Establishment and implementation of safety check project for invasive procedures outside the operating room
2021-05-19YnHouXioyuDiChnellConcepcionXioynShenYingSun
Yn Hou ,Xioyu Di ,* ,Chnell Concepcion ,Xioyn Shen ,Ying Sun
aNursing Administration,Beijing United Family Hospital,Beijing,China
bOperating Department,Beijing United Family Hospital,Beijing,China
ABSTRACT Objective:This study aimed to describe the implementation of the surgical safety check policy and the surgical safety checklist for invasive procedures outside the operating room (OR) and evaluate its effectiveness.Methods:In 2017,to improve the safety of patients who underwent invasive procedures outside of the OR,the hospital quality and safety committee established the surgery safety check committee responsible for developing a new working plan,revise the surgery safety check policy,surgery safety check form,and provide training to the related staff,evaluated their competency,and implemented the updated surgical safety check policy and checklist.The study compared the data of pre-implementation(Apr to Sep 2017) and two post-implementation phases (Apr to Sep 2018,Apr to Sep 2019).It also evaluated the number of completed surgery safety checklist,correct signature,and correct timing of signature.Results:The results showed an increase in the completion rate of the safety checklist after the program implementation from 41.7% (521/1,249) to 90.4% (3,572/3,950),the correct rates of signature from 41.9%(218/521)to 99.0%(4,423/4,465),and the correct timing rates of signature from 34.4%(179/521)to 98.5%(4,401/4,465),with statistical significance (P <0.01).Conclusion:Implementing the updated surgery safety check significantly is a necessary and effective measure to ensure patient safety for those who underwent invasive procedures outside the OR.Implementing surgical safety checks roused up the clinical staff’s compliance in performing safety checks,and enhanced team collaboration and communication.
Keywords:Invasive procedures outside the operating room Safety management Surgical safety checklist Patient safety
What is known?
· Surgical procedures on the wrong patient,wrong procedure,and wrong operative site are significant safety concern for the patient in the operating room(OR).
· The surgical safety checklist was widely used in the OR to ensure correct patient,correct operation,and correct operation side and site.
· Miscommunication among healthcare providers is a common issue in the OR,which often contributes to adverse events.
What is new?
· Safety checklists should be applied not only in the OR but also in other departments where invasive procedures are performed.
· Description of the hospital’s process in developing policy and procedures to address the same standard of safety check inside and outside the OR.
· Safety checklist and procedures were modified to promote communication,teamwork,and staff accountability outside the OR.
1.Introduction
Surgical or invasive procedure events,including wrong patient,wrong procedure,wrong site,and faulty implants,are consistently on the top list of sentinel events reported by The Joint Commission[1].The World Health Organization (WHO) introduced the use of the WHO surgical safety checklist (the 1st edition) in 2008 [2],which are reinforce accepted safety practices and foster better communication and teamwork between clinical disciplines[3].The National Healthcare Commission(NHC)of the People’s Republic of China(PRC)announced the surgical safety check as the core policy for hospitals to ensure the quality and safety of care for surgical patients [4].The China government launched the Modern Surgery and Anesthesia Safety Management System Construction and Promotion(MSCP)in 2014.Part of the strategy was using the WHO surgical safety checklist beyond the Operating Room (OR) to integrate it into the entire clinical process [5,6].The Joint Commission International (JCI) requires accredited hospitals to develop and implement a Time-Out method performed immediately before any surgical procedures and the Sign-Out after the procedure completion.This is an integral part of the International Patient Safety Goal(IPSG)espoused by JCI to ensure patient safety for surgical patients[7].Implementing the surgical safety checklist quality improvement program has significantly increased the safety policy’s compliance rate and consequently created a positive impact on clinical staff’s teamwork and safety awareness [8].Invasive procedures performed outside the OR include inpatient,outpatient,and emergency department (ED) for routinely planned procedural sedation or local anesthesia cases.Nowadays,invasive procedures are becoming more complex and require multidisciplinary team management.Braham et al.[9]recognized that although the surgical safety check is widely implemented in the OR,the same standard for invasive procedures outside the OR is lacking.In 2017,our hospital initiated the surgical safety check project using the updated surgical safety checklist for invasive procedures outside the OR and achieved effective outcomes.
