Realities,scope,challenges,and facilitators for implementation of nurse practitioner’s role in India:A review
2021-05-19MlrKodiSureshShrm
Mlr Kodi S ,Suresh K.Shrm
a Department of Nursing,All India Institute of Medical Sciences,Rishikesh,Uttarakhand,India
b Department of Nursing,All India Institute of Medical Sciences,Jodhpur,Rajasthan,India
ABSTRACT India is in dire need of an alternative to general medical practitioners to overcome a severe shortage of doctors,especially in rural and underprivileged regions.Empowering nurses through nurse practitioner(NP) role is the superlative solution to provide quality health care in primary care setting.Based on conceptions and research findings of the NP’ s role,we analyzed and examined the realities,scope,and barriers for implementing the NP’ s role in India and propose future strategies to create a NP cadre.
Keywords:Advanced nursing practice Nursing care Nurse practitioners Role India
What is known?
· Most of the institutes in India have implemented nurse practitioner(NP)programs since 2007;however,there is no specified role and the scope and designated cadre.
What is new?
· This article reviewed the background and situation of the NP program in India.
· This review has deliberated the prospective scope for NP roles in India.
· It discusses the potential barriers for implementing the NP’s role in the country and elaborated on future strategies for implementing the NP cadre and viable solutions for considerations.
1.Introduction
Most developing countries are facing severe health care workforce challenges,particularly concerning physician availability.The doctor-to-population ratio in India is 0.725 per 1,000 population,mainly strenuous in concentration in urban areas leading to limited health care access in rural settings [1].The rising demand for healthcare services on the root level places huge concern and strain on healthcare delivery systems,thus leading to quality comprised health care services.Therefore,there is a significant need to reorganize and decentralize healthcare services by a task-shifting approach.Nurses and midwives are the largest anchor of the health care delivery system and play a significant role in providing preventive,promotive,and rehabilitative care services[2,3].Hence World Health Assembly passed a resolution in 2011 to strengthen and expand nurses’ roles by including them in the primary care settings [4].
Registered nurses get special training and license for advanced practice,giving them a license to make medical decisions,administer drugs/therapies,order diagnostic tests,and perform specified procedures.The nurse practitioner(NP)is a generic term and has a variety of titles,including advanced nurse practitioner (ANP),clinical nurse specialist (CNS),nurse specialist,and advanced clinical practitioner [5].The role is existing in the USA since 1965,the United Kingdom since 1980,in Australia since 1990,and in the Netherlands since 2010 as a result of primary care physician shortage[6].The NP role is sprouting enormously worldwide.It has provided primary,acute,specialty health care to patients of all ages for more than a half-century across the globe [6,7].
The International Council for Nurses (ICN) reports,almost 70 countries across the globe successfully implemented nurse practitioner roles,including Asian countries like South Korea,Singapore,and Thailand [6,8].Evidence worldwide highlights the benefits achieved by the advancement of nursing care through the NP role.Cochrane reviews and meta-analysis have demonstrated that NPs can manage the patients at the primiary care level [8,9],and the substitution of physicians by nurses in primary care settings enhances quality care that leads to better health outcomes.It also shows that time spends by NPs caring for patients and health teaching leads to higher satisfaction among patients and family[10,11].
According to ICN reports,the number of NPs doubled in a decade,from 120,000(in 2007)to more than 270,000 in 2017[12],and beneficiaries have faith in health care offered by NPs that over 1.06 billion people evidence visits NPs annually.The number of primary care NPs is projected to increase by 84%between 2010 and 2025.If this trend continues by 2030,the proportion will bounce from 19% to 29% and continue to rise [13,14].
Global statistics show that the highest proportion of ANPs are in the USA,i.e.,40.5 per lakh population,followed by Netherland(12.6),Canada (9.8),Australia (4.4),and New Zealand (3.1).Moreover,their number is rapidly increasing in most of the country about 27.8% compound growth rate in Netherland,and it was 6.1%in the USA[15].Surprisingly,the growth of NPs is 3-9 times higher than doctors in the Western world,which signifies that their role is well accepted in the health care delivery system of these countries.Studies found that 67%-93% of curative primary care services are managed by NPs in the Western world.To our surprise,it was much cost-effective compared to care provided by physicians,i.e.,29%in primary care and 11%-18% in inpatient services [14,16].
