Impact of biliary complications on quality of life in live-donor liver transplant recipients
2021-11-04ReginiaNabilGuirguisEhabHasanNashaatAzzaEmamYassinWesamAhmedIbrahimShereenSalehMohamedBahaaMahmoudElMeteiniMohamedFathyHanyMansourDabbousImanFawzyMontasserManarSalahGhadaAbdelrahmanMohamed
Reginia Nabil Guirguis, Ehab Hasan Nashaat, Azza Emam Yassin, Wesam Ahmed Ibrahim, Shereen A Saleh,Mohamed Bahaa, Mahmoud El-Meteini, Mohamed Fathy, Hany Mansour Dabbous, Iman Fawzy Montasser,Manar Salah, Ghada Abdelrahman Mohamed
Reginia Nabil Guirguis, Ehab Hasan Nashaat, Azza Emam Yassin, Wesam Ahmed Ibrahim, Shereen A Saleh, Ghada Abdelrahman Mohamed, Department of Internal Medicine, Gastroenterology and Hepatology Unit, Faculty of Medicine, Ain Shams University, Cairo 11591, Egypt
Mohamed Bahaa, Mahmoud El-Meteini, Mohamed Fathy, Department of General Surgery, Faculty of Medicine, Ain Shams University, Cairo 11591, Egypt
Hany Mansour Dabbous, Iman Fawzy Montasser, Manar Salah, Department of Tropical Medicine, Faculty of Medicine, Ain Shams University, Cairo 11591, Egypt
Abstract BACKGROUND Despite significant advancements in liver transplantation (LT) surgical procedures and perioperative care, post-LT biliary complications (BCs) remain a significant source of morbidity, mortality, and graft failure.In addition, data are conflicting regarding the health-related quality of life (HRQoL) of LT recipients.Thus, the success of LT should be considered in terms of both the survival and recovery of HRQoL.AIM To assess the impact of BCs on the HRQoL of live-donor LT recipients (LDLT-Rs).METHODS We retrospectively analysed data for 25 LDLT-Rs who developed BCs post-LT between January 2011 and December 2016 at our institution.The Short Form 12 version 2 (SF 12v2) health survey was used to assess their HRQoL.We also included 25 LDLT-Rs without any post-LT complications as a control group.RESULTS The scores for HRQoL of LDLT-Rs who developed BCs were significantly higher than the norm-based scores in the domains of physical functioning (P = 0.003), role-physical (P < 0.001), bodily pain (P = 0.003), general health (P = 0.004), social functioning (P = 0.005), role-emotional (P < 0.001), and mental health (P < 0.001).No significant difference between the two groups regarding vitality was detected (P = 1.000).The LDLT-Rs with BCs had significantly lower scores than LDLT-Rs without BCs in all HRQoL domains (P < 0.001) and the mental (P < 0.001) and physical (P = 0.0002) component summary scores.CONCLUSION The development of BCs in LDLT-Rs causes a lower range of improvement in HRQoL.
Key Words: Live-donor liver transplantation; Quality of life; The Short Form 12 version 2; Cirrhosis; Biliary complications; Mental health
INTRODUCTION
Health-related quality of life (HRQoL) is a multidimensional model reflecting the domains of social, mental, emotional, and physical health[1,2].More than 50 different HRQoL tools have been used in liver transplant (LT) research[3], and no golden standard instrument has existed until now[4].These tools can be classified into generic and disease-specific tools[3,5].Generic HRQoL tools, of which the validated Short Form 36 (SF-36) health survey is the most frequently used for evaluating LT recipients, allow assessments across various medical conditions and health states[6,7].
Short Form 12 version 2 (SF-12v2) is a validated concise version of the SF-36 version 2 (SF-36v2) with only 12 questions[8,9].Similar to the SF-36v2, it evaluates the same eight dimensions of HRQoL covering the previous 4 wk: General health, bodily pain, physical functioning, role physical, vitality, role emotional, mental health, and social functioning.Physical Component Summary (PCS) and Mental Component Summary (MCS) scores were created from patient responses[10].The sum of scores ranges from 0 to 100, where 0 indicates the worst state of health and 100 indicates the best state of health[10,11].
The data are conflicting regarding the HRQoL of LT recipients.The heterogeneity between studies regarding the type of graft, diversity of included patients, and health survey precludes definitive conclusions[4,12].In addition, an overlap exists between the primary liver disease and LT process with diverse events during peri- and postoperative management.
