血管内机械取栓术治疗急性基底动脉闭塞性卒中预后及其影响因素分析
2021-03-25高林
高林




【摘要】 目的:探討血管内机械取栓术治疗急性基底动脉闭塞性卒中患者的预后及其影响因素。方法:选取本院2018年1月-2021年3月收治的接受血管内机械取栓术治疗的急性基底动脉闭塞性卒中患者54例。记录患者基线资料、诊疗情况,治疗3个月后评估患者的预后,将患者分为预后良好组及预后不良组。分析不同指标对患者预后的影响。结果:54例患者中,48例(88.89%)患者血管再通,12例(22.22%)患者死亡,29例(53.70%)患者预后良好,25例(46.30%)患者预后不良。两组年龄、性别、既往病史、吸烟、饮酒、TOAST分型、基底动脉闭塞部位、rt-PA静脉溶栓及症状性颅内出血发生率比较,差异均无统计学意义(P>0.05);与预后不良组比较,预后良好组入院NIHSS评分低、侧支循环良好率高、发病至入院时间及发病至再通时间均较短,差异均有统计学意义(P<0.05)。预后良好组血管再通率高于预后不良组,术后24 h NIHSS评分低于预后不良组(P<0.05)。logistic回归分析显示,入院及术后24 h NIHSS评分、发病至入院时间、发病至再通时间为预后不良的危险因素,而侧支循环良好、血管再通为保护因素(P<0.05)。结论:血管内机械取栓术治疗急性基底动脉闭塞性卒中血管再通率较高,入院及术后24 h NIHSS评分、发病至入院时间、发病至再通时间为预后不良的危险因素,而侧支循环良好、血管再通为保护因素。
【关键词】 机械取栓 急性基底动脉闭塞 卒中
Prognosis and Influencing Factors of Endovascular Mechanical Thrombectomy for Acute Basilar Artery Occlusive Stroke/GAO Lin. //Medical Innovation of China, 2021, 18(32): 0-019
[Abstract] Objective: To investigate the prognosis and influencing factors of endovascular mechanical thrombectomy for acute basilar artery occlusion stroke. Method: A total of 54 patients with acute basilar artery occlusive stroke treated by intravascular mechanical thrombectomy in our hospital from January 2018 to March 2021 were selected. Baseline data and diagnosis and treatment were recorded. After 3 months of treatment, the patients’ prognosis was evaluated, and they were divided into good prognosis group and poor prognosis group. The effects of different indexes on the prognosis of patients were analyzed. Result: Among the 54 patients, 48 cases (88.89%) had vascular recanalization, 12 cases (22.22%) died, 29 cases (53.70%) had good prognosis and 25 cases (46.30%) had poor prognosis. There were no significant differences in age, sex, past medical history, smoking, drinking, TOAST classification, basilar artery occlusion, rt-PA intravenous thrombolysis and symptomatic intracranial hemorrhage between the two groups (P>0.05). Compared with the poor prognosis group, the good prognosis group had lower NIHSS score at admission, higher rate of good collateral circulation, shorter time from onset to admission and from onset to recanalization, the differences were statistically significant (P<0.05). The vascular recanalization rate in the good prognosis group was higher than that in the poor prognosis group, and the NIHSS score 24 h after operation was lower than that in the poor prognosis group (P<0.05). logistic regression analysis showed that NIHSS scores at admission and 24 h after operation, time from onset to admission and time from onset to recanalization were risk factors for poor prognosis, while good collateral circulation and vascular recanalization were protective factors (P<0.05). Conclusion: Intravascular mechanical thrombectomy has a high rate of vascular recanalization in the treatment of acute basilar artery occlusive stroke, NIHSS scores at admission and 24 h after operation, time from onset to admission and time from onset to recanalization are risk factors for poor prognosis, while good collateral circulation and vascular recanalization are protective factors.
