Associations between risk factors for cardiovascular diseases and frailty among community-dwelling older adults in Lanzhou,China
2021-05-19YnhongWngHnWiYngHonghnZhngJingZhngHihuiRunNnTngJingjingRnXiSunChunrongLiLinHn
Ynhong Wng ,H-R Hn ,Wi Yng ,Honghn Zhng ,Jing Zhng ,Hihui Run ,Nn Tng ,Jingjing Rn ,Xi Sun ,Chunrong Li ,Lin Hn ,*
aSchool of Nursing,Lanzhou University,Lanzhou,China
bSchool of Nursing,Johns Hopkins University,Maryland,USA
cGastroenterology Department,The First Hospital of Lanzhou University,Lanzhou,China
dCommunity Health Services Center of Tuanjiexincun,Lanzhou,China
eCommunity Health Services Center of Jiaojiawan,Lanzhou,China
ABSTRACT Objectives:To examine the relationship between cardiovascular disease risk factors and frailty in a sample of older Chinese adults.Methods:A total of 458 community-dwelling older adults (≥65 years) in Lanzhou,Gansu Province of China participated in a cross-sectional survey.Their status was evaluated in terms of frailty phenotype(unintentional weight loss,exhaustion,low activity levels,slowness and weakness).Participants were categorized as not frail,prefrail or frail.Cardiovascular disease risk factors that were assessed included:blood pressure,body mass index,waist circumference,blood glucose,total cholesterol,triglycerides,lowdensity lipoproteins and high-density lipoproteins.Results:Individuals with obesity had an increased risk of prefrailty (OR:2.26;95% CI:1.05,4.84).Hypertension was inversely associated with frailty among the participants(OR:0.31;95%CI:0.11,0.87)after adjusting for covariates.Conclusions:The findings suggest that much more attention should be paid to weight control of the elderly in the community for preventing them from transition to prefrailty or frailty.Active prevention and control of cardiovascular diseases among the community-dwelling elder are still of great importance.
Keywords:Aged Cardiovascular disease China Community health centers Frailty Risk factors
What is known?
· Frailty has become increasingly relevant in the field of cardiovascular medicine and can even increase the mortality rate of cardiovascular diseases.
· The pathophysiology underlying the relationship between cardiovascular disease risk factors and frailty relates to shared common conditions such as chronic inflammation and insulin resistance.
What is new?
· Chinese older adults with obesity had an increased risk of prefrailty which indicate that future intervention should address weight control among prefrail older adults as a targeted strategy to prevent or delay the transition to frailty.
· Hypertension was inversely associated with frailty among the participants of the present study.
1.Introduction
The world’s population has grown rapidly over the past 60 years.Between 2015 and 2050,it has been projected that the proportion of individuals aged 60 or over will almost double from 12% to 22%(or 2 billion)[1].China has experienced one of the largest increases in its population of older adults.According to the National Bureau of Statistics of China,the population aged 65 and over increased from 109 million in 2008 to 150 million in 2017 [2].This dramatic increase in China’s older population over a short period of time has caused a significant burden on the country’s public health and social economy,particularly in relation to frailty associated with aging.Frailty is characterized by decreased physiological reserves and increased vulnerability to stressors due to impairments in multiple,inter-related systems,such as the brain,endocrine system,immune system and skeletal muscle [3,4],resulting in an increased risk of falls (OR:1.84;95% CI:1.43-2.38) [5],functional disability (OR:2.76;95% CI:2.23-3.44) [6],hospitalization (OR:1.26;95%CI:1.18-1.33)[7]and even death[8,9].For example,using the Fried frailty criteria(unintentional weight loss,exhaustion,low activity levels,slowness and weakness),Crow et al.followed 4,984 community-dwelling older adults in the United States (mean age:71.1 years,44% male) for 8 years and found that the prefrail(meeting one or two criteria) and frail (three or more criteria) individuals had a greater risk of death (hazard ratio,HR:1.64 and 2.79,respectively) [8].Frailty is also economically burdensome.A cross-sectional study of 2,598 older adults (mean age:69.6 years,48.5%male)in Germany demonstrated that the difference in mean total 3-month healthcare costs between frail and non-frail participants amounted to $2,100;P <0.05 (four or five symptoms) and$750;P <0.05(three symptoms)after controlling for comorbidities and general socio-demographic characteristics in multiple regression models [10].These findings underscore the importance of understanding factors associated with frailty in order to minimize or delay the development of frailty among older adults.