The American Association of Nurse Practitioners (AANP) observes National Nurse Practitioners week every year between November 10-16 to nudge the lawmakers about the significance of transforming outworn laws,policies,and practices so that NPs can practice to their fullest scope incommensurate to their education and training[6,17].Studies reveal that there is significant variation in expected practice and actual practice of NP in different states and countries because of variation in legislative autonomy;however,they were found practicing assessment,ordering tests,making the diagnosis,prescribing medicines,referring patients to higher centers as the scope of practice [17].
Hence introducing the NP role is the answer to address health care challenges,deliver quality health care services,and accomplish sustainable development goals (SDGs) in our country.This review aims to comprehend the reality,scope,challenges,and future strategies for implementing the NP role in India.
2.Search strategy
We summarized evidence concerning the reality,scope,barriers,and facilitators in implementing independent NP’ roles in India.An integrative literature search was executed by browsing databases including Scopus,PubMed,CINAHL,Psych INFO,EMBASE,ScienceDirect,Web of Science,and nursing professional organization Webpages.The search was done by using keywords and Boolean operators of (nurse practitioner role) OR (advanced nurse practitioner) OR (barrier for advanced nurse practitioners)OR (scope for nurse practitioners) AND India OR Indian nursing council.We also screened the reference list of selected articles to find other relevant items.Selected Literature was assessed,and findings synthesized.
3.Scenario and realities of nurse practitioner role in India
The National Health Policy (2017) recognizes that redesigning the health care delivery system and establishing cadres like NPs and public health nurses to increase their availability in most needed areas [18].Our country’s workforce experts agreed on a growing wide gap between the populations and demand for primary care physicians.The introduction of the NP role is a better way to meet these challenges [19].
The Ministry for Health and Family Welfare (MoHFW) emphasized that the nurses occupy an essential position in healthcare delivery.They can be utilized equally to doctors when we think of achieving the SDGs [20].The union government is considering creating a cadre of NPs to address the shortage of doctors in rural areas [19,20].
Roots of unorganized and unregulated NPs can be found in states like Rajasthan;many RNs practice as general nurse practitioners,especially in rural areas though it is very well accepted by the public but not legalized[21].In the year 2002,the Government of West Bengal was the first state in India to start nurse practitioner in midwifery course (NPM) under the India-AusAID project provided training for 18 months to diploma and graduate nurses yet unable to obtain due recognition [22].On a track,Gujarat’s government started in 2009 and sanctioned 25 posts of independent midwifery practitioners (IMP) but still waiting to appoint [21,23].The policy process was delayed for several reasons includes less drive and shared vision,unconfined about developing an autonomous cadre of midwives,and less space for open dialogue.Similar steps to train registered nurses in NPM by Telangana,Kerala,West Bengal,and other states [21,24].However,it could not attract the candidates due to the absence of clarity about registration with the nursing councils,the scope of practice,and the employment.
The government also came up with expanded role nurses through nurse-led health care delivery models.Few institutions in India took up this model of nurse-led clinics.A few extended their roles like stoma nurses,stroke nurses,public health nurses,and diabetes nurse educators.But they are trained in-house,and their titles are not protected by any legislation [25].
The Indian Nursing Council (INC) implemented a NP in the critical care program with the approval of the MoHFW all over the country since 2017 to expand the role of registered nurses.INC has signed a memorandum of understanding (MoU) with the University of Houston College of Nursing in April 2018.In continuation of MoU,INC invited two faculties from the University of Houston to share and guide in the implementation of the nurse practitioner in critical care (NPCC) and a doctorate of nursing practice (DNP)programs in India [26].The number of Institutes (Fig.1) offering NPCC course in the country [26,27]illustrates that it is declined over the years due to lack of a specified role for NPs in the health care delivery system,no provision of registration in nursing councils as NPs,lack of legal protection to NP title and limited scope of employment/practice,conversely recently passed out NP graduates in critical care are working as a routine clinical nurse [28].
