变应性鼻炎患儿中白介素-33高表达对Th2和Th17炎症反应的正向调控作用
2021-05-10王远明李楚凌罗香林许德瑜徐亚雄
王远明 李楚凌 罗香林 许德瑜 徐亚雄

【摘要】 目的:探討白介素-33(IL-33)在变应性鼻炎患儿中的表达和对Th2和Th17炎症反应的调控作用。方法:选取2017年1-6月就诊于本院的50例变应性鼻炎患儿,根据是否合并哮喘分为变应性鼻炎组(n=40)与变应性鼻炎伴哮喘组(n=10),另选取同期于本院体检的20例正常儿童作为对照组。比较三组血清和鼻腔灌洗液中IL-33和Th2、Th17细胞因子的表达情况,分析变应性鼻炎患儿IL-33和Th相关细胞因子的相关性。纯化外周血单个核细胞进行IL-33的体外调节实验,分析重组IL-33和相关细胞因子对外周血单个核细胞Th2和Th17炎症反应的调控作用。结果:变应性鼻炎组与变应性鼻炎伴哮喘组中血清和鼻腔灌洗液IL-33、IL-4、IL-5、IL-17均高于对照组,且变应性鼻炎伴哮喘组均高于变应性鼻炎组(P<0.05)。变应性鼻炎患儿血清和鼻腔灌洗液中IL-4、IL-5、IL-17均与IL-33表达呈正相关(P<0.05)。血清ECP、粉尘螨特异性IgE水平及嗜酸性粒细胞计数均与血清IL-33表达呈正相关(P<0.05)。HDM和1、10、100 ng/mL rhIL-33的IL-4、IL-5、IL-17水平均高于PBS,且10、100 ng/mL rhIL-33均高于1 ng/mL rhIL-33(P<0.05)。100 ng/mL rhIL-33的IL-4、IL-5及IL-17水平均高于HDM(P<0.05)。HDM+anti-IL-33的IL-4、IL-5及IL-17水平均高于PBS,而低于HDM(P<0.05)。结论:变应性鼻炎中IL-33的表达上调促进了Th2和Th17炎症反应,并为IL-33在变应性鼻炎发病机制中的调节作用提供了可能的解释。
【关键词】 白介素-33 变应性鼻炎 儿童
[Abstract] Objective: To investigate the expression of interleukin-33 (IL-33) in children with allergic rhinitis and its regulation of Th2 and Th17 inflammatory responses. Method: A total of 50 children with allergic rhinitis admitted to our hospital from January to June 2017 were selected, they were divided into allergic rhinitis group (n=40) and allergic rhinitis with asthma (n=10) according to whether they had asthma or not. Another 20 normal children underwent physical examination in our hospital during the same period were selected as the control group. The expression of IL-33 and Th2 and Th17 cytokines in serum and nasal lavage fluid of three groups were compared. The correlation between IL-33 and Th related cytokines in children with allergic rhinitis were analyzed. Purified peripheral blood mononuclear cells were used to conduct in vitro IL-33 regulation experiments, and the regulatory effects of recombinant IL-33 and related cytokines on Th2 and Th17 inflammatory response of peripheral blood mononuclear cells were analyzed. Result: The serum and nasal lavage fluid IL-33, IL-4, IL-5 and IL-17 in allergic rhinitis group and allergic rhinitis with asthma group were higher than those in the control group, and those in allergic rhinitis with asthma group were higher than those in allergic rhinitis group (P<0.05). The expression of IL-4, IL-5 and IL-17 in serum and nasal lavage fluid of children with allergic rhinitis were positively correlated with IL-33 (P<0.05). Serum ECP, dust mite specific IgE levels and eosinophil count were positively correlated with serum IL-33 expression (P<0.05). The levels of IL-4, IL-5 and IL-17 in HDM and 1, 10, 100 ng/mL rhIL-33 were higher than those in PBS, and those in 10 and 100 ng/mL rhIL-33 were higher than those in 1 ng/mL rhIL-33 (P<0.05). IL-4, IL-5 and IL-17 levels in 100 ng/mL rhIL-33 were higher than those in HDM (P<0.05). The levels of IL-4, IL-5 and IL-17 in HDM+anti-IL-33 were higher than those in PBS, but were lower than those in HDM (P<0.05). Conclusion: Up-regulated IL-33 protein in allergic rhinitis promote Th2 and Th17 inflammation, and provide a possible explanation for IL-33s regulatory role in the pathogenesis of allergic rhinitis.
