Techniques of assessment:Elastography and contrast enhancement techniques
Real-time elastography(RTE)has been developed for the assessment and quantification of liver tissue stiffness.Qualitative RTE uses the degree of deformation by the compression of structures as an indicator of tissue stiffness and is depicted using a color map wherein hard tissue is blue,intermediate stiffness is green and soft tissue is red.Quantitative RTE,on the other hand,uses hue histogram and strain ratio.Whilethe former is a graphical representation of the color distribution in a selected image field,the strain ratio is calculated as the ratio of the target area(A)by reference area(B)(Figure 5)[20].

Figure 3 Endoscopic ultrasound-guided internal drainage of loculated ascites.A:Puncture of the loculated ascites with 19-G aspiration needle;B:Guidewire negotiated across as visualized on endoscopic ultrasound;C:Fluoroscopic view of guidewire coiled inside the loculated ascites;D:Naso-cystic drain placed inside the loculated ascites.

Figure 4 Endoscopic ultrasound anatomy of liver segments.A:Anatomy of the left lobe with S2 and S3 segments;B:Ligamentum teres with umbilical portion of the left portal vein;C:Middle hepatic vein with segments of the liver;D:Anatomy of the bifurcation of portal vein from the duodenal bulb.PV:Portal vein;MHV:Middle hepatic vein;LHV:Left hepatic vein;RPV:Right portal vein;LPV:Left portal vein.
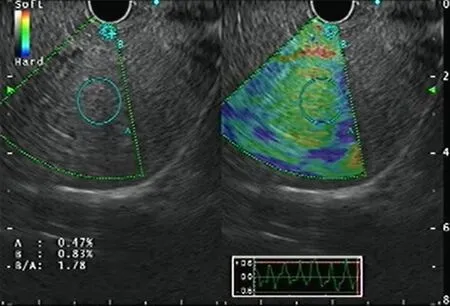
Figure 5 Endoscopic ultrasound elastography of the liver parenchyma.
CE-EUS is a more valuable technique to improve the diagnostic performance of focal liver lesions.It is of 2 types:CE-EUS with the Doppler method(CE-EUS-D)and CE-EUS with harmonic imaging(CE-EUS-H).The former helps distinguish vascularrich and hypovascular areas of a liver SOL,whereas the latter helps provide a detailed roadmap of the vasculature of the same.Of the contrast agents available,Sonovue and Sonazoid are more commonly used[21].
The concept of CE-EUS depends on the dual blood supply of the liver and has 3 phases:arterial phase(20-45 s),portal venous phase(lasting up to 120 s),and the late phase(contrast agent clearance,around 6 min)[21].
The advantages of CE-EUS over CT and MRI are that:(1)It provides real-time imaging;(2)Contrast is not excreted by the kidneys,and thus can be used in cases with renal insufficiency;(3)Contrast is confined to the vascular space only and so has prolonged enhancement of vascular system;(4)Higher resolution helps in targeted biopsies;and(5)Can characterize lesions less than 1 cm.
EUS imaging in chronic liver diseases
Certain tests such as transient elastography(TE),Fibroscan,and RTE can aid in the diagnosis of the degree of liver fibrosis.However,these tests are fraught with limitations in people with obesity and ascites.EUS can be used similarly with probably better diagnostic sensitivity for the same.Schulmanet al[22]reported that liver fibrosis index(LFI)correlated with abdominal imaging(LFI in normal,fatty liver and cirrhosis patients were 0.8,1.4 and 3.2,respectively).Similar findings were replicated in liver fibrosis assessment for chronic hepatitis C cases(LFI of 2.38 had an area under the receiver operating characteristic curve of 0.73)compared with the gold standard of liver biopsy.Histogram acquisition was successful in 82% of patients[23].A recent study by Tuet al[24]in early-stage cirrhosis showed that the accuracy of a combination of EUS,EUS-RTE,acoustic radiation force impulse(AFRI)and aspartate aminotransferase-to-platelet ratio(APRI)had the highest diagnostic rate(sensitivity 87%).Thus,EUS can provide a one-stop diagnostic modality to screen and rule out a host of conditions in patients with liver disease,from the screening of varices,pancreaticobiliary pathology to hepatic parenchymal/SOL assessment.
EUS imaging in focal liver lesions
The diagnostic accuracy of EUS in detecting focal liver lesions,mostly less than 1 cm,exceeds that of USG,CT,and MRI[25,26].Singhet al[27]addressed the diagnostic yield of EUSvsCT for hepatic metastasis(98%vs92%),wherein EUS identified a significantly greater number of metastatic lesions(40vs19).Diagnostic criteria proposed by Fujii-Lauet al[28]can be used to differentiate between benign and malignant metastatic hepatic lesions based on EUS findings with a positive predictive value of 82%.Lesion shape,borders,echogenicity,homogeneity,and size are used to delineate malignant lesions.It is said to be neoplastic if it meets at least three criteria:(1)Lack of isoechoic/slightly hyperechoic center;(2)Post-acoustic enhancement;(3)Adjacent structures distortion;(4)Hypoechogenicity(slightly or distinctly);and(5)At least 10 mm in size.
