The impact of the New Rural Cooperative Medical Scheme on the“health poverty alleviation” of rural households in China
2021-03-23QINLijianChienpingCHENLIYuhengSUNYanmingCHENHong
QIN Li-jian,Chien-ping CHEN,LI Yu-heng,SUN Yan-ming,CHEN Hong
1 Research Center for Health Economics,Anhui University of Finance and Economics,Bengbu 233000,P.R.China 2 School of Business Administration,University of Houston-Victoria,Sugar Land 77449,USA 3 Institute of Geographic Sciences and Natural Resources Research,Chinese Academy of Sciences,Beijing 100101,P.R.China 4 Institute for Global Innovation and Development/Institute of Eco-Chongming/School of Urban and Regional Science,East China Normal University,Shanghai 200062,P.R.China 5 School of Languages and Media,Anhui University of Finance and Economics,Bengbu 233000,P.R.China
Abstract This study investigates the impact of the New Rural Cooperative Medical Scheme (NRCMS) on rural households to escape poverty. We employ the instrumental variable method,the IVProbit model,to analyze the national data from the rural-resident field survey by the China Family Panel Studies (CFPS) in 2016. Based on the large-scale data,we found that,first,the hospitalization of family members is the key factor in increasing the risk of the family falling into poverty. The NRCMS has significantly reduced the likely risk of falling into poverty. Second,the impact of the NRCMS on poverty alleviation varies among groups with different levels of income. There is no impact on the upper-middle and high-income groups; in contrast,the NRCMS has substantially improved the capacity of low-income rural families to prevent poverty due to illness,especially for the lower-middle-income group. Third,there exist significant regional differences in the impact of NRCMS on the health poverty alleviation of rural households in China. The NRCMS has successfully reduced the risk of rural households in the western region falling into poverty,simultaneously,no significant impact on those in the eastern and central regions. In order to diminish and eliminate poverty eventually and boost rural residents’ capacity for income acquisition,we propose the following:raise the actual compensation ratio of the NRCMS,control the rising expense of NRCMS by promoting the payment method reform,construct the comprehensive healthcare system in the western region,strengthen the medical security for the poor in remote area,and enhance the living environment for rural residents.
Keywords:New Rural Cooperative Medical Scheme,rural households,health poverty alleviation
1.Introduction
One of the most important tasks for governments at all levels is to resolve and eradicate poverty. China has been working hard in domestic poverty alleviation to significantly reduce global poverty (United Nations 2017; Luoet al.2020).However,poverty in China is still a serious issue.As indicated in Huang (2019),it is a very challenging task to resolve poverty among all 16 000 villages in which the poverty rate is even higher than 20%. Illness is one of the key causes to trap rural families into poverty. Due to the uncertainty of disease and high medical expenses,the governmental policy goal of full relief of poverty,advocated by the slogan of “Health Poverty Alleviation” (Wang and Liu 2019),is unlikely to be achieved in 2020 (SCOPRC 2017). From the relative costs perspective,we observe that the growth rate of medical expenses has been far exceeded the growth rate of GDP and rural household income for many years in China. On the other hand,from the absolute costs perspective,China’s per capita hospitalization cost has reached 8 891 CNY. Meanwhile,the rural households’ per capita disposable income is only at 8 452 CNY,even lower than the per capita hospitalization cost (NBSC 2016).Theoretically,medical insurance can serve as a remedy to disperse family financial risk. For the purpose,China’s New Rural Cooperative Medical Scheme(NRCMS) has been implemented since 2003,at a relatively low per-capita funding rate,570 CNY per year initially. Is the low-funding NRCMS still effective in poverty alleviation?It becomes one of the most important research topics to explore the impact of the NRCMS on poverty alleviation to improve rural revitalization by effective policy modifications at all levels of government in China.
There are abundant studies on the impact of medical insurance on households in different countries. Shmueliet al.(2008),Hamidet al.(2011),Aryeeteyet al.(2016),and Alatinga and Williams (2019) found that health insurance has reduced medical costs for farmers,improved the labor efficiency and health of rural residents,increased rural household income,and reduced the probability of poverty caused by illness in Bangladesh and Spain. Benitezet al.(2018),Fry and Sommers (2018),and Kwonet al.(2018)studied the impact from varied medical insurances on household income,based on data from the US Health and Retirement Survey (HRS) and matched with data from the US Rand Research Center for Aging. They found that private insurance participants shouldered higher medical expenses and heavier personal financial burdens than the insured under public insurance. Low-income and middleaged people have the greatest burdens carried with medical issues and are most likely to fall into poverty.
