Effects of a theory of planned behavior-based intervention on breastfeeding behaviors after cesarean section:A randomized controlled trial
2021-05-19JunWenGuilingYuYnKongHollyWeiShurnZhoFurongLiu
Jun Wen ,Guiling Yu ,Yn Kong ,Holly Wei ,Shurn Zho ,Furong Liu ,*
aQingdao Women and Children’s Hospital,Qingdao,China
bCollege of Nursing at East Carolina University,Greenville,NC,USA
cSchool of Nursing,Qingdao University,Qingdao,China
ABSTRACT Objectives:To examine the efficacy of an intervention based on the theory of planned behavior (TPB) in improving breastfeeding behavior among women with cesarean sections (C-sections)Methods:This research was a randomized controlled trial.Women with planned elective C-sections were recruited to participate in a randomized controlled trial between June and September 2020.One hundred thirty-two women were divided randomly into the intervention (n=66) and control group (n=66) by systematic random sampling.In the intervention group,an intervention project was implemented after the C-section to establish positive breastfeeding attitudes,cultivate supportive subjective norms,enhance perceived behavioral control,and strengthen breastfeeding intention to change behaviors.Those in the control group received routine pre-and post-delivery care.Exclusive breastfeeding rate and breast problem were collected at 5 days,2 weeks,and 1 month after C-section.The modified Breastfeeding Attrition Prediction Tool(BAPT)on the first day in the hospital,two weeks,and one month after C-section and Numerical Rating Scale(NRS)24 h postoperatively were used to compare the intervention effect between the two groupsResults:After the intervention,the intervention group had significantly higher exclusive breastfeeding rates than the control group at five days (86.4% vs.60.6%),two weeks (77.3% vs.57.6%),and one month(74.2% vs.50.0%) after the C-section.Besides,the intervention group was less likely to have sore nipples at five days (6.1% vs.18.2% in the control group,P <0.05) and two weeks (9.1% vs.12.1% in the control group,P <0.05).After two weeks of intervention,attitude scores(90.64±8.31 vs.87.20±8.15,P <0.05),subjective norm scores (88.07 ± 24.65 vs.79.42 ± 19.47,P <0.05)and behavior control scores in the intervention group were significantly higher than those in the control group.After one month of intervention,attitude scores (90.34 ± 10.35 vs.84.22 ± 10.51,P <0.05) and behavior control scores(43.13±5.02 vs.39.15±4.69,P <0.05)in the intervention group were significantly higher than those in the control group,which resulted in the higher breastfeeding intention in the intervention groupConclusion:This study indicated that the TPB-based interventions effectively improved women’s breastfeeding behaviors after C-sections.
Keywords:Breastfeeding Cesarean section Intervention studies Theory of planned behavior
What is known?
· Breastfeeding benefits children and their mothers in both the short and the long term.
· A significant disadvantage of a cesarean section (C-section) is breastfeeding’s the adverse effect in the early postpartum period.C-section likely affected breastfeeding primarily by jeopardizing the establishment of lactation during the first month postpartum.
What is new?
· This article highlights the value of intervention based on the theory of planned behavior (TPB) design to improve breastfeeding behavior among women after cesarean delivery.
· This study recommends that community health providers plan more effective and continuous education that will better support and be responsive to mothers’ breastfeeding about one month after cesarean delivery.
1.Introduction
Breastfeeding has both short-and long-term benefits for children and their mothers.It can reduce mothers’ risk of postpartum bleeding,breast and ovarian cancers,and type 2 diabetes mellitus[1].Breastfeeding is also correlated with a lower risk of certain illnesses in a child,such as respiratory disease,gastrointestinal infection,asthma,and obesity [1].However,the prevalence of breastfeeding has not been optimized to date in China.According to data released by the China Development Research Fund in 2019,the exclusive breastfeeding rate in the first six months was 29%[2].The prevalence of exclusive breastfeeding in China falls short of the global nutrition target of at least 50% exclusive breastfeeding [3].Thus,promoting breastfeeding has become one of the major initiatives in improving women’s and children’s health.
Cesarean section (C-section) is considered a significant barrier to breastfeeding in the early postpartum period [4].A metaanalysis of more than 84,518 participants showed that women undergoing C-sections had a lower breastfeeding rate than women undergoing vaginal delivery [4].Previous research reported that factors influencing breastfeeding post-C-sections included postpartum fatigue,physical restrictions,perioperative medication,decreased infant sucking activity,and delayed breastfeeding initiation [5].Besides,cesarean delivery was correlated with the increased use of formula in hospitals,delayed early sucking,and shortened breastfeeding duration [6,7].In East Asia,including China,the average C-section rate rose from 13.4%in 2000 to 28.8%in 2015.The rate increase was more than 15% and was one of the fastest worldwide[8].Therefore,it is essential to explore a nursing intervention model in line with C-sections for mothers.
One of the behavior-change theories showing effects on promoting breastfeeding is the theory of planned behavior (TPB) [9].The TPB is a theory used to help predict and explain healthy behaviors in general and guide intervention programs [10,11].Previous research explored the factors affecting breastfeeding after Csection based on TPB variables.The results showed that the challenges for breastfeeding after C-sections included physical discomfort,knowledge and skills deficit of breastfeeding,lactation deficiency,and lack of knowledge and coping skills in managing their depressive mood [12].C-sections’ negative impacts on longterm breastfeeding could be reduced with planned breastfeeding behavior interventions[5].Thus,the present study aimed to study the feasibility and effectiveness of a set of TPB-guided interventions on breastfeeding rates among women after C-sections.
