Diabetes mellitus is a risk factor of acute kidney injury in liver transplantation patients✩
2021-07-24YuJiWngJinHuLiYiGunQiongHongXieChunMingHoZhengXinWng
Yu-Ji Wng ,#,Jin-Hu Li ,#,Yi Gun ,#,Qiong-Hong Xie ,Chun-Ming Ho ,Zheng-Xin Wng ,
a Division of Nephrology, Huashan Hospital, Fudan University, Shanghai 200040, China
b Division of General Surgery, Huashan Hospital, Fudan University, Shanghai 200040, China
Keywords:Acute kidney injury Liver transplantation Diabetes Renal function
ABSTRACT Background:Diabetes mellitus has become an increasing global health burden with rapid growing prevalence.Patients with diabetes have higher susceptibility to acute kidney injury (AKI).Liver transplantation(LT) predisposes the kidney to injury.However,the association between diabetes and AKI in LT patients remains unclear.Methods:We conducted a retrospective cohort study examining risk factors for AKI in patients undergone orthotopic LT.Potential risk factors including baseline estimated glomerular filtration rate (eGFR),the model for end-stage liver disease (MELD) score,diabetes,hypertension and intraoperative blood loss were screened.The primary endpoint was AKI occurrence.Multivariate logistic regression was used to analyze the association between potential risk factors and AKI.Results:A total of 291 patients undergone orthotopic LT were included in the present study.Among them,102 patients (35.05%) developed AKI within 5 days after LT.Diabetes was identified as an independent risk factor for AKI.Patients who developed AKI had worse graft function recovery and higher mortality within 14 days after LT compared to those who did not develop AKI.AKI patients with diabetes had a significant decline of eGFR within the first postoperative year,compared with patients who did not develop AKI and who developed AKI but without diabetes.Conclusions:Diabetes is an independent risk factor for AKI after orthotopic LT.AKI is associated with delayed graft function recovery and higher mortality in short-term postoperative period.Diabetic patients who developed AKI after LT experience a faster decline of eGFR within the first year after surgery.
Introduction
Liver transplantation (LT) is a lifesaving therapy for patients with end-stage liver diseases.A steady growth in number of LT cases has been reported in the USA,with an increase of 24% over a decade [1].Acute kidney injury (AKI) is a common postoperative complication after LT with an incidence exceeding 50% [2–4].AKI after LT,even if transient,has been associated with higher mortality rate,poor long-term survival and worse graft outcomes [5].The risk factors of AKI in LT patients have been analyzed [6],and reduced renal function [7]and more advanced stage of liver diseases [8]have been identified to be associated with AKI after the surgery.Understanding the risk factors for AKI is important to develop preventive strategies and improve outcomes of the patients.
Diabetes has become an increasing global health burden.According to the International Diabetes Federation (IDF) calculations,an estimated 8.8% of the global population have diabetes and the number will climb to 10.4% by 2040 [9].Diabetes will not only lead to diabetic nephropathy but also may increase the susceptibility of the kidney to damage.It has been documented that diabetes is an independent risk factor of AKI following cardiac surgery [10–12].In the present study,we examined the incidence of AKI in LT patients and analyzed the risk factors for AKI.
Methods
Study subjects
This is a retrospective study conducted from December 2016 to December 2019 in Division of General Surgery,Huashan Hospital,Fudan University.The study was approved by the Ethics Committee of Huashan Hospital,Fudan University.All the donor livers were sourced from donation after circulatory death (DCD) in an ethical manner and matched by the China Organ Transplant Response System (COTRS).Adult patients aged ≥18 years who have undergone orthotopic LT were screened for enrollment.Exclusion criteria included chronic kidney disease (CKD) stage 3–5,AKI developed before the surgery,combined liver-kidney transplantation,second LT,and incomplete clinical information.