[Key words] IL-33 Allergic rhinitis Children
First-authors address: Dongguan Women and Childrens Hospital, Dongguan 523000, China
doi:10.3969/j.issn.1674-4985.2021.06.003
变应性鼻炎是耳鼻喉科常见的过敏性疾病,儿童患病率达10%~40%,且在国内患病率有日益增加的趋势[1-2]。变应性鼻炎的组织学特征包括Th2炎症反应的增强,嗜酸性粒细胞浸润,变应原特异性IgE的产生和基底膜增厚[3-4]。Th2细胞的激活和进一步释放的细胞因子诱导各种免疫细胞的聚集,导致了变应性鼻炎的发生[5]。最近研究表明,Th17细胞可以增强哮喘小鼠模型中Th2细胞介导的嗜酸性粒细胞气道炎症[6-7]。此外,变应性鼻炎患者血清白介素-17(IL-17)水平的有所增加,且其与临床症状、外周嗜酸性粒细胞计数和药物相关[8-9]。白介素-33(IL-33)是IL-1超家族成员,其受体为ST2[10]。IL-33与其在不同细胞表面的ST2受体之间的相互作用进而促进Th2反应[11]。在变应性鼻炎中,IL-33与疾病严重程度相关[12-13]。在变应性鼻炎的实验性小鼠模型中,过敏原暴露诱导鼻上皮细胞产生IL-33,并且通过增加肥大细胞释放组胺和诱导嗜碱性粒细胞产生趋化因子,这对于鼻黏膜中嗜酸性粒细胞和嗜碱性粒细胞的积累起关键作用[14]。越来越多的证据表明,IL-33可能在Th2和Th17相关的变应性鼻炎中发挥积极作用。本研究旨在探讨IL-33在变应性鼻炎中的表达和对Th2和Th17炎症反应的调控作用,现报道如下。
1 资料与方法
1.1 一般资料 选取2017年1-6月就诊于本院的50例变应性鼻炎患儿。纳入标准:5~12岁;根据疾病史(临床症状喷嚏、清水样涕、鼻塞、鼻痒等症状出现2项以上,每天症状持续或累计在1 h以上),体格检查(鼻黏膜苍白、双下甲水肿,总鼻道及鼻底可见清涕或粘涕),皮肤点刺试验和特异性IgE的检测(主要包括常见过敏原,如尘螨、猫毛、狗毛等)符合变应性鼻炎2010年版指南和全球哮喘倡议(GINA)的诊断标准[15-16]。排除标准:慢性疾病(如营养不良,呼吸系统解剖畸形,慢性肺病,心脏病,胃食管反流病,囊性纤维化);一个月内有药物使用史(如口服或鼻用皮质类固醇,抗癫痫药,免疫抑制剂)。50例变应性鼻炎患儿根据是否合并哮喘分为变应性鼻炎组(n=40)与变应性鼻炎伴哮喘组(n=10)。另选取同期于本院体检的20例正常儿童作为对照组。本研究经东莞市妇女儿童医院伦理委员会批准,并由儿童父母签署知情同意书。