The findings of existing research indicated that risk factors for cardiovascular disease are predictors of frailty [11,12].The pathophysiology underlying the relationship between cardiovascular disease risk factors and frailty relates to shared common conditions such as chronic inflammation and insulin resistance.Specifically,chronic inflammation,which plays a central role in the oxidation of lipoproteins and activation of plaques in cardiovascular disease,results in the redistribution of amino acids from skeletal muscle to other organ systems [13].Insulin resistance leads to impaired muscle protein breakdown,which in turn leads to reduced availability of amino acids for maintenance and repair functions [13].Hence,both inflammation and insulin resistance can result in a profound loss of muscle mass,a key component of frailty [4].
Several studies have examined the relationship between cardiovascular disease risk scores and frailty.For example,data from two longitudinal studies (n=1,726;mean age:71.6 years,43.0%male and n=3,895;mean age:55.2 years,73.4% male,respectively),both conducted in the UK,demonstrated that cardiovascular disease risk scores predicted risks of developing frailty 4 and 10 years later,respectively[11,12].In order to examine the association between specific cardiovascular disease risk factors and frailty,Ramsay et al.surveyed 1,622 British men(mean age:79 years)and found that a range of cardiovascular disease risk factors (e.g.obesity,high-density lipoproteins,hypertension) was associated with an increased risk of frailty [14].Thus,previous research has described cardiovascular disease risk profiles in relation to frailty among older adults.Little is known about whether an adverse cardiovascular risk profile exists in prefrail older adults.An average 4.4-year follow-up study of 1,567 Italians aged 65-96 years suggested that prefrailty was an independent risk factor for predicting the development of cardiovascular disease in the elderly [15].However,the mechanism by which the risk factors of cardiovascular disease affect the occurrence of prefrailty has not been well addressed in the literature,yet it is reversible and can be prevented[16].Interventions such as cardiac rehabilitation,physical exercise,vitamin D supplementation,increasing protein intake and reduction of unnecessary drugs can delay the progression of frailty and even transferred the frail status to prefrailty or non-frailty [17].A better understanding of the cardiovascular risk profile,particularly in relation to prefrailty,may enable researchers and clinicians to develop targeted strategies for preventing or delaying frailty among older adults.Therefore,the aim of this study was to examine cardiovascular disease risk factors in association with frailty status among community-dwelling older Chinese adults.
2.Methods
2.1.Setting and study population
This investigation was a descriptive correlational study.From July 2017 to July 2018,the community-dwelling elderly individuals,who living in the local area for one year or more,were recruited from two community hospitals in Lanzhou,a city in North-West China.The community hospitals served five communities and provided primary health care for almost 150,000 people.All the elderly individuals (aged 65 and over) in the communities were asked for annual physical examination.Potential participants were approached by trained research assistants when they visited the community hospitals for their annual physical examinations.Individuals with hearing or visual impairments affecting daily activity,dementia (Mini-Mental Status Examination,MMSE <15),functional impairment(Barthel Index ≤35),those with a history of schizophrenia or bipolar disorder or those who had a terminal illness such as end-stage cancer,were excluded.The required sample size to demonstrate significant differences was estimated by the following formula [18]:
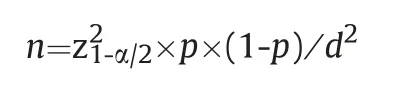
Here z1-α/2 is the standard normal variate for a 5% type I error(P <0.05).Based on a prior study,the proportion of adults who were prefrail in a community-dwelling Chinese population was 46%[19].The calculation suggested an approximate sample size of 381 subjects,thus with a 25%dropout rate,476 subjects were required.Eighteen participants were excluded from the study for the following reasons:two had severe hearing impairment,one had dementia (MMSE<15),ten had missing or incomplete data related to frailty criteria and five older adults refused to participate.In the end,458 participants remained in the study,with a response rate of 96.2%.
The ethics committee of Lanzhou University approved the study protocol.The two community hospitals agreed on the data collection and all participants provided informed consent.