Clinical data
The data were collected from outpatient and inpatient medical records.Baseline characteristics included age,sex,body mass index (BMI),the model for end-stage liver disease (MELD) score,hemoglobin A1c (HbA1c),hemoglobin (Hb),white blood cell(WBC),neutrophil percentage (N%),platelet count (PLT),alanine aminotransferase (ALT),aspartate aminotransferase (AST),total bilirubin (TB),albumin,blood ammonia,total cholesterol,triglycerides,low density lipoprotein (LDL),high density lipoprotein(HDL),prothrombin time (PT),international normalized ratio (INR),pro-brain natriuretic peptide (pro-BNP),blood urea nitrogen (BUN)and serum creatinine (SCr).Estimated glomerular filtration rate(eGFR) was calculated based on 2009 CKD-EPI equation [13].SCr of five consecuti ve day after LT were recorded to determine the development of AKI.Graft function and patients’ survival at day 14 after LT were recorded.SCr levels within the first postoperative year were obtained from outpatient records.Operative-associated parameters included intraoperative blood loss,warm and cold ischemic time.Warm ischemic time was defined as the time starting from the withdrawal of life support when donor systolic blood pressure dropped below 50 mmHg or the SaO 2 dropped below 70%until theinsituaortic cold perfusion.Cold ischemic time was defined as time from cross-clamp of the aorta and cold flush in the donor to the time of the first anastomosis in the recipient.Indications for orthotopic LT and comorbidities including diabetes and hypertension were also recorded.
Diabetes mellitus was diagnosed based on medical history or HbA1c ≥6.5% or order sheets recording diet or drug therapy of di-abetes.SCr within 3 days before LT was recorded as the baseline.The maximum SCr change was calculated by the variance from baseline to the peak value within 5 days after LT.AKI was defined according to Kidney Disease: Improving Global Outcomes (KDIGO)criteria with an increase of SCr by ≥26 mmol/L within 48 h as well as an increase to more than 1.5 times from baseline within 7 days as threshold for diagnosis [14].Severe AKI was defined as stage 2 and stage 3 AKI according to KDIGO criteria.
Statistical analysis
Continuous variables were presented as medians and interquartile range (IQR) and compared with the Mann-WhitneyUtest.Categorical variables were presented as numbers and percentages and compared with the Pearson Chi-square test or Fisher’s exact test.Univariate and multivariate logistic regression analysis were used to determine independent risk factors of AKI and association between levels of HbA1c and AKI.Statistical analyses were performed with SPSS v25.0 (IBM Corp,Armonk,New York,USA).All the statistical tests were 2-sided,and differences were considered significant for aPvalue<0.05.
Results
Patients’ baseline characteristics
A total of 291 orthotopic LT patients with 79.73% male were enrolled.The median (IQR) age of the patients was 51.0 (44.0–58.0)years.Hepatitis B virus (HBV) infection was the predominant etiology,accounted for 71.82% of all patients.Sixty-one patients had diabetes.Diabetic patients were older and more likely to have hypertension,higher BUN and SCr elevation from baseline.In diabetic patients,55.74% of them developed AKI after surgery and 29.51%developed severe AKI (AKI KDIGO stage 2 and 3),which were significantly higher than the percentages in non-diabetic patients(29.57% and 10.00% for AKI and severe AKI,respectively).There were no significant differences in baseline eGFR,serum lipids or other test results between the diabetic and non-diabetic groups( Table 1 ).
