Intraparenchymal hepatic hematoma following endoscopic retrograde cholangiopancreatography: Risk factors and conservative approach in acute management
2021-07-24VleriOvidioGiovnniBrunoGiulioSodniCristinLucidiMrcoEmilioBzuro
Vleri D’Ovidio ,,Giovnni Bruno ,Giulio Sodni ,Cristin Lucidi ,Mrco Emilio Bzuro
a GI Endoscopy Unit, S. Eugenio Hospital, Rome 0 010 0, Italy
b Unit of Radiology, S. Eugenio Hospital, Rome 0 010 0, Italy
Endoscopic retrograde cholangiopancreatography (ERCP) is an invasive procedure with a complication rate ranging from 4% to 10% [1].While post-procedure pancreatitis is the most common risk,bleeding also deserves attention.The most common symptoms of post-procedure bleeding were abdominal pain (91.7%),anemia (43.8%),hypotension (29.2%) and fever (20.8%) [ 2,3 ].
Risk factors for post-procedure bleeding are coagulopathy,liver cirrhosis,renal failure,sphincterotomy and papillectomy [4].Postsphincterotomy bleeding can be differentiated according to the onset (immediate or delayed) or the severity (mild,moderate,severe) while intrahepatic hematoma,most frequently located in the right hepatic lobe,is a rare and potentially life-threatening post-ERCP complication [ 5,6 ].So far,peripheral vasculopathies have not been reported as a concomitant risk factors for severe postprocedure bleeding.Herein,we report a case with peripheral vasculopathies suffering from intraparenchymal hepatic hematoma following ERCP.
An 83-year-old male patient came to our attention presenting abdominal pain,vomiting and fever,without jaundice.In his medical history,a previous cholecystectomy,peripheral vasculopathies and a post-ischemic dilated cardiomyopathy were reported.The laboratory findings showed a total bilirubin of 1.82 mg/dL (direct bilirubin 1.17 mg/dL),raised gamma-glutamyl transpeptidase and procalcitonin levels.Abdominal computed tomography (CT)and magnetic resonance cholangiopancreatography (MRCP) showed a bile duct obstruction with multiple bile duct stones (diameter ranging from 7–9 mm) ( Fig.1 A).
