Association between coronary artery calcification and cognitive function in a Chinese community-based population
2021-08-14YaNanMAWuXiangXIEZhiHuiHOUYunQiangANXinShuangRENYanJunMAChengLongLIYangFengWUBinLU
Ya-Nan MA, Wu-Xiang XIE, Zhi-Hui HOU, Yun-Qiang AN, Xin-Shuang REN,Yan-Jun MA, Cheng-Long LI, Yang-Feng WU,✉, Bin LU,✉
1. Department of Radiology, Fuwai Hospital, Peking Union Medical College & Chinese Academy of Medical Sciences;State Key Lab and National Center for Cardiovascular Diseases, Beijing, China; 2. Peking University Clinical Research Institute, Peking University First Hospital, Beijing, China
ABSTRACT Background Coronary atherosclerosis and cognitive impairment are both age-related diseases, with similar risk factors. Coronary artery calcium (CAC), a marker of coronary atherosclerosis, may play a role in early detection of individuals prone to cognitive decline. This study aimed to investigate the relationship between CAC and cognitive function, and the capability of CAC to identify participants with a high risk of dementia in a Chinese community-based population.Methods A total of 1 332 participants, aged 40−80 years and free of dementia from a community located in Beijing were included. All participants completed neurocognitive questionnaires and noncontrast CT examinations. Cognitive performance tests(including verbal memory, semantic fluency, executive function, and global cognitive function tests), the Cardiovascular Risk Factors, Aging, and Incidence of Dementia (CIDE) risk score, and the CAC score (CACS) were evaluated by questionnaires and CT. A CAIDE score ≥ 10 was considered to indicate a high risk of dementia in late-life. Participants were divided into three groups according to CACS (0, 1−399, ≥ 400).Results After adjusting for risk factors, CACS was significantly associated with verbal memory (r = −0.083, P = 0.003) and global cognitive function (r = −0.070, P = 0.012). The prevalence of a high risk of dementia in the subgroups of CACS = 0, 1−399, and ≥400 was 4.67%, 13.66%, and 24.79%, respectively (P < 0.001). Individuals with CACS ≥ 400 had a higher risk of CAIDE score ≥ 10[OR = 2.30 (1.56, 4.56), P = 0.014] than those with CACS = 0. The receiver-operating characteristic curves showed that the capability of CACS to identify participants with a high risk of dementia was moderate (AUC = 0.70, 95% CI: 0.67−0.72, P < 0.001).Conclusions CAC, a marker of subclinical atherosclerosis, was significantly associated with cognitive performance in verbal memory and global cognitive function. CAC had a moderate capability to identify participants with a high risk of dementia, independent of age, education, and other risk factors.
Coronary atherosclerosis and cognitive impairment are both age-related diseases. The incidences of the two diseases are increasing with the rapid aging of the population. There are 50 million people with dementia in the world, and this number is likely to rise to 152 million by 2015. The cost of dementia is forecasted to be approximately two trillion dollars by 2030.[1,2]Therefore, early prevention of cognitive impairment is of great significance.
Cognitive decline has risk factors similar to those for atherosclerosis such as smoking, hypertension,and diabetes.[3]Intracranial and carotid artery atherosclerosis has been indicated to be related to a higher risk of cognitive decline or dementia.[4,5]Coronary artery calcium (CAC), a marker of coronary atherosclerosis, may play a role in the early identification of individuals who are prone to cognitive decline.However, several studies investigating the association between CAC assessed by CT and cognitive function have reported controversial results.[6–10]In addition, these previous studies mainly focused on Europeans and Americans, and the relationship between CAC and cognitive function in the Chinese population is still uncertain. The Cardiovascular Risk Factors, Aging, and Incidence of Dementia(CAIDE) score was the first dementia risk score developed to predict late-life dementia risk. Individuals with a CAIDE score ≥ 9 or ≥ 10 were considered to have a high risk of dementia.[11–13]The capability of CAC to identify participants with a high risk of late-life dementia (CAIDE score ≥ 9 or ≥ 10) was discrepant as well.[14]Moreover, CAC is currently available convenient in clinical practice, and noncontrast chest CT scans and cardiac computed tomography angiography could both be used to assess CAC, especially in smokers undergoing lung cancer screening and patients suspected with coronary artery disease.