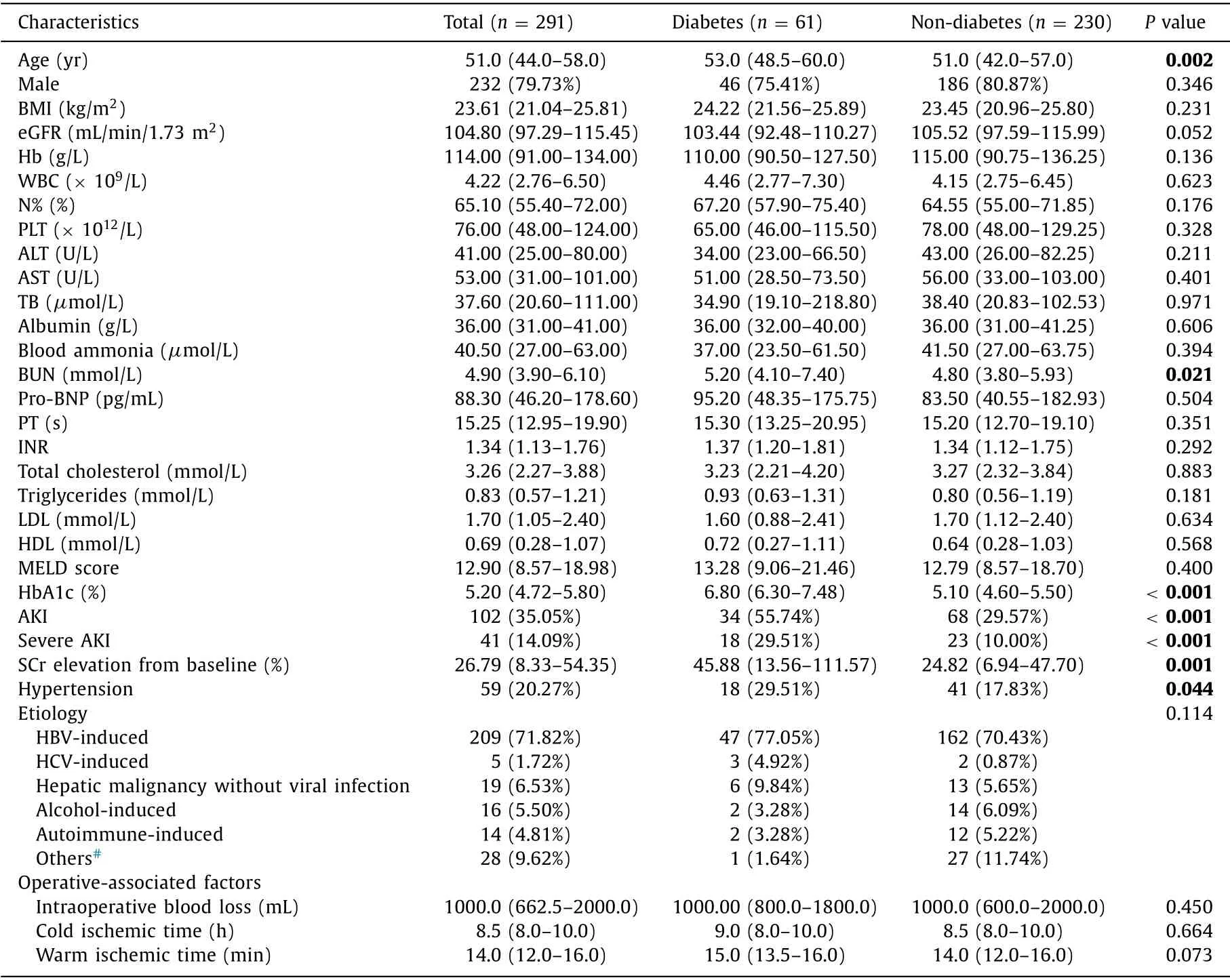
Table 1 Pre- and intra-operative characteristics of patients according to diagnosis of diabetes.
Risk factors of AKI
One hundred and two patients (35.05%) developed AKI within 5 days after LT.None of these patients required postoperative renal replacement treatment (RRT).AKI patients had higher BMI,MELD score and HbA1c,lower baseline eGFR and more intraoperative blood loss compared with those who did not develop AKI.Among AKI patients,33.33% of them had diabetes and 27.45% had hypertension,significantly higher than those in the non-AKI group( Table 2 ).In multivariate logistic regression analysis,potential confounding risk factors were adjusted.Age and sex were adjusted in Model 1; age,sex,hypertension,and MELD score were adjusted in Model 2; and all above plus intraoperative blood loss were further adjusted in Model 3.In all adjusted models,diabetes remained independently associated with incidence of AKI after LT ( Table 3 ).Associations of HbA1c levels with AKI and severe AKI outcomes were presented in Table 4.HbA1c level was categorized into three intervals with cutoff points as 5.5% and 6.5% and analysis suggested an ascending tendency for AKI and severe AKI in patients with higher HbA1c,indicating that poor glycemic control might be associated with increased risk of AKI.