The global assessment of HRQoL after LT usually confirms improvement compared with pretransplant status[13]; however, it may remain suboptimal compared to the general population due to post-LT complications, recurrence of primary liver disease, or adverse effects of immunosuppressants[14-17].In addition, cirrhosis leads to loss of muscle mass, sarcopenia, malnutrition, and physical impairment that manifest as physical frailty, increasing the risk of pretransplant mortality[18-20] and delayed improvement of physical functioning post-LT[21-23].
Fatigue affects up to 50% of patients with chronic liver disease; moreover, it demonstrates a significant association with poor HRQoL[24,25].It also affects up to 60% of LT recipients[26].It is a complex symptom that may be influenced by physical and mental states, including poor sleep quality, anxiety, and depression[27].
The LT candidates often have impaired HRQoL with a high prevalence of anxiety and depressive symptoms[28,29].Moreover, LT was considered as post-traumatic stress disorder and was also found to be associated with anxiety and depression, which may further impair the HRQoL of LT recipients[30-33].
In the light of the above, HRQoL should be considered in terms of the outcome after LT[34,35].Hence, we aimed to assess the impact of biliary complications (BCs) on the HRQoL of live-donor LT recipients (LDLT-Rs).
MATERIALS AND METHODS
Study design
We retrospectively analysed all LDLT-Rs at Ain Shams Centre for Organ Transplantation, Ain Shams Specialised Hospital, Cairo, Egypt, between January 2011 and December 2016.During this period, 215 adult patients underwent right-lobe LDLT at our centre.We included LDLT-Rs who developed BCs post-LT.We excluded LDLTRs with any of the following situations: cholestatic liver diseases (primary biliary cirrhosis or primary sclerosing cholangitis), vascular complications, acute or chronic rejection, recurrent hepatitis C virus (HCV) infection, graft failure, failure to follow up for at least one year post-LT, or patients who refused to participate in the research.As a result, 25 LDLT-Rs with BCs were included in the final analysis.We enrolled 25 LDLT-Rs who did not develop any post-LT complications as a control group.LT recipients were assessed at least 12 months post-LT, with median follow up duration of 5.5 years (range: 12 mo - 8 years).
This study was performed per the ethical principles of the declaration of Helsinki and was approved by the ethical committee of the Faculty of Medicine, Ain Shams University (No: FMASU MD 187/2016), which waived the requirement of informed consent due to the retrospective nature of the research.
Quality-of-life assessment
Eligible LDLT-Rs were invited to fulfil the SF-12v2 questionnaire during follow-up visits after obtaining verbal consent.We used anonymous questionnaires to ensure strict confidentiality.The SF-12v2 includes 12 questions: one question on general health perceptions, two questions concerning physical functioning, two questions on role limitations because of physical health problems, one question on bodily pain, one question on vitality, two questions on role limitations, one question on social functioning, and two questions on general mental health.
Statistical analysis
The data were analysed using IBM SPSS Statistics (v.23; IBM Corp., Armonk, New York).Nonparametric numerical variables are presented as the median and interquartile range.Nominal variables are presented as the number and percentage.Ordinal data were analysed using the chi-squared test for trends.Two-sidedPvalues < 0.05 were considered statistically significant.
RESULTS
This study included 25 adult right-lobe LDLT-Rs who experienced BCs.At the time of LT, the mean age of the recipients was 52 ± 7 years, and 19 (76%) recipients were male.Cirrhosis due to HCV was the most common indication for LT in 21 patients (84%; Tables 1 and 2).
Development and management of biliary complications
Among the 25 LDLT-Rs included in this study, minor biliary leakage occurred in 15 recipients (83.3%) and stopped spontaneously without further management.In only three (16.6%) recipients, pigtail insertion and further interventional management were needed.Moreover, 25 recipients developed a biliary infection, mainly occurring early(23; 92%) and in one to two episodes in 16 (64%) recipients (Table 1).Furth-er, 20 (80%) recipients developed biliary stricture, most of which presented in one to two episodes (13; 65%).The development of BCs caused a prolonged hospital stay (median = 46 days; range: 15 - 67 days), with nine (36%) patients needing ≥ three episodes of admission.Concerning the management of BCs, endoscopic retrograde cholangiopancreatography (ERCP) with stenting ± dilatation was done for 20 (80%) recipients, with seven (28%) recipients needing ≥ three ERCP sessions.Percutaneous transhepatic cholangiography was needed for only three (12%) recipients, with one recipient requiring another session.These methods only failed in one recipient who needed surgical reconstruction of the biliary stricture (Table 1).

