Extra-anatomic aortic bypass for the treatment of a mycotic pseudoaneurysm after liver transplantation for hilar cholangiocarcinoma
2021-07-24LurLldoElenIorrEmilioRmosNuriAlCheroJonFregt
Lur Lldo ,,Elen Iorr ,Emilio Rmos ,Nuri Sé,Al Chero ,Jon Fregt
a Liver Transplant Unit, Hospital Universitari Bellvitge, University of Barcelona, Barcelona, Spain
b Vascular Surgery Department, Hospital Universitari Bellvitge, University of Barcelona, Barcelona, Spain
c Infectious Disease Department, Hospital Universitari Bellvitge, University of Barcelona, Barcelona, Spain
Liver transplantation (LT) after neoadjuvant chemoradiotherapy in patients with unresectable hilar cholangiocarcinoma (HC) is an accepted treatment strategy [1].Neoadjuvant therapy is associated with an increased risk of arterial and portal complications after LT [ 1,2 ].In most cases,radiation therapy makes the use of the native hepatic artery inadvisable,and an aortic anastomosis is needed,either with or without a graft [2].
The development of a mycotic pseudoaneurysm after LT is a rare complication that is associated with a high incidence of graft failure and mortality.Radiotherapy,local infections and the use of grafts are known risk factors for the development of a mycotic pseudoaneurysm,which is always challenging to manage [3].
Herein,we reported a case diagnosed with a mycotic pseudoaneurysm in the donor celiac trunk at the site of the supraceliac aortic anastomosis,resolved by an extra-anatomic bypass.The patient gave signed informed consent for the publication.
A 47-year-old man diagnosed with an unresectable Bismuth type IV HC was evaluated for LT.After percutaneous biliary drainage,a biliary stent was inserted in February 2017.After this drainage,he had severe acute pancreatitis,complicated by a colopancreatic fistula.He recovered successfully with medical treatment and drainage,before undergoing radiotherapy (SBRT,50 Gy) and chemotherapy (5-fluorouracil) until July 2017.Then he had 4 episodes of cholangitis,the last one in December 2017,and a liver abscess.Biliary drainage was optimized and hepatic abscess was drained.Bile culture showed colonization by beta-lactamase OCA-49 positiveKlebsiellapneumoniae.Due to multiple episodes of infections,he was not able to continue with chemotherapy.One year after the initial diagnosis,the infection was controlled,and there was no tumor progression.Finally,LT was performed in January 2018,using the piggy-back technique.An arterial anastomosis was performed directly between the donor celiac trunk and the supraceliac aorta,without the need for a graft.We preferred to perform a supraceliac aortic anastomosis because the use of a graft was unnecessary in most cases,and it was associated with a lower incidence of hepatic artery thrombosis and renal insuffi-ciency [4].Arterial flow was 670 mL/min.Postoperative evolution was uneventful,and the patient was discharged with good graft function on postoperative day (POD) 8.Pathological study of the liver confirmed moderately differentiated adenocarcinoma,pT2N1,with perineural invasion and focal portal vein invasion.There was no margin invasion and therefore resection was considered R0.
Two months after LT,a mycotic pseudoaneurysm at the arterial anastomosis to the aorta and portal vein stenosis was observed on a routine CT scan ( Fig.1 A,B).The patient had no pain,fever or any sign of bleeding.He was hemodynamically stable,but an arterial leakage was observed on the CT scan.After initial empiric treatment with antibiotics (ceftazidime-avibactam) and an antifungal agent (anidulafungin),the first approach was to percutaneously place a portal vein stent (MedtronicR○ 12 × 40 mm,Plymouth,Minnesota,USA) to ensure graft perfusion ( Fig.1 C).Afterwards,on the same day,an endovascular covered stent (Aortic BegraftR○20 × 48 mm,Bentley,Inchinhan,Scotland) was placed in the aorta covering the celiac anastomosis ( Fig.1 D).The stent extended from 14 mm above the pseudoaneurysm (proximally) to 10 mm above the superior mesenteric artery (distally),and had the same size as that of the aorta (20 mm).Initially,we did not consider embolizing the celiac trunk,as we thought that the covered stent would resolve an aortic leak,and the celiac trunk could be preserved.However,probably due to the mycotic infection,the stent failed.Despite the initial good arteriographic results,the CT scan performed 48 h later showed persistent leakage (type 1 endoleak).

Fig.1.Diagnosis and endovascular treatment.A: A computed tomography scan showing the mycotic pseudoaneurysm; B: a computed tomography scan showing the portal vein stenosis; C: portal vein stent (12 × 40 mm) placement; D: an aortic endovascular-covered stent (20 × 48 mm) was placed covering the pseudoaneurysm.SMA: superior mesenteric artery.
The patient was clinically stable,but due to the high risk of rupture,we decided to perform open surgery.