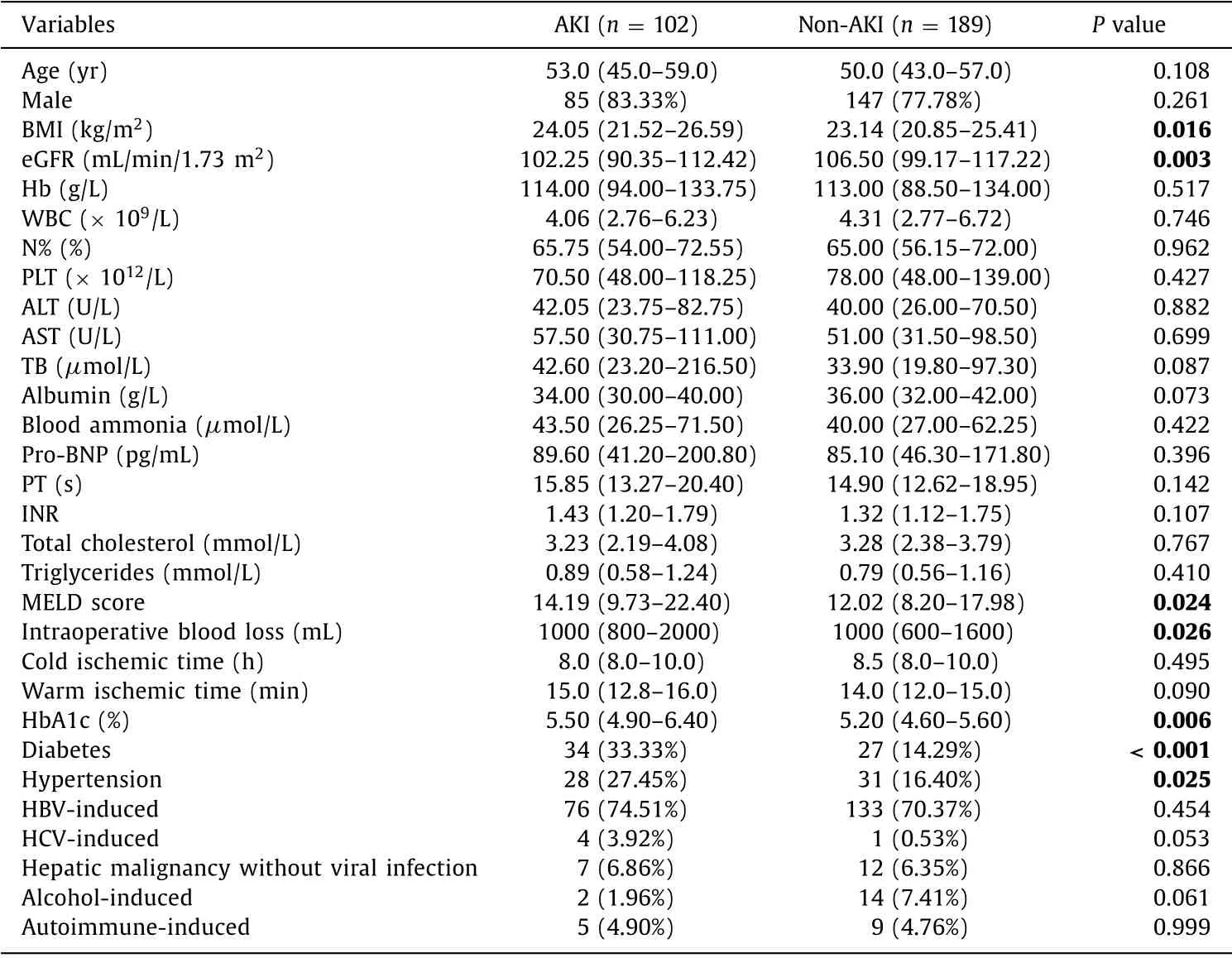
Table 2 Univariate analysis of variables between AKI and non-AKI patients.
