Therapeutic plasma exchange in liver failure
2021-09-03AbimbolaChrisOlaiyaAanchalKapoorKristinRicciChristinaLindenmeyer
Abimbola Chris-Olaiya, Aanchal Kapoor, Kristin S Ricci, Christina C Lindenmeyer
Abimbola Chris-Olaiya, Aanchal Kapoor, Department of Critical Care, Cleveland Clinic, Cleveland, OH 44195, United States
Kristin S Ricci, Department of Hematology and Medical Oncology, Cleveland Clinic, Cleveland, OH 44195, United States
Christina C Lindenmeyer, Department of Gastroenterology, Hepatology and Nutrition, Cleveland Clinic, Cleveland, OH 44195, United States
Abstract The multi-organ failure syndrome associated with acute and acute-on-chronic liver failure (ACLF) is thought to be mediated by overwhelming systemic inflammation triggered by both microbial and non-microbial factors.Therapeutic plasma exchange (TPE) has been proven to be an efficacious therapy in autoimmune conditions and altered immunity, with more recent data supporting its use in the management of liver failure.Few therapies have been shown to improve survival in critically ill patients with liver failure who are not expected to survive until liver transplantation (LT), who are ineligible for LT or who have no access to LT.TPE has been shown to reduce the levels of inflammatory cytokines, modulate adaptive immunity with the potential to lessen the susceptibility to infections, and reduce the levels of albumin-bound and water-bound toxins in liver failure.In patients with acute liver failure, high volume TPE has been shown to reduce the vasopressor requirement and improve survival, particularly in patients not eligible for LT.Standard volume TPE has also been shown to reduce mortality in certain sub-populations of patients with ACLF.TPE may be most favorably employed as a bridge to LT in patients with ACLF.In this review, we discuss the efficacy and technical considerations of TPE in both acute and acute-on-chronic liver failure.
Key Words: Therapeutic plasma exchange; High volume plasma exchange; Acute liver failure; Acute-on-chronic liver failure; Cirrhosis; Liver transplantation; Cytokines
INTRODUCTION
Acute liver failure (ALF) and acute-on-chronic liver failure (ACLF) are two distinct classifications of severe hepatic dysfunction associated with secondary multi-organ failures (MOFs), both of which effect significant morbidity and mortality[1-4].The exact mechanisms by which MOFs are mediated have not been definitively established but are thought to be driven by excessive systemic inflammation and dysregulated immune activation triggered by both microbial and non-microbial factors, and less so by the primary insult to the liver[3,5-7].
The pathogenesis of MOFs in ALF has been attributed to the release of damageassociated molecular patterns (DAMPs) from injured hepatic cells and microbial pathogen-associated molecular patterns (PAMPs) in the presence of superimposed infection or bacterial translocation[7].The innate immune cells activated by PAMPs and DAMPs produce proinflammatory cytokines [interleukin (IL)-6, IL-1ß, IL-8, tumor necrosis factor-alpha (TNF-α)] that mediate systemic inflammation and further hepatocyte injury[7,8].In support of this hypothesis, levels of TNF-α and IL-6 have been shown to be significantly higher in patients with fulminant hepatitis when compared to patients with acute liver injury[9].
Similarly, the hallmark of the ACLF clinical syndrome is excessive systemic inflammation and bacterial translocation mediated by PAMPs and DAMPs[1,6,10].ACLF patients have been shown to manifest elevated levels of pro- and anti-inflammatory cytokines, as well as white blood cell count and C reactive protein.Moreover, there is a proven correlation between cytokine levels and number of organ failures in ACLF[6,11].
Despite advances in the supportive medical management of patients with liver failure, significant morbidity and mortality persist[12,13].Urgent liver transplantation (LT) remains the definitive treatment in patients with high likelihood of death; however, access to transplant remains limited.In addition, eligibility for transplant can be hampered by psychosocial factors, active substance use, and progressive MOFs that may preclude safe LT or contribute to mortality while awaiting LT[14,15].Expanded treatment options are needed to bridge critically ill patients to LT or to preserve liver function when LT is either contra-indicated or unavailable.Therapeutic plasma exchange (TPE) has been proposed as a beneficial treatment modality in these patients.The practice of exchange transfusion in patients with cirrhosis dates back to the 1960s when exchange blood transfusion was employed for the treatment of hepatic coma[16].Therapies were later modified to TPE as apheresis equipment became more widely available and as a means to reduce the risks associated with whole blood transfusion[17,18].Historically, TPE in liver failure has been primarily described in case series and cohort studies.The first randomized control trial (RCT) describing the utility of TPE in ALF patients was reported in 2016 by Larsenet al[19].