The TPB assumes that intentions are a primary determinant of behaviors and are affected by the following three variables:attitude,subjective norms,and perceived behavioral control [9,13].A theoretical framework of the TPB in breastfeeding is shown in Fig.1.Research indicates that attitude is related to favorable or unfavorable views of breastfeeding behaviors [12].Increasing maternal awareness of the breastfeeding benefits and mastering related knowledge are the most common strategies to improve attitudes.Subjective norms refer to individuals’perception of their potential referent groups,a source of their identity,or social pressure,determining women’s decision-making on breastfeeding.For the current study,subjective norms were defined as the degree of support from participants’ referent groups,medical staff,families,particularly husbands,mothers,and mothers-in-law.These people can potentially affect women’s breastfeeding intentions.Perceived behavioral control reflects individuals’perceived ability to perform a particular behavior.Higher behavioral control indicates women’s heightened awareness and belief to reassess their existing breastfeeding barriers after C-section.As a theoretical framework,the TPB has been well used to guide research to predict or intervene in behavior change [14,15].In this study,the TPB provided a holistic perspective to help researchers develop a framework for promoting breastfeeding behaviors.
2.Methods
2.1.Study design
This is a randomized clinical trial with parallel grouping.The control group received routine care with primary breastfeeding health education;the intervention group received TPB-based interventions to promote breastfeeding after C-section.
2.2.Participants and setting
The study was conducted from June to September 2020 in the obstetric unit of a university-affiliated women and children’s hospital in China.Pregnant women with a planned elective C-section were screened on admission to confirm their qualifications for inclusion.Women meeting the inclusion criteria were contacted and invited to participate in the study.Inclusion criteria were that participants should be:1) 18 years or older;2) physically and mentally capable of communicating;3) without illnesses or problems(such as severe infection,serious heart attack,and long-term medication)that prohibit breastfeeding;4)able to attend the study,and 5) with access to internet access to complete the follow-up questionnaires online.The exclusion criteria were as follows:1)had a gestational age less than 37 weeks;2)intended to bottle feed with formula;3) had already received or attended other comprehensive breastfeeding interventions;4) had multiple pregnancies,and 5) had inverted nipples.
Preliminary studies suggested that the exclusive breastfeeding rate for one month after cesarean delivery was 50%.We estimated that the behavior change rate was 25%,and the missed rate was 20%.The study’s sample size was calculated using PASS 22.0,a power-analysis software.With a power of 80%and an alpha of 0.05,we needed 66 participants in each group.
A block randomization method was used to ensure an equal number of participants between groups.Participants were randomly assigned to the intervention and control groups with a block of 4.The randomization list was generated using SPSS 22.0 software.The block randomization pattern was created by a researcher who was not involved in recruiting participants.Block order and grouping information were not revealed to participants,researchers,and data analysts.
2.3.Ethical consideration
The hospital’s Ethics Committee approved this study.Informed consent was obtained before data collection.Participants were fully aware of the risk and benefits of the research and the right to withdraw at any time.They were assured that study participation was anonymous and that their personal information was protected throughout the study.
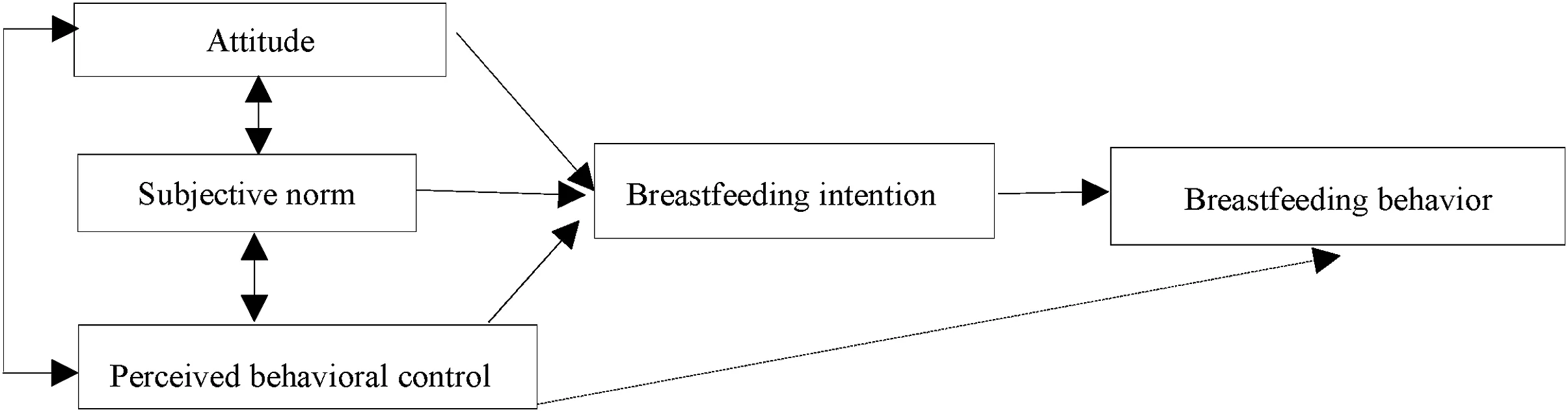
Fig.1.Theoretical framework of the theory of planned behavior in breastfeeding.