1.2 方法 每组抽血时间为晨起空腹8~9点。静脉血样品收集到真空管中并在3 000 g 4 ℃离心15 min。使用LH-785系统(爱尔兰Beckman Coulter公司)进行全血细胞计数。使用Unicap系统测定血清IgE。所有儿童保持坐位,身体前倾,每侧鼻孔用0.9%氯化钠溶液冲洗鼻腔并搜集灌洗液[17]。将样品离心以除去细胞碎片,并将等份的上清液在-20 ℃下分装备用。根据Bradford使用Bio-Rad蛋白质测定法测定总蛋白质浓度。使用酶联免疫吸附测定试剂盒来检测血清和鼻腔灌洗液IL-33、IL-4、IL-5、IL-17和ECP水平(美国R&D公司)。检测敏感度分别为:IL-33:125 pg/mL、IL-4:1.56 pg/mL、IL-5:7.8 pg/mL、IL-17:5 pg/mL。使用淋巴细胞分离液Ficoll制备外周血单个核细胞,然后以2×106/mL的密度在24孔板的RPMI 1640培养基中培养(5%人AB血清、5 mmol/L谷氨酰胺、青霉素和链霉素)。通过添加磷酸缓冲盐溶液(PBS)、粉尘螨蛋白(HDM,100 ng/mL)、重组人(rh)IL-33(1~100 ng/mL)、rhIL-33+rhIL-4(100 ng/mL)、rhIL-33+rhIL-5(100 ng/mL)、rhIL-33+rhIL-17(100 ng/mL)、HDM+anti-IL-33(100 ng/mL)进行刺激实验48 h,试剂均由美国R&D公司提供。所有实验重复三次。
1.3 观察指标 比较三组血清和鼻腔灌洗液中IL-33和Th2/17细胞因子的表达情况,分析变应性鼻炎患儿IL-33和Th相关细胞因子的相关性。纯化外周血单个核细胞进行IL-33的体外调节实验,分析重组IL-33和相关细胞因子对外周血单个核细胞Th2/17炎症反应的调控作用。
1.4 统计学处理 采用SPSS 20软件对所得数据进行统计分析,符合正态分布的计量资料用(x±s)表示,比较采用t检验;不符合正态分布的计量资料用M(P25,P75)表示,比较采用Mann-Whitney U检验;计数资料以率(%)表示,比较采用字2检验。采用Pearson相关分析用于分析生物标志物表达之间的相关性。以P<0.05为差异有统计学意义。
2 结果
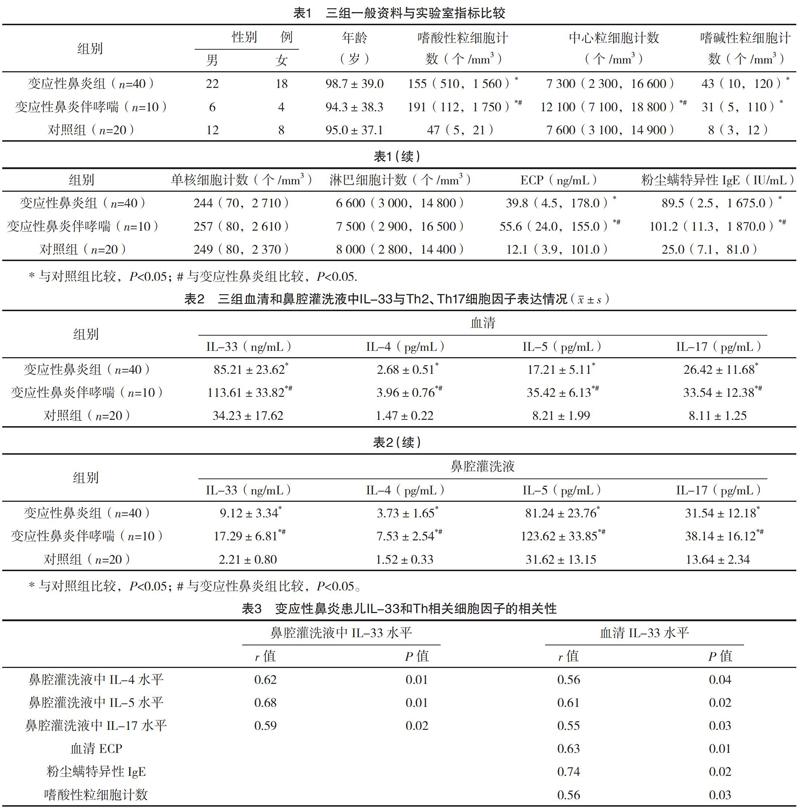
2.1 三组一般资料与实验室指标比较 三组性别与年龄比较,差异均无统计学意义(P>0.05),具有可比性。变应性鼻炎组嗜酸性粒细胞计数、ECP及粉尘螨特异性IgE均高于对照组,而均低于变应性鼻炎伴哮喘组,差异均有统计学意义(P<0.05)。变应性鼻炎伴哮喘组中心粒细胞高于变应性鼻炎组与对照组(P<0.05)。变应性鼻炎组与变应性鼻炎伴哮喘组嗜碱性粒细胞计数均高于对照组(P<0.05)。三组单核细胞计数与淋巴细胞计数比较,差异均无统计学意义(P>0.05)。见表1。
2.2 三组血清和鼻腔灌洗液中IL-33与Th2、Th17细胞因子表达情况 变应性鼻炎组与变应性鼻炎伴哮喘组血清和鼻腔灌洗液IL-33、IL-4、IL-5、IL-17均高于對照组,且变应性鼻炎伴哮喘组均高于变应性鼻炎组,差异均有统计学意义(P<0.05)。见表2。
2.3 變应性鼻炎患儿IL-33和Th相关细胞因子的相关性 血清和鼻腔灌洗液中IL-4、IL-5、IL-17均与IL-33表达呈正相关(P<0.05)。血清ECP、粉尘螨特异性IgE水平及嗜酸性粒细胞计数均与血清IL-33表达呈正相关(P<0.05)。见表3。
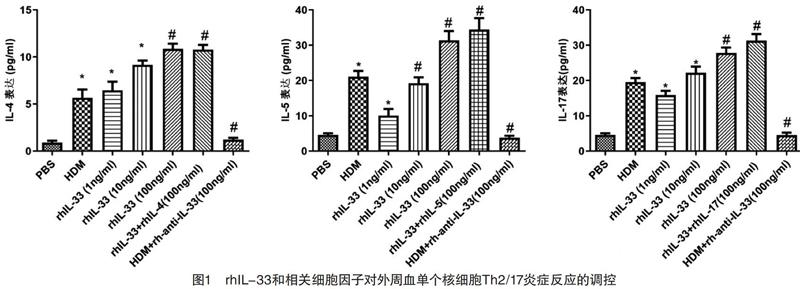