2.2.Measurements
2.2.1.Demographic data
A study questionnaire was used to collect information on sociodemographics (e.g.,age,gender,education),health behavior (e.g.,drinking,smoking) and medical characteristics (e.g.,self-reported hypertension,diabetes or other forms of health condition,such as angina or myocardial infarction,stroke/transient ischemic attack,peripheral artery disease,chronic obstructive pulmonary disease or cancer) via face-to-face interviews.Data on the usage of antihypertensive,anti-diabetic or cholesterol-lowering medication were also self-reported.
2.2.2.Frailty phenotype
Frailty phenotype was used to assess frailty status using five criteria:unintentional weight loss,exhaustion,low activity level,slowness and weakness [3].Participants were classified as frail if they met three or more of the five criteria,prefrail if they met one or two,or as not frail if they met none of the criteria [3].Unintentional weight loss (i.e.,not due to dieting or exercise) was assessed by self-reporting and defined as weight loss of more than 3 kg,or greater than 5% of body weight in the previous year.The original criteria [3]used 4.5 kg as a threshold.This definition was modified in this study,using 3 kg instead to adjust for the smaller body size of the East Asian population.Exhaustion was identified when the participant,in at least 3 days of the previous week,could agree with either of the two following statements from the Center for Epidemiologic Studies Depression Scale (CES-D):“I felt that everything I did was an effort.”or“I could not get going.”Activity level was assessed using the short version of the International Physical Activity Questionnaire(IPAQ)which asks about the level of exercise in the previous week and the number of minutes dedicated to each activity.The metabolic equivalent (MET) was then calculated for each activity [20]and calories expended based on these METs[21].Participants were classified as being low activity if their weekly energy expenditure for activities ≥2METs was less than 1,600 kJ for men and 1,130 kJ for women[3].Slowness was assessed by the time required to walk 5 m at their usual pace,measured three times,and confirmed if the mean value was below the threshold specified by the subject’s sex and height,as suggested by Fried et al.[3].Finally,weakness was determined from three measurements of handgrip strength of the dominant hand with confirmation of weakness if the mean value was below the specific thresholds for gender and body mass index (BMI) suggested by Fried et al.[3].
2.2.3.Anthropometric measurements
In addition,anthropometric characteristics were measured by trained research assistants.These included weight,height,waist circumference(WC),and systolic and diastolic blood pressure(SBP and DBP,respectively).The weight of participants was measured barefoot,preferably fasted and with an empty bladder.Height was measured without shoes using a stadiometer and rounded down to the nearest cm.BMIwas calculated as weight(in kg)/height squared(in m2) [22].WC was measured from the mid-point between the highest point of the iliac crest and the lowest part of the costal margin in the mid-axillary line.Blood pressure was measured in the right arm with a validated mercury sphygmomanometer after the participant had rested quietly for >5 min in a seated position and without caffeine,exercise or smoking for at least 30 min.The mean of three measurements of all the parameters above was used in the analysis.
2.2.4.Blood measurements
Blood samples were obtained for biochemical tests following an overnight fast.Serum samples were stored frozen at -80°C until required for analysis.Total cholesterol(TC),triglycerides(TG),lowdensity lipoprotein cholesterol (LDL-C) and high-density lipoprotein cholesterol(HDL-C)were estimated using enzymatic methods.
2.2.5.Covariates
Cognitive function was assessed using a 30-question MMSE.The threshold for those who were illiterate was ≤17 [23].Functional ability was assessed based on the capacity of individuals to perform instrumental activities of daily living (IADL),involving more complex tasks such as financial and medication management,driving,shopping,house cleaning and meal preparation [24].Depressive symptoms were assessed through the Geriatric Depression Scale(GDS)with a score >6 indicating the presence of clinically-relevant depressive symptoms[25].The Mini Nutritional Assessment(MNA)has been applied to rapidly assess nutritional status in older individuals.Scores between 17.0 and 23.5 identify those at risk of malnutrition [26].