Remarkably,some works of literature found that health insurance has no effect on household economics (Ekman 2007; Wagstaff and Lindelow 2008; Antuneset al.2018;Mozumdaret al.2018). Studies in China and Vietnam even concluded that insured rural residents tend to seek treatment at high-level medical institutions with higher overall medical costs and without any reduction in the direct out-of-pocket medical costs (Nguyenet al.2003; Chaudhuri and Roy 2008; Wagstaffet al.2009; Saksenaet al.2011;Lattof 2018). Furthermore,Ahmedet al.(2018) found that residents in the Mekong Delta region of Vietnam raised their out-of-pocket medical expenses after participating in medical insurance,and the poverty rate even increased. Umeh(2018) investigated national health insurance in Ghana,Kenya,Nigeria,and Tanzania,to find that health insurance plays no role in poverty alleviation due to the relatively low medical insurance funds and the relatively large scale of the poor population and informal employment.
Due to the late establishment of NRCMS,there are limited studies focusing on the impact of insurance coverage with varied findings such as Wanget al.(2009),Song and Zhao (2015),Zhu and Li (2017),and Chenet al.(2019). Based upon the 2003–2006 Fixed Rural Observation Point of the Ministry of Agriculture of China of 360 villages,Qi (2011) employed the instrumental variable method to resolve the endogenous problem and found that the NRCMS can reduce the poverty rate for rural farmer households when the coverage rate of NRCMS reaches 40.00% at the provincial level. However,the data were neither up to date nor collected by random sampling in the study. Huang (2019) investigated the 2000–2011 data of China Health and Nutrition Survey (CHNS) to find that the phenomenon of switching between poverty and out of poverty is quite frequent,especially for those vulnerable rural households who are easy to be trapped into poverty again. The impact of NRCMS on poverty reduction was significant only in the initial period (2000–2006). After the NRCMS was fully implemented in 2009,its impact on poverty reduction became insignificant due to the lack of focus on the compensation for catastrophic medical expenses such as hospitalization. However,the endogenous problem was not resolved in the model of Huang (2019). Yaoet al.(2014) used the China Health and Retirement Longitudinal Study (CHARLS) collected in 2011 to find that rural residents face more induced demand such as transportation after participating in the NRCMS. The cost of public hospital visits is even higher than that of private hospitals. Yuet al.(2018) studied a central province and found that the hospitalization rate of the poor is 12.46%,which is much higher than that for the population at 4.86%. After the NRCMS,the proportion of unreasonable hospitalization cases in township health institutions boosts up to as high as 26.50%. Yanet al.(2006),Xie (2008) and Fang (2013) found that the implementation of the NRCMS has increased the incidence of medical consultations among rural households;however,it has no impact on poverty alleviation. Zhu (2013)and Wang and Ning (2018) also studied poverty in the ethnic areas and found that the NRCMS participation rate of the ethnic minorities is lower than that of local Han residents.The poverty caused by illness in the ethnic minority areas is very noticeable. Undoubtedly,the task of a full poverty alleviation in China is very arduous.
There are several common problems in the existing literatures about the impact of NRCMS in China. First,the data are relatively outdated. As Huang (2017) indicated,most previous studies use data in or before 2006. Even in Yaoet al.(2014) and Huang (2019),the survey periods are in or before 2011 which only cover the initial years of the pilot promotion of the NRCMS. Second,most previous studies draw conclusions from the same data,CHNS,lack of comparisons in the research conclusions. Third,the sample representation is generally insufficient to reflect the population. Several studies only investigate a few counties or provinces. For example,Yuet al.(2018) inspected six counties in the province of Anhui and Yanet al.(2006) only explored five provinces. Even the CHNS data,the sampling is also limited within the nine provinces. Fourth,most previous studies focus on income,consumption,or medical services for rural households but ignore the impact of NRCMS on their poverty. Fifth,the endogenous problem remains in most regressions. It will mislead the estimation results.
