Captopril alleviates lung inflammation in SARS-CoV-2-infected hypertensive mice
2021-10-18Wen-CongGao,XinMa,PengWang等
Severe acute respiratory syndrome coronavirus 2 (SARSCoV-2) is the etiologic agent responsible for the global coronavirus disease 2019 (COVID-19) pandemic. Numerous studies have demonstrated that cardiovascular disease may affect COVID-19 progression. In the present study, we investigated the effect of hypertension on viral replication and COVID-19 progression using a hypertensive mouse model infected with SARS-CoV-2. Results revealed that SARS-CoV-2 replication was delayed in hypertensive mouse lungs. In contrast, SARS-CoV-2 replication in hypertensive mice treated with the antihypertensive drug captopril demonstrated similar virus replication as SARS-CoV-2-infected normotensive mice.Furthermore, antihypertensive treatment alleviated lung inflammation induced by SARS-CoV-2 replication (interleukin(IL)-1β up-regulation and increased immune cell infiltration).No differences in lung inflammation were observed between the SARS-CoV-2-infected normotensive mice and hypertensive mice. Our findings suggest that captopril treatment may alleviate COVID-19 progression but not affect viral replication.
Patients with cardiovascular comorbidities such as hypertension are at an increased risk of SARS-CoV-2 infection(Parra-Bracamonte et al., 2020). However, the proposal that antihypertensive drug treatment increases mortality in hypertensive COVID-19 patients remains controversial. While recent animal studies and clinical trials have focused on the risk of sudden death, information concerning the impact of antihypertensive drugs, such as angiotensin-converting enzyme inhibitors (ACEi), on lung function in COVID-19 patients is limited. Hence, the potential impact of antihypertensive drugs on lung function remains an important clinicopathological parameter informing specific drug choice.The mortality rate in COVID-19 patients with cardiovascular disease is higher than that in COVID-19 patients with normal cardiovascular function, and ACE2 expression in the lungs of rats is increased by ACEi treatment, thus providing a potential explanation for the increased mortality (Pedrosa et al., 2021).In the present study, we examined the effect of ACEi on lung function in the context of hypertension.
This study was carried out in accordance with the Animal Welfare Act, and all applicable international, national, and institutional guidelines for the care and use of animals were strictly followed. All animal sample collection protocols complied with the current laws of China. The animal experiments were conducted under the authority of a license issued by the government of Yunnan Province, and with approval from the Animal Experimentation Ethics Committee and Care and Use of Laboratory Animal Committee of the Kunming Institute of Zoology (approval license number:SMKX-20200301-01). All SARS-CoV-2 research was performed under biosafety level 3 protocols using animal BSL3 containment.
We previously created a SARS-CoV-2-infected mouse model, C57BL/6N-Ace2em2(hACE2-WPRE,pgk-puro)/CCLA, to simulate human patients with SARS-CoV-2 infection (Liu et al., 2021).We also established an angiotensin II (Ang II)-induced hypertensive mouse model (Zheng et al., 2021). Briefly,humanized ACE2 (hACE2) mice were anaesthetized with isoflurane and surgically implanted with osmotic pumps containing Ang II (1.4 mg/kg/day) to increase blood pressure.After validating their elevated blood pressure at 14 days post Ang II treatment (dpa), mice were treated intragastrically with captopril (Cap, 10 mg/kg/day, i.g.) or vehicle before intranasal inoculation with SARS-CoV-2 (2×106TCID50, i.n.) at 15 dpa(Figure 1A). After SARS-CoV-2 infection, mice in the Ang II+SARS-CoV-2 group were treated with Ang II. Likewise,mice in the Ang II+SARS-CoV-2+Cap group were treated with Ang II and Cap. Mice were finally sacrificed at 3 days postinfection (3 dpi) or 7 dpi (18 dpa or 22 dpa, respectively) to harvest lungs for measurement of viral load, as described elsewhere (Song et al., 2020; Xu et al., 2020). Viral load in mouse feces was monitored daily, as described elsewhere(Liu et al., 2021). SARS-CoV-2 was detected by quantitative real-time polymerase chain reaction (qRT-PCR) with a TaqMan probe (see Supplementary Materials and Methods).The sequences of the SARS-CoV-2 primers and probes can be found in previous study (Tian et al., 2021). Figure 1A (left panel) shows a schematic of the experimental protocol.