2.3.Statistical analysis
Study variables were summarized using means,standard deviations and frequencies.Comparisons of variables between groups were conducted using a chi-square test or Fisher’s exact test for categorical variables and analysis of variance for continuous variables.Logarithmic transformation was used for data with a skewed distribution.Multinomial logistic regression was performed to estimate covariance adjusted OR and 95% CI,according to categories of frailty,with“non-frail”as the reference group.Covariates considered in the regression analysis included age,sex,average monthly household income,education,drinking,smoking and the usage of antihypertensive,antidiabetic or cholesterol-lowering medication.In addition,cognitive status,depression,functional status and nutritional status were also included in the model as covariates as they have been previously associated with frailty[27,28].All statistical analyses were performed using SPSS 19.0(SPSS,Inc.,Chicago,IL,USA),with the level of significance established at 5% for two tails.
3.Results
3.1.The characteristics of the study participants
Table 1 summarizes the characteristics of the study participants according to frail phenotype.The prevalence of not frail,prefrail,and frail status was 30.8%(141/458),60.0%(275/458)and 9.2%(42/458),respectively.Frail individuals tended to be older than prefail or non-frail ones (P <0.05).Frail individuals were less educated compared with the other groups (P <0.05).Frail older adults tended to have a higher percentage of using antihypertensive and cholesterol-lowering medication compared with those that were not frail (P <0.05).Additionally,frail individuals exhibited significantly lower functional and cognitive ability,poorer nutrition and higher depressive symptom scores than non-frail and prefrail individuals (P <0.05).
3.2.Association of cardiovascular disease risk factors with frailty status
Table 2 presents the cardiovascular disease risk factors in the three groups of participants.Overall,the prevalence of cardiovascular disease risk factors observed in the groups was not different except for total cholesterol.Prefrail individuals had a significantly higher level of total cholesterol compared with non-frail individuals (P <0.05).
Table 3 displays the association of each risk factor for cardiovascular disease with frailty status in the study participants using Chinese-specific threshold values for BMI,WC [29],lipid profile[30]and blood pressure [31-33].Hypertension was inversely associated with frailty status,even after adjusting for study covariates.Specifically,Chinese older adults with hypertension had odds of experiencing frailty 69%lower(OR:0.31;95%CI:0.11-0.87)than their non-frail counterparts.In addition,obese individuals(BMI ≥28 kg/m2)were more than two times as likely to experience prefrailty(OR:2.26;95%CI:1.05-4.84)than those with normal BMI after controlling for all covariates.
4.Discussion
By examining the relationship between cardiovascular disease risk profile and frailty,the current study offers further insights into the association of each cardiovascular disease risk factor with frailty status in community-dwelling older adults in China.We found that obese Chinese older adults were at increased risk of prefrailty,whereas hypertension was associated with a lower risk for frailty.
The prevalence rate for frailty was 9.2% in the present study.A survey on older adults in 8 communities in Beijing(n=683;mean age:74.1 years,17.1%male),found that the prevalence of frailty was 11.1%[19].Similarly,a systemic review of studies revealed that the prevalence of frailty was 9.9% (95% CI:9.6-10.2;15 studies with 44,894 participants) [34].Different operational dimensions of the frailty phenotypes identified by Fried could explain variations in the estimated prevalence of frailty.We used the short version of the IPAQ to measure the physical activity of older individuals,because the activities in the Minnesota Leisure Time Activity Questionnaire included mowing the lawn,raking,gardening,bowling and golf,etc.,activities which are unpopular in China[3],therefore the IPAQ was more suitable for the Asian population [35].Additionally,the prevalence rate for prefrailty was 60.0% in our study which was relatively higher compared with a study of Xi et al.(the prevalence of prefrailty of 45.7%) [19].For the participants of the study were more than 60 years old,younger than our study,which might contribute to the inconsistency [19].