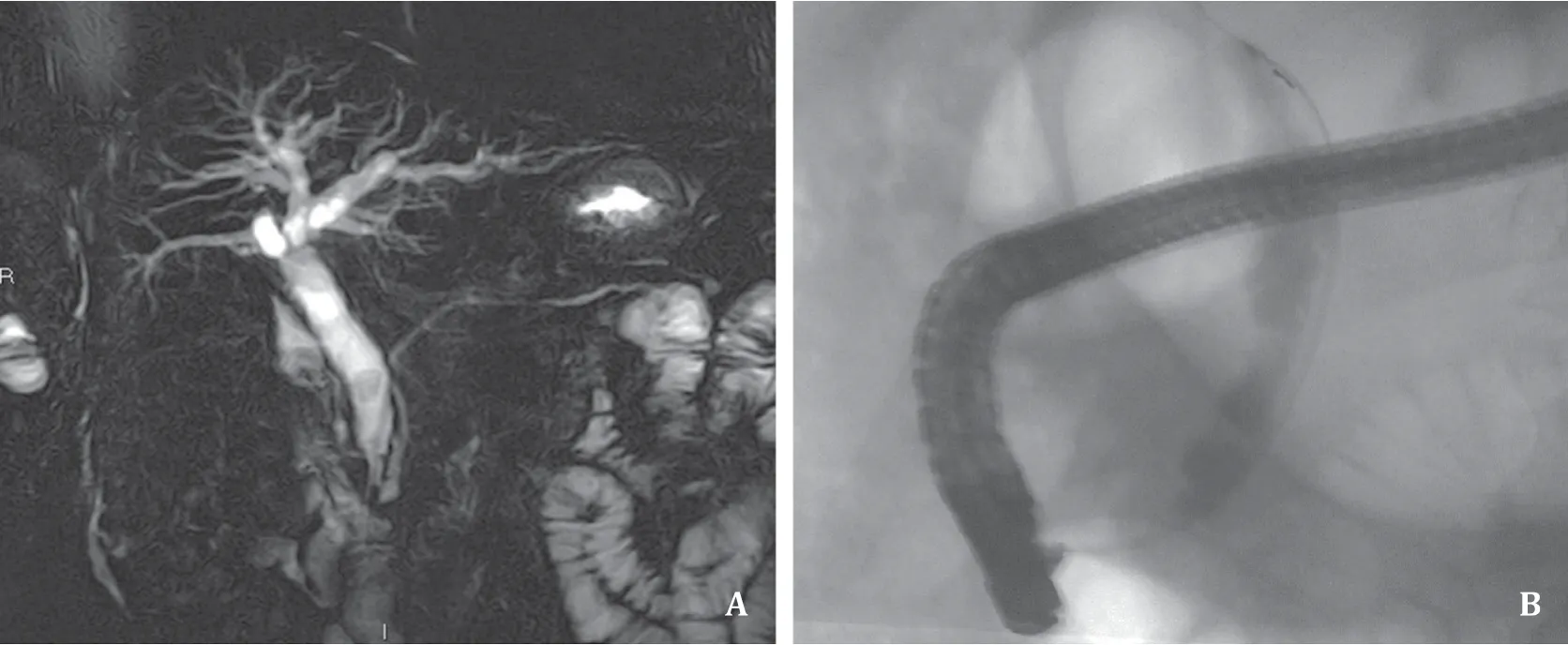
Fig.1.Magnetic resonance cholangiopancreatography ( A ) and endoscopic retrograde cholangiopancreatography ( B ) showing the presence of biliary stones in the medium and distale portion of common bile duct.
In the next few days,after obtaining the patient’s informed consent and an anesthesiologic clearance,an ERCP was successfully performed.During the ERCP,following an easy cannulation of the common bile duct,the presence of multiple stacked stones was confirmed via contrast injection into the duct (mean diameter 9.2 mm) ( Fig.1 B).Based on the stones’ diameter,a sphincterotomy over the 0.0035 inch guidewire was performed.The bile duct was then completely cleared with a Fogarty catheter (ExtractorTMPro XL-Boston Scientific,Voisins-le-Bretonneux,France) over the guidewire.Neither technical difficulties nor complications were experienced during the procedure.Overall,the ERCP duration was 22 minutes.According to the literature by Cappell and Friedel,the examination could be defined as grade 1 in terms of performance difficulty [7].
Late in the afternoon on the same day of the ERCP,the patient experienced an acute abdominal pain on the epigastric abdominal quadrants.CT scan and laboratory tests documented a massive left hepatic hematoma (15 × 9 × 4 cm) ( Fig.2 A),a decrease in hemoglobin levels from the baseline (hemoglobin 8.7 g/dL) and acute elevated transaminase values.Digital subtraction angiogram showed active extravasation of contrast media in the left hepatic lobe ( Fig.2 B).
