Clinical, biochemical and imaging characteristics of adrenal histoplasmosis in immunocompetent patients in a non-endemic area: A case series
2021-11-19SharminJahanTahseenMahmoodMdFariduddinIbrahimFaisalMdShahedMorshedAnilYadavAnilKumarShahChomonAbdullahEmranUrRashidChowdhuryFerdousiBegumMAHasanat
Sharmin Jahan, Tahseen Mahmood, Md Fariduddin, Ibrahim Faisal, Md Shahed Morshed, Anil Yadav, Anil Kumar Shah, Chomon Abdullah, Emran-Ur-Rashid Chowdhury, Ferdousi Begum, MA Hasanat
1Department of Endocrinology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
2Department of Endocrinology, Combined Military Hospital, Dhaka Cantonment, Dhaka, Bangladesh
3Division of Endocrinology, Department of Internal Medicine, Indira Gandhi Memorial Hospital, Kanbaa Aisa Rani Higun, Male'- 20402, Republic of Maldives
4Department of Emergency, Kurmitola General Hospital, Dhaka, Bangladesh
5Division of Endocrinology, Department of Internal Medicine Birat Medical College Teaching Hospital, Biratnagar, Nepal
6Division of Endocrinology, Department of Internal Medicine, Chitwan Medical College, Chitwan 44300, Nepal
7Department of Pathology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
ABSTRACT
KEYWORDS: Histoplasmosis; Immunocompetent; Nonendemic;Adrenal CT
Significance
Most cases of adrenal histoplasmosis have been reported in immunocompromised individuals residing in endemic areas.This article describes clinical, biochemical and imaging characteristics of 18 immunocompetent patients from a nonendemic area (Bangladesh) who presented with primarily adrenal involvement with few pulmonary symptoms. In most cases of bilateral adrenomegaly, the patients are initially misdiagnosed and treated as tuberculosis in non-endemic areas where high index of suspicion is required for correct diagnosis of histoplasmosis.
1. Introduction
Disseminated histoplasmosis is an infrequent but potentially fatal disease caused by dimorphic soil fungus Histoplasma capsulatum[1].During dissemination, it frequently (80%) affects the adrenal glands[2]. In such cases, patients often present with bilateral adrenal masses[3]. Adrenal histoplasmosis must be followed particularly with vigilance due to the possibility of advancing to the point of causing adrenal insufficiency-the most common cause of death in patients with disseminated histoplasma infection[4,5]. The clinical and radiologic features are similar to those seen in tuberculosis(TB), malignancy or adrenal metastasis and other deep fungal infections. In endemic areas of TB, it is frequently misdiagnosed and treated with anti-tubercular drugs. The only investigation that is confirmatory in confusing cases is demonstration of fungal components in adrenal tissue derived from ultrasonography/computed tomography (USG/CT) guided fine needle aspiration cytology (FNAC). Most cases of adrenal histoplasmosis have been reported in immunocompromised individuals residing in endemic areas. Here we present the clinical, biochemical and imaging characteristics of 18 immunocompetent patients from a nonendemic area (Bangladesh) who presented with primarily adrenal involvement without pulmonary symptoms.
2. Subjects and methods
The clinical, biochemical and radiologic data of 18 patients with cytology proven adrenal histoplasmosis that presented consecutively in the Department of Endocrinology, BSMMU between 2014 and 2020 were retrospectively analyzed in this case series. Informed written consent was obtained from all the patients for publication of the submitted article and the accompanying images before data collection. Ethical approval was taken from institutional review board, BSMMU (reg. no: 547;No.BSMMU/2021/6608). Demographic parameters including age, sex, occupation and clinical features were recorded. Routine hematologic, biochemical, relevant hormonal investigations and radiologic characteristics were noted. Serum cortisol and plasma adrenocorticotropic hormone (ACTH) were measured by chemiluminescent microparticle immunoassay (SEIMENS ADVIA Centaur XP, USA). Computed tomography (CT) scan was done in adrenal protocol (Toshiba Aquilion Prime, 160 slice, Japan). Presence of any immunocompromised state like steroid intake, evidence of diabetes mellitus (DM), chronic liver(CLD) or renal disease (CKD) and human immunodeficiency virus (HIV) status (enzyme linked immunosorbent assay) were recorded. Diagnosis of all cases were established on the basis of histopathologic evidence of histoplasmosis from CT guided adrenal FNAC. Data were expressed in frequency (%) for qualitative variables, and mean±SD or median (interquartile range, IQR) for quantitative variables depending on their distribution.