With the intention of performing an anastomosis on healthy aorta,a left thoraco-phreno-laparotomy was performed.The supraceliac and infrarenal aorta were exposed,and the left renal artery was identified and controlled.The superior mesenteric artery and celiac trunk were surrounded by fibrous tissue,making dissection impossible.Renal arteries and the superior mesenteric artery were preserved.After lateral clamping of the infrarenal aorta,a rifampicin-soaked Dacron prosthetic graft (Gelsoft®,Vascutek/Terumo,Inchinhan,Scotland) was prepared by soaking the Dacron graft in 60 mg/mL of rifampicin solution for 30–60 min.The prosthetic graft was laterally anastomosed to the infrarenal aorta.The distal anastomosis was performed first to minimize medullar and visceral ischemia.The supraceliac aorta was then dissected and ligated.A proximal anastomosis was performed end-toend on distal healthy thoracic aorta,proximal to the previous hepatic anastomosis,with an aortic clamping of 13 min ( Fig.2 ).During the aortic clamping,the pseudoaneurysm was opened,and this aortic segment containing the covered stent was resected and cultured.The donor celiac artery ostium was identified and sutured because it was included in the aortic pseudoaneurysm ( Fig.2 ).The decision to exclude the arterial supply to the liver was made through necessity.It was included in the mycotic pseudoaneurysm,and to debride and resect this aortic segment,we had to suture the donor celiac ostium.The phrenotomy was closed,leaving the bypass in the lateral position,away from the infection site.The operation lasted 300 min,and 5 units of red blood cells were required.
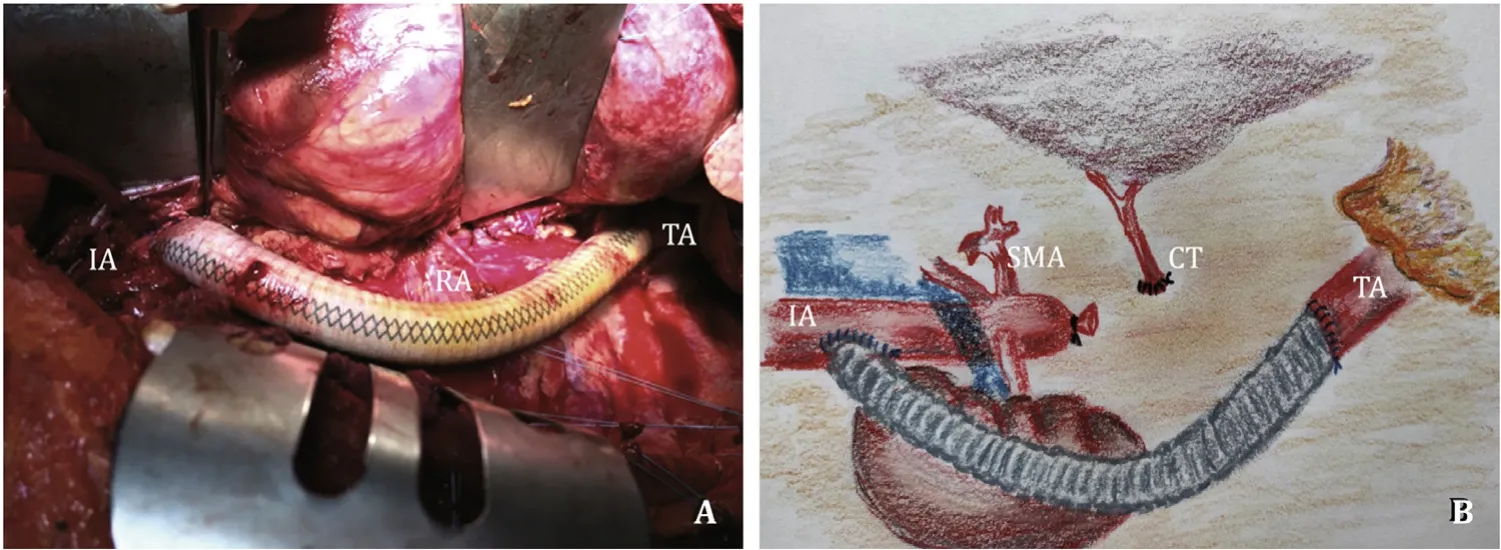
Fig.2.Surgical procedure.The prosthetic graft was laterally anastomosed to the infrarenal aorta and proximally anastomosed end-to-end to distal healthy thoracic aorta proximal to the hepatic anastomosis.A: Surgical view; B: surgical scheme.IA: infrarenal aorta; RA: resected aorta with a pseudoaneurysm; TA: thoracic aorta; SMA: superior mesenteric artery; CT: celiac trunk.
Postoperative evolution was uneventful,with normal hepatic and renal function.No medullar damage was observed.The pseudoaneurysm culture confirmedCandidainfection that was sensitive to fluconazole treatment.Fluconazole treatment was maintained for 12 months until normalization of uptake on18F-fluoro-deoxyglucose positron emission tomography (FDG-PET).The maximum standardized uptake value (SUVmax) on FDG-PET was 6.2 at one month after surgery,and 4.6 at the end of treatment.Currently,18 months after the procedure,the patient is alive without complications and has normal hepatic function.A control CT scan has shown permeability of the prosthesis.Antiaggregation therapy was indicated due to the use of a prosthetic graft.Although a portal vein stent was used,we decided not to use anticoagulants,only maintaining antiaggregation therapy indefinitely.