2.Methods
2.1.Identified problems and problem analysis
The quality and safety committee identified the increased risk in using only the Time-Out checklist right before the start of the procedure instead of performing safety checks on three occasions,first before induction of sedation,second,procedure start or skin incision,and finally before the process complete for invasive procedures outside of the OR.The practice then was not in full compliance with the National Healthcare Commission(NHC)of the People’s Republic of China (PRC),WHO and Joint Commission International Accreditation (JCIA) standards.The WHO recommends that hospitals develop and implement a process for perioperative verification of surgical and invasive procedures including,but not limited to,open surgical procedures,percutaneous aspiration,selected injections,and biopsy in all areas of the hospital where these procedures occur[10].NHC of PRC and JCIA has made this rule for the hospital to implementing as core policy and standards.
2.2.Procedures
2.2.1.Establishment of a safety check committee
Before adopting the new workflow,our safety check process for an invasive procedure included going over a Time-Out checklist by the clinicians who were performing the procedure,assisting the system,and given sedation as applicable.The checklist is only required to be done one time before initiating the process and only focuses on the correct patient,correct procedure,and correct site.The checklist was simple and easy to use.However,it did not address all the possible risks,which may lead to a wrong patient,wrong procedure,wrong procedure side,and site,consequently not meeting the safety check standards.Invasive procedures are performed in almost all the clinical departments and involve many clinicians such as physicians,surgeons,anesthesiologists,nurses,and technicians.As the safety check involved multiple departments and multiple team’s participation,the Quality&Safety Committee suggested establishing a safety check committee to improve the procedure.
2.2.1.1.Member of the committee.The safety check committee was established.Eight members were selected,including department directors of surgery,internal medicine and dentistry,an ED physician,a radiologists,deputy director of nursing department,the head nurse of the outpatient operating room setting,and the quality &safety department’s manager.The committee was composed predominantly of physicians and nurses who perform invasive procedures.
2.2.1.2.Responsibility of committee members.To increase the committee’s efficiency,responsibilities for each member were clearly articulated.The committee chair was responsible for the overall project,leadership,and governance of the committee.The chair’s specific tasks include formulating the committee charter,reviewing the safety check policy and checklist,organizing the clinical monitoring of multidisciplinary and multi-departmental,urging the continuous quality improvement using the plan-do-check-act(PDCA) tool,and convening the committee regularly.The committee members were mainly responsible for drafting and modifying the safety check policy and checklist,staff training,and monitoring implementation in the clinical departments.The committee members were also in charge of the medical record auditing.The initial task of the committee was examining the WHO surgical safety check policy and the implementation rules [2],ensuring alignment with the regulations prescribed with JCI[7]and the NHC of PRC [4],and benchmarking best practices with the National Health Services (NHS) in the United Kingdom [11].The committee reached a consensus on the specific requirements needed to implement the program to fit the hospital conditions and circumstances.The successful implementation of the safety check policy and checklist required strong leadership,clear delegation of responsibilities,team collaboration,organizational support [12],and physician engagement.The safety check policy and checklist were required to be used for all patients who receive invasive procedures[13].To achieve the proper implementation of the surgical safety checklist,the safety check committee was also responsible for conducting process and quality monitoring through education and training,quality inspection,and regular medical record auditing.
2.2.2.Improvement plan
2.2.2.1.Define the invasive procedures outside the operating room.Invasive procedures commonly occur in ED,ICU,inpatient wards,outpatient setting,radiology department,etc.,which may be performed by ED physicians,ICU physicians,surgeons,radiologists,and anesthesiologists,etc.Invasive procedures in various locations by multiple clinicians brought challenges to the safety checklist implementation.By reinterpreting the guidelines of WHO and JCI,the importance of the surgical safety checklist has roused the attention of the clinical staff.Studies have shown that when the safety checklist is irrelevant and does not conform to conditions in the actual healthcare environment,hospital staff are less likely to use it [8,10].The committee enumerated the list of procedures(Table 1) requiring safety checks no matter where they were performed.The re-establishment of the approach enables the departments to serve evidence-based practice and have clear rules to follow.