4.1.Obesity and prefrailty
Obesity was associated with increased odds for prefrailty in the study sample,with this trend also being observed in the frail group,although the relationship was not statistically significant.Similarly,Ferriolli et al.investigated 5,638 Brazilian older adults (mean age:73.1 years,34.8% male),finding that obese older individuals presented a higher risk of prefrailty (OR:1.29;95% CI:1.09-1.51).However,they failed to find a relationship between obesity and frailty [24].Population-based cohort studies have also demonstrated an association between higher BMI and frailty status[36,37].Researchers from Finland investigated 1,815 initially healthy men (mean age:47 years) in 1974.After a 26-year followup in 2000 they surveyed the survivors (n=1,125) and found that compared with those of normal weight,the development of frailty was significantly higher among those who were overweight or obese in midlife,with fully adjusted ORs (95% CIs) of 2.06(1.21-3.52) and 5.41 (1.94-15.1),respectively.Even the development of prefrailty increased significantly when participants had been overweight (OR:1.39;95% CI:1.03-1.87) or obese (OR:2.96;95% CI:1.49-5.88) in midlife [37].A physiological explanation of this association may be that among individuals with obesity,excess visceral fat produces pro-inflammatory cytokines and is infiltrated by macrophages,lymphocytes and monocytes which are able to produce additional inflammatory compounds that probably appear in the circulation[38].Higher levels of inflammatory markers in the blood are associated with a greater loss of muscle mass and strength,accelerated loss of mobility,lower-extremity performance and physical activity and depression in older individuals,all essential parameters that define frailty on the basis of the Fried frailty criteria [38].In addition,we did not find an association between being underweight and frailty,which was inconsistent with other studies [39].The difference might pertain to the small proportion of underweight older adults (11/458,2.4%) in our population.However,further epidemiological studies with a larger sample size are required to explore the relationship between being underweight and frailty because weight loss has been proposed as one of the five criteria of the frailty phenotype[3].It is associated with sarcopenia,a particularly deleterious condition that is associated with low muscle mass and lack of strength.
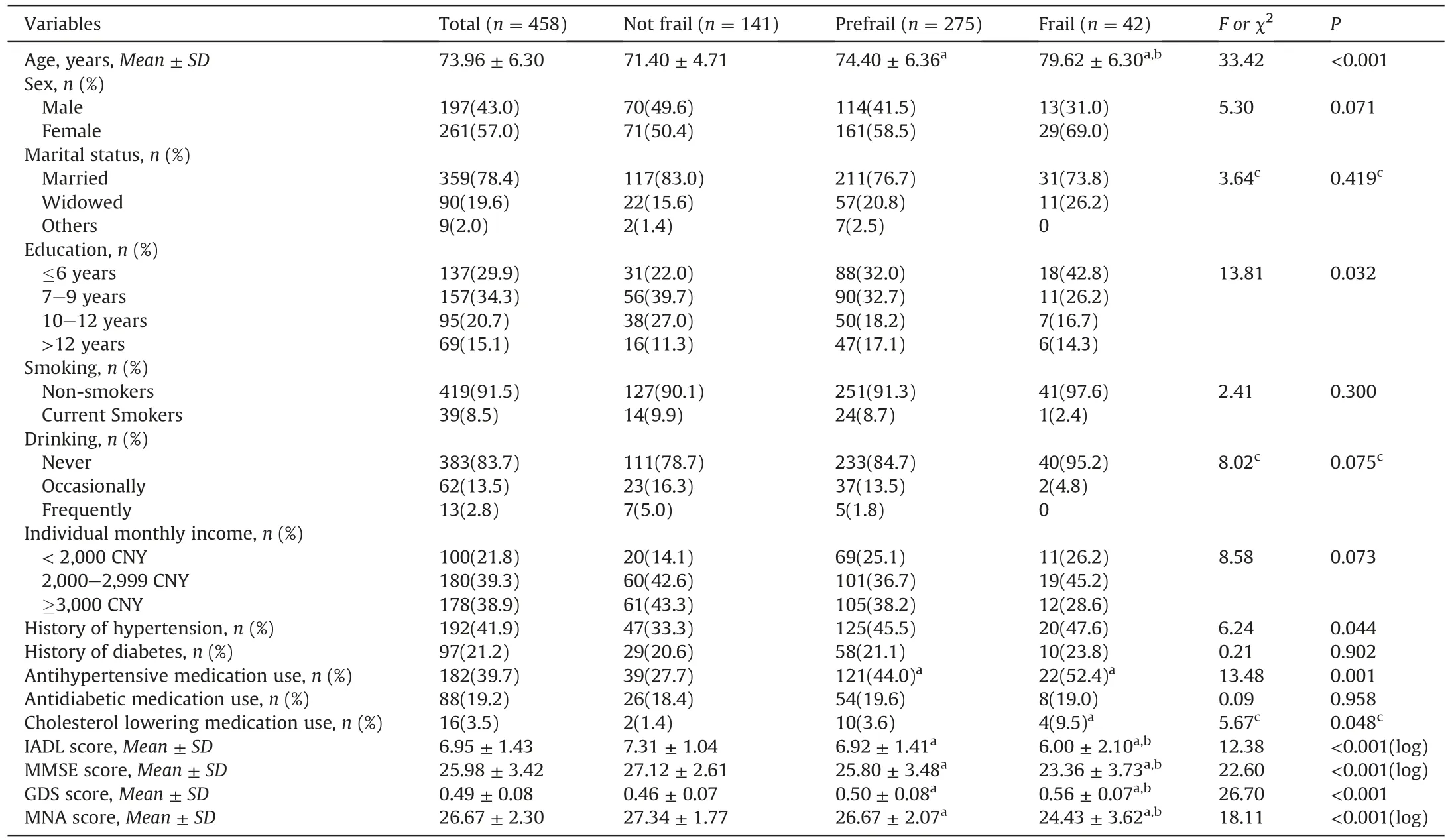
Table 1 Participant characteristics stratified by Fried phenotype in 458 Chinese older adults aged 65-94 years.