This study was designed to determine: (1) whether CAC is related to cognitive performance, including verbal memory, semantic fluency, executive function and global cognitive function, and (2) the capability of CAC to identify participants with a high risk of late-life dementia in a Chinese communitybased population.
MATERIALS AND METHODS
Participants
This study is the baseline survey of Beijing Research on Aging and VEssel (BRAVE), which is an ongoing prospective cohort study investigating the relationships of baseline vascular structure and function with consequent cognitive function in a community-based population. From October to November 2019, all 1 789 residents who were aged 40 to 80 years, were free of dementia, and lived in the Paochang community located in Shijingshan District were invited to participate in this baseline survey, and 1 554 residents were recruited (response rate = 87%). Informed consent was obtained from all participants. This study was performed in accordance with the “Declaration of Helsinki” and approved by Peking University Institutional Review Board (ethical review approval number:IRB0001052–19060) and Fuwai Hospital Institutional Review Board (ethical review approval number:IRB2012-BG-006).
Of the 1 554 participants, 10 were excluded from this study due to missing data for key variables, 178 were excluded because they had not undergone CT scans, and 34 participants were excluded because of coronary stents that would affect coronary calcification assessment. Finally, 1 332 participants were included in this analysis.
Coronary Artery Calcification (CAC)
CAC was measured using a multi-slice CT scan(Brilliance iCT, Philips Healthcare, Cleveland, OH,USA). CT scans were performed when breath-holding, at a tube voltage of 120 V and slice thickness of 2.5 mm. Scan range was from the bifurcation of trachea to the bottom of heart. All images were transferred to a workstation (Advantage Work station version 4.6, GE Healthcare, American) and coronary calcium was evaluated independently.Coronary calcium was quantified with the Agatston score.[15]Each calcium lesion was identified as the hyperattenuating region exceeding the CT density of 130 Houndsfield unit (HU). The CACS was automatically calculated by manually adding all detectable calcification lesions.
Cognitive Function
We assessed cognitive performance in the domains of verbal memory, semantic fluency, executive function and global cognitive function face-to face by using various neurocognitive questionnaire tests.
The verbal memory test involved two parts: immediate and delayed recall. The trained examiners read ten unrelated nouns at 2 s intervals. Participants recalled and repeated the nouns immediately in 2 min. One point was awarded for each correct noun provided. After approximately 5−7 min,participants were required to recall the ten nouns again, and one point was awarded for each correct noun again. The final score (ranging from 0 to 20)was obtained by adding the two scores together.
Semantic fluency was evaluated by the category fluency test (CRF).[16]Participants were required to name as many animals as possible in one minute.Repeated animals did not count. The score was equal to the total number of animals given in one minute.
Executive function was assessed by the Trail Making Test (TMT).[17]Participants needed to complete two tests. For test A, participants were asked to draw lines connecting numbers (1−25) in ascending order without considering colour. For test B, participants were asked to draw lines connecting pink or yellow numbers in an order that alternated between increasing numeric values and colour (i.e., one with pink color; two with yellow color; three with pink color, etc). Considering that some people with a low level of education could not recognize letters, we used numbers of different colors instead of letters in test B. Each test had a maximum duration of three minutes.The test score was the total time taken to complete the two tasks, in seconds.
Global cognitive function was assessed by the Chinese version of the Montreal Cognitive Assessment Basic (MoCA-B) which was designed as a quick evaluation scale to screen for mild cognitive impairment (MCI).[18]The Chinese version of the MoCA-B is a 30-point test administered in 15 min,that assesses nine cognitive domains (executive function, language, orientation, calculation, conceptual thinking, memory, visuoperception, attention and concentration). The total MoCA-B score represented global cognitive function. All interviewers involved in the cognitive tests had attended a Training &Certification program for the MoCA.
