Efficacy and effect on serum VEGF-C of mild moxibustion plus functional exercise for upper-limb lymphedema after breast cancer surgery
2021-08-26HuXiangli胡向丽ChenFang陈芳
Hu Xiang-li (胡向丽), Chen Fang (陈芳)
The First Affiliated Hospital of Xinjiang Medical University, Urumchi 830054, China
Abstract
Keywords: Moxibustion Therapy; Moxa Stick Moxibustion; Exercise Therapy; Breast Neoplasms; Postoperative Complications; Breast Cancer Lymphedema; Vascular Endothelial Growth Factor C
Breast cancer is one of the most common types of female malignant tumor and its incidence continues to exhibit an upward trend year-by-year that seriously threatens female’s health[1]. Surgery is the preferred treatment for breast cancer. Post-operative complications include subcutaneous effusion, flap necrosis, lymphedema of the affected upper limb,incision infection and so on[2]. Upper-limb lymphedema is one of the most common complications after breast cancer surgery, clinically manifested by swelling, pain,numbness, and limited lifting of the affected limb. It seriously affects the patients’ quality of life, and results in negative emotional states such as anxiety and depression, thereby delaying radiotherapy,chemotherapy and other necessary treatments[3-4].Current treatments of upper-extremity lymphedema mainly include pharmacotherapy (e.g. diosmin and batroxobin) and physical therapy (e.g. upper-extremity exercise, manual lymphatic drainage and compression bandages), which can relieve symptoms to some extents,but with unstable efficacy, and symptoms are prone to relapse after withdrawal of these treatments[5].Moxibustion is an important component of traditional Chinese medicine (TCM), which can tonify qi to warm yang and expel blood stasis to dredge collaterals. It shows remarkable curative effects in the treatment of edematous diseases[6]. Thus, this study aims to observe the clinical efficacy of mild moxibustion plus functional exercise against upper extremity lymphedema after breast cancer surgery and its effect on serum vascular endothelial growth factor C (VEGF-C). The report is described as follows.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Diagnostic criteria in Western medicine
The diagnostic criteria of upper-limb lymphedema after breast cancer surgery referred theSurgery[7]:diagnosed with breast cancer via pathological examination; circumference of the affected upper limb exceeds that of the healthy upper limb by at least 2 cm.
1.1.2 Diagnostic criteria in TCM
Adopting the syndrome differentiation criteria of qi deficiency and blood stasis in theGuiding Principles for Clinical Study of New Chinese Medicines[8]. Primary symptoms: swelling, numbness of the affected limb, a fixed local stabbing pain, shortage of qi, no desire to speak and fatigue; secondary symptoms: pale complexion, symptom exacerbation due to physical activity, spontaneous sweating, scaly skin, a purple or ecchymotic tongue with white coating, and sunken,unsmooth and weak pulse.
1.2 Inclusion criteria
Those who met the diagnostic criteria of upper-limb lymphedema after breast cancer surgery and the syndrome differentiation criteria of qi deficiency and blood stasis; aged 20-60 years old; had an estimated survival time of more than 6 months; informed and consented to participate in this study.
1.3 Exclusion criteria
Those who had breast tumor recurrence or metastases; with cardiac, hepatic, renal disease or other serious diseases; with upper-limb lymphedema caused by deep vein thrombosis or tumor thrombus; were pregnant or during lactation.
1.4 Criteria for elimination and dropout
Those who did not receive treatment as prescribed or used other treatments due to poor compliance;condition deteriorated or severe adverse reactions occurred; proposed to withdraw from the study.
1.5 Statistical analysis
The data were analyzed by SPSS 22.0 software. The measurement data conforming to normal distribution and homogeneity of variance were expressed as mean ±standard deviation (±s) and analyzed witht-test. Nonparametric tests were used for measurement data that did not conform to normal distribution or homogeneity of variance.P<0.05 was taken as statistically significant.
1.6 General data
A total of 78 patients were enrolled from our hospital between January 2018 and March 2020. The patients were divided into a control group and an observation group by the random number table method, with 39 cases in each group. No dropout occurred during the trial.The youngest and oldest were 34 and 58 years old in the patients in the observation group, and 32 and 60 years old in the control group, respectively. There were no statistically significant differences between the two groups in baseline age, tumor site and pathological type(allP>0.05), confirming that the two groups were appropriately comparable (Table 1).

