Think twice before implanting leads in a swimmer: challenges in lead implantation of an implantable cardioverter-defibrillator
2021-08-14DimitriosVarvarousisVasileiosDoulamisNikolaosParzakonisGeorgiosKourgiannidis
Dimitrios Varvarousis, Vasileios Doulamis, Nikolaos Parzakonis, Georgios Kourgiannidis
1. Cardiology Department, Asklepeion General Hospital, Athens, Greece; 2. Cardiology Department, 251 Air Force General Hospital, Athens, Greece
An 84-year-old male patient with an im-plantable cardioverter defibrillator(ICD) was admitted due to an alarming sound of his ICD. He had a left-sided, dual chamber, dual-coil ICD implanted 7 years ago due to ischemic cardiomyopathy and sick sinus disease.He was asymptomatic, with an excellent functional status. Of note, he was a highly active patient and a regular swimmer (6 months per year). His device interrogation revealed high-voltage lead impedance values over 3 000 Ohms, suggesting a lead fracture, which was confirmed by a chest X-ray (Figure 1A). Additionally, numerous sustained ventricular tachycardia episodes, properly treated, were identified. The decision for the implantation of a new ICD lead was made. This option was favored against the removal of the damaged lead, considering the high risks of such a procedure due to patient’s age and the long time-period since the initial lead implantation. During the procedure, the new lead could not be advanced because of left subclavian venous obstruction (Figure 1B). The decision to implant the new lead on the contralateral side was made. We performed a right subclavian venography, which unexpectedly revealed an additional subtotal obstruction of the vein, at the level near its join with the internal jugular vein (Figure 1C). The procedure was stopped and, in a second procedure, the obstruction in the right subclavian vein was treated with balloon angioplasty and stenting (Figure 1D),before successful re-implantation of the device from the left pocket to the right subclavian area, along with two new leads. The two left-sided leads were abandoned in place. The patient has remained asymptomatic during his two-year follow-up visits,with a good functional status, having followed instructions for limitation of strenuous exercise with the upper extremities. Moreover, chest X-rays have not shown evidence of damage in the venous stent struts after one and two years (Figure 2).
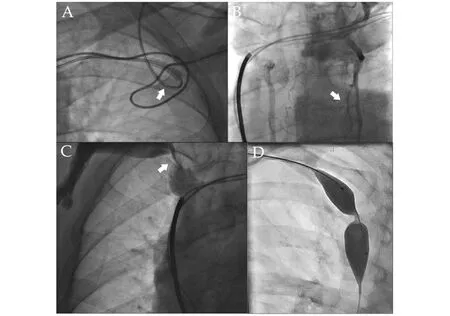
Figure 1 Various chest fluoroscopy views of the patient during different stages in his management. (A): the chest X-ray of the patient has been enlarged, in order to better illustrate the damaged ventricular lead (arrow); (B): left subclavian venography showing a total occlusion of the vein. Large bridging collateral vessels are visible (arrow); (C): right subclavian venography showing a tight stenosis of the vein at the level near its join with the internal jugular vein; and (D): angioplasty of the right subclavian vein with stent implantation.
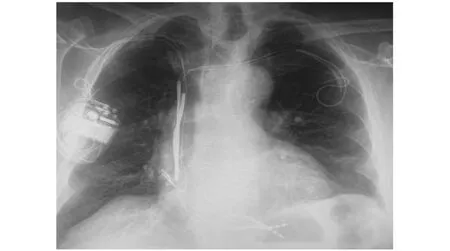
Figure 2 Chest X-ray of the patient two years after device implantation on the contralateral side, via the patent right subclavian vein. There is no evidence of stent damage.
We believe this to be an interesting case, because of the unusual asymptomatic finding of bilateral subclavian venous obstruction in this elderly patient. Ipsilateral asymptomatic subclavian venous obstruction after lead implantation for a cardiac implantable electronic device is not a rare phenomenon,making the implantation of a new lead challenging,in case of lead failure or a device upgrade.[1]Patients carrying dual-coil ICDs carry an even higher risk for venous obstruction, due to increased lead diameter and the presence of a second coil in the superior vena cava.[1]In cases of lead-associated venous occlusion, obscuring the implantation of a new lead, the presence of an additional venous stenosis on the contralateral side is not a frequent observation, and further complicates the clinical dilemmas.In our case, in the absence of trauma- or tumor-related causes, one may be tempted to suspect the Paget-Schroetter Syndrome, the venous variant of the thoracic outlet syndrome.[2]It consists of axillary or subclavian vein thrombosis related to vein compression at the thoracic outlet, eventually with fibrosis and obstruction, attributed to regular and strenuous exercise, using the upper extremities.Anatomical anomalies of the thorax also predispose to this condition. Although the syndrome is encountered more commonly in much younger patients, our patient had been a very regular swimmer with repetitive, intense physical activity for many years. Patients may occasionally present with chronic and non-specific symptoms. Regarding the management of such patients, in the absence of randomized trials or a broad consensus about the best approach, physicians often individualize treatment.[2]Therapeutic options include anticoagulation, avoidance of strenuous physical activity, thrombolysis or pharmacomechanical thrombectomy, in patients in the acute phase with recent-onset symptoms and,while definite treatment consists of surgical thoracic outlet decompression, a complex procedure which must be performed by experienced surgeons and is,thus, reserved for younger, active patients.[2]Venoplasty or stenting together with decompression or exercise restriction based on the patient’s clinical background may be a therapeutic individualized option, especially in elderly patients when patency of the subclavian vein is of utmost importance, as in this case with the indication for implantation of pacing leads.
In conclusion, clinical history of regular exercise with use of upper extremities should be evaluated with extra caution in cases of lead implantation.This is particularly true with large caliber leads as ICD leads or in cases of an extra lead implantation.Preprocedural ultrasound or venography may be exremely useful in such cases and may prevent unexpected challenges during the implantation of pacing or ICD leads regarding venous access.
杂志排行
Journal of Geriatric Cardiology的其它文章
- Leadless cardiac pacemaker implantations after infected pacemaker system removals in octogenarians
- Association between coronary artery calcification and cognitive function in a Chinese community-based population
- Prevalence and modifiable risk factors of degenerative valvular heart disease among elderly population in southern China
- Cardiovascular injuries and SARS-COV-2 infection: focus on elderly people
- Aging is associated with cardiac autonomic nerve fiber depletion and reduced cardiac and circulating BDNF levels
- Acute heart failure in elderly patients: a review of invasive and non-invasive management
