Analysis of risk factors for lymphedema of the lower limbs after endometrial cancer surgery and suggestions for prevention and treatment
2021-06-29
ABSTRACT
Keywords: Endometrial cancer, lower extremity, lymphedema, prevention and treatment, risk factors is one of the risk factors. However, there are few reports on such related studies in China. In order to better understand the
INRODUCTION
Endometrial cancer is a group of epithelial malignant tumors that occur in the female endometrium and has the second highest incidence of malignant tumors in women,[1]and according to statistics, the number of deaths from endometrial cancer is about 10,000/year in the world.[2]Up to one quarter of patients with endometrial cancer will have lower limb lymphedema after treatment.[3]Lower limb lymphedema is caused by obstruction of lymphatic flow, resulting in swelling, pain, and other pathological changes in the limbs,which affects the patient’s daily life, activities, and quality of life.[4-6]Multiple studies[7,8]have shown that multiple factors are associated with lower limb lymphedema of endometrial cancer, but the conclusions are not consistent, such as about whether the number of lymph nodes removed during surgeryoccurrence of lower limb lymphedema in endometrial cancer patients after surgery, we analyzed the factors associated with lower limb lymphedema in endometrial cancer patients and makes suggestions for the prevention and treatment of postoperative lower limb lymphedema.
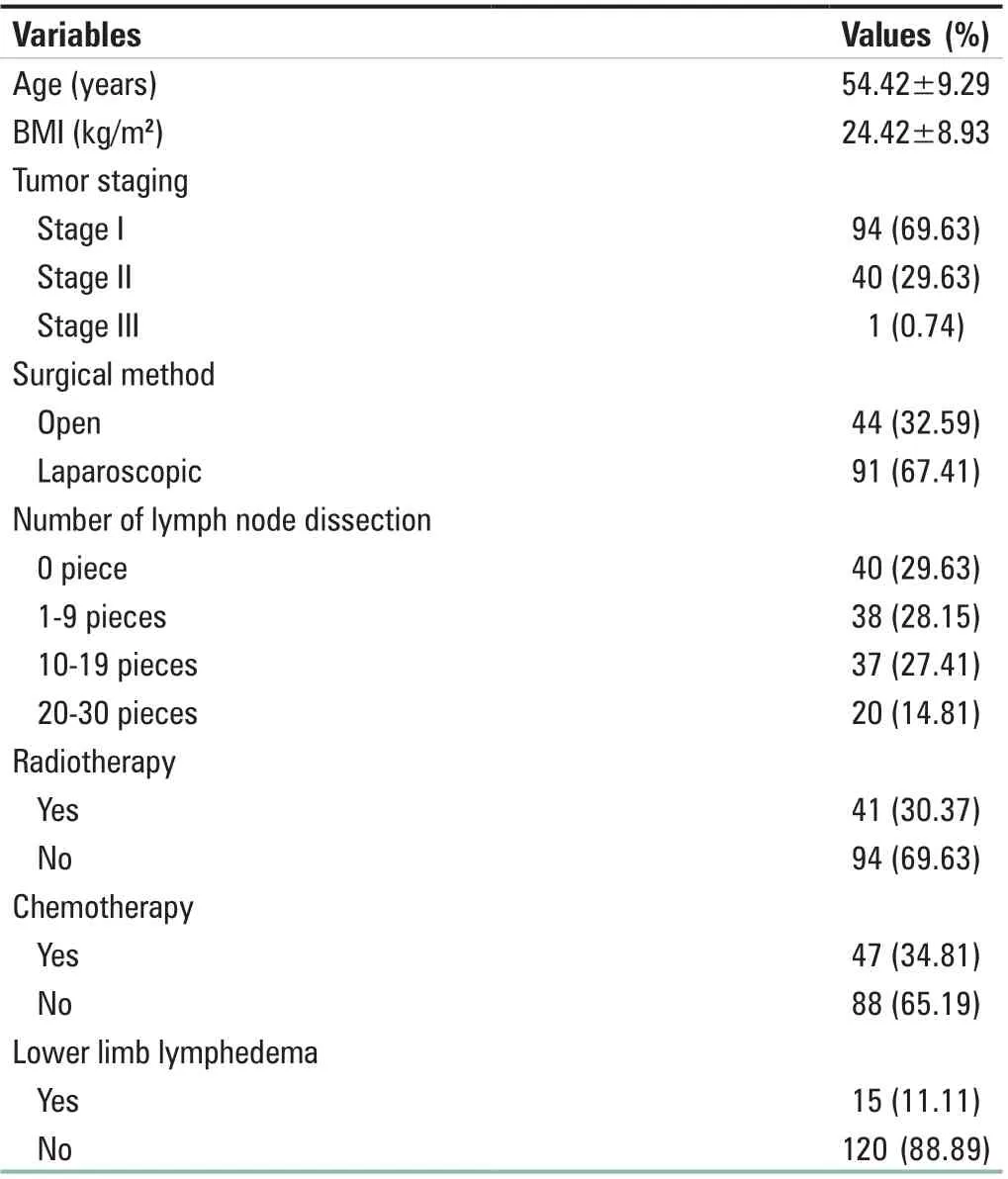
Table 1: Basic information of 135 patients with endometrial cancer
MATERIALS AND METHODS
Case selection
Data of 135 patients with endometrial cancer treated at the Department of Gynecology, Affiliated Hospital of Shaanxi University of Traditional Chinese Medicine from January 2013 to December 2019 were collected for the retrospective analysis.The inclusion criteria were patient who aged 30–82 years old,were diagnosed with endometrial cancer, underwent surgical treatment for endometrial cancer, and had normal cognitive function and ability to communicate normally. The exclusion criteria were as follows: (1) patients with other malignant tumors at the same time, (2) patients with primary lymphoid diseases or other nonendometrial cancer surgery-induced lower limb edema,or (3) those with serious lack of clinical data or follow-up data.