Table 1. Baseline characteristics in the two groups
2 Treatment Methods
2.1 Control group
The control group received functional exercise, mainly including shoulder rotation movement, rope pulling movement, finger climbing movement and upper-limb extension movement. The functional exercise lasted for 20 min each time. The patient performed twice per day,once in the morning and the other at night, for a total of 4 weeks.
2.2 Observation group
The observation group was treated with the same functional exercise plus mild moxibustion.
Acupoints: Quchi (LI 11), Jianyu (LI 15) on the affected side, and bilateral Xuehai (SP 10), Zusanli (ST 36) and Yinlingquan (SP 9).
Methods:The patient took a supine position and exposed the local skin. After igniting the moxa stick, the doctor aimed the moxa stick at the selected acupoints and conducted mild moxibustion approximately 3 cm away from the skin. Moxibustion was applied at each acupoint for 5-10 min. Slight redness of the local skin and warm feeling without burning pain was preferable. The patient received treatment once every other day for 4 weeks.
3 Results Observation
3.1 Observation items
3.1.1 Difference in circumference of the two upper limbs
The circumferences of the two upper limbs were measured at 15 cm above the cubital crease, and the difference between the two sides was compared before and after treatment.
3.1.2 Lymphatic flow of the affected upper limb
Lymphatic flow of the affected upper limb was measured before and after treatment by radionuclide method.
3.1.3 Disability of arm, shoulder and hand (DASH)
DASH questionnaire was used to evaluate patient’s affected limb function before and after treatment, with a score ranging from 0 to 100 points (the higher the score,the more severe the disability)[9].
3.1.4 Functional assessment of cancer therapy-breast(FACT-B)
FACT-B questionnaire was used to evaluate patient’s quality of life before and after treatment, with a score ranging from 0 to 144 points and the higher the score,the better the post-mastectomy quality of life[10].
3.1.5 Serum VEGF-C level
Fasting venous blood of the patient was drawn before and after treatment, and then the serum VEGF-C level was determined by the enzyme immunoassay method.
3.2 Efficacy evaluation
The efficacy index was calculated by the change of difference in circumference between the two upper limbs, and the clinical efficacy was evaluated according to the efficacy index[11]. The efficacy index = (Beforetreatment circumference of the affected upper limb -After-treatment circumference of the affected upper limb) ÷ Difference in circumference between the two upper limbs × 100%.Markedly effective: The efficacy index was >90%.Effective: The efficacy index was ≥10%, but ≤90%.Invalid: The efficacy index was <10%.
3.3 Results
3.3.1 Comparison of the therapeutic efficacy
After treatment, the total effective rate was 94.9% in the observation group, and it was significantly higher than 71.8% in the control group (P<0.05), (Table 2).
3.3.2 Comparisons of the difference in circumference between the two upper limbs and lymphatic flow of the affected upper limb
Before treatment, there was no significant difference in the difference in circumference between the two upper limbs or lymphatic flow of the affected upper limb between the two groups (bothP>0.05). The difference in circumference between the two upper limbs of the two groups decreased significantly after treatment (bothP<0.05), but it was significantly lower in the observation group than in the control group (P<0.05). The lymphatic flow of the affected upper limb of the two groups increased significantly after treatment (bothP<0.05), but it was significantly greater in the observation group than in the control group (P<0.05), (Table 3).
3.3.3 Comparisons of the DASH and FACT-B scores
Before treatment, there were no significant differences in the DASH and FACT-B scores between the two groups (bothP>0.05). The DASH scores of the two groups decreased significantly after treatment (bothP<0.05), but it was significantly lower in the observation group than in the control group (P<0.05). The FACT-B scores of the two groups increased significantly after treatment (bothP<0.05), but it was significantly higher in the observation group than in the control group (P<0.05),(Table 4).
3.3.4 Comparison of the serum VEGF-C level
Before treatment, there was no significant difference in the serum VEGF-C level between the two groups(P>0.05). After treatment, the serum VEGF-C level increased significantly in the observation group (P<0.05),whereas the control group did not show significant change (P>0.05). The post-treatment serum VEGF-C level in the observation group was significantly higher than that in the control group (P<0.05), (Table 5).