2.2.2.2.Modification of the surgical safety checklist.In terms of the core policy of surgical safety checks issued by NHC and JCIArequirements to ensure surgery patient safety,the safety check committee revised the checklist of three safety checks for all invasive procedures.The three statements are Sign-In prior induction of sedation or process,Time-Out before procedure start or skin incision or,and Sign-Out before the end of the procedure(Table 2).Except for the three checks’ emphasis,the checklist also set up the details of using two identifiers to ensure correct patients,the correct type of procedure,correct site,surgical site marking,etc.Those are the critical safety checks for invasive procedures.To emphasize the team cooperation to conduct three safety checks,upon each checking,the participants involved in the safety check were required to sign their names and enter the time of each checking.Documents with the safety checklist were prepared by nurses,checked by all the team members involving in an invasive procedure and signed immedialy after completing the procedure.Table 2 illustrated the updated safety checklist contents,which were revised based on the WHO surgical safety checklist.
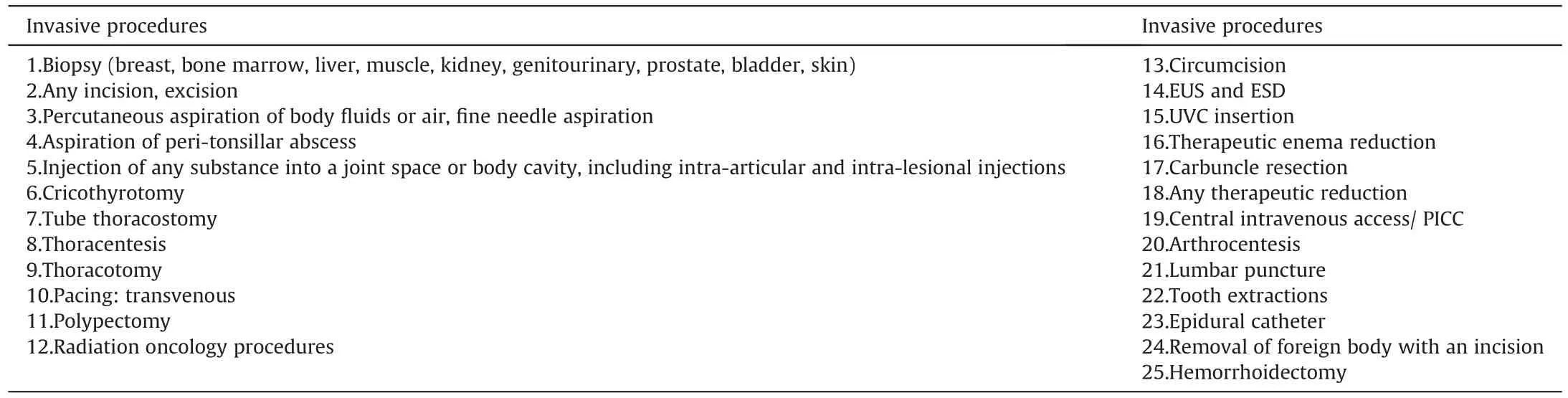
Table 1 Invasive procedures outside the operation room requiring a safe checklist.