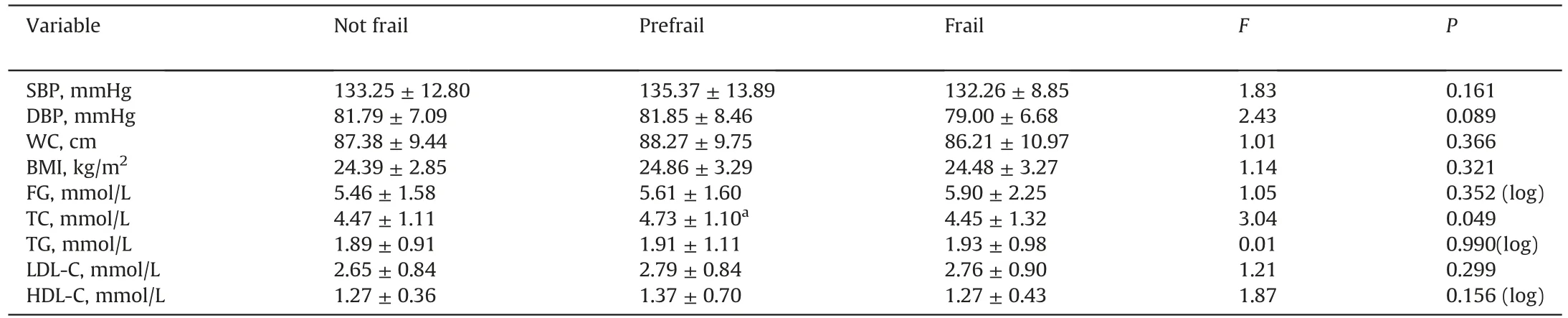
Table 2 Cardiovascular disease risk factors stratified by Fried phenotype in 458 Chinese older adults aged 65-94 years (Mean ± SD).
4.2.Waist circumference and frailty status
A number of authors have observed that the accumulation of abdominal fat,which can be measured indirectly by means of WC,might be a major factor that connects obesity with frailty [39,40].However,the results of our study indicated that there was no relationship between WC and frailty status.In contrast,Ferriolli et al.found that older people with a large WC had a higher risk of prefrailty(OR:1.09;95%CI:1.02-1.17)and frailty(OR:1.15;95%CI:1.03-1.27) regardless of their BMI [24].Ramsay et al.also demonstrated that,compared with those that were not frail,those with prefrailty and frailty had higher odds of having a large waist circumference (OR:1.69;95% CI:1.32-2.15 for prefrailty and OR:2.30;95% CI:1.67-3.17 for frailty) [14].These studies applied a threshold value for WC of 88 cm for women and 102 cm for men,as recommended by WHO [41].In the present study,we applied Chinese-specific criteria,i.e.,80 cm for women and 85 cm for men[29].These different cut-off values might explain the contradiction between the studies.Although some covariates such as age,sex,cholesterol lowering medication etc.have been adjusted in multinomial logistic regression,we did not justify the potential confounding factors such as physical activity,which might play an important role in the relation between WC and frailty [42].More accurate identification of visceral fat tissue and subcutaneous fat tissue through CT or MRI will help us better understand the mechanism of frailty in people with high waist circumference[43].