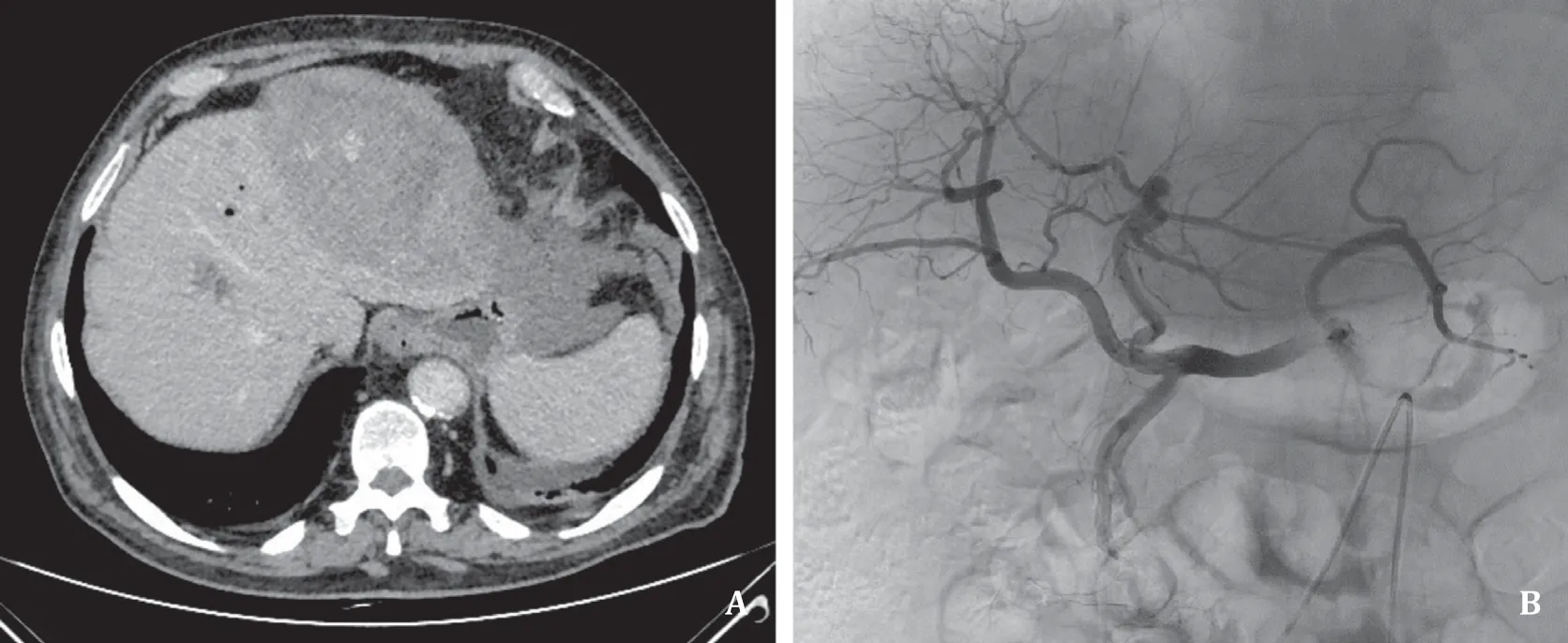
Fig.2.CT scan and digital subtraction angiogram results.A: Axial contrast enhanced CT scan showing large subcapsular and intraparenchymal hematoma of the left hepatic lobe; B: digital subtraction angiogram showing active extravasation of contrast media in the left hepatic lobe.
Antibiotics and fluid supplementation were administered to the patient,obtaining stability of the clinical conditions.A conservative management was chosen.However,as abdominal pain was intensifying,another CT scan was performed,which documented an increase of the intrahepatic bleeding.The patient was submitted to an endovascular embolization of the vascular bleeding site using Contour coils (250–350 micron).The bleeding was resolved,however,an acute necrotic collection occurred at the hepatic bleeding site ( Fig.3 ).

Fig.3.Digital subtraction angiogram and CT scans after embolization.A: Digital subtraction angiogram showing successful exclusion of the hemorrhage; B: axial contrast enhanced CT scan showing a large hematoma associated with hepatic necrosis and bile leaks in the left hepatic lobe.
Further to a multidisciplinary consultation with the surgeon and the interventional radiologist,considering the general critical condition of the patient,a CT-guided percutaneous drainage of the left hepatic lobe collection was planned and successfully performed ( Fig.4 A).The patient was discharged 15 days later,carrying out a 14F drainage catheter for the hepatic remnant fluid collection.In the following 3 months,a follow-up was planned to remove the drainage and perform another CT scan ( Fig.4 B).