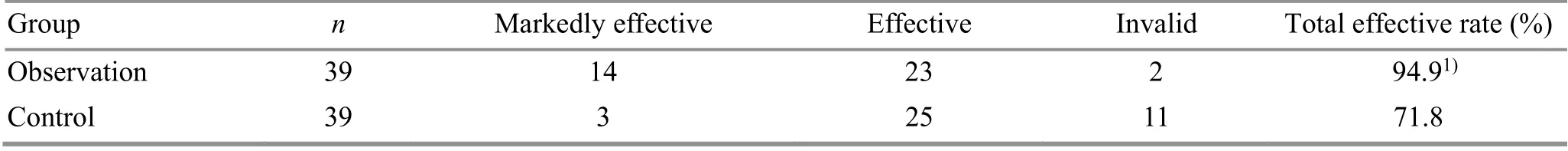
Table 2. Comparison of the total effective rate between the two groups (case)
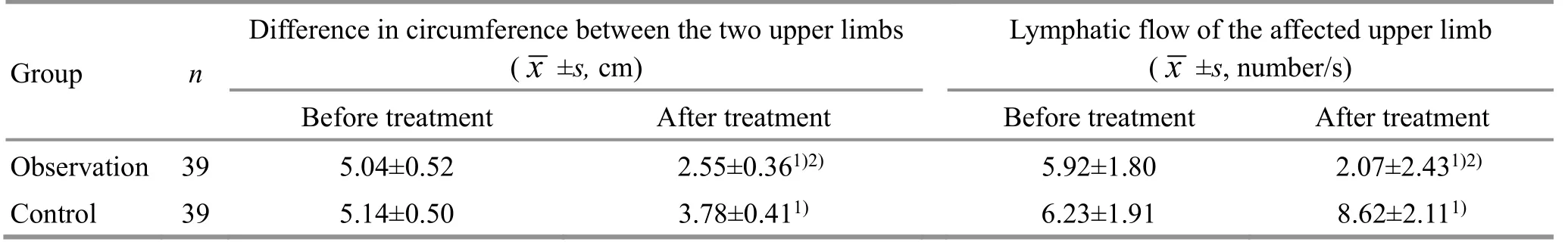
Table 3. Comparisons of the difference in circumference between the two upper limbs and lymphatic flow of the affected upper limb between the two groups

Table 4. Comparisons of the DASH and FACT-B scores between the two groups ( x ±s, point)

Table 5. Comparison of the serum VEGF-C level between the two groups ( x ±s, pg/mL)
4 Discussion
Upper-limb lymphedema is a common complication after breast cancer surgery, mainly caused by axillary lymph node dissection. This surgery usually disrupts plenty of lymphatic vessels, leading to lymphatic obstruction. If the compensatory capacity of lymphatic circulation is diminished or the lymphoid load increases,lymphedema of the affected upper limb can occur[12].Radiotherapy can cause local tissue fibrosis, radiationinduced skin damage and muscular contractures,thereby compressing the reflux pathway of lymph.Radiotherapy can also induce lymphangitis and inhibit lymphangiogenesis, which may increase the risk of lymphedema[13]. Further, age, body mass index and the size of the breast mass also appear to be risk factors of upper-limb lymphedema after breast cancer surgery[14].
VEGF-C is a cell-specific growth factor. It has a high affinity for vascular endothelial growth factor receptor 3(VEGFR-3), which is expressed on endothelial lymphatic cells. The binding of VEGF-C to VEGFR-3 can influence the differentiation of lymphatic endothelial cells, inhibit their apoptosis and promote lymphangiogenesis[15]. In study of Visuri MT,et al[16], VEGF-C was injected into the hind limbs of sows. The results showed that the growth of new lymphatic vessels in the area of excision was induced, and no signs of sprouting angiogenesis or increased blood vascular permeability were observed. In study of Hou CQ,et al[17], VEGF-C was injected into lymphedema limbs of rabbits. The results suggested that the swelling of the limbs was reduced and the microlymphatic vessel number declined. The efficacy increased gradually with time. It can be seen that sufficient VEGF-C concentration can promote lymphangiogenesis and alleviate lymphedema.Therefore, modulation of the serum VEGF-C level may be a potential therapeutic target in upper-limb lymphedema after breast cancer surgery.
Functional exercise is a widely used physical therapy.It can increase muscle strength, prevent muscle atrophy and joint stiffness in order to avoid venous compression by scar tissue and reduce the obstruction of venous return. It can also promote lymphatic reflux to relieve edema through the stress of muscles contraction and relaxation on lymphatic vessel[18]. Functional exercise should be gradual and stepwise because lymphedema can be induced or aggravated by excessive exercise.