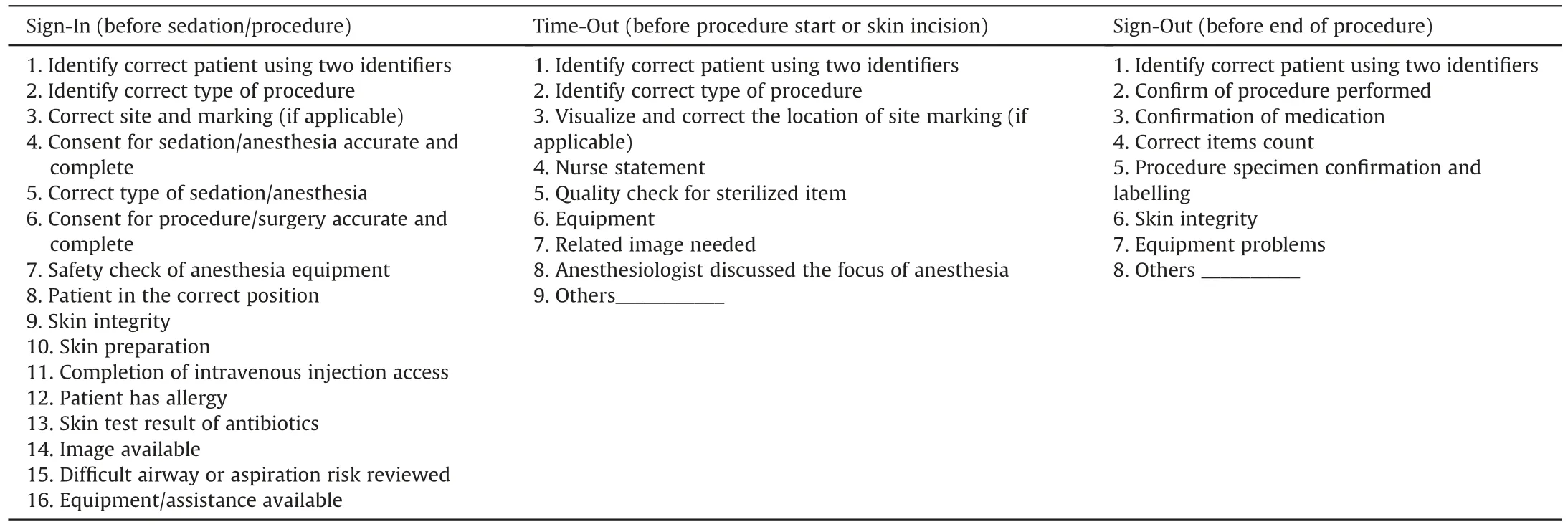
Table 2 Surgery/invasive procedure safety checklist.
2.2.3.Implementation of new policy and checklist
2.2.3.1.Policy and checklist approval.The safety check committee submitted the revised policy and forms to the Medical Advisory Board (MAB) and policy committee for approval.After the procedure and conditions were approved,the announcement was sent to the related departments and staff for implementation.
2.2.3.2.Education and training.Education and training play an essential role in empowering medical and nursing staff proficiency and knowledge [14].The safety check committee conducted multiple training sessions and required that all doctors,nurses,and technicians involved in the invasive procedures attend training before using the safety checklist.The training content included the historical background of the surgical safety checklist,scope of application,methods,and best practices of the general safety checks in various countries.The training also emphasized the surgical safety check policy and checklist made by our hospital,specific workflow,department and staff responsibilities,and precautions during the implementation.
Furthermore,the trainers demonstrated the checklist in various situations and critical thinking skills to implement the policies and procedures.The training promoted the staff’s understanding of the rationale behind the safety checks.Simulation has proved to be an effective learning method,which facilitated the learning and practices of complex skills within the hospital safety culture[15].To enhance the training effect and stimulate clinical staff awareness of the significance in compliance with the surgical safety checklist,the training team prepared scenarios for role-playing.This provides a more intuitive and comfortable atmosphere for the staff to understand the policy and procedures’ rationale.
2.2.3.3.On-site monitoring.The safety check committee members were assigned to various departments to observe the safety checking’s actual implementation and workflow.They also clarified issues raised by clinical staff,provided coaching,and addressed barriers to the safety checklist’s proper performance.It was also an opportunity to gather feedback from the team and consider further improvement.Each department was required to monitor and report the compliance with the safety check of invasive procedures each month.