With the advent of EUS-RTE,the characterization of liver SOLs and their biopsies have become better(Figure 6).A study reported a hue histogram cutoff of 170 to discriminate between benign and malignant tumors(sensitivity 92.5%,accuracy 88.6%)[29].In addition,the use of contrast agents in CE-EUS helps in differentiating primary tumors and metastasis[30].CE-EUS has also been utilized for the assessment of treatment response in hepatocellular carcinoma(HCC)post-trans-arterial catheter embolization[31].Hence,EUS with RTE,CE-EUS and CE-EUS-H might be a promising tool for diagnosing focal liver lesions and targeted intervention.
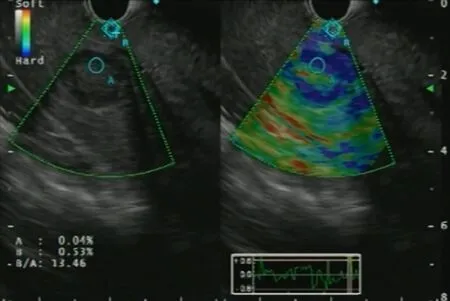
Figure 6 Endoscopic ultrasound elastography of a focal liver lesion with strain ratio calculation.
EUS-FNA of focal liver lesions
Several studies exist on the use of EUS-FNA/FNB(fine needle biopsy)for solid liver lesions with a complication rate of 0%-6%(Table 4).A recent systematic review by Ichimet al[42]showed the diagnostic yield of EUS-FNA to be 80%-100%.
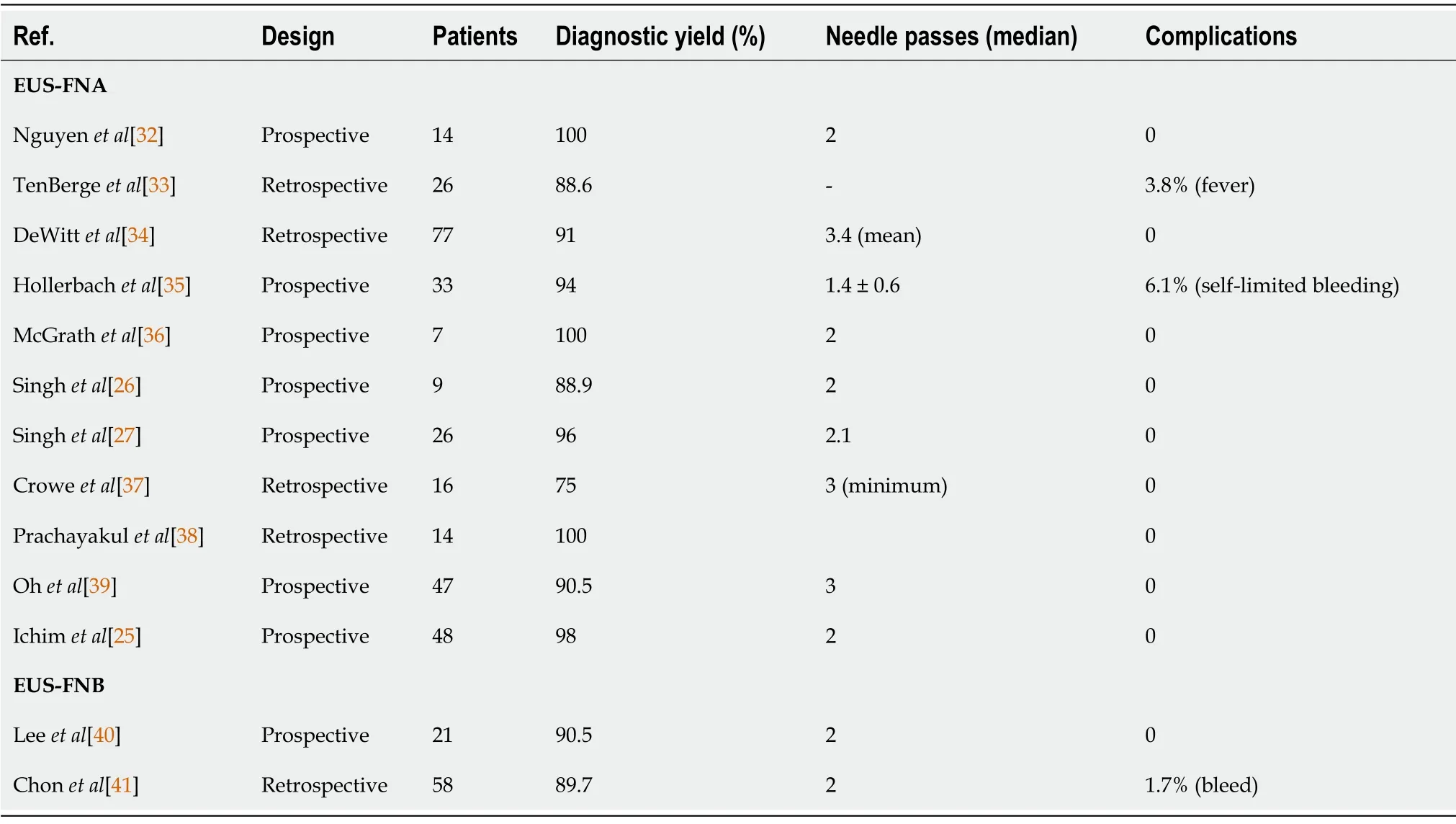
Table 4 Studies on endoscopic ultrasound guided fine needle aspiration/fine needle biopsy of focal liver lesions
Future trends
Studies have reported additional assessment of KRAS mutation in inconclusive cytological samples,which has resulted in an improved diagnostic yield from 89.3% to 96.4%[43].Similarly,an animal study has evaluated the art ofin vivocytological observation using a high-resolution micro-endoscopy(HRME)system under EUS guidance[44]to decrease the number of needle-passes and subsequent adverse events.Recently,Minagaet al[45]have reported the additive role of CE-EUS-H in the detection of left lobe liver metastasis from pancreatic ductal adenocarcinoma.The diagnostic accuracy of CH-EUS was 98.4% compared to 90.6% with CECT.