Table 1 Descriptive categorical data for live-donor liver transplant recipients with biliary complications

Table 2 Descriptive numerical data for live-donor liver transplant recipients with biliary complications
Health-related quality of life
The scores of HRQoL of LDLT-Rs with BCs were significantly higher than the normbased scores in the domains of physical functioning (P= 0.003), role-physical (P< 0.001), bodily pain (P= 0.003), general health (P= 0.004), social functioning (P= 0.005), role-emotional (P< 0.001), and mental health (P< 0.001).In contrast, no significant difference was found between the two groups regarding vitality (P= 1.000; Table 3 and Figure 1).The LDLT-Rs with BCs had significantly lower scores than LDLT-Rs without BCs in all HRQoL domains (P< 0.001) and in the mental (P< 0.001) and physical (P= 0.0002) component summary scores (Tables 4 and 5; Figures 1 and 2).

Figure 1 Short Form 12 (v.2) domains in patients and controls compared to the norm-based score.

Figure 2 Physical and mental component summary scores of patients and controls.
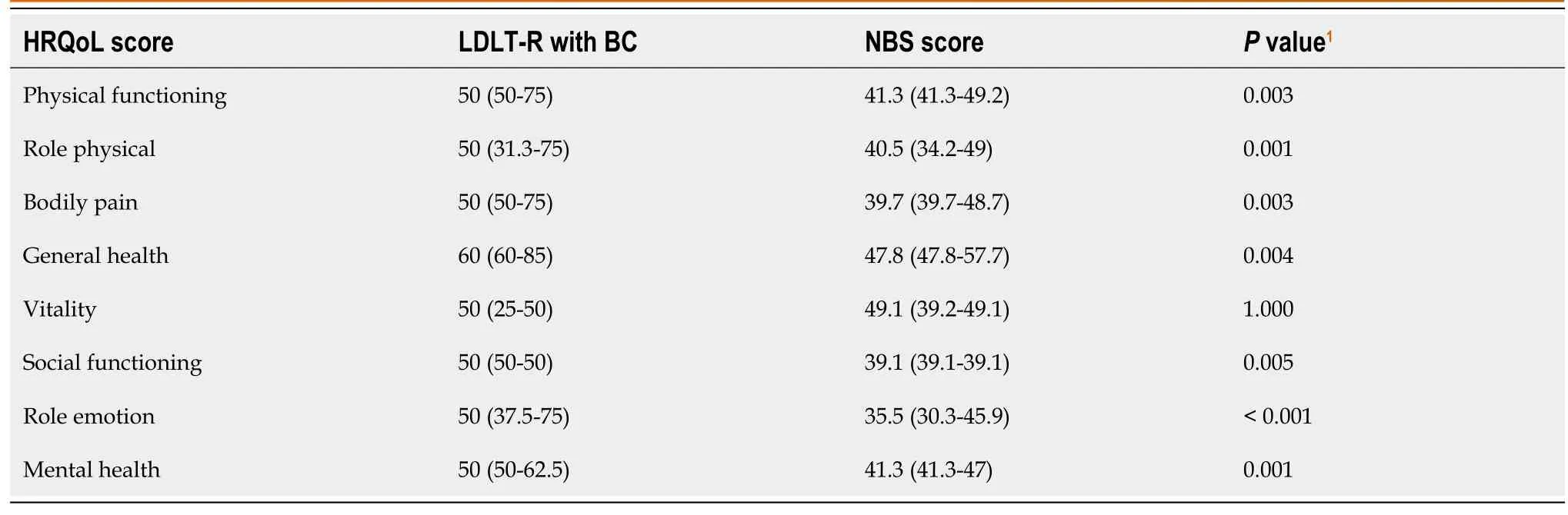
Table 3 Comparison of the quality-of-life scores for live-donor liver transplant recipients with biliary complications and their corresponding norm-based scores

Table 4 Comparison of health-related quality-of-life scores between patients and controls
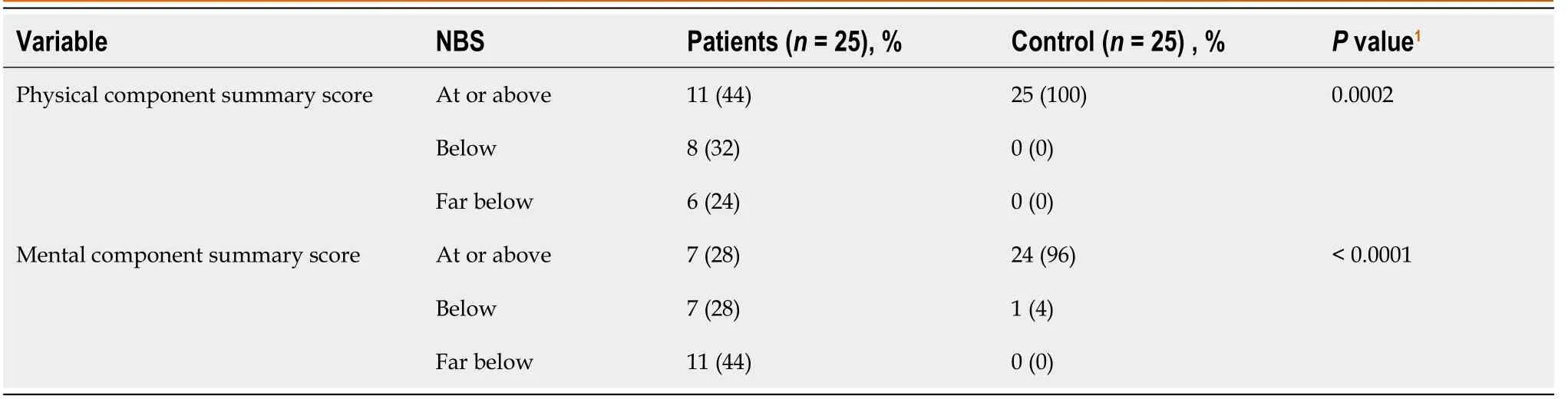
Table 5 Physical and mental component summary scores in patients and controls compared with norm-based scores
DISCUSSION
Despite the considerable advances in LT surgical techniques and perioperative care, post-LT BCs remain a significant source of morbidity, mortality, and graft failure[36].To our knowledge, no previous study has specifically assessed the impact of BCs on the HRQoL of LDLT-Rs.In our study, LDLT-Rs with BCs had significantly higher HRQoL domain scores except for the vitality domain than norm-based scores; however, those patients gained a significantly lower range of improvement in HRQoL domains with lower MCS and PCS scores than those without BCs.This result can be attributed to more prolonged and frequent hospital admission and expectation reduction with anxiety, stress, and depression[37].In agreement with the current results, the published literature has observed the positive effects of LT on therecipients’ HRQoL[12,37-40].