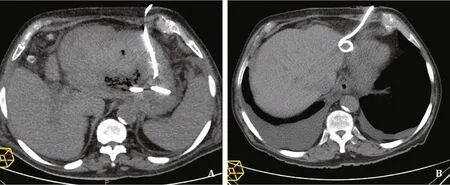
Fig.4.CT scans during percutaneous drainage and after 3 months.A: CT-guided percutaneous drainage of the left hepatic lobe collection with 14F pigtail catheter.B: CT scan after 3 months (checking up on a weekly basis) showing complete resolution of the remarkable improving of necrotic collection.
The literature review found few,probably underestimated cases of post-ERCP hepatic hematoma.The majority of the reported post-ERCP hepatic hematoma is subcapsular,differing from the present case.
The exact pathological mechanism of post-ERCP hepatic hematoma is still unclear.However,the accidental puncture of peripheral vessels by the endoscopic guide wire may explain the phenomenon [ 5,6,8 ].It has also been postulated that the hepatic damage may be secondary to the traction exerted by the balloon inside the common bile duct during the procedure,in an attempt to remove the stones.This force may cause bile ducts or vessels rupture,resulting in hepatic bleeding [3].This explanation could likely apply to our patient,suffering from vasculopathies.Some authors postulated that in case of anomalies of the biliary tree,the incidence of this complication could be higher than suspected,although this opinion is not supported by published evidence [2].
The symptoms and signs of post-ERCP hepatic hematoma (sudden abdominal pain,hypotension,post-ERCP tachycardia),may appear early or have a late onset (time range reported between 4–48 h),resulting in higher mortality.The sudden hematoma rupture with hemoperitoneum is a high-risk complication of post-ERCP hepatic hematoma,with high mortality if misdiagnosed.CT scan and ultrasound,not laboratory tests (albeit necessary),are the gold standard for the post-ERCP hepatic hematoma diagnosis.Different treatment approaches are proposed in literature,based on the patient hemodynamic and clinical conditions [9].In a stable patient with a peripheral hematoma,a conservative management (fluid supplementation and prophylactic antibiotics administration) should be considered.Whenever hemodynamic instability with concomitant extravasation of contrast is reported,an immediate radiological or surgical approach is required.
In the present case,the symptoms started a few hours after the procedure; the patient had clinical instability and the first approach was radiological via vessel embolization.A hepatic drainage was further required after the resolution of the bleeding.The patient was discharged a few days later.
In conclusion,hepatic hematoma is a rare and probably underestimated post-ERCP complication,deserving our full attention.Generally,a conservative approach can be adopted for post-ERCP hepatic hematoma,especially in stable patients.Surgical intervention is associated with high mortality risk and is suggested in case of peritoneusm.Serial follow-up CT scans are mandatory to monitor the hematoma dimensions.A special effort is needed to identify intraprocedural-related or patient-related risk factors for this life-threatening complication.
Acknowledgments
None.
CRediTauthorshipcontributionstatement
ValeriaD’Ovidio:Writing - original draft,Writing - review &editing.GiovanniBruno:Methodology,Writing - original draft,Writing - review & editing.GiulioSodani:Methodology,Writing - original draft,Writing - review & editing.CristinaLucidi:Methodology,Writing - original draft,Writing - review & editing.MarcoEmilioBazuro:Methodology,Writing - original draft,Writing - review & editing.
Funding
None.
Ethicalapproval
Written informed consent was obtained from the patient.
Competinginterest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Cross-talk between hepatic stellate cells and T lymphocytes in liver fibrosis
- Diabetes mellitus is a risk factor of acute kidney injury in liver transplantation patients✩
- Hepatobiliary&Pancreatic Diseases International
- Application of machine learning models for predicting acute kidney injury following donation after cardiac death liver transplantation
- Postoperative adjuvant transcatheter arterial chemoembolization improves the prognosis of patients with huge hepatocellular carcinoma
- The effects of stereotactic body radiotherapy on peripheral natural killer and CD3 + CD56 + NKT-like cells in patients with hepatocellular carcinoma