2.4 外周血单个核细胞刺激实验结果 HDM和1、10、100 ng/mL rhIL-33的IL-4、IL-5及IL-17水平均高于PBS,且10、100 ng/mL rhIL-33均高于1 ng/mL rhIL-33(P<0.05)。100 ng/mL rhIL-33的IL-4、IL-5及IL-17水平均高于HDM(P<0.05)。HDM+anti-IL-33的IL-4、IL-5及IL-17水平均高于PBS,而低于HDM(P<0.05)。rhIL-33+rhIL-4、rhIL-33+rhIL-5、rhIL-33+rhIL-17与100 ng/mL rhIL-33的IL-4、IL-5及IL-17水平比较,差异均无统计学意义(P>0.05)。见图1和表4。
3 讨论
变态反应是遗传因素与环境因素共同作用的疾病。鉴于其免疫学机制的复杂性,对源头发病机制的认识将有助于获得新的治疗靶点,并可望取得更持久、更彻底的疗效。目前研究表明变应性鼻炎的中IL-33表达升高与Th2、Th17炎症的发展密切相关,为变应性鼻炎的发病机制提供了新思路。
IL-33是细胞因子IL-1家族的成员,如IL-1β和IL-18。IL-33被认为与Th2介导的变应性疾病相关,如哮喘、特应性皮炎以及宿主防御寄生虫[18]。在哮喘的实验模型中,阻断IL-33/ST2信号级联可降低疾病的严重程度[19-23]。抗IL-33抗体显著降低体内2型细胞因子产生、嗜酸性粒细胞炎症和气道高反应性[24]。本研究结果显示,变应性鼻炎全身和局部IL-33细胞和Th2细胞因子的表达都显著增加,而进一步相关性分析提示,血清和鼻腔灌洗液中IL-33表达与2型细胞因子相关,提示IL-33可促进全身和局部Th2炎症。
研究显示在小鼠哮喘模型中,Th17细胞不仅增强中性粒细胞气道炎症,而且同样促进Th2细胞介导的嗜酸性粒细胞气道炎症[25]。IL-17是由Th17细胞产生的关键细胞因子。变应性鼻炎患者血清IL-17水平升高,并与临床症状,外周嗜酸性粒细胞计数和用药需要有关[8-9]。在本研究中,发现升高的IL-17表达与IL-33表达相关,提示IL-33可能参与Th17炎症。
为了确定IL-33在变应性鼻炎中的直接作用,本研究提纯了变应性鼻炎和对照组供体的外周血单个核细胞。粉尘螨作为常见过敏原可引发Th2炎症反应,因此被选为阳性对照。本研究结果显示,用HDM和1、10、100 ng/mL rhIL-33刺激后,来自变应性鼻炎的外周血单个核细胞中的Th2细胞因子(IL-4、IL-5)和IL-17水平显著上调,且呈剂量依赖模式。这些细胞因子可能来源于Th2、Th17细胞或者ILC细胞等,但其确切情况有待于后续研究。为了研究Th2细胞因子对IL-33表达的影响,进一步使用rhIL-4、rhIL-5、rhIL-17刺激外周血单个核细胞,结果显示rhIL-33和rhIL-4、rhIL-5、rhIL-17分别联合刺激外周血单个核细胞时,Th2、Th17细胞因子产生与IL-33单独刺激无明显变化,说明IL-4、IL-5和IL-17对IL-33的调控并无干预作用。然而,阻断IL-33可减少粉尘螨诱导的Th2、Th17细胞因子产生,表明IL-33在Th2、Th17炎症中起重要作用。这些结果表明IL-33参与变应性鼻炎的Th2、Th17炎症反应是单向调控的。