TPE in liver failure requires the extracorporeal removal of large compounds from the blood, including albumin-bound and water-soluble toxins and replacement with plasma and/or albumin.As shown in Figure 1, these toxins include cytokines, endotoxins, bilirubin, bile acids, ammonia, and aromatic amino acids[20,21].These substances have been proposed as important mediators of both hepatic encephalopathy (HE) and MOFs in ALF and ACLF[8,22-24].By comparison, extracorporeal albumin dialysis (ECAD) systems remove albumin-bound and water-soluble toxinsviahemodialysis augmented by an albumin-infused dialysate with or without the addition of adsorption columns (charcoal filter and anion exchange resins).These ECAD systems include the molecular adsorbent recirculation system (MARS), single pass albumin dialysis, and fractionated plasma separation and adsorption[25-27].
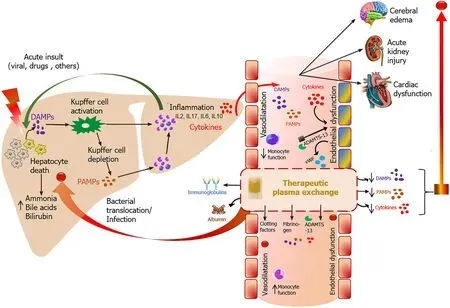
Figure 1 Theoretical model depicting the therapeutic effects of therapeutic plasma exchange in liver failure.
When considering the therapeutic differences between TPE and ECAD, MARS in particular has been recognized to be more costly than TPE and can entail a more logistically complex initiation.Furthermore, the MARS filter-membrane dictates a size selection threshold of approximately 50 KDa[28], whereas TPE is capable of removing larger molecular proteins, including antibodies, immune complexes, and lipoproteins[29].To date, no head-to-head adult clinical trial has directly compared TPE with MARS or any of the ECAD systems.However, in a retrospective single center pediatric study comparing MARS with the combination of TPE and hemodialysis, TPE and hemodialysis effected a greater reduction in bilirubin, ammonia, and international normalized ratio[30].Another theoretical advantage of TPE over ECAD hinges on the exchange of plasma, which replaces plasma proteins, including clotting factors, that may be decreased as a result of impaired hepatic synthetic function in both ALF and ACLF.
EFFECT ON BIOCHEMICAL PARAMETERS AND CLINICAL OUTCOMES
Acute liver failure
TPE has been shown to reduce levels of circulating inflammatory cytokines, improve hemodynamics, and improve transplant-free survival in ALF[9,19,31-33].While encouraging, head-to-head comparisons between the studies supporting these findings have been challenging due to the broad variation in treatment protocols.Often the volume of exchange, treatment frequency and duration of therapy vary between studies.
Specifically, TPE has been shown to moderate TNF-α, histone-associated DNA (member of the DAMP family), IL-6, IL-8, endotoxins, bilirubin, ammonia, and to improve coagulopathy[9,19,34].In addition, TPE modulates adaptive immunity in ALF through the reduction of soluble B7 molecules, particularly sCD86[35].Soluble B7 molecules are produced by injured hepatocytes and increase the expression of cytotoxic T-lymphocyte-associated protein 4 on CD4+ T cells, resulting in impaired antimicrobial responses and increased susceptibility to infections[35].
In the only RCT designed to study outcomes associated with high volume TPE (HVTPE) in ALF, patients who received HV-TPE manifested significantly improved mean arterial blood pressure (MAP) with associated reduction in vasopressor requirement when compared to patients who received standard medical therapy (SMT) only[19].In the same study, plasma creatinine remained stable in the HV-TPE group but increased significantly in the SMT group.Accordingly, fewer HV-TPE patients required renal replacement therapy when compared to those who received SMT.In contrast, Wiersemaet al[31] reported no significant reduction in vasopressor requirement in ALF patients receiving TPE, despite reporting significantly improved MAP on therapy.Notably, this single arm, single centered study employed standard volume TPE as opposed to HV-TPE.
In addition to hemodynamic benefits, TPE has been shown to reduce ammonia level, improve HE grades and cerebral hemodynamics independent of simultaneous filtration or dialysis[33,36].However, TPE has not been shown to effect significant differences in intracranial pressure (ICP) in ALF, though few patients in Larsen’s study underwent invasive ICP assessment (32 of the randomized 182 patients)[19].On the contrary, a retrospective review of 43 patients with Wilsonian-ALF who received HVTPE manifested no improvement in ammonia or creatinine levels, but did demonstrate improved transplant-free survival at 90 d[37].