Survey methods Data collection methods
The patients’ inpatient medical records were reviewed to collect relevant information such as patients’ age, body mass index (BMI), tumor staging, surgical methods, number of lymph node dissection, receiving radiotherapy or not,receiving chemotherapy or not, and whether lower limb lymphedema occurred. Whether lower limb lymphedema occurred was evaluated by professional medical personnel in the form of telephone follow-up visits.
Assessment method of lower limb lymphedema
The Gynecologic Cancer Lymphedema Questionnaire (GCLQ)developed by Carter et al.[9]was used for assessing the presence of lower limb lymphedema. It contains 20 items,including whether there is restriction of movement, whether there is pressure, heaviness, numbness, and other self-sensory symptoms. The questionnaire has good reliability and validity,and has been widely used in the assessment and diagnosis of lower limb lymphedema,[10]and the total score of GCLQ ≥4 can confirm the diagnosis of lower limb lymphedema.[11]
Statistical analysis
The data were analyzed descriptively using the SPSS 20. 0 statistical software (SPSS, Chicago, IL, USA), and the data obtained from the follow-up results were analyzed by Chi-square test for one-way analysis and by multi-factor logistic regression analysis.
RESULTS
Basic information of 135 patients with endometrial cancer
The basic data and the occurrence of postoperative lymphedema of the lower extremities of the 135 patients with endometrial cancer were counted. The incidence of postoperative lower limb lymphedema in patients with endometrial cancer was 11.11% (15/135) [Table 1].
Univariate analysis
In this study, seven factors were selected as independent variables, namely age, BMI, tumor stage, surgical method, number of lymph node dissection, radiotherapy,chemotherapy, and the occurrence of lower limb lymphedema as the dependent variable. The results of the univariate analysis showed that the occurrence of lower limb lymphedema was related to different BMI, surgical methods, radiotherapy, and number of lymph node dissection (P < 0.05), but not to different chemotherapy,age, and tumor staging (P > 0.05) [Table 2].