EUS guided liver biopsy
Despite the advances in various non-invasive testing available to determine the degree of fibrosis,liver biopsy remains the gold standard method for accurate assessment in diagnosis and staging.As first described in 1883 by Dr.Paul Ehlrich,percutaneous liver biopsy(PC-LB)has evolved from a mere percussion method to an “imageguided” technique in the last ten years using ultrasound/CT imaging to accomplish it.However,despite image guidance,the risk of bleeding persists,occurring in up to 0.6% of cases,including other adverse events like pneumothorax and gallbladder puncture and even death in a few cases[46].The transjugular technique of liver biopsy,introduced in 1973,can help reduce this risk,especially in patients with underlying coagulopathy.However,this method also carried added risks of local site hematoma,intraperitoneal bleeding,arrhythmia and carotid puncture[47].
EUS guided liver biopsy(EUS-LB)initiated as early as 2007 is currently emerging as a cost-effective,safe and well-tolerated procedure and helps in more representative sampling.The American Association for the Study of Liver Diseases recommends a tissue length of at least 2-3 cm with ≥ 11 or more complete portal tracts(CPTs)for determining the adequacy of liver biopsy samples[48].The mean tissue length and CPTs for EUS-LB,PC-LB and TJLB,as shown in various studies is 36.9,9 and 17.7 mm,and 7.7,13.5 and 6.8 mm,respectively[49,50].This can be achieved with a regular 19 G EUS-FNA needle(71).Similarly,a meta-analysis on EUS-LB revealed that pooled successful histological diagnosis was achieved in 93.9% of cases.Adverse event rateswith EUS-LB,PC-LC and TJLB were 2.3%,0.09%-3.1% and 0.56%-6.5%,respectively[48,51,52].A recent meta-analysis between the three techniques revealed that EUS-LB was comparable to PC-LB in terms of CPT,but tissue length was better with the former with no complication rates[53].
EUS-LB has been used in the setting where patients undergo other endoscopic procedures such as screening of the biliary tree,assessment of surrounding structures and lymph nodes and variceal screening in those not affected with ascites and obesity[50],thereby saving time and resources.Furthermore,EUS-LB is theoretically less painful as it does not require skin puncture,eliminates the need for breath-hold and allows visualization and avoidance of blood vessels even 1 mm in size and is suitable for anxious patients by using adequate sedation(Figure 7).Moreover,bilobar biopsy can be achieved,reducing sampling error and helping in better assessment of disease activity and fibrosis[54].

Figure 7 Endoscopic ultrasound-guided liver biopsy.
Technique:The technique of EUS-LB is described in Table 5.
Future trends:In attempts to acquire better quality and quantity of specimens,various studies have been published on different needles and methods of executing a EUS-LB procedure.A recent RCT comparing a 19 G FNB needle(fork-tip)vs19 G standard FNA needle yielded better results with the former(pre-processing length 2.09 cmvs1.47 cm and more CPTs)[55].In contrast,a recent meta-analysis showed the superiority of FNA needles over core biopsy needles in terms of better tissue acquisition[51].Thus,19 G FNA needle may be used for EUS-LB procedures except for the cases where immunohistochemistry and architecture characterization are warranted,in whom core biopsy needle may be used.
Moket al[56]showed that the “wet heparin” suction technique had greater tissue yield compared to “dry suction”(aggregate specimen length 49.2 mmvs23.9 mm;mean CPT count 7vs4).Thus,the combination of wet-heparinized suction and a 19-G second-generation(FNA/FNB)needle might help achieve better specimens with minimal fragmentation.