2.2.3.4.Medical record auditing.The medical record quality ensures the continuity of patient care and accountability of healthcare staff[16].Medical record auditing aims to check the compliance in the completion of the surgical safety checklist.To check the effectiveness of implementing the surgical safety checklist,weekly medical record auditing was conducted.The audit focused on ensuring that the safety checklists were used correctly and accurately for all invasive procedures,including checking of correct patient,correct operation site,correct operation,and correct signature and timing.The final auditing result would be reported to the safety check committee,the medical safety committee,and the quality management committee.One of the disadvantages of medical record auditing is that it is time-consuming.However,its benefits to clinical practice far outweigh the disadvantages [17].
2.2.3.5.Monthly documentation tracing.As all the safety checklist were documented in the electronic medical record,the usage of safety checklist was traced to evaluate the staff’s compliance with the safety checks for invasive procedures,such as the correct documentation of the checklist,the correct signature and the correct timing of signature.The surgery safety check committee will trace the data and disseminate it to each department for the staff to further review,learn excellent experience and identify the weakness for further improvement.
2.3.Data collection
The surgical safety check documentation data was traced from the hospital Business Intelligence(BI) system.For comparison,the six-month data from Apr to Sep 2017 was collected as pre-implementation data and another six-month data from Apr to Sep 2018 as post-implementation data.Further more,data from Apr to Sep 2019 was collected to evaluate the implementation’s consistency.
2.4.Data analysis
SPSS version 19.0 was used to perform statistical analysis.Descriptive statistics data included implementation rates of safety checking,correct signature on the surgical safety checklist and correct timing of signature.Chi-square test was used to determine the difference between the data of pre-implementation and postimplementation phases.The level of statistical significance was set at P <0.05.
2.5.Ethical aspects
Ethics approval was obtained from the Institutional Ethics Committee of Beijing United Family Hospital with approval ID of BJUIRB.E2020-0002.
3.Results
There were no adverse events during the pre-implementation and post-implementation phases of the project in our hospital,such as errors in patient identification,procedure,and operative site.The completion rate of the safety checklist,and correct rates of signature and timing on the completed checklists during the postimplementation phases were higher than those of the preimplementation phase (P <0.01) (Table 3).No significant difference was found between the data in 2018 and 2019(P >0.05).
4.Discussion
Multiple research studies have shown that the three-time safety check during a surgical procedure improves the patients’safety and has been widely implemented as hospital practice standards worldwide.However,most of the studies only focus on the surgical procedures performed in the OR but excluded the invasive procedures outside of the OR.In this study,we have reviewed the invasive procedures performed outside the OR for 18 months over three years.In the 10,216 invasive procedures performed,no wrong patient,wrong operation,and wrong operation side/site was identified,indicating that the patients’ safety was ensured.The increased rates of correct signature and correct timing of signature showed significant improvement after the implementation,which means high compliance in performing the surgical safety check and high quality of medical documentation.
The hospital requires that all clinical teams participating in the invasive procedures must perform a three-time safety check to ensure patient safety.Based on understanding the international patient safety goals,the clinical staff’s risk and safety awareness was strengthed to improve implementation of the policy and safety checks.
Several studies have indicated that safety checklists improved teamwork,communication and decreased preventable errors due to poor team skills.Implementing the checklist usually requires the surgery department,anesthesiology department,and nurses [18].Effective and efficient communication is crucial in healthcare and promotes safe,high quality,and patient-centered care.The benefits of multidisciplinary collaboration in the hospital reduce adverse events,improve outcomes,and increase patients and employees[19].These benefits from establishing an open communication platform at the beginning of a procedure by sharing critical caserelated information,promoting team collaboration and decisionmaking,identifying knowledge gaps,and enhancing team cohesion [20].
Hospital safety culture is an essential component of many efforts to improve patient safety and care quality.Core hospital safety culture includes the determination of direction to create a safe environment,the committee’s goals and roles,the system’s redesign,creating a learning environment,and continuousimprovement [21,22].Strategies to promote patient safety culture may include team training,team communication tools,interdisciplinary rounding,system-level change,reporting structure,and executive walk rounds that directly engage organizational leadership with front-line care providers [23].In establishing and implementing the safety check policy outside the OR,the leaders’core cohesion,leadership skills,team member’s cooperation in redesigning,revising,and implementing the policy,workflow,and team spirit were fully demonstrated.