Multi‑factor analysis
The results of multi-factor logistic regression analysis showed that BMI, number of lymph nodes dissection, and radiotherapy were the independent risk factors for the occurrence of lower limb lymphedema in patients with endometrial cancer aftersurgery, and higher BMI, higher number of lymph nodes dissected, and radiotherapy received after surgery increased the incidence of lower limb lymphedema [Table 3].
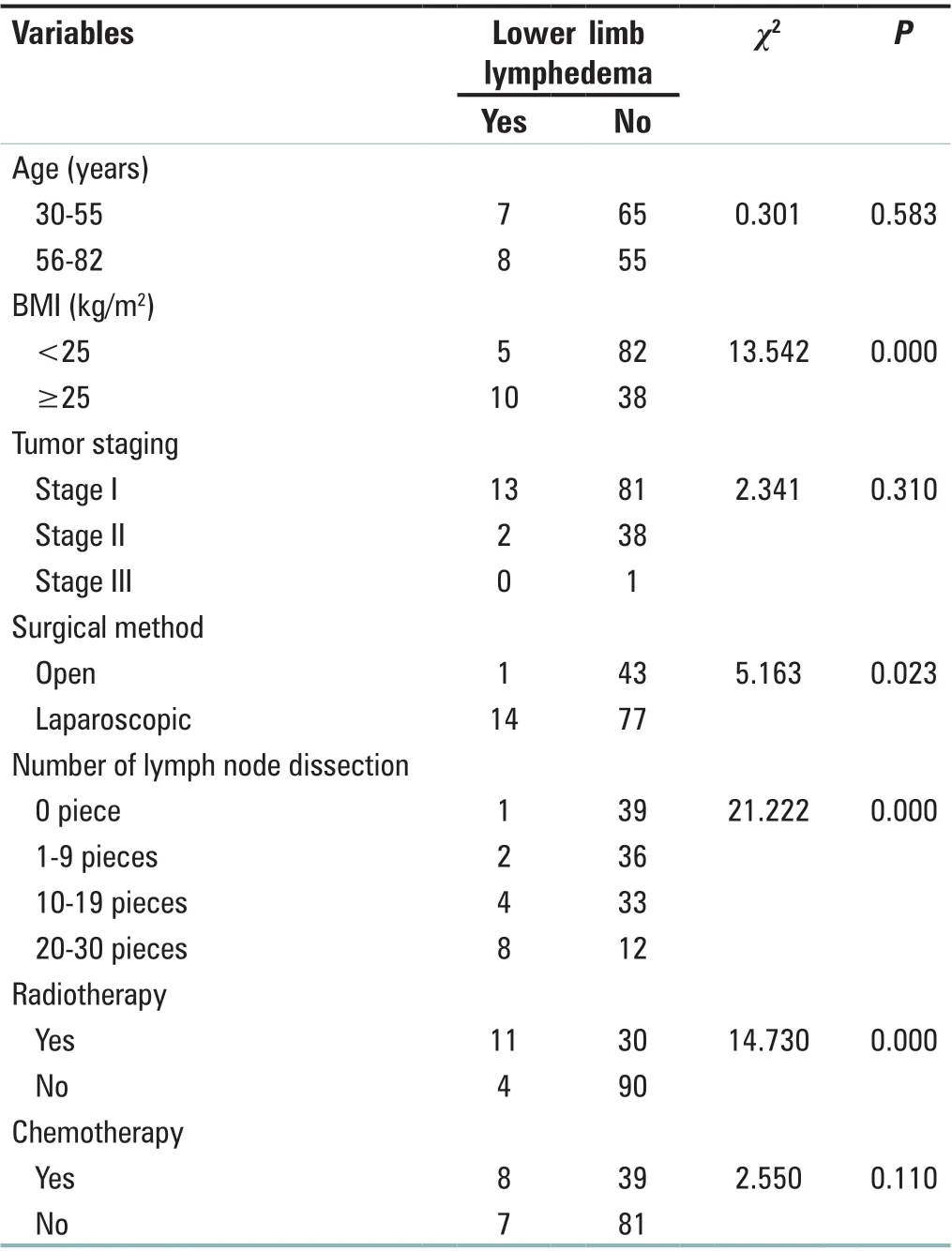
Table 2: Univariate analysis of risk factors for postoperative lower limb lymphedema in patients with endometrial cancer
DISCUSSION
Current status and risk factors for the occurrence of postoperative lower limb lymphedema in patients with endometrial cancer
Due to differences in assessment methods and diagnostic criteria, the results of existing studies on postoperative lower limb lymphedema associated with endometrial cancer vary widely. Mitra et al.[12]adopted subjective judgment, self-report, and clinical examination to assess 212 patients with endometrial cancer and found that the incidence of postoperative lower limb lymphedema was 7.1%, while Watson et al.[3]found that the incidence of lower limb lymphedema in patients with endometrial cancer was 19%–27% from 4 weeks to 18 months postoperatively using objective measurement techniques. The GCLQ is a subjective symptom assessment form. Because subjective symptoms often appear earlier than objective indicators,this questionnaire can help medical personnel to identify patients with lymphedema in a timely manner, which provides an important basis for the diagnosis and prevention of lower limb lymphedema in clinical practice.[13,14]In this study, we found that patients with endometrial cancer had subjective discomfort in lower limb lymphedema after surgery, but most of them did not pay attention to it, believing that rest and reduced activity could relieve the edema, but after relief, the edema would recur, which would bother patients and affect their quality of life, so it is important to screen high-risk groups and provide preventive and curative measures.