Frailty is not an irreversible,one-way process towards disability or death,but a dynamic process that might involve improvement.For instance,a recently published systematic review analyzed 16 prospective studies (42,775 community-dwelling older people with a mean age ≥60 years and a mean follow-up of 3.9 years)which found that 23.1% of prefrail individuals improved to being not frail,while only 3%of frail participants did so[44].It is plausible that appropriate interventions such as weight control in a timely manner could promote the transition of prefrail older people backto health and potentially prevent related consequences.
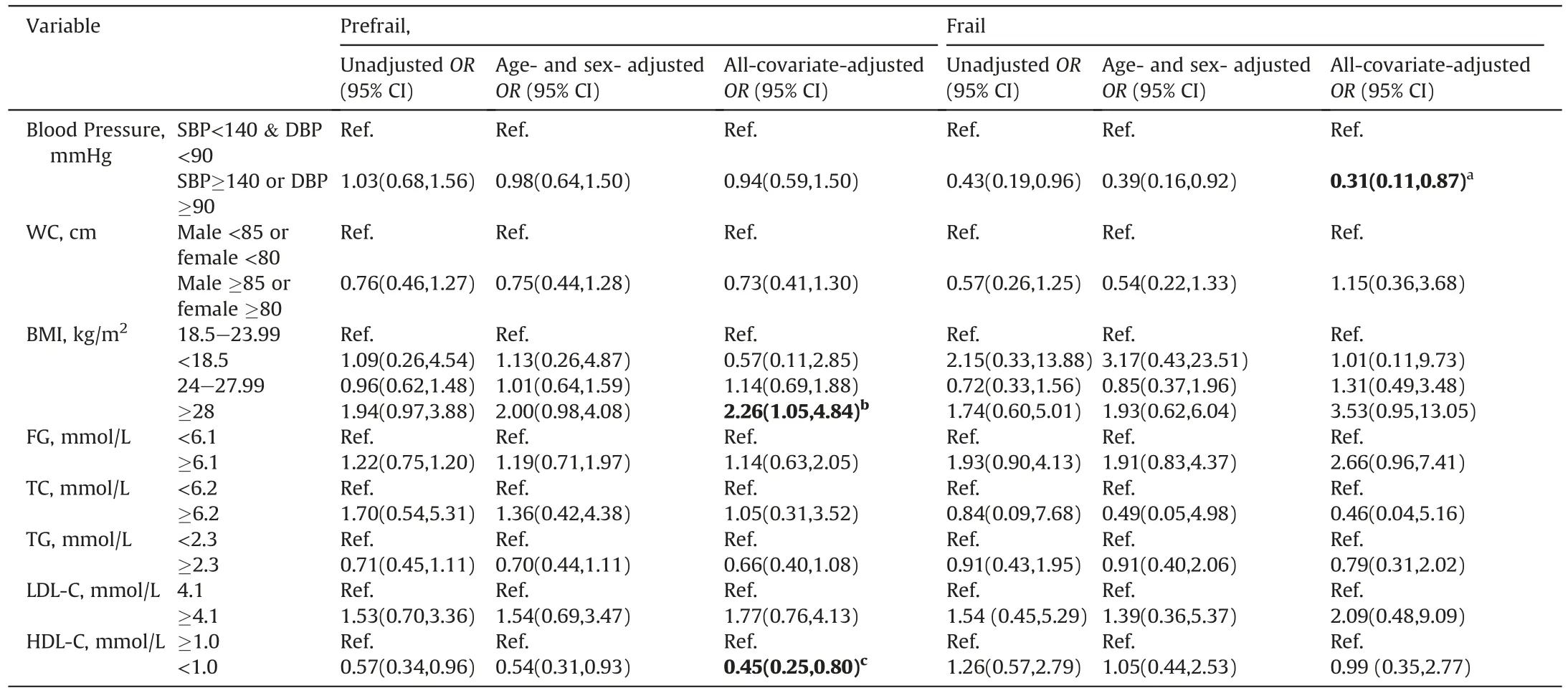
Table 3 Association of cardiovascular disease risk factors with frailty status in 458 Chinese older adults aged 65-94 years.