2.4.Intervention
After grouping,participants were randomly assigned to different rooms to avoid or reduce contamination between the control and intervention groups.The two groups’ allocation was“unbiased,”and the obstetrics department provided all routine postpartum maternity care.
Experienced clinical nurses and obstetric professionals also validated the intervention content to ensure suitability.Three experienced nurses in an obstetric unit delivered the TPB-based interventions.Before the study,three obstetric nurses were trained online and offline by breastfeeding professionals under the intervention protocol to ensure intervention consistency.The intervention protocol covers important theoretical content,intervention programs,communication skills,and confidentiality.The intervention integrated the breastfeeding promotion guidelines with the influencing factors based on the TPB framework [12,16].The following steps were implemented.
2.4.1.Establishing a positive attitude
The first period is the first day in the hospital before the Csection.We first introduced the program to the participants in the intervention group before their C-sections.A video was displayed for approximately 10-min participants to facilitate the educational process.The video was made by the researchers based on a previous study[12]and clinical experience.Three obstetric professionals validated the content of the video.The footage provided breastfeeding information,including why babies should be breastfed after C-section,application of an analgesic pump,effects of medication on breastfeeding,and care of the incision site.Besides,video images were designed to improve women and their families’understanding and learning of postoperative breastfeeding positions (focus on“biological nurturing”).Through face-to-face discussions,we encouraged participants to ask questions.
2.4.2.Providing supportive subjective norms
Next,on the day of the C-section,supportive subjective norms were promoted.We created supportive environments,encouraging significant family members to accompany the participants and becoming more confident in themselves.Family members were instructed to promote breastfeeding and help participants to achieve early skin contact and early sucking.Throughout the breastfeeding process,family members were involved,ensuring participants that they were not alone and had the support as needed.After returning to the postpartum unit,the primary nurse instructed family members to give the woman foot massages to relieve the pain and anxiety.This is a routine process on the postpartum team,encouraging family members to massage postpartum women’s feet for five min.Massage therapy was added to the common practice because massage can increase the patients’activity levels,increase their share in care,and reduce the patient’s anxiety [17].The therapy included petrissage (alternate fingers of both hands to do a slow,rhythmic pressing activity);kneading(squeeze the muscles and skin in hand,wringing and twisting and turning them alternately);and friction (rub with the palm or the last phalanx to create a displacement of the skin and deep layers).
2.4.3.Promoting perceived behavioral control
The third period (day 2-5 after C-sections) was designed to improve maternal behavioral control through latching-on and applicable breastfeeding positions.To ensure sustained support and education for mothers and babies at the bedside,a structured post-cesarean breastfeeding checklist was designed for nurses.The list was developed based on the“Mother-Infant Breastfeeding Progress Tool”[18].Several items were added,including pain,respect and support from caregivers,emotional stability of infant,infant defecation,and decrease in infant physiological weight.The checklist was used to assess required behaviors and skills for breastfeeding among women and infants after C-sections during hospitalization.Nurses considered maternal breastfeeding by observing the breastfeeding process,asked about specific items on the checklist,and then provided targeted guidance.
2.4.4.Strengthening transition from intention to actions
After discharge,we set up groups in WeChat,a social media platform widely used in China.The purpose of the groups was to strengthen postpartum women to transition from breastfeeding intention to action.The WeChat groups were used to consult and answer questions.Lactation consultants and trained obstetric nurses provided support and guidance in the WeChat group to manage different lactation problems,such as cracked/sore nipples,breast engorgement,or psychological support.The WeChat platform was used to release relevant knowledge twice a week,including breastfeeding videos from a global breastfeeding expert and breastfeeding articles recommended by lactation consultants.Mothers who had successfully breastfed after C-sections were invited to provide breastfeeding peer support to the participants.
2.4.5.Providing routine care to the participants in the control group
According to the Baby-Friendly Hospital Initiative’s requirements,the control group received current routine maintenance,including regular pre-and post-delivery care.During the pre-birth time at our hospital,women received prenatal breastfeeding education,during which nurses introduced knowledge of breastfeeding,including breastfeeding benefits,duration,and frequency.After delivery,nurses instruct early sucking,address breastfeeding issues,and provide clinic consultation or 24-h breastfeeding counseling hotlines after discharge.
2.5.Evaluation indicator
The exclusive breastfeeding rate was the primary outcome indicator for the results of this study.Our study’s exclusive breastfeeding means feeding infants only on mothers’ milk without supplementing other liquids or solid foods,except vitamins,minerals,and medicine.Another outcome indicator was breast problems,including sore nipples,cracked nipples,engorgement,and mastitis.
Also,data were collected through evaluation tools,including a demographic information questionnaire,modified Breastfeeding Attrition Prediction Tool(BAPT),and Numerical Rating Scale(NRS).
2.5.1.Demographics questionnaire
The demographic characteristics were collected through a researcher-designed questionnaire,including age,education,BMI,occupation,parity (primiparous/multiparous),and living region(urban/village),the causes of C-sections.
2.5.2.Numerical Rating Scale (NRS)
The NRS was applied to measure the intensity of postoperative pain.Babazade et al.’s [19]study found that every one-point increase in average pain score was associated with a 21%reduction in the odds of exclusive in-hospital breastfeeding relative to exclusive formula feeding.Therefore,the pain score was used as an indirect outcome indicator to evaluate breastfeeding behavior in this study.With 0-10 representing different degrees of pain,the NRS is an assessment scale in which 0 indicates no pain and ten means severe pain.The following questions will be asked:How powerful is your pain?Alternatively,the participants were asked to mark a number that best represented their level of pain.A score of 0 indicates no pain,1-3 indicates mild pain,4-7 indicates moderate pain,and 8-10 indicates severe pain.The reliability and validity of this pain measuring instrument have been previously confirmed [20].