The various studies using EUS-LB(FNA/FNB)in patients with chronic liver disease are highlighted in Table 6.The average technical success and diagnostic yield for EUSFNA and EUS-FNB-guided liver biopsy are 100% and 89.8%,respectively,with a complication rate of 3.3%,consisting entirely of minor events[70].In addition,studies reporting the use of EUS-LB in patients with NAFLD(overall technical success rate 100%,yield 96.8% with 7.7% complication rate)are reported in Supplementary Table 1.
EUS guided therapeutic management of liver cysts,liver abscess and biloma
Symptomatic liver cysts,abscesses and bilomas may require drainage.Traditionally,these were approached through surgical or interventional radiology using percutaneous catheter drainage(PCD).Recently,EUS guidance has been used to drain simple intrahepatic cysts of varied etiologies,liver abscesses and bilomas.EUS guided drainage may be superior to PCD as it enables a one-step approach,leading to internal drainage and thus avoiding the complications of catheter dislodgement,pericatheter leak,multiple interventions and movement restrictions.
EUS guided treatment of hepatic cysts:The most frequent liver cysts encountered for drainageviaEUS include simple hepatic cysts and intrahepatic pancreatic pseudocysts.Those located in the left lobe of the liver or the caudate lobe can be drainedviaEUS guidance.PCD would be preferred for right lobe cysts as it is difficult to access the right lobe in the duodenal bulb with an unstable scope position.Therapies offered by EUS include fine-needle aspiration,ethanol lavage and transmural stent placement.
In a retrospective study by Leeet al[71],19 cases of hepatic cysts were treated by PCD and EUS guided ethanol lavage and reported a 97.5% reduction in cyst volume at 11.5 mo of follow-up in the PCD group and a 100% reduction at 15 mo in the EUS arm.The studies on EUS guided treatment of hepatic cysts are outlined in Supplemen-tary Table 2.
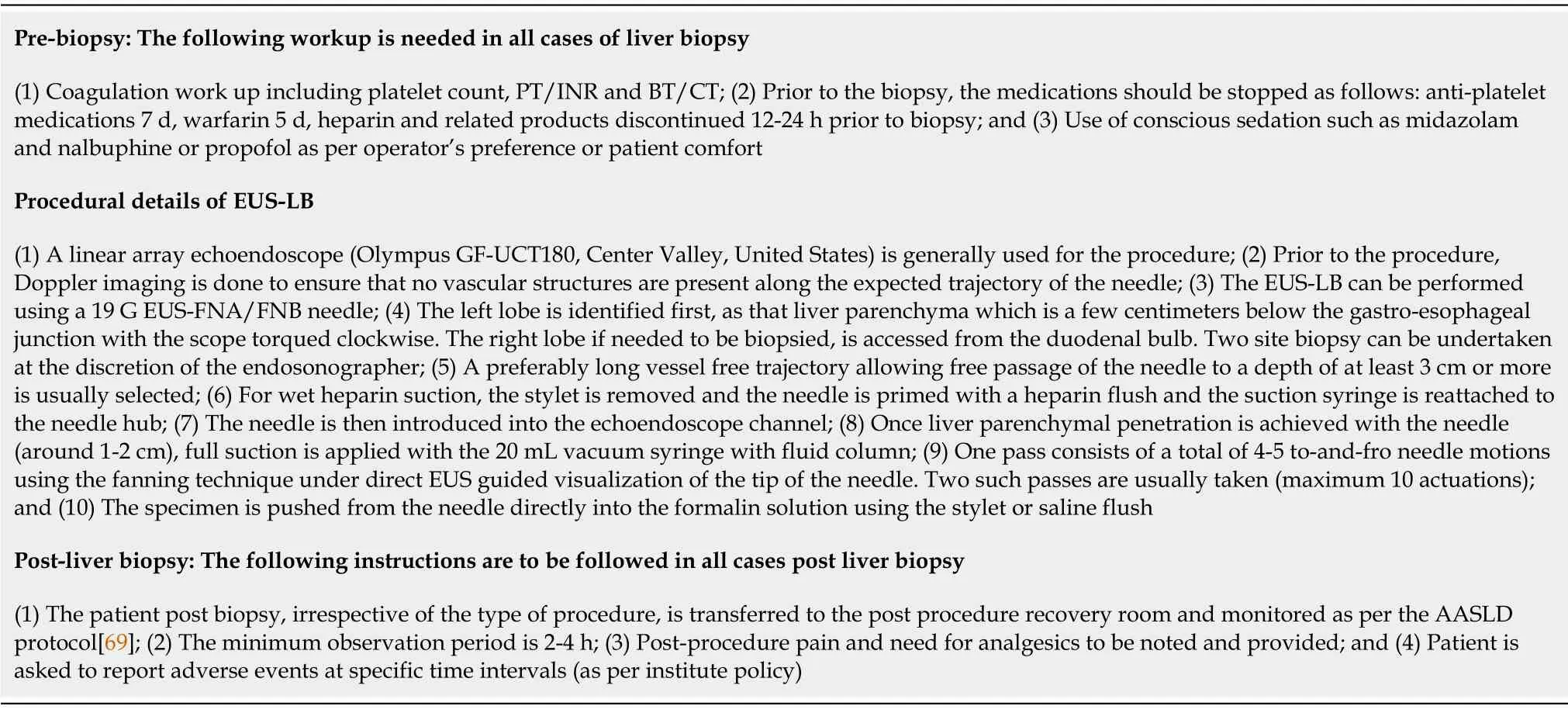
Table 5 Technique of endoscopic ultrasound guided liver biopsy[50,51]
EUS guided drainage of liver abscess:Traditionally,pyogenic and amoebic liver abscesses have been drained by PCD with a high technical success rate.However,EUS guided drainage of liver abscesses is a promising new approach,especially for difficult-to-reach locations.Additionally,the advantage of internal drainage with a single-step procedure and easy access from the stomach makes transmural drainage of left and caudate lobe abscess convenient.