[Key words] Mechanical thrombectomy Acute basilar artery occlusion Stroke
First-author’s address: Fukuang General Hospital, Liaoning Health Industry Group, Fushun 113008, China
doi:10.3969/j.issn.1674-4985.2021.32.004
急性基底动脉闭塞(ABAO)导致的缺血性卒中约占所有缺血性卒中的1%,但具有较高的致残率及致死率[1-2]。据报道,仅给予抗血小板和抗凝治疗的病死率为40%,在患有严重疾病,如伴有昏迷、闭锁综合征或四肢瘫痪的患者中,病死率为54%[3-4]。早期血管再通是受急性后循環缺血性卒中影响的患者获得良好临床效果的最重要预测因素之一[5],其治疗方式包括静脉溶栓、动脉内溶栓、机械取栓术等,尽管静脉注射重组组织型纤溶酶原激活剂(rt-PA)仍然是急性缺血性卒中的一线治疗方法,但其应用时间窗短且在ABAO中实际应用再通率较低[6]。血管内机械取栓术对前循环大血管闭塞的有效性及安全性已被证实[7-8],其对ABAO亦是有效的[9-10];但文献[11]研究显示,ABAO引起的卒中患者血管内治疗后90 d死亡率约为前循环大血管闭塞患者的2倍。本研究对ABAO患者血管内机械取栓术治疗的预后及其影响因素进行分析,现报道如下。
1 资料与方法
1.1 一般资料 选取本院2018年1月-2021年3月收治的接受血管内机械取栓治疗的急性基底动脉闭塞性卒中患者54例为研究对象。纳入标准:(1)年龄≥18岁;(2)符合急性缺血性卒中诊断标准[12],且经影像学检查确定为ABAO并接受血管内机械取栓治疗;(3)入院时神经功能缺损评分(美国国立卫生研究院卒中量表,NIHSS)≥6分;(4)发病至穿刺时间在24 h内。排除标准:(1)颅内出血及梗死体积≥1/3脑干体积;(2)凝血功能障碍或正在接受抗凝治疗;(3)2周内大手术史或活动性出血;(4)严重心肝肾功能异常;(5)药物无法控制的顽固性高血压;(6)无法配合完成研究。本研究经医院医学伦理委员会批准,患者或家属知情同意。
1.2 方法 所有患者均给予改善循环等常规治疗,对于发病4.5 h内的患者先给予rt-PA静脉溶栓治疗。手术在局部麻醉下进行,选择股动脉入路,置入动脉鞘,造影明确闭塞部位及侧支循环情况,微导丝及微导管送至闭塞段远端,微导管造影证实在真腔,沿微导管送入取栓支架并跨闭塞段释放,3~5 min后回收取栓装置,复查造影评估闭塞血管血流情况,视情况进行2次或3次取栓,并视患者情况行动脉溶栓、球囊扩张或支架植入等治疗。
1.3 观察指标及评价标准 (1)记录患者治疗及预后情况。①血管再通评价:采用改良脑梗死溶栓治疗分级系统(mTICI)评估,分为0、1、2a、2b、3级,2b及3级为血管再通[10]。②预后判断:治疗3个月后对患者进行随访,采用改良Rankin量表(mRS)评价预后情况,得分0~6分,其中0~2分为预后良好,3~6分为预后不良[10]。(2)比较不同预后患者基线资料,包括年龄、性别、既往病史、吸烟情况、饮酒情况。(3)比较不同预后患者诊疗相关指标:入院NIHSS评分、缺血性脑卒中TOAST分型(大动脉粥样硬化、心源性栓塞、原因不明)、基底动脉闭塞部位(近段、中段、远段)、发病至入院时间、发病至再通时间、接受rt-PA静脉溶栓、侧支循环情况,侧支循环根据ASITN/SIR侧支循环评估系统进行分级,分为0~4级血流,以2~4级为侧支循环良好[13-14]。(4)比较不同预后患者血管再通、术后24 h NIHSS评分、症状性颅内出血情况。(5)分析预后的影响因素。