2.5.3.Modified Breastfeeding Attrition Prediction Tool (BAPT)
We used the BAPT modified by Zhang et al.[21]to assess breastfeeding behavioral intention,attitude,subjective norms,and perceived behavioral control.The original version was developed by Janke [22].The modifications included deleting five items(family doctor,baby doctor,midwife,educator,and La Leche League) of breastfeeding subjective norm subscale and changing the response scale from a 6 to a 5-point scale.Behavioral intention for breastfeeding was measured using three dimensions related to individuals’ plans and intentions regarding future breastfeeding behaviors.This measure comprises attitudes(29 items),subjective norms (5 items),and perceived behavioral control (10 items).All questions in this section are rated on a five-point Likert scale ranging from“strongly agree”to“strongly disagree.”Attitude scores and perceived behavioral control scores were derived from the items’ sum,with higher scores indicating greater intention.Subjective norms regarding breastfeeding were measured using multiplication of normative belief and motivation to compliance measures.Cronbach’s α coefficient for the domains ranged from 0.81 to 0.92.
2.6.Data collection
Upon receiving consent to participate,participants were asked to complete a baseline questionnaire to determine demographics.Participants’ baseline measure of the modified breastfeeding attrition prediction tool was achieved for both groups.A study[23]suggested that women’s pain score was the highest within 24 h after C-sections,so the present study collected the frequency of formula supplementation and pain scores at 24 h postoperatively.The breastfeeding rate and frequency of breastfeeding problems were collected five days post-operation;participants in both groups were surveyed again on infants’ feeding options and modified breastfeeding attrition prediction scores at two weeks and one month after delivery.A nursing graduate student collected the data,and the post-discharge data were collected via the WeChat group in the form of electronic questionnaires.
2.7.Data analysis
The Shapiro-Wilk test was used to examine the normal distribution of the data.Participants’ demographics were described as the mean,median (interquartile range),or percentage.Categorical data were compared and statistically analyzed using the chi-square test or Fisher’s exact test.Continuous data were statistically analyzed using the independent-samples t-test or Mann-Whitney U test.The primary data were examined using intention-to-treat analysis.Repeated-measures analysis of variance (ANOVA) was applied with a change from baseline as the dependent variable,intervention,time,and the intervention multiplied by time interaction as independent variables.Mauchly’s sphericity test was used to examine the compound symmetry assumption.Data were analyzed using SPSS version 22,and P <0.05 was regarded as statistically significant.
3.Results
In total,132 women who met the inclusion criteria and agreed to participate were successfully allocated into the two groups.In Fig.2,reasons for dropout from the study are displayed in the Consolidated Standards of Reporting Trials (CONSORT).To avoid breaking the balance between the two groups,all participants participating in the random allocation should be included in the data analysis.Participants lost to follow-up were entered into the intention-to-treat study.Data of the lost follow-up were collected from the last measurement.
3.1.Baseline characteristics
The age range of our participants was from 24 to 43.The mean ages of mothers in the intervention and control groups were 32.48 ± 3.73 and 32.15 ± 4.07,respectively.The majority was primiparous (83.3% vs.75.8%).In the intervention (control) group,more than 19.7% (22.7%) of participants were unemployed,and 74.2% (74.2%) lived in urban centers.There were no significant differences between the two groups at baseline (Table 1).
3.2.Exclusive breastfeeding
Comparison of the two groups in terms of behavioral intentions of exclusive breastfeeding showed no statistically significant variation between the two groups during the prenatal period(86.4%vs.84.8%,P=0.804,Table 1).Within 24 h after C-section,the Mann-Whitney U test showed that the average frequencies of the formula supplement of the two groups were significantly different(P <0.05;Table 2).The results of the intention-to-treat analysis showed that participants in the intervention group presented substantially higher rates of exclusive breastfeeding than controls at five days(86.4%vs.60.6%),two weeks(77.3%vs.57.6%),and one month(74.2%vs.50.0%)follow-up periods(Table 2).After the TPBbased intervention,17 (25.8%) participants in the intervention group and 33 (50.0%) participants in the control group stopped breastfeeding within a month.