3. Results
The age of the patients was 45.00 (IQR: 39.25, 56.25)years ranging between 32 and 84 years. Majorities were male (16, 88.9%). All the patients resided in a non-endemic area of histoplasmosis without any significant travel history.One of the patients was a cultivator with probable risk of exposure to the fungal pathogen. Otherwise, the occupational history was unremarkable. None of them had any underlying immunocompromised conditions like CKD, CLD, malignancy,chronic alcohol abuse or steroid use. They were all seronegative for HIV infection. Only 5 (27.8%) had DM as co-morbidity well controlled on insulin or oral antidiabetic drugs and 10 (55.6%)had history of smoking. Other comorbidities included ischemic heart disease and prediabetes that were present in two different patients. The extensive work-up for TB, lymphoma and systemic malignancy was negative in all of them though initially 5 (27.8%)had empiric anti-Koch treatment that was proven to be ineffective.Their symptoms lasted between 3 and 24 months with a median duration of 6.00 (IQR: 4.00, 11.25) months. All of them had significant weight loss, anorexia and weakness whereas fever,predominantly of low grade, was present in 11 (61.1%) cases.Night sweat was an unusual feature presenting in 5 (27.8%) cases.Rare features included cervical lymphadenopathy and clubbing that were present in two different cases. The classic features of primary adrenocortical insufficiency namely hyperpigmentation and hypotension were present in 12 (66.7%) and 10 (55.6%) cases respectively. Three patients (16.7%) presented with adrenal crisis(Table 1 and Supplementary Figure 1).

Table 1. Clinical characteristics of 18 cases of adrenal histoplasmosis.
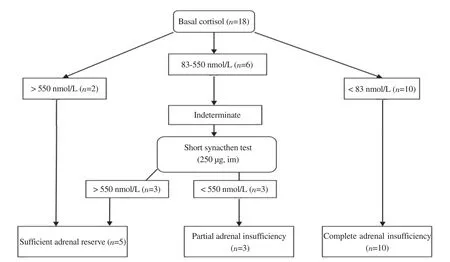
Figure 1. Status of adrenal reserve in the study population.
Erythrocyte sedimentation rate in the 1st hour (Westergren) was high (>30 mm) in 9 cases (50.0%) while 12 (66.7%) had anemia(Hb: M<13 gm/dL; F<12 gm/dL). Chest X-ray was abnormal in 3 patients. One had ill-defined patchy opacity in the right upper zone and another had bilateral hilar lymphadenopathy with nodular opacities and the 3rd case had right-sided pulmonary nodule later found as inflammatory lesion on FNAC. Though hyponatremia(<135 mmol/L) occurred in 10 (55.6%) cases, hyperkalemia(>5.5 mmol/L) was present in none and 15 (83.3%) had high serum ACTH (>46 pg/mL). Anti-histoplasma antibody was advised in two doubtful cases that were proven positive (Table 2). While 10 (55.6%) patients had subnormal basal cortisol (<83 nmol/ L)and 3 (16.7%) had partial cortisol insufficiency (stimulated cortisol <550 nmol/L) (Figure 1). Adrenal mass FNAC was done under CT guidance in all patients. Histopathology demonstrated histoplasmosis in each of the cases (Figure 2).