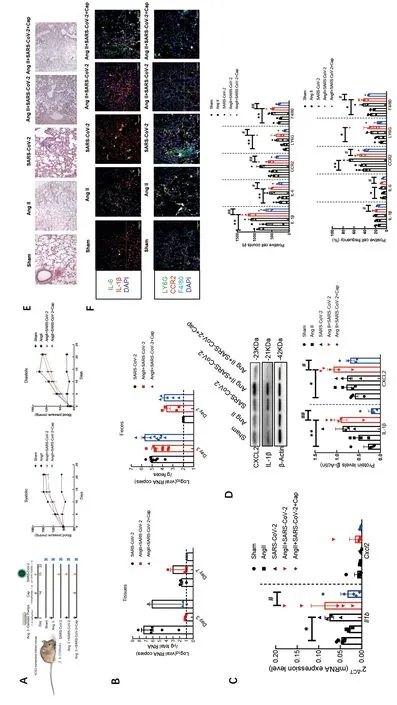
Figure 1 Captopril alleviates lung inflammation in SARS-CoV-2-infected hypertensive mice
After 14 days, Ang II treatment increased systolic and diastolic blood pressure in the three experimental groups,while SARS-CoV-2-infected mice (with and without Cap treatment) did not show significant changes in systolic or diastolic blood pressure (Figure 1A, right panel). Furthermore,qRT-PCR viral load detection suggested the absence of SARS-CoV-2 in lung tissue from the Ang II-treated C57BL/6NAce2em2(hACE2-WPRE,pgk-puro)/CCLAmice at 3 and 7 dpi (Figure 1B).To validate the effects of Ang II on SARS-CoV-2 replication,fecal viral load was also estimated. SARS-CoV-2 was not detected in fecal samples from the control mice at 7 dpi(Figure 1B). In contrast, SARS-CoV-2 was detected in fecal samples from Ang II- and Cap-treated mice until 7 dpi. These results suggest that Ang II may prolong SARS-CoV-2 replication. The observed viral loads in SARS-CoV-2-infected mice are consistent with previous findings (Gu et al., 2020).
To examine the impact of SARS-CoV-2 on Ang II-induced hypertension, lung tissue expression of two inflammatory markers, i.e.,Il1bandCxcl2, was analyzed by qRT-PCR at 7 dpi (Winkler et al., 2020) (Figure 1C). SARS-CoV-2 infection selectively increasedIl1bmRNA levels, whileCxcl2mRNA levels were unaffected. Furthermore,Cxcl2expression in the lungs of SARS-CoV-2-infected hypertensive mice was unaffected by Cap administration. In contrast, Cap treatment down-regulatedIl1bexpression in the lungs of Ang II-treated SARS-CoV-2-infected mice (Figure 1C). To validate these results, CXCL2 and IL-1β protein levels (which reflect inflammation status) were also determined in the lungs.SARS-CoV-2-infected hypertensive mice exhibited increased lung inflammation (in comparison with the Sham group),reflected by the up-regulation of IL-1β and CXCL2. However,Cap treatment reduced lung inflammation in SARS-CoV-2-infected hypertensive mice (Figure 1D).
Histopathological evaluation of mouse lung tissues using hematoxylin-eosin (H&E) staining revealed no obvious lesions in the lungs of the non-infected Sham group (except for one mouse with interstitial pneumonia but without bronchial lesions). In contrast, pulmonary inflammation was extensively observed in Ang II-induced hypertensive mice at 7 dpi (though to different extents). In general, this inflammation was characterized by moderate local inflammatory cell infiltration,alveolar wall thickening, and partial alveolar destruction.However, these changes were not obvious in all mice. In comparison with hypertensive mice, alveolar wall thickening was reduced, and inflammatory cell infiltration was increased in SARS-CoV-2-infected hypertensive mice at 7 dpi. These changes were largely reversed by Cap treatment, which yielded a more complete alveolar structure (Figure 1E).