High BMI is a causative factor for all diseases and has also been shown by several authors to be an important risk factor for lymphedema.[15,16]Some studies have pointed out one of the similarity of risk factors for upper and lower extremity lymphedema is BMI.[17]Wu et al.[18]and Shen et al.[19]studied the risk factors for the development of lymphedema after breast cancer surgery, and both found that patients with BMI ≥25 kg/m2were more likely to develop lower extremity lymphedema. Similarly, the results of this study suggest that BMI ≥25 kg/m2is a risk factor for the development of lower extremity lymphedema after endometrial cancer surgery.Some researchers suggest that it may be that body fatness predisposes to lymphatic vessel obstruction, lymphangitis, or that the lymphatic system needs to transport more lymphatic fluid, which leads to the development of edema.[18,19]
Lymph node status is one of the important factors in determining the prognosis and adjuvant treatment needs of endometrial cancer,[20]and lymph node dissection in the treatment of malignant tumors, although beneficial, carries certain risks, so there has been no consensus about the significance of lymph node dissection in the treatment of endometrial cancer. In this study, the number of lymph node dissection was found to be a risk factor for the development of lower limb lymphedema in patients with endometrial cancer, which is similar to the findings of Beesley et al.[21]It is mainly because the higher the number of lymph node dissection, the greater the damage to the lymphatic system and the more severe the impairment of lymphatic return,which is more likely to cause lower limb lymphedema.[14]
Radiotherapy causes lymphatic vessels to dilate and edema, limiting the return of lymphatic fluid, leading to lymphangitis and causing lymphedema.[22]In this study,41 patients underwent postoperative radiotherapy, of which 11 (26.83%) patients developed edema, while 94 patients did not undergo postoperative radiotherapy of which 4 (4.26%)patients developed edema, showing that the incidence of lower limb lymphedema was much higher in radiotherapy patients than in nonradiotherapy patients. Therefore, it was concluded that radiotherapy was one of the risk factors forthe occurrence of postoperative lower limb lymphedema in endometrial cancer patients, Mitra et al.[12]similarly found that postoperative radiotherapy was associated with an increased risk of lymphedema in patients with endometrial cancer, while confirming a 5.6-fold increase in the risk of developing lower limb lymphedema in patients receiving radiotherapy. The increased risk of occurrence of 8.081-fold in patients treated with radiotherapy was found in this study,which may be related to the number of cases in this study.