Dementia Risk Score
The CAIDE dementia risk score is a validated tool to predict late-life dementia risk based on midlife vascular risk factors comprising age, education level, sex, hypertension, obesity, hyperlipidaemia and physical activity.[12,19]We selected a score of 10 as the cut-off value. A CAIDE score ≥ 10 was considered to indicate a high risk of dementia.[11,13]
Covariates
Blood samples were collected from participants after 12 h of fasting. Total cholesterol (TC), highdensity lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), creatinine and highsensitivity C-reactive protein were measured. Body mass index (BMI, kg/m2) was calculated. Smoking status was categorized as current smoker, former smoker (defined as no smoking in the past 30 days)and never-smoker (defined as smoking fewer than 100 cigarettes in lifetime). Systolic blood pressure(SBP) and diastolic blood pressure (DBP) were measured three times. The average of the second and third measurements was used in the analysis.Hypertension was defined as SBP/DBP≥140/90 mmHg or the use of antihypertension medication.Diabetes was defined as a fasting glucose level ≥126 mg/dL or the use of any hypoglycaemic medication. Depressive symptoms were defined as a score on the Short Version of Center for Epidemiological Studies, Depression Scale (CES-D-10) ≥12.[20]Stroke was defined as an acute episode of focal dysfunction of the brain, retina, or spinal cord lasting longer than 24 h, or of any duration if imaging (CT or MRI)showed focal infarction or haemorrhage relevant to the symptoms.[21]Myocardial infarction was diagnosed according to the fourth universal definition of myocardial infarction.[22]Cancer history was defined as an occurrence of malignant or benign tumour in the past, regardless of treatment.
Data Analysis
CAC was the main independent variable. The CACS was analysed using base-10 logarithm of the CACS plus 1 [log(CACS + 1)] when used as a continuous variable. All participants were divided into three groups according to CACS (CACS = 0, 1−399, ≥400). Baseline characteristics are presented by CACS stratum. The Kolmogorov-Smirnov test was used to assess the distribution of continuous variables. Continuous variables are presented as mean ± SD or median (lower and upper quartile), whereas categorical variables are presented as the number (proportion). Analysis of variance was used to test means across groups for normally distributed variables, and nonparametric Kruskal-Wallis was used for nonnormally distributed variables. Chi-square analysis was used to test differences in distributions for categorical variables.
To determine if there was a relationship between CACS and cognitive performance, we first used the Kruskal-Wallis test to assess cognitive test scores among groups. Then, the estimated mean scores of cognitive tests were compared using analysis of covariance controlling for variables. Model 1 was unadjusted. In model 2, analyses were adjusted for age, education, sex, BMI, TC, HDL-C, LDL-C, highsensitivity C-reactive protein, creatinine, hypertension, diabetes, smoking, stroke, depressive symptoms, myocardial infarction, and cancer. Partial Spearman correlations between CACS and four cognitive function scores were performed, controlling for age, education, sex, BMI, TC, HDL-C, LDL-C,high-sensitivity C-reactive protein, creatinine, hypertension, diabetes, smoking, stroke, depressive symptoms, myocardial infarction, and cancer because these variables may affect cognitive function.
Logistic regression models were used to assess the influence of CACS on whether patients had a high risk of dementia (1 = yes, 0 = no). Using CACS =0 as a reference, odds ratios (ORs) and 95% confidence intervals (95% CI) were presented in CACS =1−399, and CACS ≥ 400 groups. The receiver-operating characteristic curve was plotted to estimate the capability of CACS to discriminate participants with a high risk of dementia (CAIDE score ≥ 10).SPSS version 22.0 was used to perform analysis. A two-sided value ofP< 0.05 was considered statistically significant.
RESULTS
Study Population
Descriptive characteristics of the study population are shown in Table1. Among the 1 332 participants, there were 728,483 and 121 individuals in the CACS = 0, 1−399, and ≥ 400 groups, respectively. The mean age was 59.90 (range 41–79) years old, and 45.35% of participants had positive CAC(CACS > 0). Compared with CACS = 0 group, participants in the CACS = 1−399 and CACS ≥ 400 groups were older, and had higher proportions of male sex, hypertension, diabetes, stroke, and myocardial infarction, as well as higher BMI, SBP,and creatinine; more current smokers, and lower proportions of high education (education ≥ 12 years), and lower TC, LDL-C and HDL-C. The prevalence of depressive symptoms and cancer history in subgroups was nonsignificant (P= 0.079, 0.387).