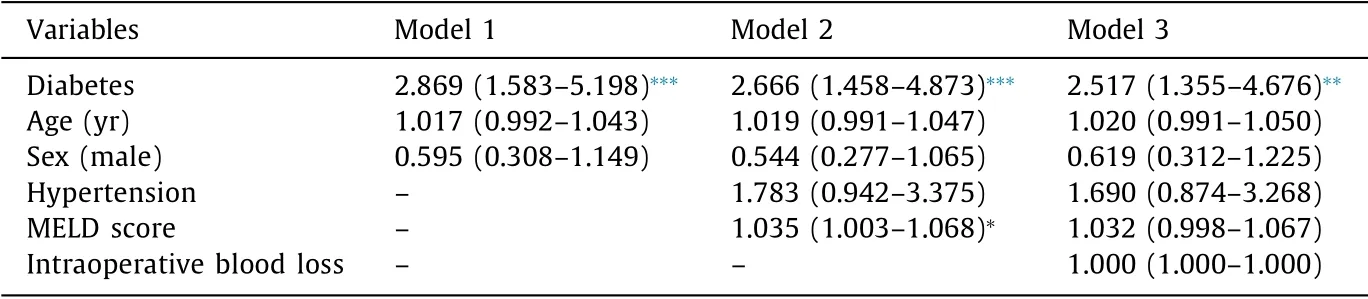
Table 3 Diabetes associates with AKI across stratified analyses.
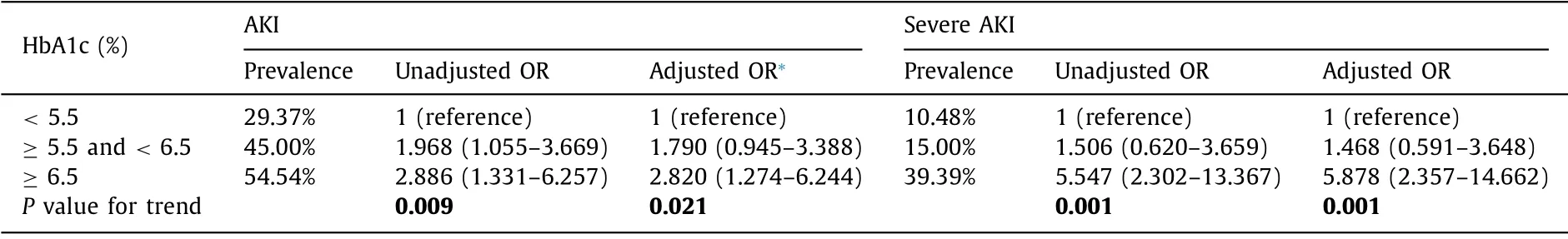
Table 4 Association of HbA1c with AKI and severe AKI outcomes.
The effect of AKI and diabetes on graft function and mortality at postoperative day 14
Compared with patients without AKI,those with AKI had worse graft function at day 14 after surgery,manifested by higher ALT,AST and TB,and lower albumin.Among AKI patients,9.80% of them died within 14 days after LT,significantly higher than that in patients without AKI (1.06%).No differences were observed between the diabetic and non-diabetic subgroups in 14-day graft function and 14-day mortality in neither the AKI nor non-AKI groups ( Table 5 ).

Table 5 Graft function at postoperative day 14 and perioperative death.
The effect of AKI and diabetes on eGFR one-year after operation
A total of 158 patients had follow-up records of renal function within the first postoperative year,and 49 (31.01%) of them had AKI.Thirteen of the AKI patients had diabetes and these patients showed the greatest decline of eGFR within the first postoperative year when compared with those without AKI and those with AKI but without diabetes ( Fig.1 ).The median (IQR) value of eGFR reduction one year after surgery in diabetic patients with AKI was 20.04 ( −0.75 to 37.66) mL/min/1.73 m2,which was significantly greater than those of non-diabetic or non-AKI patients[5.23 ( −2.59–16.98) mL/min/1.73 m2].Three (23.08%) out of the thirteen patients with diabetes and AKI had eGFR lower than 60 mL/min/1.73 m2one year after surgery ( Table 6 ).

Fig.1.eGFR decline trend within postoperative one-year period.eGFR: estimated glomerular filtration rate.