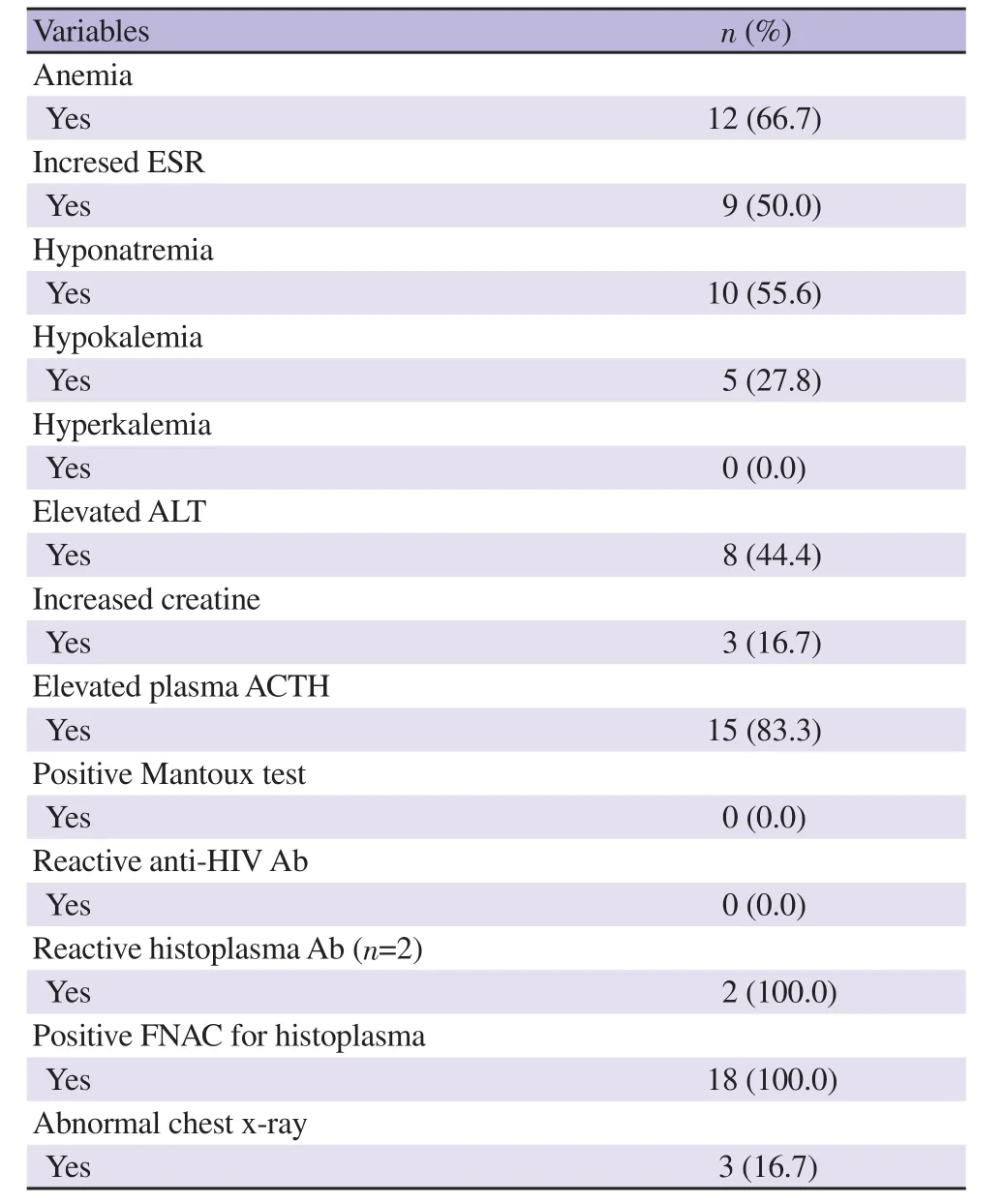
Table 2. Laboratory findings of the patients at the time of diagnosis (n=18).

Figure 2. Microphotograph of left adrenal tissues from fine needle aspiration cytology (FNAC) (periodic acid schiff staining) showing few histoplasma capsulati (arrows) (case No. 18).