Table 1 Characteristics of participants by CACS stratum.
Correlation Between CACS and Cognitive Function
On average, the participants recalled 8 (6−10)nouns in the verbal memory test, named 15 (13, 18)animals in 1 min, took 194 (153, 242) s to complete the TMT tests and obtained a score of 25 (23, 27) in the MoCA-B test. Figure 1 shows that the scores of cognitive function tests in subgroups of CACS were different. Compared with the negative CAC group,participants with CACS = 1−399 or ≥ 400 recalled fewer nouns in the verbal memory, took a longer time to complete the executive test, and got lower score on the MoCA-B test (allP< 0.001). In the semantic fluency test, there was a significant difference only between subgroups of CACS = 0 and CACS ≥ 400 (P= 0.003).

Figure 1 Cognitive performance scores in subgroups stratified by CACS. CACS: coronary artery calcium score.
Table 2 shows the adjusted estimated value of cognitive function tests by CACS stratum. In model 1 (not adjusted for any variable), participants with CACS ≥ 400 had lower scores on verbal memory, semantic fluency and global cognitive function tests,and took a longer time to finish the executive function test, than participants with CACS = 0, whereas there was no significant difference in semantic fluency between participants with CACS = 1−399 and those with CACS = 0. In model 2, after adjusting for age, education and other risk factors, only verbal memory function remained significant between subgroups of CACS ≥ 400 and CACS = 0.
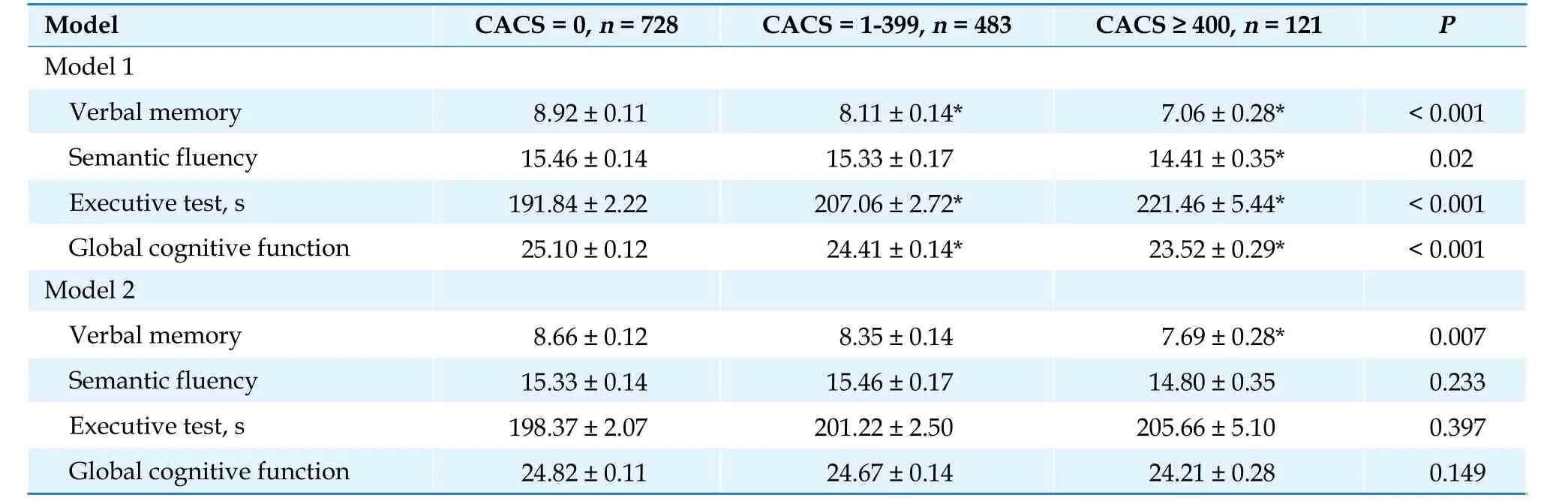
Table 2 The adjusted estimated value of cognitive function tests by CACS stratum.