Vascular complication after LT is a significant cause of morbidity and mortality.Risk factors for the development of mycotic pseudoaneurysms include previous bacterial colonization,technical difficulties in performing an arterial anastomosis,the use of vascular conduits,reconstruction with a bilio-enteric anastomosis and postoperative bile leaks [3].Management of mycotic pseudoaneurysms after LT is always challenging.The use of endovascular stent grafts for the exclusion of the aortic aneurysm is now standard procedure,with low morbidity and mortality [ 5,6 ].However,when interventional techniques fail,surgical revascularization is indicated.
The initial interventional techniques were attempted in this case.A portal vein stent was placed successfully to ensure hepatic vascularization,in case we had to sacrifice arterial inflow.After failure of the aortic stent,we undertook surgical management.A report describedinsituprosthetic graft repair [7]; however,due to the history of previous radiotherapy,severe pancreatitis and LT,we decided against performing surgery through an anterior laparotomy and resolving the hepatic artery pseudoaneurysm(HAP) with aninsituprosthesis.Instead,we performed an extraanatomic prosthetic bypass in the retroperitoneum,as reported previously [8].To the best of our knowledge,this is the first case of an extra-anatomic bypass being performed in the setting of LT.Placement of the prosthesis far from the previous surgical site allows easier access and may reduce the risk of prosthesis infections.This retroperitoneal bypass is in fact an extra-anatomic bypass,because it avoids the infected aortic site.Indeed,we chose this type of bypass because it can preserve renal perfusion and superior mesenteric artery perfusion,better than other types of extraanatomic bypass (such as an axillo-bifemoral bypass).Additionally,with this access,we could debride the pseudoaneurysm and suture the supraceliac aorta to ensure that there was no progression of infection or bleeding.
As suggested by recent studies,FDG-PET was used to assess infection of the graft [9].Treatment was discontinued upon normalization of FDG-PET results.
Our patient had several risk factors for HAP development (e.g.,bilioenteric anastomosis,antibiotic treatments,technical difficulty in performing an arterial anastomosis,and bile colonization).As previously suggested,patients at risk of developing HAP should be initially followed up with CT scans [10].Confirmation of a stable situation allowed a staged endovascular and open repair of the HAP to be performed successfully.
Although we were afraid of excluding the arterial supply to the liver due to the risk of graft dysfunction and ischemic cholangitis,we had no other option.However,arterial ligation or thrombosis does not necessarily result in these consequences,especially when they occur a long time after LT.We were not highly confident in this case because we performed this procedure only two months after LT.Luckily,the patient had no complications and is currently alive with normal liver function.He shows no clinical or radiological signs of ischemic cholangitis.Similar results were reported by Volpin et al.[10],who performed hepatic artery ligation or occlusion in their series of 3 patients,all showing long-term survival and normal liver function.
We consider that this case shows the importance of combining different techniques to manage this type of urgent situations.Firstly,the possibility to assure hepatic vascularization with endovascular portal stent,combined with endovascular aortic stent to stabilize the patient.The development of this new endovascular technique is crucial to improve the results of different type of aortic aneurysms in different settings [ 7,8 ].
Secondly,lessons learned from the use of anatomic versus extra-anatomic bypass in different vascular scenarios can be applied to new situations like our case,after LT.Other cases of aneurysms in the field of radiotherapy,or infection may consider the use similar extra-anatomic bypass.
Indeed,the availability of different type of grafts,with different sizes,and with the possibility to treat with antibiotics,can allow us to fit treatment to each patient.
In conclusion,the use of an extra-anatomic aortic bypass is a new option for the management of patients with a mycotic pseudoaneurysm.This access avoids the previous surgical site affected by radiotherapy and infections.
Acknowledgments
We thank Michael Maudsley from the Language Services at the University of Barcelona for reviewing the English language of the manuscript.
CRediTauthorshipcontributionstatement
LauraLlado:Conceptualization,Writing - original draft,Writing - review & editing.ElenaIborra:Data curation,Writing - review & editing.EmilioRamos:Data curation,Supervision,Writing- review & editing.NuriaSabé:Data curation,Writing - review &editing.AlbaCachero:Data curation,Writing - review & editing.JoanFabregat:Conceptualization,Supervision,Writing - review &editing.
Funding
None.
Ethicalapproval
Permission to use images was obtained from the patient.
Competinginterest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Cross-talk between hepatic stellate cells and T lymphocytes in liver fibrosis
- Diabetes mellitus is a risk factor of acute kidney injury in liver transplantation patients✩
- Hepatobiliary&Pancreatic Diseases International
- Application of machine learning models for predicting acute kidney injury following donation after cardiac death liver transplantation
- Postoperative adjuvant transcatheter arterial chemoembolization improves the prognosis of patients with huge hepatocellular carcinoma
- The effects of stereotactic body radiotherapy on peripheral natural killer and CD3 + CD56 + NKT-like cells in patients with hepatocellular carcinoma