CT scan in adrenal protocol revealed bilateral adrenal enlargement in all cases. The transverse, antero-posterior and vertical diameters of right adrenal gland were (4.82±1.71) cm, (3.31±1.50) cm &(2.28±1.78) cm and the left adrenal gland were (4.36±1.57) cm,(3.52±1.46) cm & (2.54±1.85) cm, respectively. Their shapes in all cases were oval with preservation of regular margin. All of them were hypodense in nature with radiodensity ranging from 21 to 90 hounsfield unit (HU) [right adrenal: lowest- (28.17±5.11),highest- (38.72±9.08); left adrenal: lowest- (36.83±14.65), highest-(47.56±14.54)]without any noticeable calcification (Table 3).The adrenals were homogeneous in 16 cases (88.9%), and 2 were heterogeneous in contrast enhancement who also had central necrosis with peripheral rim enhancement (Table 3 and Figure 3).Hepatomegaly was present in 6 cases (33.3%), splenomegaly in 3 cases (16.7%); 5 patients (27.8%) had abdominal lymphadenopathy and 1 case had ascites revealed by imaging.

Table 3. CT scan findings of adrenal glands.
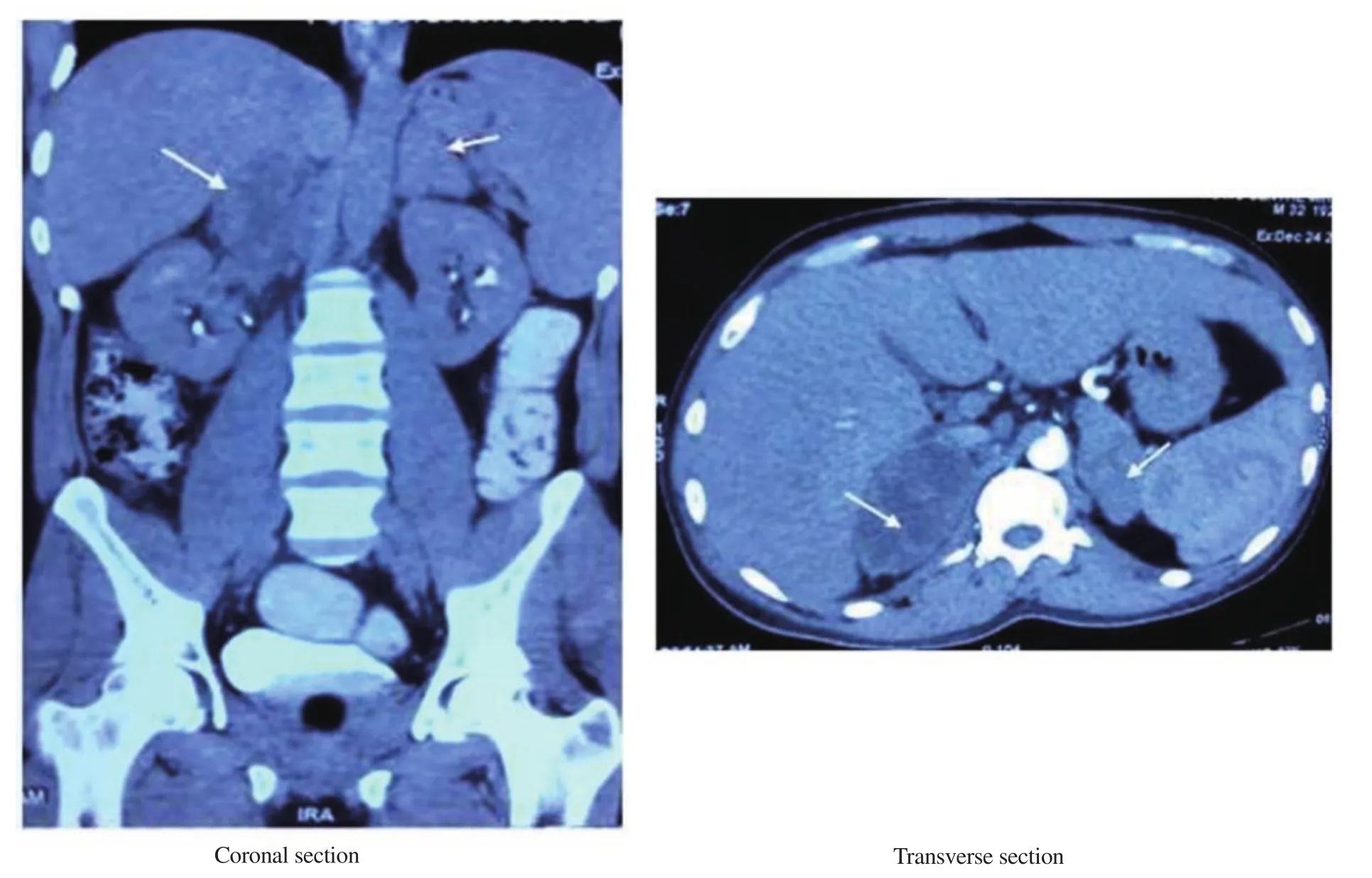
Figure 3. Contrast CT scan of the abdomen showing bilateral adrenomegaly with rim enhancement, septation and areas of necrosis (arrows) in a 40-year-male with adrenal histoplasmosis (case No. 10).