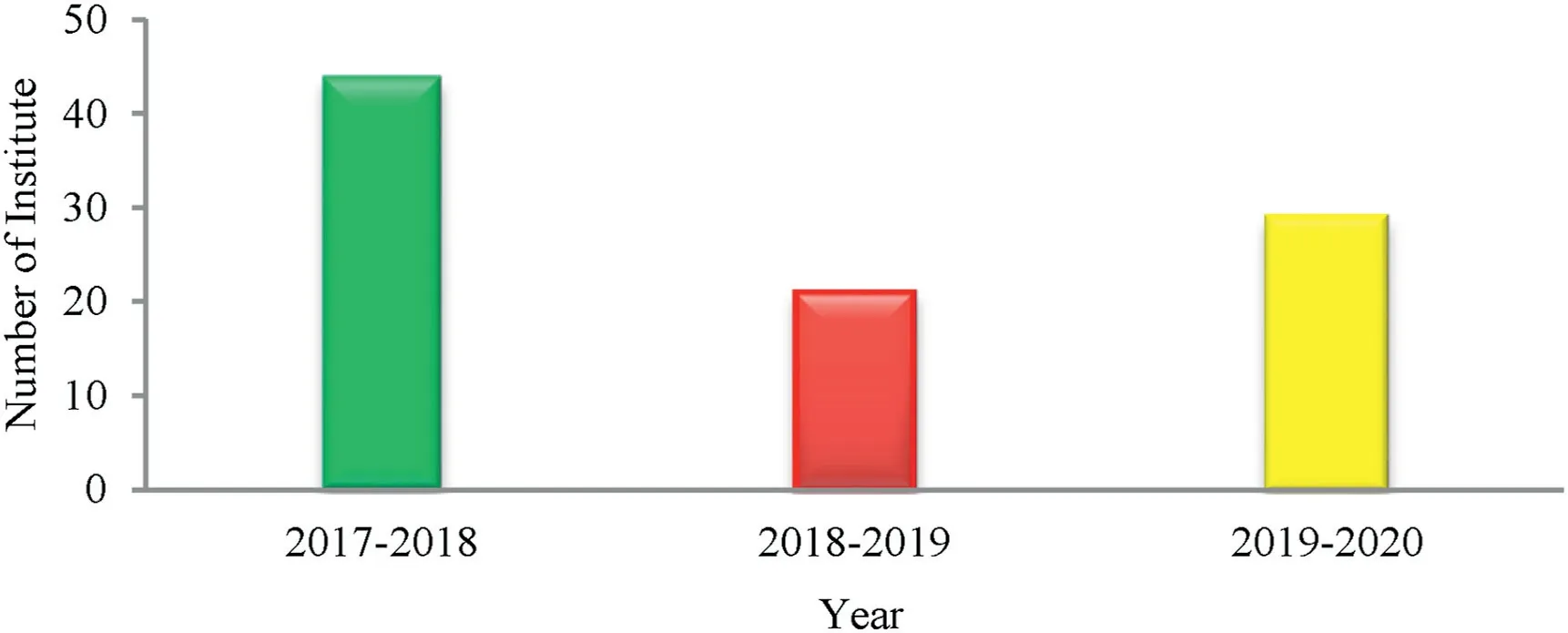
Fig.1.Number of institutes offering nurse practitioners in critical care program in India [20,21].
The NP role is promising in India.However,implementing the NP role in the multi-professional structure is a complex and recurring task in the country.Nevertheless,it is possible with meticulous planning and execution through strong legislation,licensure with a clear scope of practice,and carrier pathways for NPs.