Similar to the present study[41], other authors have assessed the LT recipients’ HRQoL using the WHOQOLBREF questionnaire[42] and Transplant Effects Questionnaire[43] and concluded that LT recipients, especially those who received LDLT, reported the highest level of HRQoL in all four dimensions of HRQoL in comparison to those with other organ transplantation.
In partial agreement with the current study, a review of 32 studies and 5402 patients found that the overall HRQoL scores of LT recipients remain improved and equivalent to the general population in the long term.However, physical functioning continues to be inferior to the general population despite a noticeable improvement from preoperative physical functioning[4].Similarly, a review article of 31 publications reported improved overall HRQoL and physical functioning in deceased donor LT (DDLT) adult recipients during the first 2 years, which remains stable in the long term but does not reach the level of the general population[35].Additionally, Sullivanet al[44] assessed the HRQoL two decades after DDLT using the SF-12 survey.In adult survivors, the MCS score (54.6) was equivalent to that of the general population; however, the PCS score (39.3) remained below average.This outcome can be explained by the presence of comorbidities, primary liver disease severity, postoperativemorbidity, and graft type[20,33].Additionally, Dunnet al[45] reported that group exercise activities were correlated with improved physical function, mental health, and HRQoL, independent of comorbidities, for up to 5 years after LT.Therefore, physical activity should be encouraged after LT[46].
In a study by Casanovaset al[47], the SF-36 scores of 156 LT candidates were assessed pre- and post-LT.They observed significantly lower patient baseline scores in all HRQoL domains than general population scores, especially in physical health.As early as 3 months till 1-year post-LT, they detected improvement in all SF-36 domains except vitality and social functioning, revealing no significant improvement.Moreover, sleeping problems were observed at the baseline and persisted post-LT.The poor sleep quality frequently noted in cirrhotic patients is known to cause fatigue and impair cognitive and physical functions[48].