The technique was first described by Seewaldet al[72],who reported complete resolution 4 weeks post-procedure.Literature on EUS guided drainage is limited to retrospective case series only in which the majority have been drained with double pigtail plastic stents[73-75].Recently,data are emerging on the use of fully covered self-expandable metal stents(SEMS)[76]for the same.Oguraet al[77]reported retrospective comparative data on EUSvsPCD guided abscess drainage wherein EUS guided abscess drainage(EUS-AD)cases showed greater clinical success(100%vs89%)with shorter hospital stay(21 dvs41 d).Studies on EUS-AD are listed in Supplementary Table 3.
EUS guided drainage of biloma:Biloma is defined as a well-demarcated collection of bile outside the biliary tree,which can be extrahepatic or intrahepatic,encapsulated or without a capsule[78].It is most frequently caused by iatrogenic biliary tree injury during cholecystectomy.It has been traditionally managed with PCD or surgery.However,large bilomas in opposition to the gastric wall can be taken up for transmural drainage(Figure 8).Similar to EUS-AD,earlier plastic stents were utilized for the same,but now SEMS has been in vogue for biloma drainage with excellent results.Post drainage,such patients should be evaluated to determine the need for endoscopic retrograde cholangiopancreatography,or sphincterotomy with/out biliary stenting or surgery[79].Studies on EUS guided drainage of bilomas are described in Supplementary Table 4.
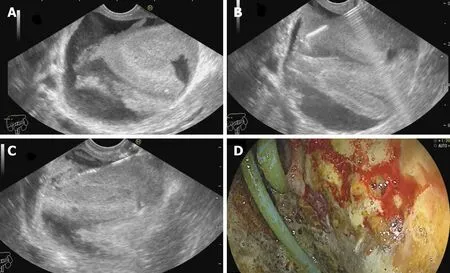
Figure 8 Endoscopic ultrasound-guided drainage of biloma.A:Post-operative biloma noted on endoscopic ultrasound(EUS)with internal echoes;B:EUS-guided puncture of the biloma;C:Guidewire negotiated into the collection followed by placement of naso-cystic drain;D:Endoscopic view of the cavity entered with catheter noted in situ.

Table 6 Studies on endoscopic ultrasound guided fine needle aspiration guided and endoscopic ultrasound guided fine needle biopsy guided liver biopsy in patients with chronic liver disease
Despite it being a point of contention,EUS guided drainage of intrahepatic lesions(cysts,abscesses and bilomas)is an upcoming promising technique and may be considered in conditions where PCD is not amenable or has failed.
EUS guided treatment of liver tumors
A thrilling offshoot of EUS guided therapeutic interventions has been EUS guided local treatment of tumor lesions(both pancreatic and hepatic tumors)[80].EUS-guided tumor management is a new experimental application that has shown promise in reaching difficult lesions(left lobe,caudate lobe),provided a rescue option in refractory cases,and has potential to improve quality of life by minimizing systemic side effects[81,82].This procedure has been extensively studied in cases of pancreaticneoplasm,but its role in hepatic tumors(primary or metastatic)is still in its infancy.
Various techniques of EUS guided liver tumor management have been described.
Fine needle injection therapy:Ethanol ablation
Percutaneous injection of ablative injections is most commonly used worldwide to manage HCC,although EUS guided fine needle injection can be performed using acetic acid or ethanol(pure alcohol 95%-99%)[83].Its advantage is that it enables realtime imaging during delivery of ethanol to the tumorous lesion and thus can help avoid collateral damage.
Initial case reports using 22 G and 25 G FNA needles have been reported with excellent technical success and complete resolution of HCC[84-87].For example,Nakajiet al[87]reported a high-resolution rate at 31 mo in 12 cases of caudate lobe HCC,whereas Jianget al[88]only showed 30% complete resolution at 12 mo.This technique has also been evaluated for the treatment of hepatic metastasis from pancreatic adenocarcinoma[89].