4. Discussion
This case series included 18 immunocompetent patients with adrenal histoplasmosis. The key findings of clinical, biochemical and imaging phenotypes are described in the following paragraphs.Histoplasmosis is an infectious disease caused by the dimorphic fungus Histoplasma capsulatum[6,7]. It is also called “Darling’s disease” after the initial description by pathologist Samuel Darling.This disease shows particularly high endemicity in the Mississippi and Ohio River Valleys of the U.S. Midwest and South, where over 90% of individuals in some locations have been infected[8]. In nature, it exists as a mycelium in soil contaminated with excrement of birds and bats[6,7]. When inhaled by humans or animals, it produces the yeast phase, which has an affinity for the macrophages that comprise the reticuloendothelial system[9,10]. Most patients’inhalation of the fungi leads to a transient pulmonary infection,which subsides without treatment. In immunocompromised individuals, it may lead to chronic pulmonary infection or disseminated disease[10]. There is a high incidence of liver,spleen, lymph node, bone marrow, and most commonly adrenal involvement in such cases[10,11]. Immunosuppression, steroid therapy, hematologic malignancies, advanced age, and chronic medical diseases predispose to disseminated histoplasmosis[12].The explanation for histoplasma tropism for the adrenal tissue is unclear. Possible explanation may be presence of glucocorticoidrich adrenal cells along with relative scarcity of reticuloendothelial cells[13,14]. Its clinico-radiologic manifestations mimic those of TB,a disease with a higher prevalence in developing countries and in HIV-positive patients. These patients therefore are often mistakenly diagnosed and treated for TB[1].
Disseminated histoplasmosis has a male predominance with male to female ratio of 3-10:1. A total of 99% cases infection is subclinical. Incidence is 2%-5% in HIV patients and <0.05% in non-HIV patients[1]. Most of the cases have been described in immunocompromised patients living in endemic areas. The current study is unique considering the facts that the disease was reported in immunocompetent individuals from non-endemic areas with predominant adrenal involvement with minimal pulmonary symptoms. In the recent years, a rising trend of reporting histoplasmosis was observed in many areas in Asian countries.Diabetes becomes a notable risk factor among HIV-negative patients with histoplasmosis in Asia. There are an increased number of immunocompetent cases of histoplasmosis from India and China indicating that Histoplasma is able to cause a disease both in immunocompromised and immunocompetent patients[15].Adrenal involvement by histoplasmosis may occur during the active course of dissemination or may evolve many years after the disease becomes inactive. Histoplasmosis presenting as asymptomatic bilateral adrenal enlargement has been described previously by other authors[3,16,17]. Adrenal histoplasmosis has a wide spectrum of clinical manifestations including chronicfatigue, weight loss, anorexia and fever. It may lead to adrenal insufficiency by progressive destruction of both adrenal glands.Around 5%-71% cases of adrenal histoplasmosis may cause primary adrenal insufficiency (Addison’s disease) and is the commonest explanation of death[18]. These patients exhibit fever,malaise, orthostatic hypotension, nausea and vomiting with hyperkalemia and hyponatremia[17]. In the present series, only 3(16.7%) patients presented with adrenal crisis. The classic feature of primary adrenocortical insufficiency namely hyperpigmentation and hypotension was present in approximately 66.7% and 55.6% of cases respectively. Nearly 75% of our patients had Addison’s disease based on either clinical or biochemical findings. Most histoplasmosis infections were associated with hepatosplenomegaly though in the current study it was much less frequent[19].