A partial Spearman’s correlation controlling for age, sex, education, depressive symptoms and other cardiovascular risk factors showed weak but statistically significant correlations between log (CACS + 1)and verbal memory and global cognitive function scores (r= −0.083,P= 0.003;r= −0.070,P= 0.012, respectively), whereas executive function and semantic fluency scores were not correlated with log (CACS + 1)(r= 0.042,P= 0.129; r = −0.011,P= 0.690).
Capability of CACS to Discriminate Participants with a High Risk of Dementia
Among all participants, 130 (9.76%) individuals had a high risk of dementia (CAIDE score ≥ 10). The prevalence of having a high risk of dementia significantly differed across CACS = 0, 1−399, and ≥ 400 subgroups (4.67%, 13.66%, and 24.79%, respectively,P< 0.001). It was a remarkable finding that the proportion of participants having a high risk of dementia increased as CACS increased.
Table 3 presents the association between CAC groups and a high risk of dementia according to CACS category. In different logistic regression models, CAC was related to a high risk of dementia overall, with ORs (95% CI) of 2.65 (2.05, 3.42) and 1.52 (1.09, 2.13) (bothP< 0.05). We also found that the risk of having a CAIDE score ≥ 10 consistently increased with CACS increasing. In model 1, participants with CACS = 1−399 or ≥ 400 had higher risks of CAIDE score ≥ 10 than those with CACS = 0[OR = 3.23 (2.10, 4.97), 6.73 (3.93, 11.52), bothP<0.001]. Individuals with CACS ≥ 400 were more than twice as likely to have a high risk of dementia than those with CACS = 0 after adjusting for age,sex, education, depressive symptoms and cardiovascular risk factors [OR = 2.30 (1.56, 4.56),P=0.014].

Table 3 The association between coronary artery calcium and high risk of dementia late-life (CAIDE scores ≥ 10) by CACS stratum.
Moreover, the receiver-operating characteristic curve showed that CACS had a moderate capability to identify participants with a high risk of dementia, with an AUC=0.70 (95% CI: 0.67−0.72,P<0.001, Figure 2).

Figure 2 The capability of CACS to identify participants with a high risk of dementia. Receiver-operating characteristic curve showed the performance of CACS in predicting a high risk of dementia (CAIDE scores ≥ 10). The AUC was 0.70 (95% CI:0.67-0.72, P <0.001). AUC: area under the receiver operating characteristic curve; CACS: coronary artery calcium score; CAIDE score: the Cardiovascular Risk Factors, Aging, and Incidence of Dementia score; CI: confidence interval.
DISCUSSION
To the best of our knowledge, this was the first prospective, cross-sectional community-based study in a Chinese population to investigate the relationship of CAC with cognition as well as the ability of CAC to identify participants with a high risk of dementia.
In this cohort study, we found that there was a statistically significant correlation between CAC and cognitive performance in verbal memory and global cognitive function. Participants with higher CACS had worse performance in verbal memory and global cognitive function tests. Furthermore,we observed that CAC could moderately identify participants with a high risk of dementia independent of age, education and other risk factors. The risk of having a CAIDE score ≥ 10 markedly increased with increasing CACS.
To date, studies focusing on CAC and cognitive function have produced inconsistent results. In the CARDIA study of middle-aged adults, higher CAC was associated with worse performance on cognitive tests, including worse psychomotor speed and verbal memory.[23]In the ELSA-Brasil cross-sectional study, individuals with higher CAC had poorer performance in executive function and global cognition tests.[7]In elderly individuals, especially white women, a lower CAC score predicted a significantly decreased incidence of dementia.[24]Furthermore,not only the baseline CAC but also the progression of CAC showed a positive association with relevant cognitive impairment. The progression of CAC was a more powerful predictor of cognitive function.[25]Conversely, some studies obtained disparate results. A cohort study conducted in Germany showed that the ankle-brachial index rather than CAC was associated with mild cognitive impairment. The MESA study indicated that CAC > 400 was not associated with dementia.[6,14]The reasons for the different results in these studies mainly include (1) different characteristics of the study population, including age, race, risk factors and so on; (2) different neurocognitive evaluation tests; and (3) diverse confounders that needed to be adjusted.