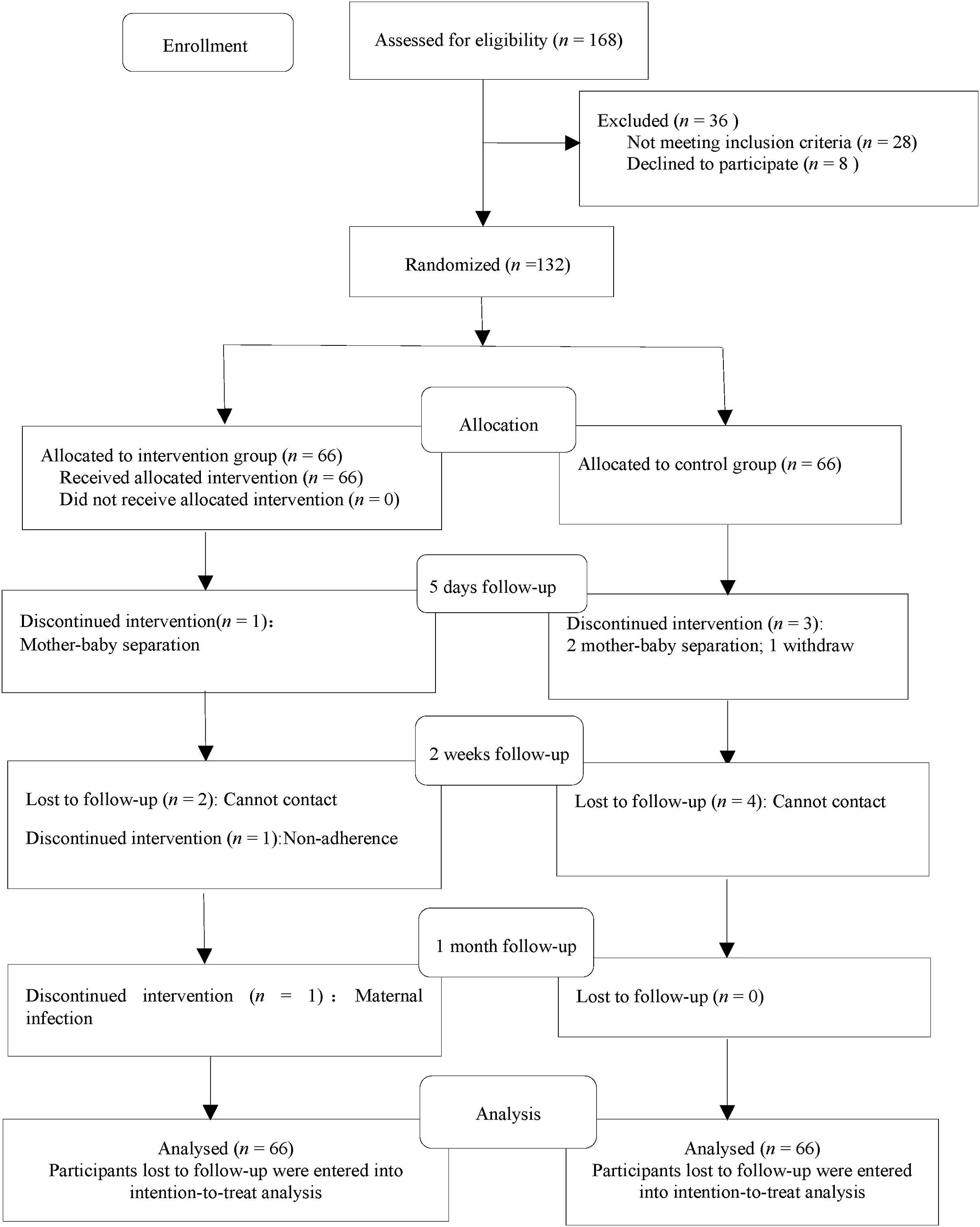
Fig.2.Flow diagram of participants.
3.3.Breast problem outcomes
Similar to the exclusive breastfeeding rate,the TPB-based intervention benefit was validated by the outcome.The intervention group was less likely to have sore nipples on five days(6.1%vs.18.2% in the control group,P<0.05) and two weeks (9.1%vs.12.1%in the control group,P<0.05).However,there were no statistically significant differences in cracked nipples and breast engorgement between the two groups.No case of mastitis in the intervention group was reported,and only one mastitis case was reported in the control group(Table 2).
3.4.Pain score
Table 2 shows the mean values of the NRS parameters of the two groups.The control group’s average pain scores were higher than those in the intervention group,but there was no statistically significant difference between the two groups(t=0.48,P >0.05).
3.5.Outcome of breastfeeding attrition prediction
The TPB variables were also compared across study groups at baseline.No significant differences could be observed in the mean scores of breastfeeding attitude,subjective norms,and perceived behavioral control between the two groups at baseline (P >0.05).Table 3 shows the means and standard deviations of three TPB variables across three measurements(antepartum,two weeks,and one month) in the intervention and control groups.
3.5.1.Attitude to breastfeeding
Participants who received TPB-based intervention had significantly higher scores on attitude scores at one month than the control group (P <0.05).The repeated-measures ANOVA test results showed that the time effect was statistically significant(F=155.92,P=0.000),with the intervention group’s scores being lower at the beginning and then increasing rapidly over time.Attitude scores dropped in both groups at one month.There was also a statistically significant group effect (F=10.33,P=0.002),indicating the difference between the two groups at different periods.The intervention group’s attitude scores were better than that of the control group(P <0.05),and the effect was the best after two weeks,followed by one month after the intervention.The groups are represented by nonparallel lines,which increase over time and gradually move away from each other(interaction effect)(F=6.32,P=0.004).
3.5.2.Subjective norm
There was a statistically significant time trend for scores of subjective norms(F=3.56,P=0.033).The general direction of the two groups’personal criteria scores increased firstly after declining.The group effect results showed that the difference was statistically significant based on repeated-measures ANOVA (F=4.57,P=0.035).There was a substantial difference in the subjective norms scores,indicating that the intervention group’s averageemotional norm scores were higher than those in the control group.The intervention group’s increased slope was greater than that of the control group,but this difference was not statistically significant (no interaction effect) (F=1.20,P=0.302).
