Anthropometric method for estimating component sizes in total hip arthroplasty
2021-11-22RajpreetSahemeyThomasMooresHannahMeacherBishoyYoussefShehzaadKhanChristopherEvans
Rajpreet Sahemey, Thomas S Moores, Hannah Meacher, Bishoy Youssef, Shehzaad Khan, Christopher R Evans
Rajpreet Sahemey, Department of Trauma and Orthopaedics, University Hospitals Coventry and Warwickshire, Coventry CV2 2DX, United Kingdom
Thomas S Moores, Department of Trauma and Orthopaedics, Walsall Manor Hospital, Walsall WS2 9PS, United Kingdom
Hannah Meacher, Bishoy Youssef, Department of Trauma and Orthopaedics, Royal Stoke University Hospital, Stoke-on-Trent ST4 6QG, United Kingdom
Shehzaad Khan, Department of Trauma and Orthopaedics, Royal National Orthopaedic Hospital, Stanmore HA7 4LP, United Kingdom
Christopher R Evans, Department of Orthopaedics, The Robert Jones and Agnes Hunt Orthopaedic Hospital, Oswestry SY10 7AG, United Kingdom
Abstract BACKGROUND Preoperative templating is essential in total hip arthroplasty (THA) as it not only helps to facilitate the correct implant type and size but also determines the postoperative biomechanics. Templating is also increasingly important from a medicolegal perspective and recommended in the British Orthopaedic Association Guide to Good Practice. Although templating has become increasingly digitised, there are no simple anthropometric models to predict implant sizes in the absence of digital methods.AIM To assess the accuracy of using an easily obtainable measurement (shoe size) to predict component sizes in THA compared with digital templating.METHODS Digital radiographs from a cohort of 102 patients (40 male, 62 female) who had undergone uncemented or hybrid THA at a single centre were retrospectively templated to desired cup and stem sizes using TraumaCad®. We compared the templated size to the actual size of the implant and assessed if there was any correlation with the patient’s shoe size.RESULTS Statistically significant positive correlations were observed between: shoe size and templated cup size (ρ = 0.92, P < 0.001); shoe size with implanted cup size (ρ = 0.71, P < 0.001); shoe size and templated stem size (ρ = 0.87, P < 0.001); and shoe size with implanted stem size (ρ = 0.57, P < 0.001). Templated and implanted acetabular cup sizes were positively correlated (ρ = 0.76, P < 0.001) and were exact in 43.1% cases; 80.4% of implanted cup sizes were within 1 size (+/- 2 mm) of the template and 100% within 2 sizes (+/- 4 mm). Positive correlation was also demonstrated between templated and implanted femoral stem sizes (ρ = 0.69, P < 0.001) and were exact in 52.6% cases; 92.6% were within 1 size of the template and 98% within 2 sizes.CONCLUSION This study has shown there to be a significant positive correlation between shoe size and templated size. Anthropometric measurements are easily obtainable and can be used to predict uncemented component sizes in the absence of digital methods.
Key Words: Anthropometric; Digital templating; Hip; Preoperative planning; Total hip arthroplasty
INTRODUCTION
Accurate preoperative templating is an essential step in total hip arthroplasty (THA) and is recommended by the British Orthopaedic Association’s Best Practice for Hip Arthroplasty[1]. Templating has proven to be effective in selecting the correct implant size, optimisation of biomechanics such as leg length discrepancy, centre of rotation and alignment. Furthermore, preoperative planning has been well documented to improve component stability, reduce the operative time and minimise wear due to implant malposition[2].
Alongside the widespread introduction of digital radiography throughout the United Kingdom, preoperative templating of THA has become increasingly digitised with several software products currently on the market. However these software packages may not be universally available and are dependent on the user’s training and level of surgical experience[3]. Digital templating and computer-navigated surgery have been used to improve the quality and outcomes of THA however these methods can be expensive and may not be a feasible option for some departments.
Preoperative estimations of implant sizes may be useful for resource-scarce departments as it allows for better organisation of hospital funds by reducing the number of excess implants “on the shelf”[4]. Shoe size is an easily obtainable and costfree anthropomorphic measurement, which is a reliable reflection of foot length, overall longitudinal growth and stature[5,6]. We propose preoperative shoe size as a simple measurement tool for predicting component sizes for primary uncemented THA. The aim of this study is to determine the accuracy of using this measurement as an estimator for acetabular cup and femoral stem sizes when compared with digitally templated sizes for the same hip.