Finally, Larsen’s RCT in ALF demonstrated a significant improvement in transplant-free survival in patients who received HV-TPE when compared to SMT [hazard ratio (HR) 0.56, 95% confidence interval (CI) 0.36-0.86,P= 0.0083], with no difference in outcomes between paracetamol and non-paracetamol etiology of liver failure[19].In subgroup analysis of the same study, HV-TPE was shown to specifically improve survival among patients not listed for LT due to contraindications.By contrast, no survival benefit was identified in patients who received HV-TPE as a bridge to LT.Other non-randomized studies in ALF have reported improvement in survival days with TPE in non-transplanted patients[38,39].There have been no studies to date that have examined the combination of TPE with any of the ECAD systems in ALF patients.
Acute on chronic liver failure
Patients with ACLF have been shown to manifest significantly higher levels of cytokines (TNF- alpha, IL-10, IL-2, IL-4, and IFN-Y) compared to healthy controls.These same cytokines are also effectively reduced after TPE[40].In the same study by Maoet al[40], higher cytokine levels predicted poor prognosis irrespective of the treatment received.Moreover, bilirubin levels, coagulopathy, and ammonia levels have been shown to improve after TPE-based therapy[41-43].The effect of TPE on blood pressure and vasopressor requirement in ACLF patients has not been reported.In their single center and small sample size study, Stahl et.al.reported no difference in vasopressor requirement between patients who underwent TPEvsSMT[44].
TPE has been shown in limited series to improve survival in ACLF; however, this data is limited by protocol variation.Many of these studies have been performed in Asia among patients with hepatitis B virus- (HBV) related ACLF, used different definitions for ACLF, combined TPE with other liver support systems, and were single center retrospective studies[42,45-47].Tanet al[48] reported improved survival with TPE-based therapies (combined with other extracorporeal therapy) compared to SMT in non-transplanted patients at 30 d and 90 d with a pooled odds ratio (OR) of 0.60 [95%CI: 0.46-0.77].In the only RCT of TPE in ACLF, patients with HBV ineligible for LT who received TPE-based therapies manifested significantly improved survival rates when compared to patients who received SMT (60%vs47%,P< 0.05) at 90 d[47].In addition, Maoet al[45] demonstrated improved survival with TPE among patients with HBV-ACLF and model for end-stage liver disease (MELD) scores between 20-30 (50%) when compared to patients with MELD scores above 30 (31.7%)[45].Whether the results of these studies can be extrapolated and generalized to the ACLF patient population at large remains uncertain.Stahlet al[44] retrospectively studied the differences in outcomes between ACLF patients bridged to LTvspatients bridged to spontaneous recovery.In this study, the risk of 30-d mortality was significantly lower in LT candidates (bridge to transplant group) than in non-transplant candidates (recovery strategy group) treated with TPE (HR 0.35, 95%CI 0.14-0.87,P= 0.024).
As described above, TPE is commonly combined with another dialysis modality depending on the individual patient profile (coagulopathy, renal function, HE, or water and/or electrolyte imbalance).Although continuous renal replacement therapy (CRRT), without TPE, is commonly employed in liver failure-induced severe hyperammonemia to reduce the risk of cerebral edema and intracranial hypertension (ICH)[49,50], no head-to-head comparison study has yet been done to compare ammonia clearance in TPEvsCRRT.Among patients with HBV-ACLF, Yaoet al[43] compared TPE with double plasma molecular adsorption (DPMAS) therapy, a special broadspectrum adsorption column that binds inflammatory mediators and bilirubin.Their group found a significantly higher rate of 28-d survival in the TPE with DPMAS group compared with TPE alone (57.4%vs41.7%,P= 0.043) only among patients with intermediate and advanced stage ACLF (defined as prothrombin activity less than 30%)[43].Separate studies have shown that DPMAS alone or in combination with TPE in ACLF does not confer survival benefits despite increasing the clearance of bilirubin[42,43].
Severe acute alcohol-associated hepatitis (SAH) is recognized to be a common precipitant of ACLF[5]; however, TPE has not been specifically studied in this important patient population.Moreover, sub-group analysis of the limited number of patients with alcohol-associated liver disease included in the available trials has not been described.Case reports suggest that TPE with standard medical therapy may lead to clinical improvement in patients with SAH[51,52].Randomized, controlled trials in patients with SAH are needed to better define the therapeutic effect of TPE for this indication.