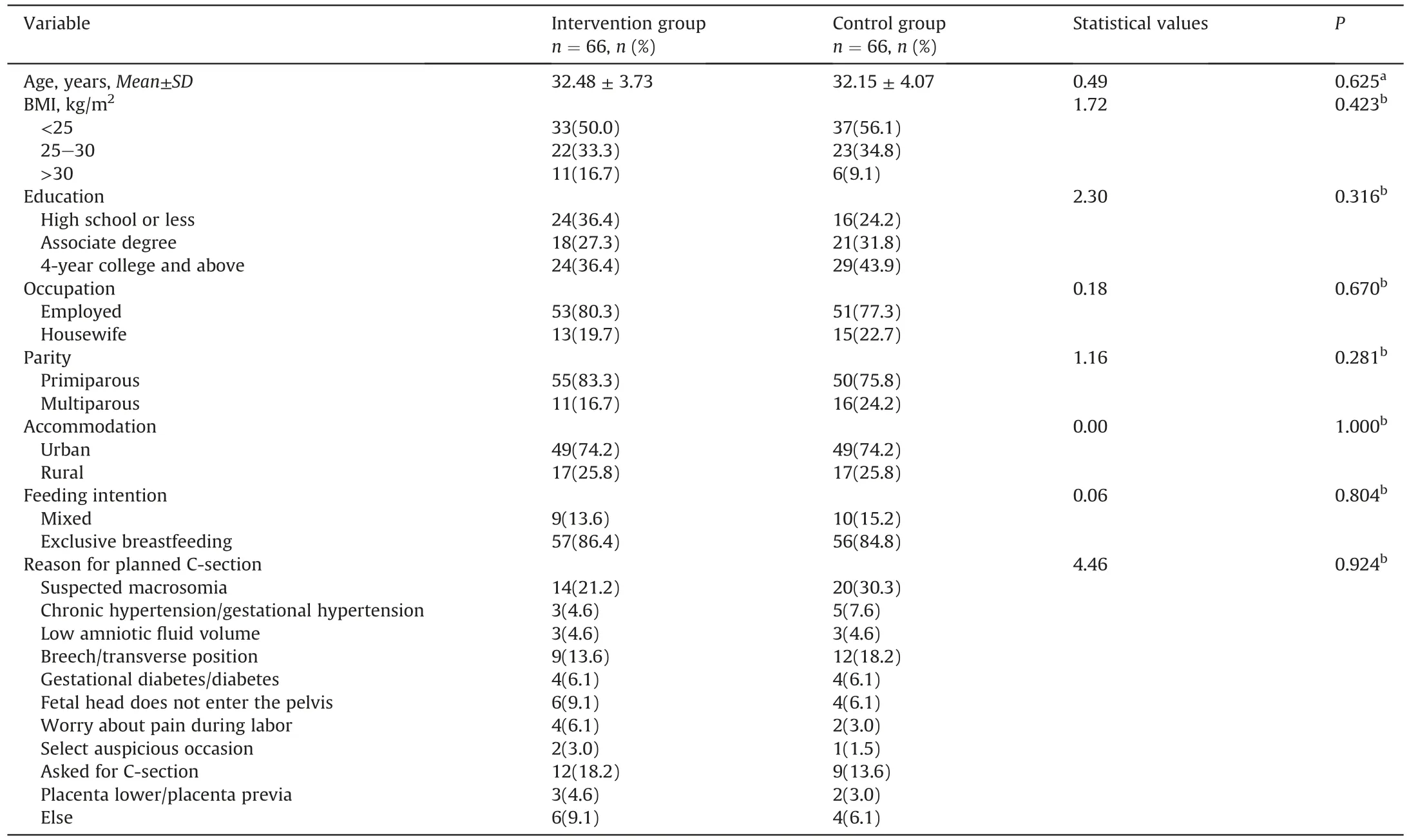
Table 1 Baseline characteristics of participant.
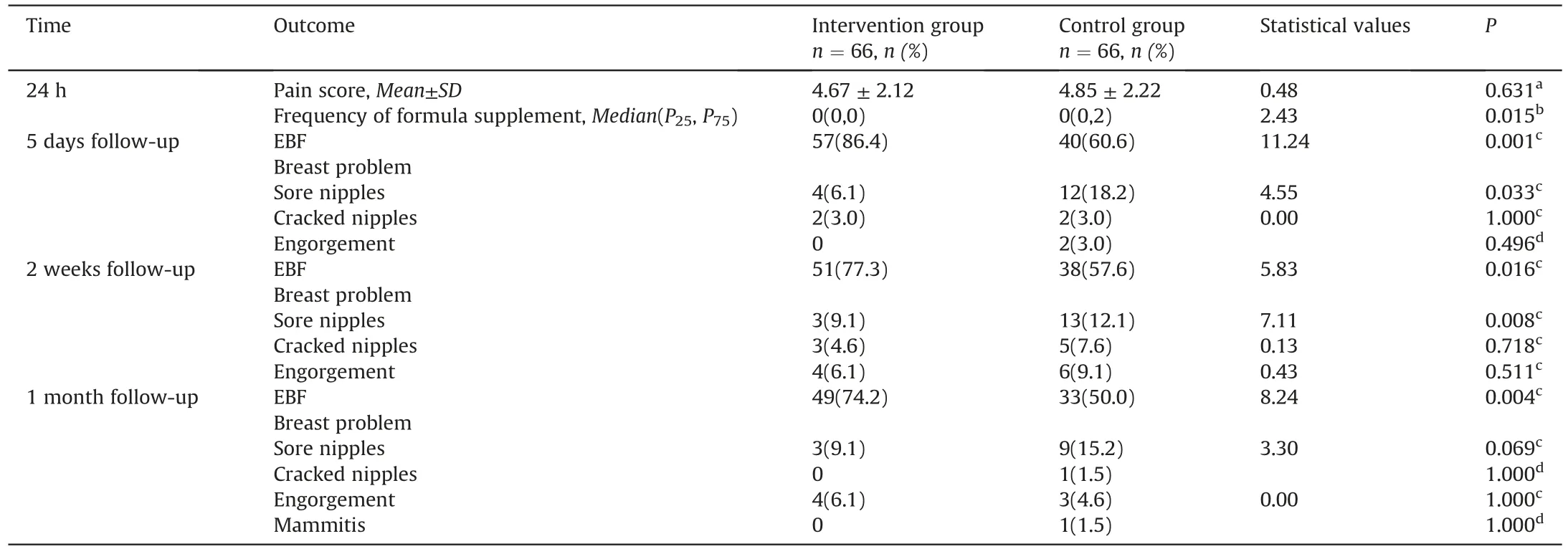
Table 2 Crude analysis of pain score and relevant breastfeeding outcomes.