1.4 统计学处理 采用SPSS 26.0统计软件进行处理,对于计量资料,符合正态分布以(x±s)表示,比较采用t检验,不符合正态分布者采用M(P25,P75)表示,比较采用Mann-Whitney U检验;计数资料用率(%)表示,比较用字2检验或Fisher确切概率法;预后影响因素分析采用多因素logistic回归分析。P<0.05为差异有统计学意义。
2 结果
2.1 患者治疗及预后情况 54例患者中,15例(27.78%)术前给予rt-PA静脉溶栓治疗,所有患者均给予支架取栓治疗,48例(88.89%)患者血管再通;5例(9.26%)给予球囊扩张及原位支架释放,6例(11.11%)给予支架植入,5例(9.26%)接受rt-PA动脉溶栓;共12例(22.22%)患者死亡,其中住院期间死亡7例,随访期间死亡5例;术后坠积性肺炎4例,应激性溃疡5例;29例(53.70%)患者预后良好,25例(46.30%)患者预后不良。
2.2 两组基线资料比较 两组年龄、性别、既往病史、吸烟、饮酒情况比较,差异均无统计学意义(P>0.05),具有可比性,见表1。
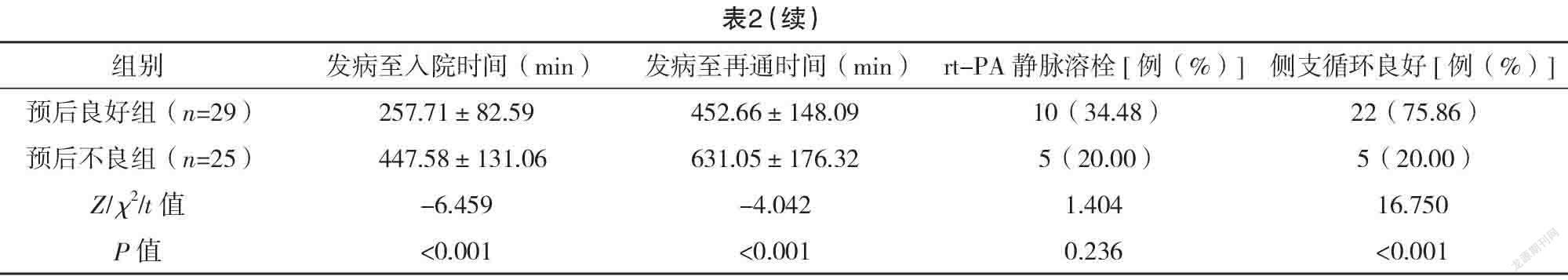
2.3 两组入院情况及治疗相关指标比较 与预后不良组比较,预后良好组入院NIHSS评分低、侧支循环良好率高、发病至入院时间及发病至再通时间均较短,差异均有统计学意义(P<0.05);两组TOAST分型、基底动脉闭塞部位、rt-PA静脉溶栓情况比较,差异均无统计学意义(P>0.05)。见表2。
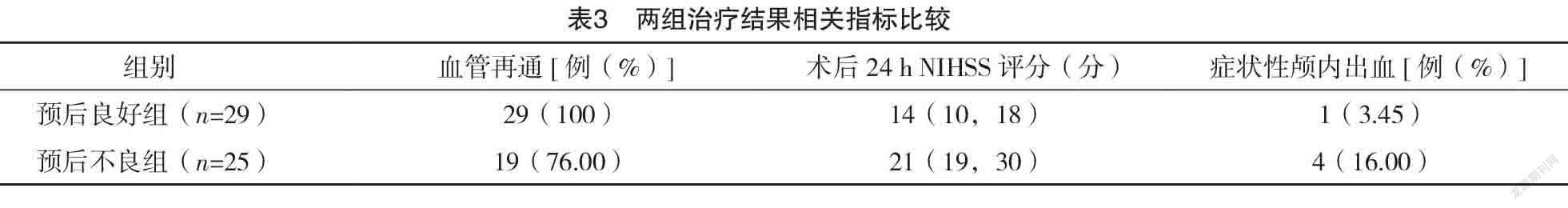
2.4 两组治疗结果相关指标比较 预后良好组血管再通率高于预后不良组,术后24 h NIHSS评分低于预后不良组(P<0.05);两组症状性颅内出血发生率比较,差异无统计学意义(P>0.05)。见表3。
2.5 预后影响因素的多因素分析 以预后是否良好为应变量(是=0,否=1);自变量中的入院及术后24 h NIHSS评分、发病至入院时间、发病至再通时间为连续变量,侧支循环良好、血管再通赋值为否=0,是=1。logistic回归分析显示,入院及术后24 h NIHSS评分、发病至入院时间、发病至再通时间为预后不良的危险因素,而侧支循环良好、血管再通为保护因素(P<0.05),见表4。
3 讨论
ABAO易引起严重的持续神经损伤及较高死亡率,基底动脉的早期再通与患者的生存和良好功能恢复密切相关[13]。机械取栓利用支架装置进行取栓治疗,可使闭塞血管快速再通,且应用时间窗较rt-PA明显更长[14]。以往研究表明,血管内机械取栓术应用于ABAO患者中,81%~100%的患者实现完全血管再通,预后良好率占20%~56%,死亡率为6%~36%[1,10]。而本研究中88.89%的患者血管再通,53.70%的患者预后良好,22.22%的患者死亡,与上述研究一致,尽管本研究的血管再通率较高,但在治疗3个月后的评估中,预后良好患者却仅占53.70%,因此除了血管再通,还有其他影响患者预后的变量。研究表明,与ABAO患者预后相关的影响因素包括卒中严重程度、年龄、治疗时间、再通成功率、側支循环、血栓位置等,但并未就此得出一致结论,甚至得出相互矛盾的结果[15-17]。