TECHNICAL ASPECTS
TPE can be performed by either centrifugation or filtration-based mechanisms.Centrifugation separates the blood into its components using density, whereas filtration uses a hollow fiber design to separate the plasma from the cellular components.Both centrifugation and filtration-based systems are similar in safety, efficiency, therapeutic effects[53,54], and are approved by the Food and Drug Administration for use in the United States.TPE is usually provided in collaboration with nephrologists or hematologists depending on the center’s preference.
REPLACEMENT FLUID, VOLUME, AND DURATION
Acute liver failure
Typical TPE treatments exchange 1 to 1.5 times the patient’s estimated plasma volume, approximately 3 L in an average sized adult.For reference, a plasma volume is an estimate of the total volume of plasma in an individual and is a common unit of measurement in therapeutic apheresis procedures.Plasma volume can be calculated from estimated total blood volume using common physiological variables, including an individual’s sex, height, weight, body muscle composition, and hematocrit[55].The removal of substances using TPE follows the formula: y/yo= e-x, where y and yoare the concentration of the removed substance after and before plasma exchange and x is the number of plasma volumes processed[56].A 1 to 1.5 plasma volume exchange will remove approximately 70% of the substances in the intravascular space[56].
The only RCT comparing TPE and SMT in ALF patients studied HV-TPE, defined as plasma replacement at 15% of ideal body weight or 8 to 12 L per session[19].HV-TPE should remove approximately 90%-98% of the toxins in the intravascular space.The majority of studies on TPE in ALF patients before this RCT treated one plasma volume (2 L to 4 L) during each exchange[38,57-59].Recently, Stahlet al[60] in their single center study compared 20 patients with ALF who received low volume TPE and SMT with 20 matched historical controls who received SMT only.TPE volume exchange was employed using 3 L to 4L per session daily until clinical improvement or LT.No head-to-head comparison of standard volume and HV-TPE in ALF has been performed, but the current evidence favors HV-TPE for ALF[61,62].
There is also no consensus or evidence-based strategy for the frequency and duration of treatment.A small single center study showed that one treatment session of TPE is associated with improvement in biochemical parameters and survival in patients with Wilsonian ALF[37].The RCT by Larsen et.al performed HV-TPE for 3 consecutive days[19].Other studies employed either the same regimen or every other day treatments, and continued until the patient improved clinically, died, or underwent LT[63-65].The most commonly used replacement fluid is plasma, although albumin or plasma substitute is sometimes used in conjunction with plasma[66-69].However, no studies have used albumin alone as a replacement fluid.Plasma is typically chosen as a replacement fluid as it contains coagulation factors and is thought to replenish those missing as a consequence of the underlying liver dysfunction.
Acute on chronic liver failure
All studies in the ACLF population have used standard volume replacement ranging from 2 L to 4.5L exchange per session.Most studies utilized plasma as replacement fluid and performed TPE sessions 2 to 3 times per week and continued until clinical improvement, transplant, or death[41,70-72].Only one study reported daily plasma exchange, but the proportion of the study population that received daily exchanges was not described[41].
ANTICOAGULATION
Sodium citrate and heparin are the two common anticoagulants employed to prevent clotting of the extracorporeal circuits.The patient’s clinical condition and physician’s preferences guide selection; both agents can be used if a single agent is inadequate for anticoagulation.Citrate is preferred because of its shorter half-life of 30-60 min, favorable safety profile, rapid reversibility with intravenous calcium, and its minimal systemic anticoagulation effect[73].Sodium citrate undergoes hepatic and renal metabolism.Patients with liver failure are particularly susceptible to citrate toxicity as a consequence of impaired hepatic metabolism, often exacerbated by concomitant renal impairment.Citrated plasma replacement fluid can further worsen the risk of procedural hypocalcemia.Citrate is partly cleared by the kidney and can be safely utilized in acute kidney injury as long as the acid-base balance is closely monitored[74,75].In a single study, tandem procedure with dialysis reduced the risk of citrate toxicity in ACLF patients undergoing TPE[76].
Common adverse effects of citrate include hypocalcemia (with or without symptoms) and metabolic alkalosis.Symptomatic hypocalcemia is not uncommon and occurs in 1.5% to 9% of all patients undergoing TPE[74].Notably patients receiving TPE for liver failure are at increased risk of hypocalcemia due to the associated metabolic impairment.Prophylactic calcium replacement based on citrate load and continuous ionized calcium monitoring is recommended[29].Supplementation with Calcium gluconate or Calcium chloride can reduce the risk of symptomatic hypocalcemia[77].
Some physicians favor heparin because of the associated risks with citrate as described above.The application of both unfractionated and low molecular weight heparin have been reported[78,79].Nevertheless, most patients can undergo filtrationbased TPE without the need for anticoagulation similar to anticoagulation-free hemodialysis and hemofiltration[80-82].