Cognitive performances were significantly different in subgroups of CACS, but after adjusting for age, education, depressive symptoms, and cardiovascular risk factors, the differences became less pronounced, except for the difference in verbal memory. This finding further illustrated that cognitive impairment was a complex process influenced by diverse factors, especially age and education. Memory impairment is the core symptom in the cognitive loss process.[26]
Dementia has become a societal issue because of worldwide population ageing and the absence of effective treatment. Therefore, primary prevention has been particularly emphasized as a key element.Our results indicated that CAC could moderately identify individuals with a high risk of dementia.People with a higher level of CAC have a higher risk of dementia. Thus, these findings can raise awareness of cognition in individuals, especially in those with a high level of CAC, and thus allow for timely prevention of dementia or cognitive decline by targeting modifiable vascular risk factors.[3]
The pathophysiological mechanisms between CAC and cognitive decline are not well understood,but may be explained by the potential mediating effect of cerebrovascular disease. Atherosclerosis is a gradual and systemic process. CAC, a marker of subclinical cardiovascular atherosclerosis disease,may also be a marker of cerebral atherosclerosis since it has similar pathogenic processes with cerebral atherosclerosis disease. The CAC Agatston score and volume were both associated with cerebral lesions, including subcortical lacunar infarction and high white matter hyperintensities even after adjusting for age, sex and cardiovascular risk factors.Individuals with high CAC scores and large calcification volumes were more likely to have more cerebral infarction, white matter lesions and intracranial arterial stenosis.[27,28]These changes will decrease cerebral perfusion and decrease functional activation of the cerebral cortex and therefore lead to poorer cognitive performance.[5,29–31]From a pathophysiological point of view, cerebrovascular atherosclerosis is more directly related to cognitive function, but in clinical practice, CAC is more commonly used and more readily available. Using CAC to identify individuals who are likely to experience cognitive decline or dementia may be of great significance in the future.
Study Limitations
This study had some limitations. First, this was a cross-sectional study that was unable to obtain the predictive value of CAC for cognitive decline or latelife dementia. Further longitudinal studies are needed to clarify the influence of CAC on cognition and dementia. Second, we analyzed only coronary calcification but did not focus on other vascular calcification, such as carotid artery or aortic atherosclerosis, both of which have been associated with cognitive performance.[4,10,32]Moreover, cognitive decline is a complex process and is correlated with multiple factors. Although we adjusted for as many variables related to cognitive performance as possible, there may still be other relevant factors we did not consider, such as sleep duration.[33]
CONCLUSIONS
CAC exhibited a weak but significant association with verbal memory and global cognitive function.CAC had a moderate ability to identify participants with a high risk of dementia, independent of age,education and other risk factors. Therefore, preventive therapeutic strategies in individuals with a high level of CAC may be effective to slow down the development of cognitive decline or dementia in the future.
Acknowledgments
This study was supported by the Ministry of Science and Technology of China (grant 2016YFC1300400)and Chinese National Key Research and Development Project (grant 2016-I2M-1-011). The authors declare that they have no conflict of interest.
杂志排行
Journal of Geriatric Cardiology的其它文章
- Leadless cardiac pacemaker implantations after infected pacemaker system removals in octogenarians
- Prevalence and modifiable risk factors of degenerative valvular heart disease among elderly population in southern China
- Cardiovascular injuries and SARS-COV-2 infection: focus on elderly people
- Aging is associated with cardiac autonomic nerve fiber depletion and reduced cardiac and circulating BDNF levels
- Acute heart failure in elderly patients: a review of invasive and non-invasive management
- Vulnerable atherosclerotic plaque features: findings from coronary imaging