MATERIALS AND METHODS
Patients
A retrospective, single-centre cohort study was performed for patients who had received primary uncemented or hybrid THA for osteoarthritis between October 2015 and October 2016. Patients were excluded if they had a body mass index (BMI) greater than 35; had undergone previous foot and ankle surgery; diagnosed with foot or ankle disease; noted a change in shoe size during adulthood or if they required a complex primary arthroplasty. Cemented components of hybrid THA were also excluded. A total of 102 acetabular cups and 95 femoral stems from 102 consecutive patients were included in the final analysis, comprising of 40 men and 62 women. The mean age of the study group was 69.9 ± 10.9 years (range 33-90) and mean BMI 32 ± 3.6 (range 20.2-39.0). All THAs were performed by a single surgeon and using a posterior approach to the hip. The uncemented components implanted were the POLAR R3 cup and POLARSTEM stem (Smith & Nephew, Memphis, TN, United States). Implant sizes were recorded along with the corresponding patient’s standard United Kingdom shoe size at the time of surgery. Shoe sizes ranged from 3 to 11. Institutional Review Board approval was not required in accordance with the United Kingdom National Research Ethics Service guidance on the use of anonymised data collected retrospectively as part of routine clinical care.
Radiographs and templating
Preoperative anteroposterior (AP) digital pelvic radiographs were obtained for all patients using a standard protocol (Figure 1) with the feet internally rotated at 15 and the X-ray beam centered on the superior margin of the symphysis pubis[7]. All patient identifiers were removed from radiographs and replaced by unique sequential numbers before being imported into TraumaCad®(Brainlab, United States) for calibration and templating. Each component was digitally templated to a desired size in a manner as described by Bono[8], by two orthopaedic surgeons who were familiar with the software (Figure 2). A third examiner (senior surgeon) reviewed all size discrepancies and a final decision was achieved by consensus. All examiners were blinded to the actual size of the implanted components.

Figure 1 Standardised anteroposterior pelvic radiograph.
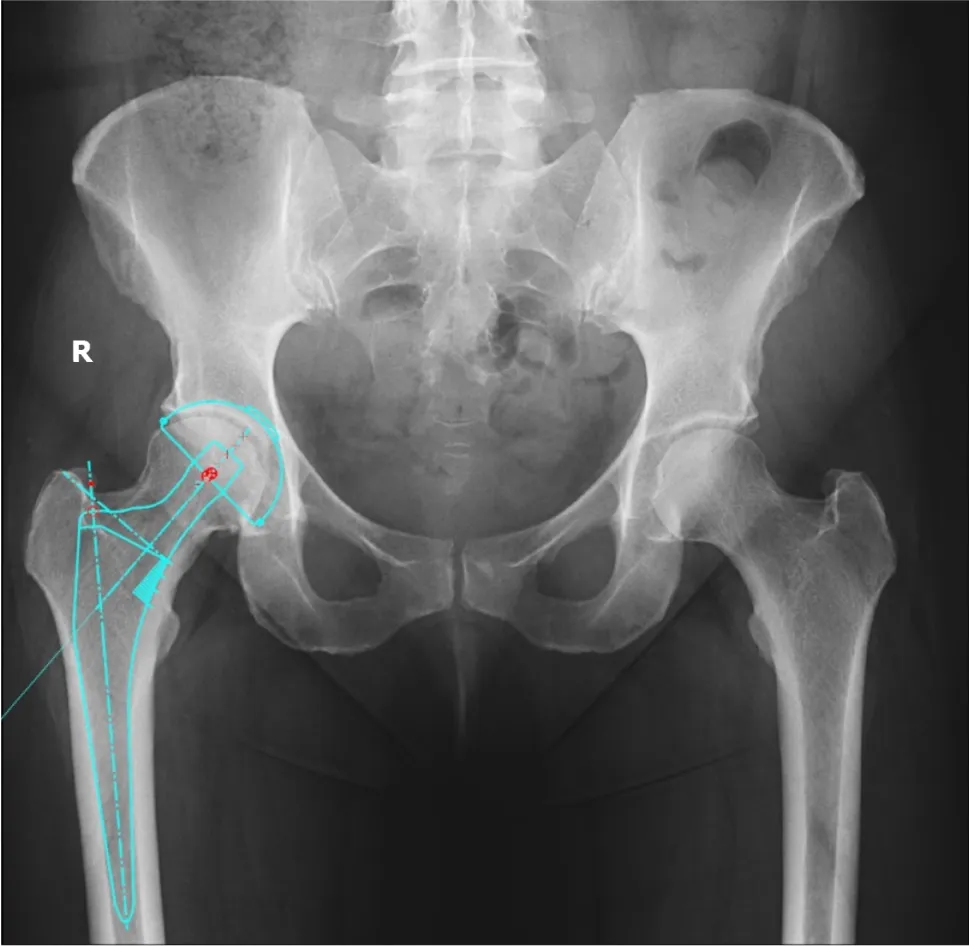
Figure 2 Digital templating using TraumaCAD®.