3.5.3.Perceived behavioral control
The mean scores of perceived behavioral control one month after C-section in the intervention and control groups were 39.15±4.69 and 43.13±5.02,respectively,indicating a significant difference between the two groups (P <0.05).The time effect results showed that the difference was statistically significant(F=9.22,P=0.000),indicating that the mean perceived behavioral control scores of the TPB-based intervention in the two groups were higher than the mean scores of the controls at baseline.There was an upward trend over time.The intervention group’s perceived behavioral control scores were better than those in the control group,and there was a statistically significant difference between the two groups (F=8.53,P=0.004).The intervention group’s increasing slope was greater than that of the control group,suggesting that the intergroup and intragroup interactions also significantly affected breastfeeding behavioral control (F=3.71,P=0.027).
4.Discussion
The present study provided valuable interventions over four periods about behavior change factors(attitude,subjective norms,perceived behavioral control,and behavioral intention) that promote women’s breastfeeding behaviors after C-sections.This study builds on existing theories and further demonstrates the positive effects of continuous support from the hospital and extending to the home setting.In our research,the intervention-based TPB led to an improved exclusive breastfeeding rate,a high mean score for each TPB variable,and reduced lactation-related sore nipples.
In our study,the exclusive breastfeeding rate was 74.2% in the intervention group and 50%in the control group at the end of one month.In general,the intervention could provide support to those women after C-section experiencing breastfeeding problems,as they were more likely to master relevant knowledge and skills.The breastfeeding results obtained from this study are consistent with those drawn from previous studies.Another study focused on determining the effect of TPB-based intervention on maternal breastfeeding outcomes in primiparous mothers[23].The exclusive breastfeeding rates increased from 40.13% to 57.32% after breastfeeding intervention at six weeks [21].
The breastfeeding posture might be one of the important reasons accounting for breast problems [24].The biological nurturing approach reduced breast problems through the more comfortable latch,facilitating the exclusive breastfeeding initiation[25].In this study,the results confirmed that the intervention did reduce sore nipples,and the intervention group was less likely to have sore nipples for five days and two weeks (P <0.05).There was not enough evidence that the intervention reduced cracked nipples,engorgement,or mastitis.This study’s results were not consistent with the study mentioned above [25],perhaps because of the different maternal groups and other study designs.
Additionally,as an effective nursing intervention presenting no side effects,foot massage can help manage post-cesarean pain and stress[16].A previous study demonstrated a significant association between an increase in post-cesarean pain scores and deterioration of breastfeeding initiation[20].Our study attempted to relieve the postpartum incision pain and uterus systole and evaluate indicators of breastfeeding behaviors based on pain scores.However,there were no statistically significant pain score differences.Measuring perceived pain may not be sufficient to examine the influence of the breastfeeding intervention.We speculated that the possible reason for this result was that performing massage only once might not be enough [26].Effective complementary therapies and nonmedical painkillers are explored in the future to help women reduce the pain that negatively affects breastfeeding after C-sections.
Attitude is regarded as the determinant of actual and potential actions.Participants in this study were educated through a video in the hospital and received WeChat counseling after discharge.This intervention aimed to inform participants and their families about the necessity and feasibility of breastfeeding after C-sections to generate a positive breastfeeding attitude.In our study,the women’s mean attitude scores after C-section at one month were lower than that measured at the end of 2 weeks,suggesting the existence of certain limitations in transferring breastfeeding knowledge through the WeChat platform.This result indicated that breastfeeding education should be strengthened one month after delivery,and face-to-face guidance should be consummated by community health services and breastfeeding consultation clinics.
The TPB-based intervention increased the mean scores of subjective norms in the intervention group from baseline to follow-up.Women’s preference for infant feeding is closely related to their significant others’ wishes,especially women’s husbands and mother-in-law/mother [27].In this study,family members were involved in the breastfeeding process,making women feel the support for breastfeeding.Besides,with the professional backing from medical staff,societal pressures to breastfeed will be significantly reduced,thus facilitating breastfeeding behaviors.However,subjective normative scores of breastfeeding had a lower mean score at the end of 1 month than that at the end of 2 weeks.We suspected that this result was due to a lack of continuous guidance for maternal support systems(especially for family members)afterdischarge,which we posited would influence their subjective norms.Although there are data about the importance of support in women’s families and the working environment that can affect decision-feeding,a lack of studies has explored the influence of norms within other possible social environments on breastfeeding.