4.Scope for nurse practitioners in India
The AANP stated that NPs could practice independently in various healthcare settings,including a primary health center,community health center,and tertiary care hospitals.They can also perform an assessment,diagnosis,treatment,and evaluation services without oversight by the physician;however,their roles and legal authority vary between countries[15,21,29].A clearly defined role is a key to practice,and this is a precise instance to make the exact scope of practice in our country.The most-reported range of ways across the world will guide us to plan meticulously and implement our country’s scope of practice (Table 1).
5.Challenges/barriers in the implementation of nurse practitioner role in India
The NPs have historically encountered many obstacles to practice throughout the world.Nursing is considered a lower-level profession in many countries,and nurses receive little acknowledgment,no authority or power [31].Even National Medical Council Bill (NMC),currently under discussion,does not mention anything about nurses or any other professional council [35].Though the WHO recognized nurses and declared 2020 as a year of nurses and midwives;however,it is tricky to implement a new nursing role in a multilayered health care context.Researchers have examined many hindrances in the implementation of NP roles worldwide.Empirical evidence about barriers to the NP’s performance presented as structural barriers,functional barriers,and perceptional barriers (Table 2).
6.Facilitator for implementation of nurse practitioner care in India
An NP role is in the infancy stage and gained significant momentum in India.The MoHFW is contemplating the introduction of NP title in consultation with the INC and other stakeholders.Recent national health policy(2017)also included establishing the cadre of NPs in the public health system[18].Various countries like the USA,United Kingdom,Australia,and the Netherlands set an example for implementing ANP roles.This is high time to implement a NP cadre in India for ensuring affordable and accessible healthcare,especially in underserved and deprived areas.However,several pertinent questions like.
How:How to get a license? How are NPs to be instituted?
Where:Where will the training take place? (refers to educational institutions/standards)
Who:who will teach?What are the educational qualifications?When:When NPs license will be renewed?
What:what will be core competencies in their respective area of practice? What will the carrier pathways of NPs?
Which requires an answer for effective planning for the implementation of NP cadre in India.Furthermore,the following strategies may help in the successful implementation of NP care in India.
6.1.Restructuring nursing education and curriculum
The NP programs must be implemented on the residency model,and the curriculum must purely competency-based.As per INC,the NP course’s entry-level criteria is a registered graduate nurse with one year of clinical experience[31,38].A NP expected to have sound knowledge of basic biomedical science subjects such as anatomy,physiology,biochemistry,microbiology,pharmacology,pathology;however,the study finding across the world reveals that the physician refuses to accept NPs due to their poor knowledge in pharmacology,pathology,anatomy,physiology,assessment skills,diagnosis,critical thinking,and decision making [21].It indicatesthat there is a need to restructure our basic nursing curriculum into a competency-based curriculum.Besides basic core competencies,it must encompass the clinical application of pharmacology and pathology,skills in assessment,pharmacology,critical thinking,decision making,nursing informatics,including soft skills like therapeutic communication,maintaining an interpersonal relationship,breaking bad news,etc.