Table 3: Multi‑factor analysis of risk factors for postoperative lower limb lymphedema in patients with endometrial cancer
Suggestions for the prevention and treatment of postoperative lower limb lymphedema in endometrial cancer patients
With regard to the high-risk factors of postoperative lower limb lymphedema in endometrial cancer in this study, the following measures can be taken to prevent it: (1) High BMI: For patients, BMI is a controllable factor, which can be adjusted in various ways, such as optimizing eating habits, dietary patterns and eating choices, performing aerobic exercise for at least 40 min at regular intervals every day.[23]At the same time, acupuncture and cupping therapy can improve BMI of patients and help to reduce the occurrence of lymphedema.[24](2) Lymph node dissection:for this drawback of lymph node dissection, many clinicians advocate abandoning lymph node dissection altogether;however, this may lead to inadequate treatment, and some researchers pointed out that sentinel lymph node labeling has become a feasible compromise between full lymph node dissection and no lymph node sampling, and will reduce the risk of lower limb lymphedema incidence, but this option is now less studied and needs to be further explored.[16,25](3)Radiotherapy: For patients with endometrial cancer who adopt surgical options, the indications for radiotherapy should be strictly controlled according to the patient’s condition, and radiotherapy should be avoided as much as possible when radiotherapy modalities are not available, so as to minimize the incidence of lower limb lymphedema and reduce unnecessary harm to patients.
For patients with lymphedema of lower extremities, they should take timely measures to reduce the edema and promote its remission. Although oral diuretic drugs in Western medicine can temporarily reduce lymphedema, long-term use will cause water and electrolyte imbalance and even aggravate edema, and surgical treatment is highly invasive, so they are not the best methods to treat lymphedema of lower limbs.In recent years, the treatment of lymphedema in the Chinese medicine has received more and more attention. Chinese herbal medicine for internal use, Chinese herbal fumigation,Chinese herbal compress, and acupuncture are effective in reducing lower limb lymphedema. To enhance the efficacy, the above methods can be combined with physical therapies such as manual massage, ligature therapy, and lymphatic drainage techniques. In addition, warm needle moxibustion combined with cupping, which has been proven to be effective for upper limb lymphedema,[26]can be conducted for clinical research.It will provide a basis for discovering the most appropriate treatment options for lower limb lymphedema.
CONCLUSION
Lower limb lymphedema is a major postoperative complication of endometrial cancer, which is often easily ignored by patients due to different degrees of autonomic sensation and mild symptoms at first, so timely detection and preventive and therapeutic measures are key issues worthy of attention. The results of this study showed that BMI, the number of lymph node dissection and postoperative radiotherapy are risk factors for lower limb lymphedema in endometrial cancer. For this group, a combination of prevention and treatment can be used to reduce the swelling, i.e. through acupuncture, physical therapy, manual drainage, bandage compression and functional exercise, which will not only effectively reduce the edema but also decrease the probability of recurrence. There are some shortcomings in this study: the sample size is small, the follow-up time is unequal,only the incidence of lower limb lymphedema was counted,and the degree of occurrence was not studied. Currently, there are few studies on lower limb lymphedema associated with endometrial cancer in China, so researchers should pay attention to this area, conduct more comprehensive and in-depth studies,screen key populations, and provide a more reliable basis for preventive and therapeutic measures.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
杂志排行
Journal of Integrative Nursing的其它文章
- Nursing care of a patient with programmed cell death protein‑1 immunotherapy‑related myocarditis combined with coronary heart disease
- Application of rehabilitation nursing technology in the pulmonary rehabilitation of the patients after lung cancer operation
- Discussion on optimizing nursing rounds model based on the inheritance of traditional Chinese medicine nursing
- The effect of baduanjin exercise in rehabilitation for functional ankle instability: A study protocol for a ra ndomized controlled pilot trial
- Effect of structured education program on physiological and psychosocial outcomes in type 2 diabetes patients:A randomized controlled trial
- Control effect of structured skin care plan of integrated Chinese and Western medicine in elderly patients with incontinence‑associated dermatitis