Thermal ablative therapy
Radiofrequency ablation:Radiofrequency ablation(RFA)uses a high-frequency alternating current(375 kHz to 500 kHz)and is minimally invasive with good tolerability[90].It can be delivered percutaneously,intraoperatively,viaan endoluminal approach or endosonographic(transmural)route.Emerging data on the latter have resulted in its application in cases wherein the percutaneous approach fails.Obesity,tumor nodules in the left lobe or caudate lobe,deep-seated and subcapsular/sub-diaphragmatic lesions that carry an inherent risk of hemothorax or pleural effusion are some of the conditions where it has been applied[81,90].A specifically designed needle tip electrode for performing EUS-RFA(EUSRA RFA Electrode,STARmed,Koyang,Korea)with a designed internally cooled needle electrode is the most extensively studied.Only a few case reports exist on EUS-RFA using EUSRA in HCC[91-93].Also,hybrid models combining EUS-RFA with cryoablation in the bovine liver have demonstrated better efficacy of the combination treatment[94].
Laser ablation by neodymium:yttrium-aluminum-garnet:Neodymium:yttriumaluminum-garnet(Nd-YAG)is a type of LITT(laser interstitial thermotherapy)wherein laser waves are introduced through the EUS needle directly into the tumor tissue leading to cell apoptosis and eventual necrosis.Only two human studies have been published so far for the treatment of HCC.Di Matteoet al[95]reported complete HCC resolution in 2 mo in a case of previously failed caudate lobe HCC.Similarly,Jianget al[96]reported resolution at 3 mo with an encouraging safety profile.
Cryotherapy ablation:Cryotherapy ablation(CYA)destroys tissue through multiple freezing-thawing cycles leading to osmotic dehydration and injury to the intracellular structures and cell death[90].No human study exists for its use in liver lesions.However,a single animal study showed the efficacy of a hybrid EUS-RFA and cryoderm device in a porcine model[97].
High-intensity focused ultrasound:This is a non-invasive technique that causes tissue necrosisviaheat generation and acoustic cavitation by the formation and collapse of bubbles produced by intense USG waves[90].Its use in EUS has only been tested in animal models[98,99],showing complete necrosis of the lesions with no immediate side effects.
Brachytherapy
This treatment modality has been used for various cancers with the advantage of less toxicity to surrounding tissues over external beam radiotherapy[81,90].For example,EUS guided brachytherapy with permanent seed placement of Iodine(I125)or palladium(Pd103)has been performed for head-neck,esophageal,and pancreatic cancer[100-102].In addition,Jianget al[88]have used EUS guided I125 seed implantation for liver tumors with high efficacy and safety.
Studies on EUS guided liver tumor treatments are outlined in Table 7.
EUS GUIDED VASCULAR INTERVENTIONS
The presence of real-time,high-resolution sonographic imaging with Doppler,along with the relative proximity of the gastrointestinal tract to the major blood vessels in the abdomen and the mediastinum,has led to a growing interest to explore the role of EUS in the field of vascular interventions.EUS may be preferred over the percutaneous route,especially in obesity,ascites and overlying distended bowel[104].
Esophageal and gastric varices:diagnosis and management
EUS guided vascular intervention in patients with PHTN has been well established in managing varices(esophageal,gastric,duodenal,and ectopic).
Management of esophageal varices:Endoscopic variceal band ligation(EVL)has been the standard treatment of esophageal varices(EV)(both primary and secondary prophylaxis).However,re-bleeding rates of 15%-65% have been reported due to the failure to obliterate perforating veins and collaterals feeding the varices[105].Lahotiet al[106]described the first report of EUS guided sclerotherapy in 5 cases,wherein sclerosant(sodium morrhuate)was injected under EUS guidance(2-4 mL per injection site)directed at the perforating vessels as determined by color Doppler with complete eradication of the varices.An RCT comparing EUSvsdirect sclerotherapy revealed no difference in both arms[107].Thus,although EUS carries a theoretical advantage for identifying the feeders,more studies are needed to assess its practical clinical benefit.
Management of gastric varices:In patients with PHTN,gastric varices(GV)are present in up to 20% with a 50%-65% re-bleeding rate[108].Endoscopic injection of CYA glue for GVs has been the treatment of choice since its first description in 1986 but is still prone to a re-bleeding rate of 40%[109].In the current era of EUS guided vascular interventions,management of GVs by EUS has many conceptual advantages,both diagnostic and therapeutic such as[110,111]:(1)A higher detection rate(6 times)over conventional endoscopy;(2)Greater success in differentiating varices from thick gastric folds;(3)Confirmation of the cessation of blood flow post-treatment;(4)Realtime varix visualization and hence accurate delivery of hemostatic agent to the varix;and(5)Targeted treatment for feeder vessels.
The first description of EUS guided CYA injection in GVs was given by Romero-Castroet al[111]and Leeet al[112].To reduce the chances of embolization with CYA,stainless steel coils alone or in combination with CYA glue have been introduced.The advantage is three-pronged:additive hemostasis and varix obliteration,reducing the volume of glue needed and acting as a scaffold to retain the glue within the varix,thereby decreasing embolization.Various studies,including RCTs,have favored coil over glue.Bhatet al[113]reported a complete obliteration in 93% with only 3% rebleeding rates using coils and glue combination.Similarly,two RCTs and a metaanalysis have reported the combination therapy of coil with glue to be superior to either agent alone[114-116].Newer treatments of utilizing coils with gelatin sponge and sclerotherapy or isolated thrombin injection have been reported in various case series and have shown good results[117-119].