COMBINATION WITH OTHER EXTRACORPOREAL THERAPY
Acute kidney injury requiring CRRT is a common manifestation of MOF in both ALF and ACLF[83-85].In addition, CRRT is commonly utilized in patients with severe hyperammonemia to reduce the risk of ICH and cerebral edema[49,50,86].CRRT is usually delivered over 24 h and the interruption of CRRT for TPE may compromise the duration of CRRT.Moreover, additional vascular access for TPE exposes the patient to the otherwise avoidable risk of catheter related complications.Simultaneous dialysis and TPE was first introduced in 1999; descriptions of the safety and feasibility of the combined therapies are limited to case reports and case series[21,87-90].There are no defined standards for connection; tandem procedures connected in series or parallel have been reported in the literature[21,80,87,75,91].These tandem connections have the advantage of minimizing vascular access procedures.
The combination of TPE with other extracorporeal therapies aside from CRRT in adults is not well described.In a randomized controlled study from Huanget al[92], MARS in combination with TPE was shown to reduce serum total bilirubin more effectively when compared with MARS monotherapy.There was no significant difference in survival between the two groups.However, the theoretical benefit of MARS therapy combined with TPE is unclear, as both therapies rely on the removal of albumin-bound toxins.TPE employed simultaneously with extracorporeal membrane oxygenation (ECMO) in adults with liver failure has not been reported.However, tandem ECMO, TPE, and CRRT combination therapy has been described in the pediatric population with sepsis-induced multiorgan failure[93].
COMPLICATIONS
The common complications associated with TPE are related to the choice of anticoagulation, replacement fluid, and vascular access.This includes citrate-induced hypocalcemia, hemodynamic instability, and transfusion reactions.In their RCT of HV-TPE in ALF patients, Larsen et.al found no significant differences in cardiac arrhythmias, pancreatitis, transfusion related acute lung injury, acute respiratory distress syndrome, hemorrhage, and infection between patients who received HV-TPEvsSMT[19].A prospective study comparing HV-TPE with SMT in Wilsonian ALF similarly demonstrated no significant difference in the incidence of complications[37].In addition, TPE has been shown to be safe and tolerable in ACLF patients; severe procedure-related adverse effects have not been reported[44,47].An open label RCT in ACLF patients reported a higher rate of hypotension in patients who received TPEbased therapy compared to SMT (20.2%vs9.2%,P= 0.02)[46].Moreover, there were no significant differences in the rates of bleeding, infection, and respiratory failure between groups[47].
CURRENT GUIDELINES
The 2019 American Society for Apheresis (ASFA) has recommended HV-TPE as a first line therapy for ALF and fulminant Wilson disease.In ALF, ASFA recommends performing at least 3 HV-TPE procedures daily and to consider performing daily treatments until LT or liver recovery.In fulminant Wilson disease, daily standard volume plasma exchange treatments until LT or liver recovery is recommended[61].The 2016 European Association for the study of liver disease recommended HV-TPE as a level I, grade I evidence in ALF, but no recommendation has been made for ACLF[62].The 2011 American Association for the Study of Liver Disease guidelines suggested plasma exchange as a means to acutely lower serum copper and limit copper-mediated kidney damage in Wilsonian ALF while waiting LT.However, no recommendation was made for the general use of TPE in ALF and ACLF patients[94].
CONCLUSION
Advanced therapies aimed at improving survival in liver failure rely on the removal of toxins and inflammatory mediators while simultaneously supporting the synthetic and metabolic function of the liver while awaiting either LT or spontaneous hepatic regeneration.Although no ideal extracorporeal liver replacement therapy yet exists, TPE remains a safe, reliable, and feasible treatment.Future studies should replicate the survival benefit demonstrated by Larsenet al[19], examine the role of combination therapies with ECADs, identify which etiologies of ALF and ACLF are best served by TPE, and confirm the optimal exchange volume, frequency, and duration of treatment.
杂志排行
World Journal of Hepatology的其它文章
- Evolution of liver transplant organ allocation policy: Current limitations and future directions
- Antibiotic prophylaxis in patients with cirrhosis: Current evidence for clinical practice
- Kidney transplant from donors with hepatitis B: A challenging treatment option
- Unpacking the challenge of gastric varices: A review on indication,timing and modality of therapy
- Pathogenesis of autoimmune hepatitis
- Current state of endohepatology: Diagnosis and treatment of portal hypertension and its complications with endoscopic ultrasound