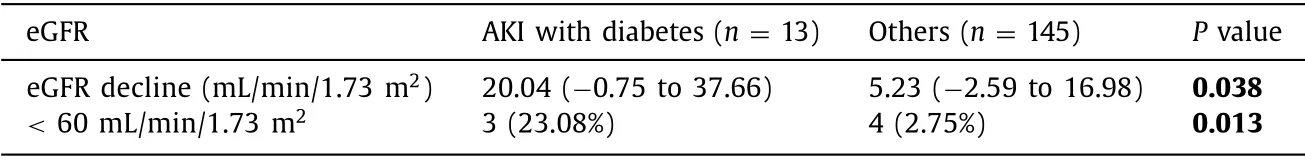
Table 6 eGFR decline from baseline one year after liver transplantation.
Discussion
Among the 291 orthotopic LT patients,102 (35.05%) developed AKI.More than half of diabetic patients developed postoperative AKI while less than 30% of patients without diabetes developed AKI.The rate of severe AKI was 29.51% in diabetic patients,nearly 3 folds higher than that in patients without diabetes.AKI was associated with poor graft function and high mortality during the first two-week postoperative period.Diabetic patients with AKI had a greater renal function decline at one year after surgery.
AKI is a common and important complication with a poor prognosis.Mortality of patients with AKI remains high,especially in critically ill patients,which reaches more than 50% [15].The present study found that the incidence of AKI after LT was 35% and that occurrence of AKI was associated with poorer graft function and higher mortality.AKI is suspected to cause microvascular organ ischemia and subsequent delayed graft function recovery [16].Additionally,AKI could be a result of poor general condition leading to multiorgan failure.Multiple studies have shown the association of AKI and subsequent chronic kidney disease (CKD) [17].In the present study,we observed that the diabetic patients who developed AKI after surgery had the greatest eGFR decline at one year after the surgery.Incomplete recovery from AKI can lead to chronic functional deficits that may lead to progressive renal function decline,especially in patients with preexisting renal lesions [18].Poorly healed renal tubules have been reported to cause disproportionately scarring with loss of peritubular capillaries,leading to volume–dependent salt–sensitive hypertension and subsequent glomerular damage [19].Diabetic patients even with seemingly normal renal function have ultrastructural changes in kidney and malfunctional renal hemodynamics,reducing the ability to repair from injury [20].Other studies demonstrated that AKI episodes were associated with a cumulative risk for developing advanced CKD in diabetic patients [21]and that pre-existing di-abetes was an independent risk factor for development of stage 3 or higher CKD after AKI [22].
Although sepsis is a major cause of hospital acquired AKI,iatrogenic factors are increasingly associated with AKI development in hospital,including surgeries,nephrotoxic drugs and so on.In our study,35.05% of patients developed AKI after LT.In the present study,diabetes is an independent risk factor on posttransplant AKI after adjusted by other confounding risk factors.The mechanism by which diabetes increases the risk of LT-associated AKI is incompletely understood.Vascular endothelium is an important target for diabetic injury and kidney is one of the most important organs involved in diabetic microangiopathy [23].Approximately 40% of patients with type 2 diabetes develop diabetic kidney disease [24],a type of disease that is well-defined with characteristic clinical and pathological manifestations.CKD is recognized as an important risk factor for AKI [25].Undoubtedly,patients with diabetes and CKD have a higher risk of AKI.In terms of patients with CKD,low eGFR and albuminuria are highly correlated with AKI [26].eGFR of 60 mL/min/1.73 m2is often considered the turning point of the AKI risk [27].In the current work,we enrolled patients with baseline eGFR ≥60 mL/min/1.73 m2.The incidence of AKI was still as high as 35.05%,and 55.7% of diabetic patients developed AKI.The present study suggested that diabetic patients are predisposed to AKI under the condition of acute stress such as major surgery.The biologic basis for this increased susceptibility to AKI in diabetic patients is incompletely understood.Nicotinamide adenine dinucleotide (NAD+) has been reported to reduce in diabetes [28]and Sirt1,an NAD+-dependent protein deacetylase was down regulated in diabetic kidney [29].NAD+and Sirt1 play protective role in cellular response to stress and the decreased level of NAD+and Sirt1 may lead to inadequate response to injury stress.Additionally,other mechanisms including oxidative stress injury,mitochondrial cleavage,changes in the autophagy response,upregulation of pro-inflammatory factors,and changes in DNA methylation have been also reported to increase AKI susceptibility in diabetic patients [17].