The technical steps of the EUS guided coil and glue placement for the obliteration of GV are outlined in Table 8 and Figure 9.
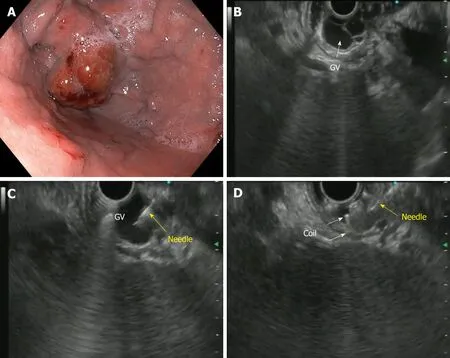
Figure 9 Endoscopic ultrasound-guided coil embolization of fundal varix.A:Endoscopic view of the fundal varix;B:Endoscopic ultrasound(EUS)view of the fundal varix;C:EUS guided puncture of the varix with a 22-G needle;D:Coil deployment inside the varix.GV:Gastric varices.

Table 7 Studies in humans demonstrating the role of endoscopic ultrasound guided therapies for liver lesions

Table 8 Steps of endoscopic ultrasound guided coil and glue placement for gastric varices obliteration
Use of EUS in the prediction of re-bleeding from EV/GV:EUS with Doppler has a higher sensitivity for detecting esophageal and GV than upper GI endoscopy and can also be used to predict re-bleeding.Certain parameters can help guide us in this direction[120,121]:(1)EUS can help in demonstrating collaterals or feeders,a strong indicator to a future occurrence of a re-bleed;(2)Hematocystic spots on EVs identifiedas saccular aneurysms on EUS is associated with a high risk of variceal rupture;(3)Digital image analysis on EUS can help to determine the cross-sectional area of EVs in the distal esophagus and a cutoff of 0.45 cm2has a sensitivity of 83% for future rebleeding;and(4)Para-esophageal diameter after EVL is a better recurrence predictor
(cutoff 4 mm has a 70.6% sensitivity).
Thus,there is a huge prospect for using EUS in PHTN,namely in the evaluation of vascular changes of the digestive wall,hemodynamic assessment by measurement of PV pressure gradient,management of variceal bleeding and re-bleeding prediction and currently liquid biopsyviaPV sampling.Nonetheless,despite the diversity of possible uses,more data on efficacy and safety are warranted.
EUS guided PV access
The PV can be accessed from both the stomach and duodenum and is in very close juxtaposition with the tip of the echoendoscope.The most frequent location to target is the intrahepatic PV through the hepatic parenchyma.The other less commonly used technique is the extrahepatic PVviathe duodenum[122,123].
Technique of the procedure:After confirming the vascular structure with color Doppler and pulse-wave verification,PV puncture is doneviathe EUS-FNA needle.Studies have shown that 25 G needle causes the least trauma.The trans-gastric,transhepatic approach is safer than the trans-duodenal approach.CO2 is better than using iodine as a contrast(allows better PV visualization and easier intravascular administration through the small-caliber FNA needle).After PV puncture,on withdrawal of the needle,the track is monitored with color Doppler to check for bleeding.In cases of blood flow being identified,the needle is kept in place until the flow has stopped[122,123].
Animal studies:The first case of PV access was reported in 2004 by Laiet al[124],wherein a EUS guided trans-duodenal access to extrahepatic PV was adopted with a 22 G FNA needle in 21 swine models,proving the technical feasibility of the procedure.Thereafter,PV angiography was reported for the first time in 2007 by Magnoet al[125],wherein autopsies revealed no injuries with a 25 G needle and a hematoma with 19 G needle.Subsequently,Gidayet al[123,126]reported trans-hepatic access to the PV with a 25 G needle.
EUS guided portal pressure gradient measurement
Measurement of PHTN is useful in determining the stage,progression,prognosis and complications of cirrhosis.Currently,the standard practice of measuring the portal pressure gradient(PPG)is the percutaneous route.However,both direct PV access and hepatic venous pressure gradient(HVPG)measurement are invasive procedures and have high complication rates.Moreover,HVPG correlated poorly in presinusoidal PHTN cases.Therefore,EUS guided PPG can be performed to overcome these difficulties.Moreover,additional analyses such as assessment of varices and liver biopsy can be carried out in the same sitting.The technique of PPG measurement and the studies(human and animal models)on the same are shown in Supplementary Tables 5 and 6.
EUS guided TIPS
TIPS has an established role in managing PHTN-related complications like variceal bleeding(pre-emptive or rescue)and refractory ascites.EUS-guided TIPS creation in a live porcine model(8 cases)was first described by Buscagliaet al[127],wherein the hepatic vein(HV)and PV were sequentially punctured,and a metal stent was inserted with the distal end in the PV and proximal end in the HV.In addition,Binmoeller and Shah[128],and Schulmanet al[129]have both reported using a lumen apposing metal stent(LAMS)in porcine models for the same purpose.