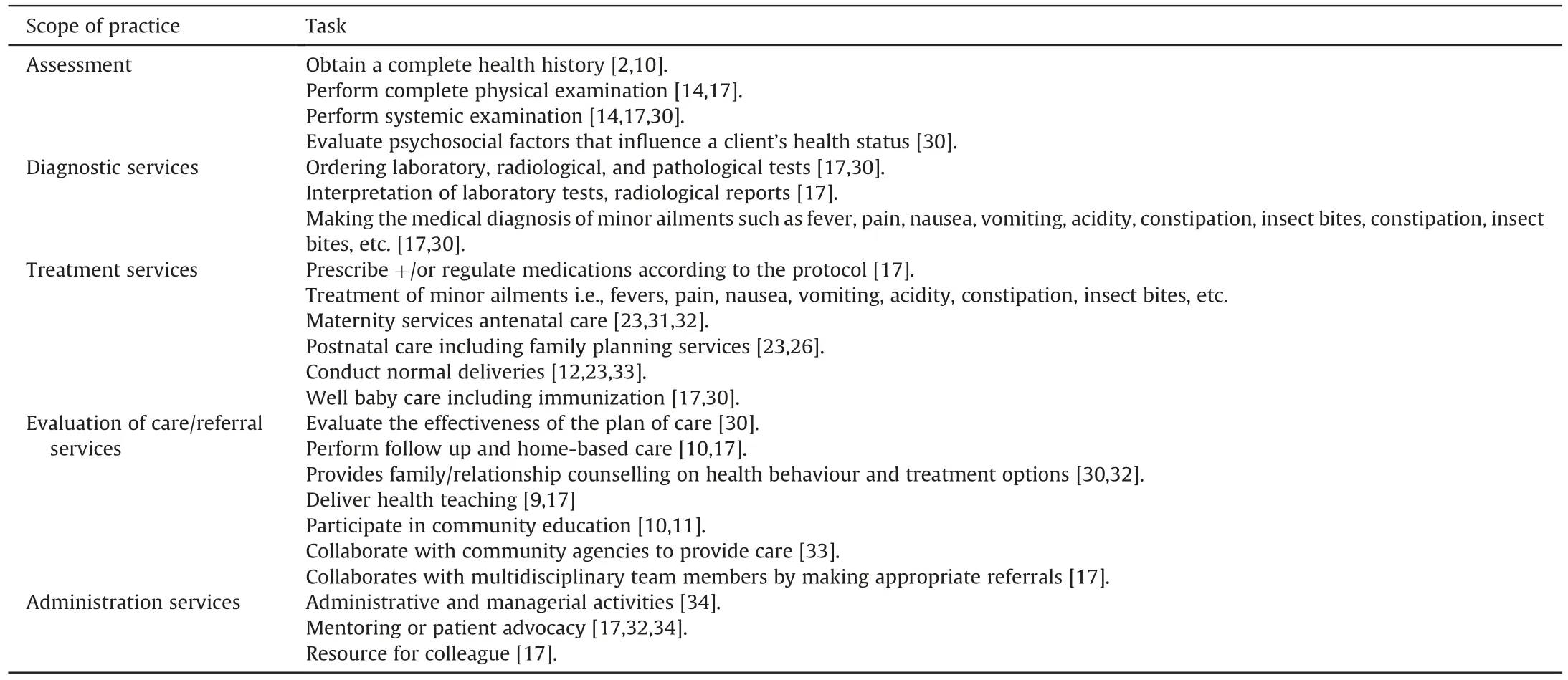
Table 1 Most often reported scope of practice for nurse practitioners.
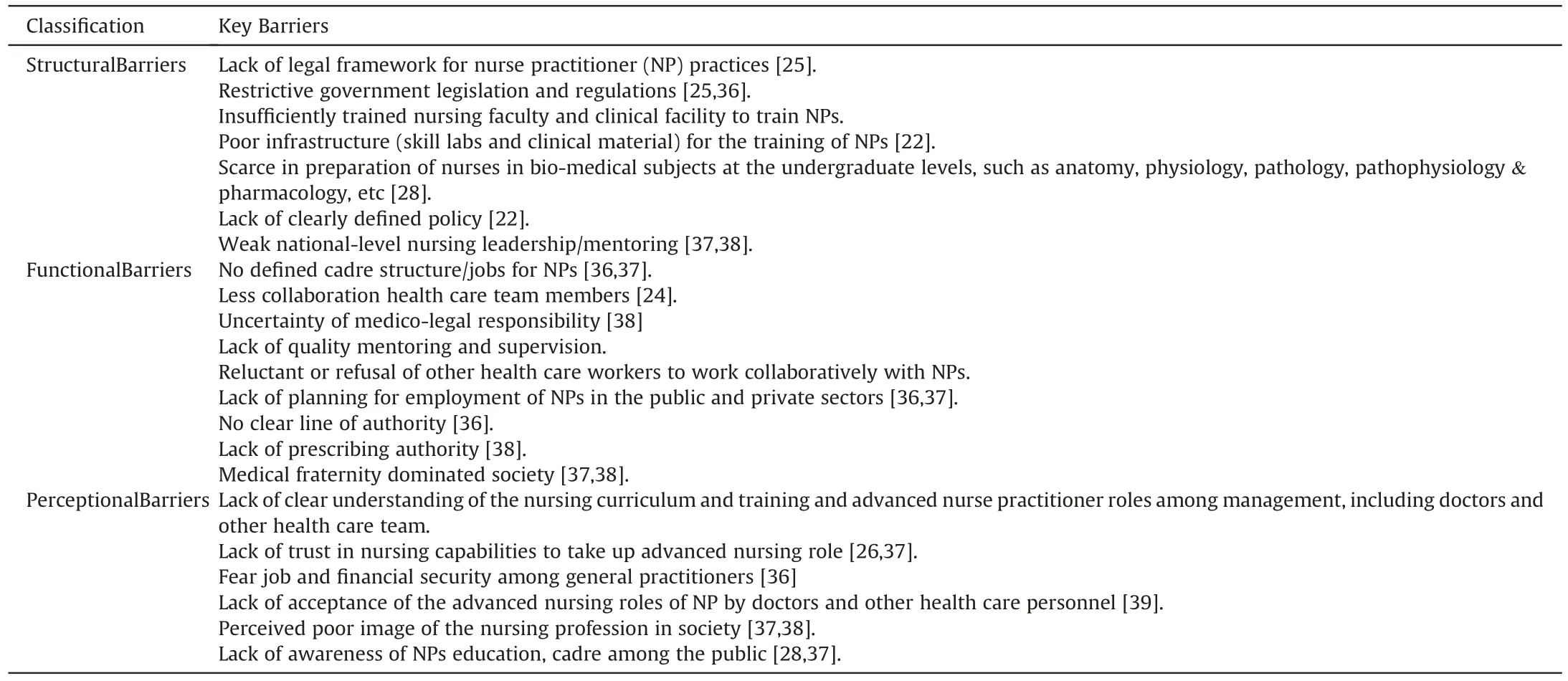
Table 2 Barriers to implement nurse practitioner role inIndia.
6.2.Building sound infrastructure for training competent nurse practitioners
The NP curriculum is designed so that the practicum accounts for 85% and theory classes for 15% [24,37].Thus to build up core competencies for NPs,the institution must have a dedicated skill lab equipped with moderate-to-high fidelity simulators and various task trainers and sufficient clinical facilities for adequate opportunities to observe and practice required competencies.
6.3.Nursing faculty capacity building to train competent nurse practitioners
Nursing education has rapidly evolved from hospital-based diploma nurse training to university-based graduate,postgraduate,and NP programs in India [37,38].Therefore,there is a serious shortage of experienced and competent nursing faculty in this country.The NP program is recently launched in India.Thus there are very limited or no trained NPs in India to teach and guide new NPs.Therefore,building and strengthening nurse educators through regular in-service education-focused and specialized training and collaborating with experienced medical faculty may help training nursing faculty for effective implementation and running the NP programs in India [36].
6.4.Radical transformation in nursing practice legislation and licensure
The INC and state nursing council should provide a clearly defined role of practice for the NPs.It should be protected by legislation through the nurse practice act,which may be done by an amendment in the existing INC act,1947,and respective state nursing councils.The amended acts must include the provision of registration for the nurse specialties and practitioners and it clearly defines the scope of practice,titles,and licenses for all levels of nurses including ANP [37].Legally protected licensure is essential to execute the NP role independently.Furthermore,amendments will also be needed in other legislations such as the Pharmacy Act(1948) and The Drugs and Cosmetics Act (1940),which have potential implications for the independent practice of NPs [38].
6.5.Regular updating and periodical licensure renewal
Health care technology,strategies,and research can change professional practice,becoming an issue for public safety.Therefore,health care professionals,including NPs,need to be regularly updated,and there must be a periodic licensure renewal system.Renewal of NP licensure policy and procedure varies between countries [30,33].ANCC recommends five-year renewal certification with the requirement of continuing education hours,practice hours,research publications,and licensure renewal examination[40].Consequently,the state nursing council should plan and implement common knowledge and skill update and licensure renewal for NPs [36].