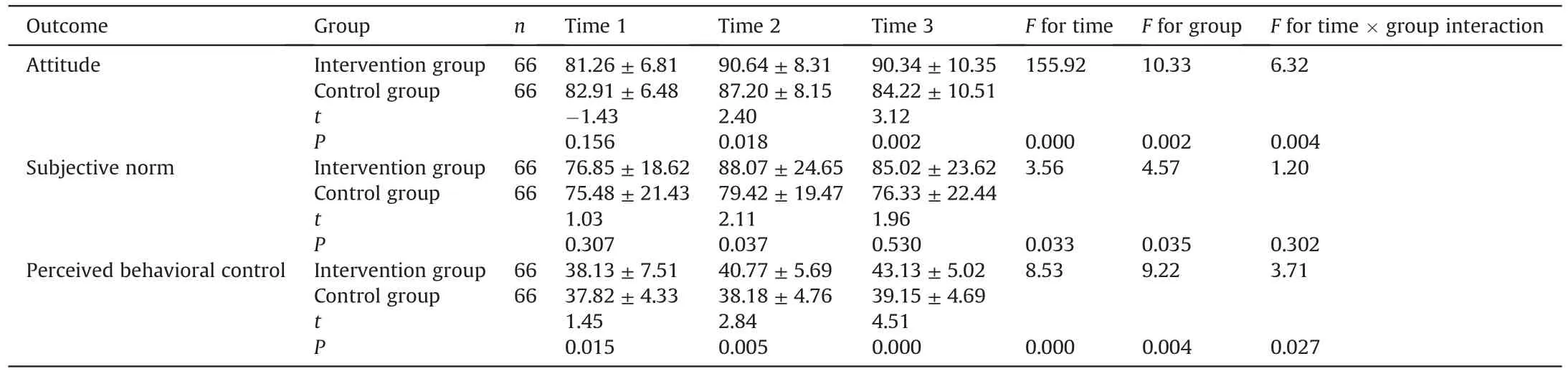
Table 3 Comparison scores of three variables before and after intervention(Mean ± SD).
Perceived behavioral control refers to the degree to which people feel that they have voluntary control over their behavior.The lack of comfortable breastfeeding skills and coping skills in managing their depressive mood were significant obstacles for breastfeeding after cesarean delivery [10].Ensuring that mothers are physically and psychologically comfortable is an essential strategy for breastfeeding.Women in the intervention groups were fostered with knowledge enhancement and were provided breastfeeding postural guidance and psychological support.In this study,the intervention group’s exclusive breastfeeding rate was higher than in the control group;therefore,the mean score of perceived behavioral control increased.Our findings also agree with a previous study reporting improved exclusive breastfeeding when interventions were delivered during both prenatal and postnatal periods,which increased behavioral control [23].
In addition to improving strategies for successful breastfeeding after cesarean delivery,reducing the C-section rate without medical instructions positively impacts breastfeeding outcomes.Elective cesarean delivery should be avoided,and mothers should be informed of the potential effects of elective cesarean delivery on feeding practices.Women who choose to give birth by elective cesarean delivery may have lower breastfeeding intentions because they may be less comfortable with biologically normal childbirth processes and breastfeeding [28].When C-section is unavoidable,adequate support should be provided.
5.Limitations
The study had some limitations.First,with participants staying in the same obstetrics department,the possibility of contamination lingered in the control group.Furthermore,the single-center intervention made it impossible to generalize the findings.Future intervention studies of this type should consider a multicenter method.
6.Conclusions
The TPB-based intervention demonstrated a positive effect on promoting exclusive breastfeeding rates,breastfeeding behavioral intention,and sore nipples among women undergoing C-sections.However,the impact of the intervention on breastfeeding attitudes and subjective norms increased firstly after declining.Further research is needed to explore practical measures to maintain breastfeeding behavioral intention upward trend over time.
CRediT authorship contribution statement
Juan Wen:Conceptualization,Data curation,Methodology,Writing -original draft,Writing -review &editing.Guiling Yu:Conceptualization,Methodology,Writing -review &editing.Yan Kong:Conceptualization,Data curation,Methodology,Writing -review &editing.Holly Wei:Methodology,Writing -review &editing.Shuran Zhao:Data curation,Methodology.Furong Liu:Conceptualization,Methodology,Writing -review &editing.
Declaration of competing interest
The authors declare that they have no competing interests.
Acknowledgement
We thank all the mothers who participated in this study.We want to acknowledge the authors of both the Chinese version and the original tool development authors for their contributions.
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2021.03.012.
杂志排行
International Journal of Nursing Sciences的其它文章
- Lived experiences of the disease journey among patients with idiopathic pulmonary fibrosis
- Supplement to the published paper“Theory-guided interventions for Chinese patients to adapt to heart failure:A quasi-experimental study”
- Using action research to evaluate a nursing orientation program in a multicultural acute healthcare setting
- Associations between risk factors for cardiovascular diseases and frailty among community-dwelling older adults in Lanzhou,China
- Examining advanced nursing practice in Hong Kong and Guangzhou
- Persistent effect of nurse-led education on self-care behavior and disease knowledge in heart failure patients