Statistical analysis
The Spearman’s rank correlation coefficient (ρ) was used to assess the correlation between the patient’s shoe size with: (1) Templated component size; and (2) Implanted component size; and if there was any difference between templated and implanted sizes. APvalue of < 0.05 was considered to be statistically significant. Statistical analysis was performed with SPSS v22.0 (IBM, Armonk, NY, United States). By analyzing any observed relationships we intended to produce a table for estimating the component size from the patient’s shoe size.
RESULTS
Statistically significant positive correlations were observed between: shoe size and templated cup size (ρ = 0.92,P< 0.001); shoe size with implanted cup size (ρ = 0.71,P< 0.001); shoe size and templated stem size (ρ = 0.87,P< 0.001); and shoe size with implanted stem size (ρ = 0.57,P< 0.001). Correlation coefficients based on gender subgroups are presented in Table 1. Templated and implanted acetabular cup sizes were exact in 43.1% cases, 80.4% of implanted cup sizes were within 1 size (+/- 2 mm) of the template and 100% were within 2 sizes (+/- 4 mm). Templated and implanted femoral stem sizes were exact in 52.6% cases, 92.6% were within 1 size of the templateand 98% were within 2 sizes. Statistically significant positive correlations were observed between implanted cups (ρ = 0.76,P< 0.001) and stems (ρ = 0.69,P< 0.001) from their templated sizes. Predicted component sizes from shoe size, adjusted for sex, are presented in Table 2.
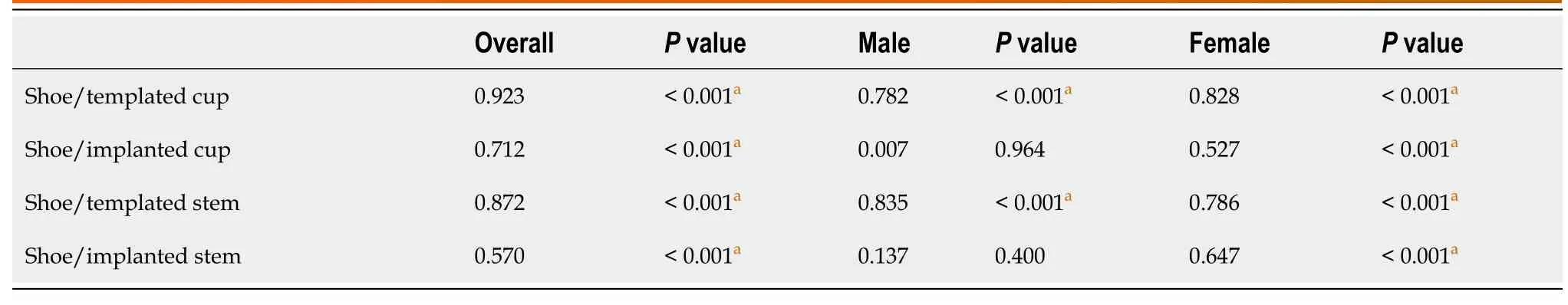
Table 1 Subgroup correlation coefficients (Spearman’s rank)
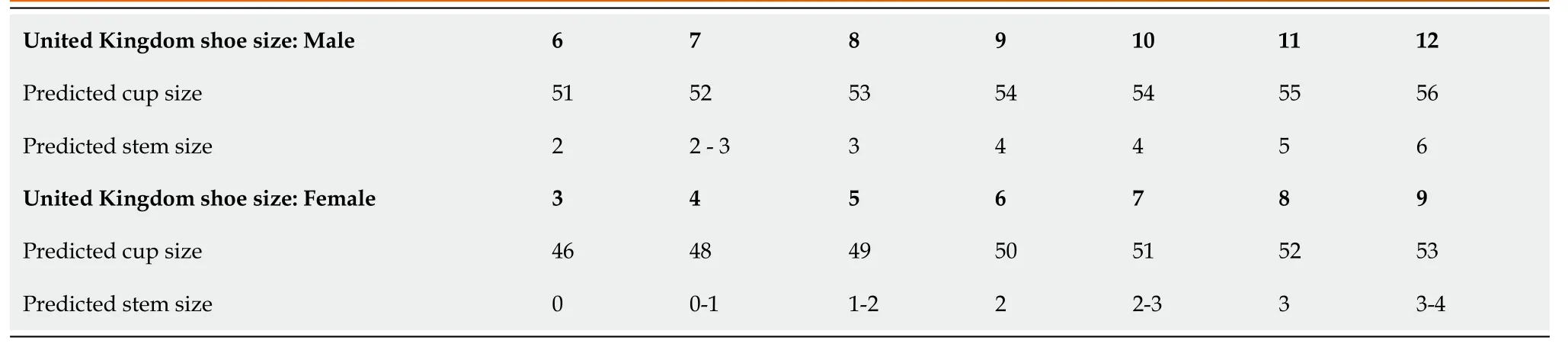
Table 2 Quick reference table
DISCUSSION
Templating is an important step prior to performing a total hip replacement, as there has shown to be a greater risk of prosthesis failure if components are inadequately sized[9]. Accurate templating should form part of the routine preoperative assessment and is not only recommended by the British Orthopaedic Association Guide to Best Practice[1] but is also associated with reduced operative time and fewer complications[10]. Preoperative planning encourages surgical precision by accounting for femoral offset restoration, leg length correction and implant alignment[2]. Analogue templating using manufacturer acetates has become incompatible since the widespread introduction of digital radiography throughout all acute hospitals in the United Kingdom. As a result templating has become digitised and allows the user to accurately calibrate the magnification and sizing of the radiograph.Predicting implant sizes can enable orthopaedic purchasing departments to procure accurate stock volumes. This is an important factor when considering the cost and shelf life of expensive implants.