4.3.Hypertension and frailty
Our finding that hypertension being should be associated with lower odds of frailty was consistent with that of population-based studies in which frail individuals had lower SBP or DBP than nonfrail participants [14,45].It is also possible that reduced blood pressure develops as a consequence of primary cardiac disease and diminished cardiac output [45].Systemic hypoperfusion might be an independent risk factor for cardiovascular disease,sarcopenia and frailty[46].The elevated SBP and DBP in the older adults may be associated with better tissue perfusion,which can prevent the process of muscle fiber atrophy and loss of strength [45].In contrast,using a cross-sectional survey of 4,735 older adults in the United States (mean age:74 years,42.3% male),Newman et al.found that for individuals with an SBP of 125 mmHg(1 mmHg=0.133 kPa)or higher,elevated SBP was associated with an increased risk of frailty by approximately 15%for each additional 10 mmHg;DBP was similarly associated with frailty,although at a lower magnitude [47].Given the inconsistent findings with particular cross-sectional study designs used in the various studies,prospective studies are required to further explore the relationship between blood pressure and frailty status.
4.4.Lipid profile and frailty status
We failed to find a significant positive association between lipid profile and frailty status in our community-dwelling Chinese sample.This was in agreement with a 10-year longitudinal cohort study of 3,895 British older adults (mean age:55.2 years,73.4%male) in which Bouillon et al.found that there was no association between TC and frailty [11].However,our results demonstrate a negative association between low HDL-C and prefrailty,which was inconsistent with other studies.A population-based study of 1,622 British men (mean age:79 years) found that low HDL-C was associated with an increased risk of frailty [14].Moreover,a prospective cohort study conducted in Italy investigated 359 individuals and found that higher HDL-C levels were associated with a faster 4 m walking-speed after adjustment for potential confounders [48].A potential explanation for the differences may pertain to differences in the study population.Further epidemiological studies with a larger sample size are required to explore the impact of lipid profile on frailty.
5.Limitations
A number of study limitations should be noted.Our use of crosssectional study design does not allow us to establish any causal inference about the relationship observed between study variables.In addition,the study sample was recruited from two community hospitals in China during their annual physical examination;hence the enrolled participants were generally healthy older adults who could move freely,limiting the generalizations of the study findings beyond the study population.Finally,the participant medical history and medication were collected via self-reporting instead of medical record review;hence there was a possibility of recall bias.
6.Conclusion
Taken together,this study found that certain cardiovascular disease risk factors (obesity and hypertension) were significantly associated with increased or reduced odds of prefrailty or frailty among community-dwelling Chinese older adults.These findings suggest that future intervention should address weight control among prefrail older adults as a targeted strategy to prevent or delay the transition to frailty.Early screening the incidence of frailty for individuals with obesity should not be neglected.Future research should grasp the prefrail period,a window of opportunity for more comprehensive preventive or therapeutic interventions for the elderly that might improve their adverse health outcomes.Integrating the risk factors of cardiovascular disease to establish a predictive scoring system is the direction that subsequent researchers should strive for.
CRediT authorship contribution statement
Yanhong Wang:Conceptualization,Methodology,Software,Writing-Original Draft,Funding acquisition.Hae-Ra Han:Writing-Reviewing and Editing.Wei Yang:Data curation.Hongchen Zhang:Investigation.Jing Zhang:Software,Validation.Haihui Ruan:Validation.Nan Tang:Visualization.Jingjing Ren:Data curation.Xia Sun:Data curation.Chunrong Li:Data curation.Lin Han:Supervision,Project administration.
Funding
This work was supported by the National Natural Science Foundation of China [grant number 71804064].
Declaration of competing interest
The authors declared no potential conflicts of interest with respect to the research,authorship,and/or publication.
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2021.03.008.
杂志排行
International Journal of Nursing Sciences的其它文章
- Lived experiences of the disease journey among patients with idiopathic pulmonary fibrosis
- Supplement to the published paper“Theory-guided interventions for Chinese patients to adapt to heart failure:A quasi-experimental study”
- Using action research to evaluate a nursing orientation program in a multicultural acute healthcare setting
- Persistent effect of nurse-led education on self-care behavior and disease knowledge in heart failure patients
- Examining advanced nursing practice in Hong Kong and Guangzhou
- Effects of a theory of planned behavior-based intervention on breastfeeding behaviors after cesarean section:A randomized controlled trial