In contrast to our results, Domingoset al[37] retrospectively assessed the HRQoL of 93 DDLT recipients who survived 10 years post-LT using the SF-36 survey and observed that LT recipients had lower mental health scores than the general population.In all other domains, LT recipients had similar (emotional limitations, pain, and general health status) or superior (physical limitations, social aspects, functional capacity, and vitality) scores than the general population.In addition, Dąbrowska-Benderet al[15] assessed the SF-36 health survey in 121 DDLT recipients and observed no change in mental health score, whereas significant physical impairment was reported by 18.18% of the recipients.
In a study by Annemaet al[30], LT had a beneficial effect on the mental health of LT recipients by ameliorating anxiety and depression symptom severity.However, recipients with persistent symptoms of anxiety and depression experienced a negative effect on HRQoL and therapeutic adherence.They also observed that persistent anxiety and depression were correlated with the development of BCs and the duration of the hospital stay.Similarly, in another report[49], the HRQoL of 82 LT recipients was retrospectively assessed, finding 94% reported high mean scores on HRQoL, the McGill Quality of Life Questionnaire, and adherence to medications.Conversely, patients with a low HRQoL reported anxiety, depression, fatigue, slowing pace, and physical limitations, suggesting that LT recipients who fail to adapt to their post-LT state experienced a decreased ability to tolerate physical symptoms and post-LT complications[50].Other causes for lower mental health scores post-LT are the worry regarding medication side effects, hepatic disease recurrence, and other potential complications[51].
Candidates for LT may have overly optimistic anticipations for post-LT improvement in their HRQoL.Unfulfillment of these expectations may negatively affect their HRQoL, highlighting the need to help patients expect and understand the outcomes of LT.Moreover, LT candidate education positively affects post-LT HRQoL[40].Education is associated with better outcomes and higher patient adherence[52].
This study is limited by its retrospective nature and small sample size.More research is required to define the predictors of HRQoL and plan multidisciplinary strategies for HRQoL improvement in LT recipients.According to the current literature, HRQoL should be integrated into the clinical care of LT[53].
CONCLUSION
We conclude that the development of BCs in LDLT-Rs causes a lower range of improvement in HRQoL.
ARTICLE HIGHLIGHTS
Research background
Despite the considerable advances in liver transplantation (LT) surgical techniques and perioperative care, post-LT biliary complications (BCs) remain a significant source of morbidity, mortality, and graft failure.Due to the current high survival rates of LT,the focus has shifted to improving the quality of life of LT recipients.
Research motivation
The data are conflicting regarding the health-related quality of life (HRQoL) of LT recipients.
Research objectives
To assess the impact of BCs on the HRQoL of live-donor LT recipients (LDLT-Rs).
Research methods
We retrospectively analysed data for 25 LDLT-Rs with BCs and described their HRQoL through the Short Form 12 version 2 (SF-12v2) health survey compared to 25 LDLT-Rs without post-LT complications.
Research results
The scores of HRQoL of LDLT-Rs with BCs were significantly higher than the normbased scores in all HRQoL domains except vitality.The LDLT-Rs with BCs had significantly lower scores than LDLT-Rs without BCs in all HRQoL domains (P <0.001) and in the mental (P < 0.001) and physical (P = 0.0002) component summary scores.
Research conclusions
The development of BCs in LDLT-Rs causes a lower range of improvement in HRQoL.
Research perspectives
The assessment of HRQoL should be integrated into the clinical care of LT recipients.Identifying the determinants of HRQoL could improve the management plan of these patients through a multidisciplinary approach.
杂志排行
World Journal of Hepatology的其它文章
- Coronavirus disease 2019 in liver transplant patients: Clinical and therapeutic aspects
- Focal nodular hyperplasia associated with a giant hepatocellular adenoma: A case report and review of literature
- Clinical outcomes of patients with two small hepatocellular carcinomas
- Acute liver failure with hemolytic anemia in children with Wilson’s disease: Genotype-phenotype correlations?
- Machine learning models for predicting non-alcoholic fatty liver disease in the general United States population: NHANES database
- Serum zonulin levels in patients with liver cirrhosis: Prognostic implications