综上所述,IL-33是介导Th2、Th17炎症的关键细胞因子,并且是预测变应性鼻炎严重程度的潜在标志物,本研究可能为今后变应性鼻炎的预防和治疗提供新的目标。
参考文献
[1] Li H,Chen S,Cheng L,et al.Chinese guideline on sublingual immunotherapy for allergic rhinitis and asthma[J].J Thorac Dis,2019,11(12):4936-4950.
[2] Liu W,Cai J,Fu Q,et al.Associations of ambient air pollutants with airway and allergic symptoms in 13,335 preschoolers in Shanghai,China[J].Chemosphere,2020,252:126600.
[3] Eifan A O,Durham S R.Pathogenesis of rhinitis[J].Clin Exp Allergy,2016,46(9):1139-1151.
[4] Voskamp A L,Kormelink T G,van Wijk R G,et al.Modulating local airway immune responses to treat allergic asthma:lessons from experimental models and human studies[J].Semin Immunopathol,2020,42(1):95-110.
[5] Paller A S,Spergel J M,Mina-Osorio P,et al.The atopic march and atopic multimorbidity:Many trajectories,many pathways[J].J Allergy Clin Immunol,2018,143(1):46-55.
[6] Wakashin H,Hirose K,Maezawa Y,et al.IL-23 and Th17 cells enhance Th2-cell-mediated eosinophilic airway inflammation in mice[J].Am J Respir Crit Care Med,2008,178(10):1023-1032.
[7] Wilson R H,Whitehead G S,Nakano H,et al.Allergic sensitization through the airway primes Th17-dependent neutrophilia and airway hyperresponsiveness[J].Am J Respir Crit Care Med,2009,180(8):720-730.