We found that hepatitis B virus infection was the leading indication for LT in our cohort,which was consistent with reports by the China Liver Transplant Registry [30].None of the indications recorded in the present study including hepatitis B virus infection,hepatitis C virus infection,alcoholic liver disease,autoimmune hepatitis,hepatic malignancy without viral infection and others were identified as a risk factor for AKI.We noted that none of the patients in the cohort were diagnosed as nonalcoholic fatty liver disease (NAFLD) and its subtype,non-alcoholic steatohepatitis(NASH),which were found to be more likely to be associated with post-LT AKI than other LT indications in Western countries [2].The prevalence of NAFLD has been reported to increase dramatically in recent years [31]and the increasing prevalence of NAFLD,along with type 2 diabetes,obesity and other metabolic syndrome is a result of rapid urbanization in China.However,the time-taking process in which NAFLD develops into cirrhosis and end-stage disease could be an explanation for the absence of this disease in the present LT cohort.
The present study showed that higher MELD score was associated with AKI after LT,which was consistent with other studies [ 8,32 ].MELD was created to predict survival in patients with varying levels of liver disease severity,with its major use in allocation of organs for LT [33].Three widely available laboratory variables including INR,SCr,and TB were incorporated in MELD score.We noted a relatively low median MELD score in the present study due to exclusion of patients with severe preoperative renal dysfunction and small portion of acute or subacute liver failure patients with high MELD score.In our study,worse baseline kidney function contributed most to the higher MELD score in AKI patients.Kidney function impairment in patients with advanced liverdisease is common,presented as hepatorenal syndrome,the incidence of which is reported as high as 40% [34–36].Hemodynamic factor is an important pathophysiology of kidney injury in liver cirrhosis.Splanchnic vasodilation caused by increased shear stress in the portal vessels results in a reduction in the effective circulatory volume.This was followed by activation of the sympathetic nervous system and the renin-angiotensin system,which induces profound renal vasoconstriction and reductions in renal blood flow [37].Although none of patients in this study presented as hepatorenal syndrome,patients with lower eGFR may have underlying kidney function impairment due to portal hypertension.
There were several limitations in the current study.First,AKI was diagnosed through reviewing SCr changes in electronic charts,which may have bias.In addition,over half of the diabetes mellitus diagnosis was based on HbA1c test,which was impossible to analyze the severity of diabetes by hypoglycemic therapy.Second,the risk factors analyzed in this study were limited.Operativeassociated parameters such as reperfusion syndrome and anhepatic phase and medications including nonsteroidal antiinflammatory drugs,antibiotics and immunosuppressive agents were not analyzed.
In conclusion,diabetes is an independent risk factor for AKI after orthotopic LT.AKI is associated with delayed graft function recovery and higher mortality during short postoperative period.AKI and diabetes have a combined effect on eGFR decline within the first postoperative year.We need to pay attention to patients with diabetes in AKI prevention and management before and after LT.
Acknowledgments
None.
CRediTauthorshipcontributionstatement
Yu-JiaWang:Data curation,Formal analysis,Writing - original draft.Jian-HuaLi:Methodology,Writing - original draft.Yi Guan:Funding acquisition,Methodology,Writing - original draft.Qiong-HongXie:Methodology.Chuan-MingHao:Funding acquisition,Writing - review & editing.Zheng-XinWang:Conceptualization,Supervision,Writing - review & editing.
Funding
This study was supported by grants from the National Natural Science Foundation of China (81700591,81520108006,and 81930120).
Ethicalapproval
The study was approved by the Ethics Committee of Huashan Hospital,Fudan University.
Competinginterest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Cross-talk between hepatic stellate cells and T lymphocytes in liver fibrosis
- Hepatobiliary&Pancreatic Diseases International
- Application of machine learning models for predicting acute kidney injury following donation after cardiac death liver transplantation
- Postoperative adjuvant transcatheter arterial chemoembolization improves the prognosis of patients with huge hepatocellular carcinoma
- The effects of stereotactic body radiotherapy on peripheral natural killer and CD3 + CD56 + NKT-like cells in patients with hepatocellular carcinoma
- ATP-citrate lyase regulates stemness and metastasis in hepatocellular carcinoma via the Wnt/ β-catenin signaling pathway