本研究多因素logistic回归分析显示,入院及术后24 h NIHSS评分、发病至入院时间、发病至再通时间为预后不良的危险因素,而侧支循环良好、血管再通为保护因素(P<0.05),而在年龄、性别、既往病史、吸烟、饮酒、TOAST分型、基底动脉闭塞部位、rt-PA静脉溶栓及症状性颅内出血发生率方面,不同预后患者并未表现出明显差异。NIHSS是评价神经功能缺损的重要指标,多项研究显示NIHSS评分高为预后不良危险因素[6,11,13,18-19],本研究得出了一致结论,无论术前及术后,NIHSS对于判断预后均有重要意义。缩短发病至入院时间及发病至再通时间对于减少脑组织因缺血缺氧而造成的不可逆损伤有重要意义,文献[20]研究显示,机械取栓治疗ABAO的预后不仅与手术时间有关,且具有时间依赖性,因此医生应提高手术技能尽量缩短手术时间。对于缺血性卒中患者,侧支循环的建立对于减小梗死面积,挽救缺血半暗带及神经功能具有重要作用[14],因此,较好的侧支循环有利于术后功能恢复,改善患者预后。血管的成功再通是缺血脑组织再灌注的基础,可明显降低致残率及病死率[21],WU等[18]研究显示,从卒中开始到再通的时间为长期预后的独立预测因素,与本研究结果一致。
综上所述,血管内机械取栓术治疗急性基底动脉闭塞性卒中血管再通率较高,入院及术后24 h NIHSS评分、发病至入院时间、发病至再通时间为预后不良的危险因素,而侧支循环良好、血管再通为保护因素。但本研究样本量较小,可能存在一定偏倚,仍需进一步大规模随机对照研究对结果加以验证。
参考文献
[1] Gilberti N,Gamba M,Premi E,et al.Endovascular mechanical thrombectomy in basilar artery occlusion: variables affecting recanalization and outcome[J].J Neurol,2016,263(4):707-713.
[2] Jk A,To B,Ku A,et al.Endovascular treatment of acute basilar artery occlusion: Outcomes, influencing factors and imaging characteristics from the Tama-REgistry of acute thrombectomy (TREAT) study[J].J Clin Neurosci,2021,86:184-189.
[3] Schonewille W J,Wijman C A,Michel P,et al.Treatment and outcomes of acute basilar artery occlusion in the Basilar Artery International Cooperation Study (BASICS):a prospective registry study[J].Lancet Neurol,2009,8(8):724-730.