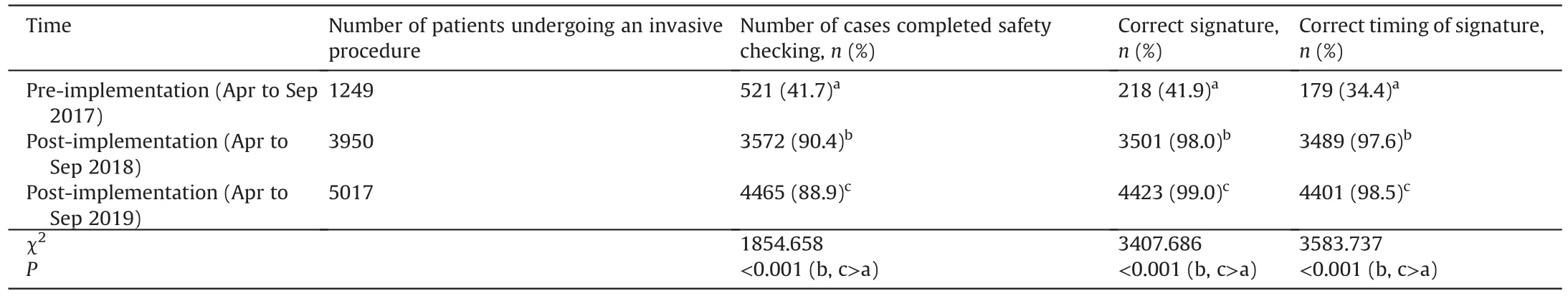
Table 3 Surgical safety checklist usage comparsion pre and post-implementation.
Even with the significant improvement of surgical safety checklist utilization for invasive procedures outside the OR during the post-implementation phases,there are still gaps to reach the full implementation for all the invasive procedures.Still,the documentation of correct signature and correct timing of signature had a slight improvement.Invasive procedures performed outside the OR require complex interactions between the interventionist,anesthesiologist,and nurses,and they may never have met the patient or each other or worked together before [24].Based on these research findings and our own experience of implementing the surgical safety checklist,further work is needed to assess the safety tool’s impact on patient safety.
5.Conclusion
The surgical environment is becoming more complex,and invasive procedures outside the OR have become equally crucial as surgeries performed in the OR.Implementing three-time safety check for invasive procedures outside the OR meets the standard of surgery/invasive procedure safety checks required by NHC of PRC and the JCIA.Implementing surgical safety checks is one of the essential measures to ensure patient safety and enhances team collaboration,communication,and safety culture.Moreover,indepth studies to achieve full compliance with the safety check for invasive procedures are needed.
Declaration of competing interest
The authors declared that they have no conflicts of interest to this work.
CRediT authorship contribution statement
Yan Hou:Conceptualization,Methodology,Software,Writingoriginal draft.Xiaoyu Di:Writing-original draft,Writing-review&editing.Chanell Concepcion:Writing -review &editing.Xiaoyan Shen:Visualization,Investigation.Ying Sun:Software,Validation.
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2021.02.002.
杂志排行
International Journal of Nursing Sciences的其它文章
- Associations between risk factors for cardiovascular diseases and frailty among community-dwelling older adults in Lanzhou,China
- Supplement to the published paper“Theory-guided interventions for Chinese patients to adapt to heart failure:A quasi-experimental study”
- Lived experiences of the disease journey among patients with idiopathic pulmonary fibrosis
- Persistent effect of nurse-led education on self-care behavior and disease knowledge in heart failure patients
- Using action research to evaluate a nursing orientation program in a multicultural acute healthcare setting
- Effects of a theory of planned behavior-based intervention on breastfeeding behaviors after cesarean section:A randomized controlled trial