[8] Liu Y,Zeng M,Liu Z.Th17 response and its regulation in inflammatory upper airway diseases[J].Clin Exp Allergy,2015,45(3):602-612.
[9] Liu W,Zeng Q,Zhou L,et al.Leptin/osteopontin axis contributes to enhanced T helper 17 type responses in allergic rhinitis[J].Pediatr Allergy Immunol,2018,29(6):622-629.
[10] Ding W,Zou G L,Zhang W,et al.Interleukin-33:Its Emerging Role in Allergic Diseases[J].Molecules,2018,23(7):1665.
[11] Bergougnan C,Dittlein D C,Hümmer E,et al.Physical and immunological barrier of human primary nasal epithelial cells from non-allergic and allergic donors[J].World Allergy Organ J,2020,13(3):100109.
[12] Glück J,Rymarczyk B,Jura-Szo?tys E,et al.Serum levels of interleukin 33 and its receptor ST2 in patients treated with subcutaneous allergen immunotherapy in intermittent allergic rhinitis[J].Cent Eur J Immunol,2019,44(2):214-217.
[13] Smejda K,Borkowska A,Jerzynska J,et al.IL-33 is associated with allergy in children sensitized to the cat[J].Allergol Immunopathol(Madr),2020,48(2):130-136.
[14] Akasaki S,Matsushita K,Kato Y,et al.Murine allergic rhinitis and nasal Th2 activation are mediated via TSLP-and IL-33-signaling pathways[J].Int Immunol,2016,28(2):65-76.
[15] Bro?ek J L,Bousquet J,Agache I,et al.Allergic Rhinitis and its Impact on Asthma(ARIA)guidelines-2016 revision[J].J Allergy Clin Immunol,2017,140(4):950-958.
[16] Pedersen S E,Hurd S S,Lemanske R F,et al.Global strategy for the diagnosis and management of asthma in children 5 years and younger[J].Pediatr Pulmonol,2011,46(1):1-17.
[17] Kristina I,J?rgen P P,Magnus P B,et al.Clara cell protein in nasal lavage fluid and nasal nitric oxide-biomarkers with anti-inflammatory properties in allergic rhinitis[J].Clin Mol Allergy,2012,10:4.
[18] Donovan C,Hansbro P M.IL-33 in Chronic Respiratory Disease:From Preclinical to Clinical Studies[J].ACS Pharmacol Transl Sci,2019,3(1):56-62.
[19] Khaitov M R,Gaisina A R,Shilovskiy I P,et al.The Role of Interleukin-33 in Pathogenesis of Bronchial Asthma.New Experimental Data[J].Biochemistry(Mosc),2018,83(1):13-25.
[20] Du X,Li C,Wang W,et al.IL-33 induced airways inflammation is partially dependent on IL-9[J].Cell Immunol,2020,352:104098.
[21] Cai H,Wang J,Mo Y,et al.Salidroside suppresses group 2 innate lymphoid cell-mediated allergic airway inflammation by targeting IL-33/ST2 axis[J].Int Immuno,2020,81:106243.
[22] Cayrol C,Girard J P.IL-33:an alarmin cytokine with crucial roles in innate immunity,inflammation and allergy[J].Curr Opin Immunol,2014,31:31-37.
[23] Pushparaj P N,Tay H K,Hng S C,et al.The cytokine interleukin-33 mediates anaphylactic shock[J].Proc Natl Acad Sci USA,2009,106(24):9773-9778.
[24] Allinne J,Scott G,Lim W K,et al.IL-33 blockade affects mediators of persistence and exacerbation in a model of chronic airway inflammation[J].J Allergy Clin Immunol,2019,144(6):1624-1637.
[25] Park S C,Kim H,Bak Y,et al.An Alternative Dendritic Cell-Induced Murine Model of Asthma Exhibiting a Robust Th2/Th17-Skewed Response[J].Allergy Asthma Immunol Res,2020,12(3):537-555.
(收稿日期:2020-06-03) (本文編辑:田婧)