The effects of ACEi on lung inflammation were assessed by immunofluorescence. Compared with uninfected mice, SARSCoV-2-infected hypertensive mice exhibited substantial lung inflammation (Figure 1F), as indicated by the significant increase in IL-1β- and IL-6-positive cells. This result is consistent with previous study (Gu et al., 2020). However,lung inflammation (i.e., positive cell counts) was markedly reduced following Cap treatment. Furthermore, IL-1β- and IL-6-positive cell frequencies (percentage of total cell count) were reduced in the lungs of SARS-CoV-2-infected hypertensive mice following Cap treatment (Figure 1F). Surprisingly, IL-1βand IL-6-positive cell frequencies in hypertensive C57BL/6NAce2em2(hACE2-WPRE,pgk-puro)/CCLAmice were unaffected by SARSCoV-2 infection. Because SARS-CoV-2 infection is known to increase the population of immune cells (Zhou et al., 2020),we next examined immune cell distribution in the mouse lungs. Notably, the increased levels of LY6G-positive cells(neutrophils) and F4/80-positive cells (macrophages) in the lungs of SARS-CoV-2-infected hypertensive mice were consistent with the increased immune response (in comparison with uninfected hypertensive mice). However, Cap treatment reduced the distribution of monocytes (CCR2 signal), neutrophils, and macrophages (Figure 1F) in the lungs. In contrast, no differences in immune cell distribution were observed between the SARS-CoV-2-infected hypertensive mice and SARS-CoV-2-infected normotensive mice.
The present study demonstrated that Cap treatment promotes normal lung physiology in hypertensive COVID-19 hACE2 mice. However, our study has several evident limitations. Firstly, the sample size of SARS-CoV-2 hACE2 mice was small due to strict regulations concerning the use of the virus. Secondly, the mice were treated with Cap for only 7 days, and their blood pressure was measured on day 8, with no significant differences found. Several studies have reported that Cap does not lower blood pressure after two weeks, and that Cap administration for a longer period is required to observe a significant change (Hijriani et al., 2020;Zhang et al., 2012). Moreover, Cap is a short-acting antihypertensive drug (Hsu et al., 2019) and, in a clinical setting, must be taken daily for three months to four years (or even longer) to control blood pressure effectively (Groel et al., 1983). As SARS-CoV-2 can only be detected for 7 days in C57BL/6N-Ace2em2(hACE2-WPRE,pgk-puro)/CCLAmice (Liu et al.,2021), we only treated mice with Cap for 7 days. Further studies are needed to obtain an in-depth understanding of the role of ACE and its inhibitors in lung function under hypertension plus COVID-19 infection.
SUPPLEMENTARY DATA
Supplementary data to this article can be found online.
COMPETING INTERESTS
The authors declare that they have no competing interests.
AUTHORS’ CONTRIBUTIONS
F.L.L., C.B.Z., and Y.T.Z. conceived and designed the study.W.C.G., X.M., and X.Y.H. performed the experiments and analyzed the data. P.W. helped analyze the data. C.B.Z. and F.L.L. wrote the manuscript. Y.T.Z. revised the manuscript. All authors read and approved the final version of the manuscript.
ACKNOWLEDGEMENTS
We would like to thank all the staff at the Kunming National High-level Biosafety Research Center for Non-human Primates for their assistance with the experiments. We thank Prof. Yu Huang of Chinese University of Hong Kong for editing.
杂志排行
Zoological Research的其它文章
- Phylogenomic relationships and molecular convergences to subterranean life in rodent family Spalacidae
- Prosecution records reveal pangolin trading networks in China, 2014-2019
- Chromosome-scale genome assembly of brownspotted flathead Platycephalus sp.1 provides insights into demersal adaptation in flathead fish
- Deletion of phosphatidylserine flippase β-subunit Tmem30a in satellite cells leads to delayed skeletal muscle regeneration
- Role of juvenile hormone receptor Methoprene-tolerant 1 in silkworm larval brain development and domestication
- Global view on virus infection in non-human primates and implications for public health and wildlifeconservation