Upper-limb lymphedema after breast cancer surgery belongs to the category of ‘edema’ and ‘vessel Bi-Impediment’, characterized by deficiency in root and excess in branch[19]. The qi of patients with breast cancer is already deficient. Surgery can further damage the qi and blood, leading to more severe deficiency of healthy qi. Deficient qi will fail to promote blood flow and result in blood stasis. Blood stasis can also result from vessel damages during surgery. Prolonged blood stasis leads to stagnation of body fluids which later on causes retention of fluid under the skin, resulting in the disease. Thus, qi deficiency and blood stasis is a common pathogenesis of upper-limb lymphedema after breast cancer surgery, and treatment should focus on tonifying qi, expelling blood stasis, dredging collaterals and eliminating dampness[20].
Mild moxibustion is characterized by warm stimulation, through which the effect of warming yang for tonifying qi, warming and dredging meridians and collaterals, and expelling blood stasis for regulating qi can be exerted. This therapy holds particularly true for the patients with qi deficiency and blood stasis. Quchi (LI 11),Jianyu (LI 15), Xuehai (SP 10), Zusanli (ST 36) and Yinlingquan (SP 9) were selected for mild moxibustion in this study. Quchi (LI 11) and Jianyu (LI 15), locate in the affected areas, can stimulate Yangming meridians,dredge collaterals and regulate qi and blood for improving the stagnation of qi, blood and water of the upper limb. Xuehai (SP 10) is good at treating various disorders of blood. It can invigorate spleen to eliminate dampness, nourish blood and expel blood stasis. Zusanli(ST 36), the He-Sea point of the Stomach Meridian of Foot Yangming, has the function of invigorating spleen and stomach and tonifying qi and blood. Yinlingquan(SP 9), the He-Sea point of the Spleen Meridian of Foot Taiyin, can strength spleen for regulating qi, dredge collaterals and induce diuresis for alleviating edema,which is an important acupoint for treating edema. The compatibility of these acupoints can achieve the purpose of tonifying qi for strengthening the vital, removing stasis for dredging collaterals, inducing diuresis for alleviating edema.
The results of this study showed that the total effective rate was significantly higher in the observation group than in the control group (P<0.05). The difference in circumference between the two upper limbs of the two groups decreased significantly after treatment (bothP<0.05), but it was significantly lower in the observation group than in the control group (P<0.05). The lymphatic flow of the affected upper limb of the two groups increased significantly after treatment (bothP<0.05), but it was significantly greater in the observation group than in the control group (P<0.05). The DASH scores of the two groups decreased significantly after treatment (bothP<0.05), but it was significantly lower in the observation group than in the control group (P<0.05). The FACT-B scores of the two groups increased significantly after treatment (bothP<0.05), but it was significantly higher in the observation group than in the control group (P<0.05).The results indicate that mild moxibustion combined with functional exercise for upper-limb lymphedema after breast cancer surgery is effective, as it can reduce the difference in circumference between the two upper limbs, increase the lymphatic flow of the affected upper limb, and improve the limb function and the quality of life. After treatment, the serum VEGF-C level increased significantly in the observation group (P<0.05), whereas the control group did not show significant change(P>0.05). The post-treatment serum VEGF-C level was significantly higher in the observation group than in the control group (P<0.05). The results indicate that the efficacy of mild moxibustion combined with functional exercise for upper-limb lymphedema after breast cancer surgery is certain, which might be associated with the regulation of serum VEGF-C level.
In conclusion, the efficacy of mild moxibustion combined with functional exercise for upper-limb lymphedema after breast cancer surgery is certain,which can reduce the difference in circumference between the two upper limbs, increase the lymphatic flow of the affected upper limb, improve the limb function and the quality of life, and regulate serum VEGFC level. Therefore, this combination therapy is worthy of clinical promotion.
Conflict of Interest
The authors declare that there is no potential conflict of interest in this article.
Acknowledgments
There was no project-fund supporting for this study.
Statement of Informed Consent
All participants were informed and consented to participate in this study.
Received: 10 July 2020/Accepted: 9 October 2020
猜你喜欢
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Modern literature study of auricular point therapy for primary insomnia
- Effects of acupuncture plus MOTOmed intelligent motor training in treating children with spastic cerebral palsy
- Adjunctive effects of acupressure therapy on pain and quality of life in patients with knee osteoarthritis: an interventional study
- Muscle regions of meridians warm needling method plus pricking Jing-Well points for blood-letting in the treatment of shoulder-hand syndrome after stroke
- Clinical study on long-snake moxibustion plus Western medicine in treating chronic heart failure due to heart-kidney yang deficiency
- Effect of moxibustion at Shenque (CV 8) on myocardial remodeling and function in exercise-induced fatigue rats