Recent studies have proposed the use of 3D computed tomography (CT) and magnetic resonance imaging with reports of up to 100% predictive accuracy for templating cup size and orientation when compared with 2D templating from digital radiographs[11,12]. However, Westacottet al[13] further observed that CT scans areperformed with the subject supine and therefore do not represent the functional position of the pelvis when the subject is standing. Consequently the pelvic obliquity due to tilt and leg length discrepancy will change the abduction angle and version when standing and may not provide the optimum functional position of the implants. Nonetheless, templating software is expensive and may not be readily available in all orthopaedic departments due to local hardware, software and financial constraints. Surgeons may also wish to avoid the additional radiation risk and cost burden associated with routine preoperative CT scanning for all their patients.
The precision of digital templating is dependent on the quality, rotation and magnification of radiographs. Various methods have been developed, notably the KingMark®, in an effort to calibrate digital radiographs for accurate templating[14]. For patients with advanced degenerative arthritis it may not be possible to obtain a good quality radiograph. In such cases the templating can be performed on the contralateral hip though in patients with bilateral deformities, this process becomes less reliable. Templating relies on the subjective decision of the examiner and can be affected by their level of surgical experience and familiarity with templating software. As a result there are varying degrees of intraobserver reliability reported in the literature[11,15].
Similar to our study findings, the difference in sizes between predicted and implanted uncemented prostheses are well documented in THA, as these implants require an element of under-reaming for press-fit fixation[16]. Consequently, surgeons may opt for a smaller than templated prosthesis size to avoid intraoperative fracture if they feel that stability has been achieved. Furthermore, some hip systems such as the POLARSTEM are designed to be impacted into a compacted cancellous bone bed for fixation. As a result post-operative radiographs may reveal an approximately 1 mm radiolucent line between the stem and the inner cortex, which represents this cancellous layer[17].