6.6.Specialization and defined career pathways for nurse practitioner
The INC has recently launched NPs in critical care;however,there is a need to expand the scope of NPs in other fields of specialization such as primary health care,family health,midwifery,diabetes,geriatrics,pediatrics,mental health,and so on[38,39].Moreover,there must be defined career pathways of NPs from entry-level[38].
6.7.Promoting research on nurse practitioner role
Numerous studies were carried out before and after the implementation of NP roles all over the world.It facilitated them to overcome barriers for successful implementation.NP role is an upcoming trend,and there are limited studies done and published in India.Thus there is a profound need for research to explore barriers,scope,and strategies throughout pre and postimplementation of NP role.Furthermore,the first batch has passed out,so they may be monitored for the acceptance and impact in society;also,awareness,perception,and acceptance of healthcare professionals and the general public,the effect on cost,patient satisfaction,etc.may be explored[38,38].
6.8.Empowering nursing associations and societies of nurse practitioners
There must be an association and society of NPs for effective political lobbying to persuade policy and image building of nurse practitioners like the AANP and the Canadian Association of Advanced Practice Nurses [36].
6.9.Create awareness regarding nurse practitioners’ role
General public knowledge about NP roles and lack of understanding by other healthcare personnel have been problematic over time.Further,it is the most frequently reported barrier,leading to a lack of acceptance of the role [17,21].As it is a novel/less known concept in India,it’s essential to familiarize the concept regarding the role and responsibilities of NP to the beneficiaries and health care personnel to gain acceptance of the cadre.
7.Conclusion
The NP cadre emerged in the 1960s in the USA and subsequently implemented in other developed and developing countries,which is found quite successful and is rapidly expanding.India has unrecognized roots of NPs in states like Rajasthan,where registered nurses independently provide curative health care services to people in rural communities,which are not regulated and legalized but accepted by people.The shortage of primary physicians has necessitated the need to implement NP care in the country.Recently,the INC has launched a NP program in critical care nursing.Evidence support that NPs can effectively provide a wide range of curative services such as assessment,diagnosis,treatment of minor ailments,curative,rehabilitative,and referral services,especially in underserved and deprived communities.However,in the absence of a clearly defined scope of their practices,nursing practice act,specified licensing,practice title,and cadre structure for NPs in the health care delivery system,it has not yet taken momentum in the country.Nevertheless,reforms in government policies,procedures,laws,nursing practice acts,licensing,and autonomy for nurses,nursing education,defined scope of rules,and creation of cadre structure may facilitate effective implementation of NP programs in India;which is the need of the hour to ensure affordable and accessible healthcare for the people especially in underserved and deprived regions of the country.
CRediT authorship contribution statement
Malar Kodi S:Methodology,Writing-original draft preparation,Visualization.Suresh K.Sharma:Conceptualization,Verification,Writing-reviewing and editing,Supervision.
Declaration of competing interest
No conflict of interest has been declared by the authors.
Acknowledgement
We thank professor Som prakas Babu,Department of general surgery,AIIMS,Rishikesh for continuous motivation and support.
Appendix A.Supplementary data
Supplementary data related to this article can be found at https://doi.org/10.1016/j.ijnss.2021.03.003.
杂志排行
International Journal of Nursing Sciences的其它文章
- Associations between risk factors for cardiovascular diseases and frailty among community-dwelling older adults in Lanzhou,China
- Supplement to the published paper“Theory-guided interventions for Chinese patients to adapt to heart failure:A quasi-experimental study”
- Lived experiences of the disease journey among patients with idiopathic pulmonary fibrosis
- Persistent effect of nurse-led education on self-care behavior and disease knowledge in heart failure patients
- Using action research to evaluate a nursing orientation program in a multicultural acute healthcare setting
- Effects of a theory of planned behavior-based intervention on breastfeeding behaviors after cesarean section:A randomized controlled trial