[4] Kaneko J,Ota T,Tagami T,et al.Endovascular treatment of acute basilar artery occlusion: Tama-REgistry of Acute Thrombectomy (TREAT) study[J].J Neurol Sci,2019,401:29-33.
[5] Kharitonova T V,Melo T P,Andersen G,et al.Importance of cerebral artery recanalization in patients with stroke with and without neurological improvement after intravenous thrombolysis[J].Stroke,2013,44(9):2513-2518.
[6] Giorgianni A,Biraschi F,Piano M,et al.Endovascular Treatment of Acute Basilar Artery Occlusion: Registro Endovascolare Lombardo Occlusione Basilar Artery (RELOBA) Study Group Experience[J].J Stroke Cerebrovasc Dis,2018,27(9):2367-2374.
[7] Goyal M,Demchuk A M,Menon B K,et al.Ran-domized assessment of rapid endovascular treatment of ischemic stroke[J].
N Engl J Med,2015,372(11):1019-1030.
[8] Saver J L,Goyal M,Bonafe A,et al.Stent-retriever thrombectomy after intravenous t-PA vs t-PA alone in stroke[J].
N Engl J Med,2015,372(24):2285-2295.
[9] Werner M,Lopez-Rueda A,Zarco F,et al.Mechanical thrombectomy in acute basilar artery occlusion:A safety and efficacy single centre study[J].Interv Neuroradiol,2016,22(3):310-317.
[10]史宗杰,郑素洁,张圣,等.血管内机械取栓治疗急性基底动脉闭塞的有效性和安全性研究[J].中华神经医学杂志,2018,17(2):161-164.
[11] Gory B,Mazighi M,Labreuche J,et al.Predictors for Mortality after Mechanical Thrombectomy of Acute Basilar Artery Occlusion[J].Cerebrovasc Dis,2018,45(1-2):61-67.
[12]中华医学会神经病学分会,中华医学会神经病学分会脑血管病学组.中国急性缺血性脑卒中诊治指南2014[J].中华神经科杂志,2015,48(4):246.
[13] Gory B,Eldesouky I,Sivan-Hoffmann R,et al.Outcomes of stent retriever thrombectomy in basilar artery occlusion: an observational study and systematic review[J].J Neurol Neurosurg Psychiatry,2015,87(5):520-525.
[14]徐英钦.机械取栓治疗急性基底动脉闭塞患者预后的影响因素[D].新乡:新乡医学院,2020.
[15] Kwak H S,Park J S.Mechanical Thrombectomy in Basilar Artery Occlusion:Clinical Outcomes Related to Posterior Circulation Collateral Score[J].Stroke,2020,51(7):2045-2050.
[16] Katsumata M,Ota T,Tsuruta W,et al.Comparisons of Characteristics and Outcomes after Mechanical Thrombectomy for Vertebrobasilar Occlusion with Cardioembolism or Atherosclerotic Brain Infarction: Data from the Tokyo-Tama-Registry of Acute Endovascular Thrombectomy (TREAT)[J/OL].World Neurosurg,2021,148:e680-e688.
[17]杨海华,缪中荣.急性基底动脉闭塞血管内治疗及临床预后预测因素研究进展[J].中国卒中杂志,2018,13(12):1271-1276.
[18] WU L F,ZHANG D,CHEN J,et al.Long-term outcome of endovascular therapy for acute basilar artery occlusion[J].J Cereb Blood Flow Metab,2021,41:1210-1218.
[19] Guenego A,Bourcier R,Guillen M,et al.Neurological improvement predicts clinical outcome after acute basilar artery stroke thrombectomy[J].Eur J Neurol,2021,28(1):117-123.
[20] Mokin M,Sonig A,Sivakanthan S,et al.Clinical and Procedural Predictors of Outcomes From the Endovascular Treatment of Posterior Circulation Strokes[J].Stroke,2016,47(3):782-788.
[21]楊磊,张世阳,张栋梁,等.后循环基底动脉急性闭塞机械再通的疗效分析[J].河北医科大学学报,2017,38(7):825-828.
(收稿日期:2021-09-29) (本文编辑:张爽)