In this study we chose shoe size as a non-invasive, fast and harm-free measurement as a predictor for stature[6]. Recent studies have also demonstrated a significant positive correlation between shoe size and component size in total knee arthroplasty with up to 80% predictive accuracy[18,19]. To date, a similar correlation has not been described for THA in the current literature. Unlike height or weight, foot length does not change significantly during adulthood[20]. Collective evidence from forensic literature advocates that shoe size can reliably predict both skeletal foot size and the overall height of the individual[5,6]. The standard United Kingdom shoe size arises from the longitudinal length of the ‘last’, which is the physical template over which a shoe is manufactured[19]. As each person determines which shoe size provides the best fit it therefore follows that the individual knows his or her size accurately. In the outpatient setting shoe size is a readily obtainable value and doesn’t require additional measurement aids such as for height or weight, which may not be easily available. We further propose a simple conversion table to enable the surgeon to make a quick estimation for the required component sizes from both male or female shoe sizes (Table 2).
We acknowledge several limitations in our study. Our modest sample size was comparable to those in mentioned in the literature though it was not large enough to calculate predictive rules pairing unique shoe sizes to their exact component sizes. This study investigated United Kingdom shoe sizes and therefore the relationships described may not translate to some countries. Patients with a history of foot and ankle surgery were excluded from this report as the dimensions of the foot may change in adulthood secondary to deformity such as hallux valgus. However, Sawalhaet al[19], in their series of 93 knee replacements did not see any change in accuracy of predicting component size from shoe size when patients with foot pathology or history of foot surgery were included. This would indicate that shoe size is a reliable predictor of component size in all patients irrespective of foot pathology. Our sample size excluded cemented implants, which may limit the broader application of our reported results to cemented hip systems. Finally, the authors appreciate the increasing worldwide use of templating software and computer navigated arthroplasty surgery. However like many other departments, templating software licences are often limited to the operating theatre suites and may not readily be available in the outpatient setting when consulting patients. The proposed advantage of an anthropometric predictive model allows for easy, rapid component size estimation in the absence of computer software and may have a role in allowing purchasing departments to procure accurate stock levels well in advance of planned arthroplasty procedures.
CONCLUSION
In conclusion, our study shows there to be a strong positive correlation between shoe size and templated component sizes in primary uncemented THA. This relationship may allow surgeons to confidently predict component sizes in the absence of digital templating.
ARTICLE HIGHLIGHTS
Research background
Preoperative templating is an essential in total hip arthroplasty (THA) as the correct size and orientation of components play a key role in the success of the prosthesis.Templating is becoming digitised yet many orthopaedic departments lack access to software due to cost and resources.
Research motivation
Available evidence surrounding the correlation between a patient’s shoe size and knee arthroplasty component sizes suggests reliable positive correlations. Our motivation for this study was to assess if there was a reliable anthropometric method to predict THA component sizes from shoe size in the absence of digital methods.
Research objectives
We aim to determine the accuracy of using an easily obtainable measurement (shoe size) to predict component sizes in THA when compared with the digitally templated sizes of the same hip.
Research methods
We performed a retrospective review of 102 patients (40 male, 62 female) who had undergone elective uncemented or hybrid THA at our single centre. Standardised digital pelvic radiographs were retrospectively templated to desired cup and stem sizes using TraumaCad®. We then compared the templated size to the actual size of the implant that the patient received and assessed if there was any correlation with the patient’s shoe size.
Research results
Statistically significant positive correlations were observed between patient shoe size: templated cup and implanted cup size; templated stem and implanted stem size. Positive correlations were also demonstrated between templated and implanted acetabular cup sizes, and templated and implanted stem sizes.
Research conclusions
Our study has shown there to be strong positive correlations between shoe size and templated component sizes in primary uncemented THA. Shoe size is an easily obtainable measurement and can allow surgeons to confidently predict component sizes in the absence of digital templating.
Research perspectives
Future research should evaluate the clinical significance of these findings with cemented hip systems.
杂志排行
World Journal of Orthopedics的其它文章
- Management of acute length-unstable Monteggia fractures in children: A case report
- Spontaneous pneumothorax in a 17-year-old male patient with multiple exostoses: A case report and review of the literature
- Pathological humerus fracture due to anti-interferon-gamma autoantibodies: A case report
- Allergic dermatitis after knee arthroscopy with repeated exposure to Dermabond Prineo™ in pediatric patients: Two case reports
- Role of coatings and materials of external fixation pins on the rates of pin tract infection: A systematic review and meta-analysis
- Femoral lengthening in young patients: An evidence-based comparison between motorized lengthening nails and external fixation