EUS guided PV sampling
“Liquid biopsy” for hepatobiliary malignancies is gaining momentum in view of the PV harboring circulating tumor cells(CTCs)from the primary tumor.These CTCs are the forerunners of future metastasis of solid organ cancers and help predict the development of liver metastasis[130].They have been inconsistently found in the peripheral blood due to hepatic sequestration.They reflect tumor signature,help in prognostic stratification,and potentially form organoids for future tumor study.
Catenacciet al[131]reported the first human study of PV sampling wherein a 19 G FNA needle was used to sample the PV as four 7.5 mL aliquots of blood.CTCs were detected in 100% cases from the PVvs4(22.2%)cases from peripheral blood.Liuet al[132]reported similar findings in cases of advanced pancreatic cancer(100% detection of CTCs in PVvs54% in peripheral blood).Besides these,further studies are needed to establish the clinical utility of EUS guided liquid biopsies.
EUS guided FNA of PV thrombosis
The presence of malignant PV thrombosis(PVT)usually portends a poor prognosis.Therefore,differentiating bland and malignant thrombus needs FNA confirmation.Various case reports have suggested the use of EUS guided FNA of the PVT by overcoming the complications encounteredviathe percutaneous route[133-135]with excellent results.
EUS guided PV injection chemotherapy
Both systemic palliative chemotherapy and transarterial microbead injection into the hepatic artery for diffuse liver metastasis are fraught with complications.However,Faigelet al[136]reported the feasibility of EUS guided PV injection chemotherapy in 24 porcine models using drug-eluting microbeads and nanoparticles.In comparison with systemic injection,systemic levels were halved,but the hepatic concentration of drugs was doubled.Human studies are warranted for the same.
EUS guided PV embolization
Preoperative PV embolization before liver resection in hepatobiliary malignancies induces affected lobe atrophy and ultimately hypertrophy in the functional liver[137].However,preliminary studies in the animal model by Mattheset al[138]and Parket al[139]using EUS guided PV embolization using ethylene-vinyl alcohol copolymer and coil with CYA glue embolization,respectively,reported high success rates.
EUS guided PV stent placement
EUS directed PV access has opened up avenues for stent placementviathis route in PV occlusion or thrombosis.Parket al[140]reported 100% technical success(all uncovered stents)in 6 swine models.
FUTURE ADVANCES
Photodynamic therapy
Photodynamic therapy(PDT)is a commonly used modality for treating malignant biliary obstruction,requiring pretreatment with a photosensitizer followed by exposure to selective tissue wavelength of light-generating singlet oxygen species(tissue necrosis from 6-40 mm depth)[141].Preliminary animal studies exist on the use of EUS guided PDT on the porcine pancreas[141,142]and pancreaticobiliary malignancies(with lesions in the caudate lobe)[143].
EUS guided fiducial marker placement
Stereotactic body radiation therapy demands high targeting accuracy to minimize toxicity to surrounding organs.Placement of fiducial markers can help localize and track the target and can be placedviaa percutaneous or surgical approach.EUS guided fiducial marker placement has come into the forefront for targeting even deeper abdominal lesions not amenableviastandard means[144,145].However,no studies exist on its use in liver malignancies.
Artificial intelligence
Artificial intelligence(AI)is a prediction technique using mathematical algorithms to create automated learning and recognize patterns in the fed data.Artificial neural network(ANN)and deep learning(DL)are powerful machine-learning-based tools used to provide high yield predictions and are being used more and more in the medical field to aid in diagnosis.Just like its widespread use in the field of endoscopic diagnosis of polyps and other lesions,AI has also found its place in the arena of diagnostic EUS.Studies have used ANN for the interpretation of EUS-elastography and CE-EUS[146].However,to date,only two studies have used DL for EUS image analysis.With the availability of additional studies,AI can add to the diagnostic armamentarium of EUS and lead to much better accuracy.
CONCLUSION
Hepatologists have always turned to radiologists for imaging and intervention of various liver-related conditions.However,with the expansion of this intersection of endoscopy in EUS and hepatology,the field of “Endo-hepatology” may soon evolve into a sub-specialty with hepatologists trained in interventional EUS.Starting from EUS-guided liver biopsy to PV interventions,the merger of EUS and hepatology seems to show invigorating scope in the future.However,more studies are needed to establish the safety and efficacy of these newer modalities in regular mainstream practice.
杂志排行
World Journal of Hepatology的其它文章
- Incidence of umbilical vein catheter-associated thrombosis of the portal system:A systematic review and meta-analysis
- Porta-caval fibrous connections—the lesser-known structure of intrahepatic connective-tissue framework:A unified view of liver extracellular matrix
- Promising diagnostic biomarkers of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis:From clinical proteomics to microbiome
- Fatty acid metabolism and acyl-CoA synthetases in the liver-gut axis
- Liver involvement in inflammatory bowel disease:What should the clinician know?
- Chelation therapy in liver diseases of childhood:Current status and response