TB and fungal infections (such as histoplasmosis,coccidiodomycosis, blastomycosis) are two most important infective causes of adrenal insufficiency and TB is the commonest cause within the endemic areas[20]. Therefore, it is not surprising that 12 (66.7%) out of our 18 patients were mistakenly diagnosed with TB and 5 of them received anti-tubercular therapy initially.Interestingly, 2 of them were misdiagnosed as TB even on histopathology, which was later re-evaluated to elucidate the correct diagnosis after treatment failure.
Several CT findings are characteristic features of adrenal histoplasmosis including bilateral symmetric enlargement with preservation of normal contour, peripheral enhancement,and central hypodensity. Healing may be associated with calcification[19]. Bilateral adrenal enlargement may also be seen in adrenal hemorrhage, lymphoma, metastatic or other disseminated infections such as TB, cryptococcosis, blastomycosis,or aspergillosis[21]. Usually, adrenal metastases do not conform to the adrenal shape but typically present as round or oval masses.It may mimic infection, because central necrosis is common in both conditions[19]. Once central necrosis and peripheral rim enhancements are found, the differential diagnoses are limited to TB and histoplasmosis[22]. However, there are no definite reliable imaging characteristics to differentiate adrenal histoplasmosis from other causes of bilateral adrenomegaly and the CT scan features depend mostly on the stage of evolution. Ultimately, the final diagnosis relies on demonstration of a typical fungal element on histopathology or culture of the tissue derived from USG/CT guided FNAC of the adrenals as in our cases.
Adrenal histoplasmosis should be treated like disseminated histoplasmosis. The mortality in untreated patients is as high as 80%-100%, but if treated with antifungal, this very high mortality rate is remarkably reduced to less than 25%[23]. Patients who are not severely ill can be treated with oral itraconazole, 200 mg bid. Patients with severe infection should be treated initially with amphotericin B at a dosage of 0.7 to 1.0 mg/kg daily or the lipid formulation of amphotericin B at a dosage of 3 to 5 mg/ kg daily[5,8,17]. We treated all our cases with oral itraconazole as liposomal amphotericin is rather expensive, nephrotoxic and not easily available in our country. Two patients completed 6 months of anti-tubercular therapy after being misdiagnosed by FNAC.Initially they had partial response possibly due to the effect of concurrent steroid replacement. However, as they relapsed, the final diagnosis was clinched after reviewing histopathology specimen. We could not incorporate the outcome of our patients in this study as they are at different stages of treatment at present.
Our case series demonstrates the fact that adrenal histoplasmosis does occur in immunocompetent individuals living in nonendemic areas. It should be considered in the list of differentials of bilateral adrenomegaly besides common disorders such as TB. Considering the wide availability of effective treatments for this unique infection, timely diagnosis is warranted to avoid fatal complications like adrenal insufficiency. Further prospective study is required to see the outcomes of these patients whether they are different from immunocompromised patients with histoplasmosis.
Conflict of interest statement
The authors declare that there is no confict of interest.
Acknowledgments
We acknowledge our colleagues from Department of Radiology and Imaging, Pathology and Microbiology of BSMMU for their support in management of the patients.
Authors’ contributions
SJ, MAH and MF conceptualized the study. SJ, TM, IF, MSM,AY, AKS, CA, EUR collected all data including figures. FB reviewed all FNAC slides. Data were analysed by TM and MSM.Manuscript was prepared by SJ, TM and MSM and revised by MAH, FB and MF. All the authors read the manuscript and approved for publication.
杂志排行
Asian Pacific Journal of Tropical Medicine的其它文章
- Favipiravir and its potentials in COVID-19 pandemic: An update
- Efficacy and safety of ivermectin for COVID-19: A systematic review and meta-analysis
- Prevalence of non-tuberculosis mycobacteria among samples deposited from the National Tuberculous Reference Laboratory of Iran (2011-2018)
- Detection of dengue virus serotype 3 in Cajamarca, Peru: Molecular diagnosis and clinical characteristics
- Prediction of malaria cases in the southeastern Iran using climatic variables: An 18-year SARIMA time series analysis
- Recovery of child immunization programs post COVID-19