In this study,we employ the instrumental variable method,the IVProbit model,to analyze the national data from the rural-resident field survey by the China Family Panel Studies(CFPS) in 2016 to resolve all the problems mentioned previously. Not only more updated,the CFPS data also cover 25 provinces to represent the majority of population in China. To resolve the endogenous problem in regression,we follow the setting in the research of migrant workers(Qinet al.2014,2018),to adopt the NRCMS participation rate in counties as the instrumental variable for household participation. We also ignore the rural individual participation of the other medical insurance or pension scheme in the study. As Qinet al.(2015) indicated,the rural migrant workers’ participation rates in the urban medical insurance and rural pension insurance are only at 15.35 and 14.09%,respectively. The basic monthly compensation from the rural pension insurance (i.e.,from 55 CNY in 2009 to 88 CNY in 2018) is also too minor to be considered as an impact on poverty alleviation.
Our findings indicate that the hospitalization of family members is a key factor in increasing the risk of the family falling into poverty. The NRCMS has significantly reduced the likely risk of falling into poverty. Second,the impact of the NRCMS on poverty alleviation varies among groups with different levels of income. There is no impact on the upper-middle-and high-income groups; the NRCMS has substantially improved the capacity of low-income rural families to prevent poverty due to illness,especially for the lower-middle-income group. Third,there exist significant regional differences in the impact of NRCMS on the poverty alleviation of rural households in China.The NRCMS has successfully reduced the risk of rural households in the western region falling into poverty,simultaneously,no significant impact on those in the eastern and central regions. The paper is arranged as follows. The next section provides the data source and descriptive statistics. Section 3 exhibits the economic theoretical framework and econometric model. The empirical results are discussed in the fourth section. The final section concludes and provides recommendations for government policymaking.
2.Data and descriptive statistics
The data used in this article are from CFPS conducted in July 2016. The survey was implemented by the Institute of Social Science Survey of Peking University of China to investigate the socio-economic,demographic,and health conditions,for all households in China. Compared with the CHNS data covering only nine provinces,the CFPS conducted 25 provinces,including the country’s autonomous regions and the municipalities. The surveyed area covers 94.50% of China’s total population except for Hong Kong,Macao and Taiwan. The CFPS survey employed the implicit stratification to perform the multi-stage probability sampling. It is a more accurate stratification method to reflect the geographical representation with varied economic development. A total of 14 019 households were selected from 162 counties and districts,including 6 782 households from rural areas. In order to examine the impact of NRCMS on rural households’ health and poverty alleviation,we only keep the sample of rural households who participate in the NRCMS without any other types of medical insurance. As a result,the number of sample rural households is reduced to 5 877. The variable definitions and descriptive statistics are detailed in Table 1.
Poverty lines serve as an important indicator of poverty verification for rural households. In China,the national poverty line is defined at the annual per-capita household income of 2 855 CNY or below. It is slightly higher than the World Bank poverty line,1.90 USD per day,equivalent to 2 665 CNY per year (NBSC 2017; World Bank 2018). Table 1 shows sample households containing the poverty ratios,according to China’s national poverty line and the World Bank poverty line,16.53 and 15.22%,respectively. The ratios are not far away from the poverty incidence of 14.40% in the 2015 National Sample Survey (Chenet al.2018,2019). One of the core independent variables is whether a rural household participates in the NRCMS or not. If the family members only participate in the NRCMS,then the value is 1; otherwise,it is 0. We can see that participation in NRCMS is as high as 91.96%. In the past year,22.98% of households with at least one family member were hospitalized. The descriptive statistics also show the low education for rural households.The household labor force’s average age is 39 years; the average schooling years are only 5.19 years. To distinguish the household head and labor force in the CFPS survey,we assume the first interviewed family member as the head of household because the first person speaks for the household is generally holding the most important role in a traditional Chinese family. Not surprisingly,the household head tends to be an older male at 56.44% with the average age at 51 years old. There are still 33.68% of the rural households using well water,cellar water or rainwater for cooking. The households in the hilly and alpine regions account for 28.71 and 20.40%,respectively,and the proportions of households in the central and western regions were 28.94 and 33.30%,respectively.
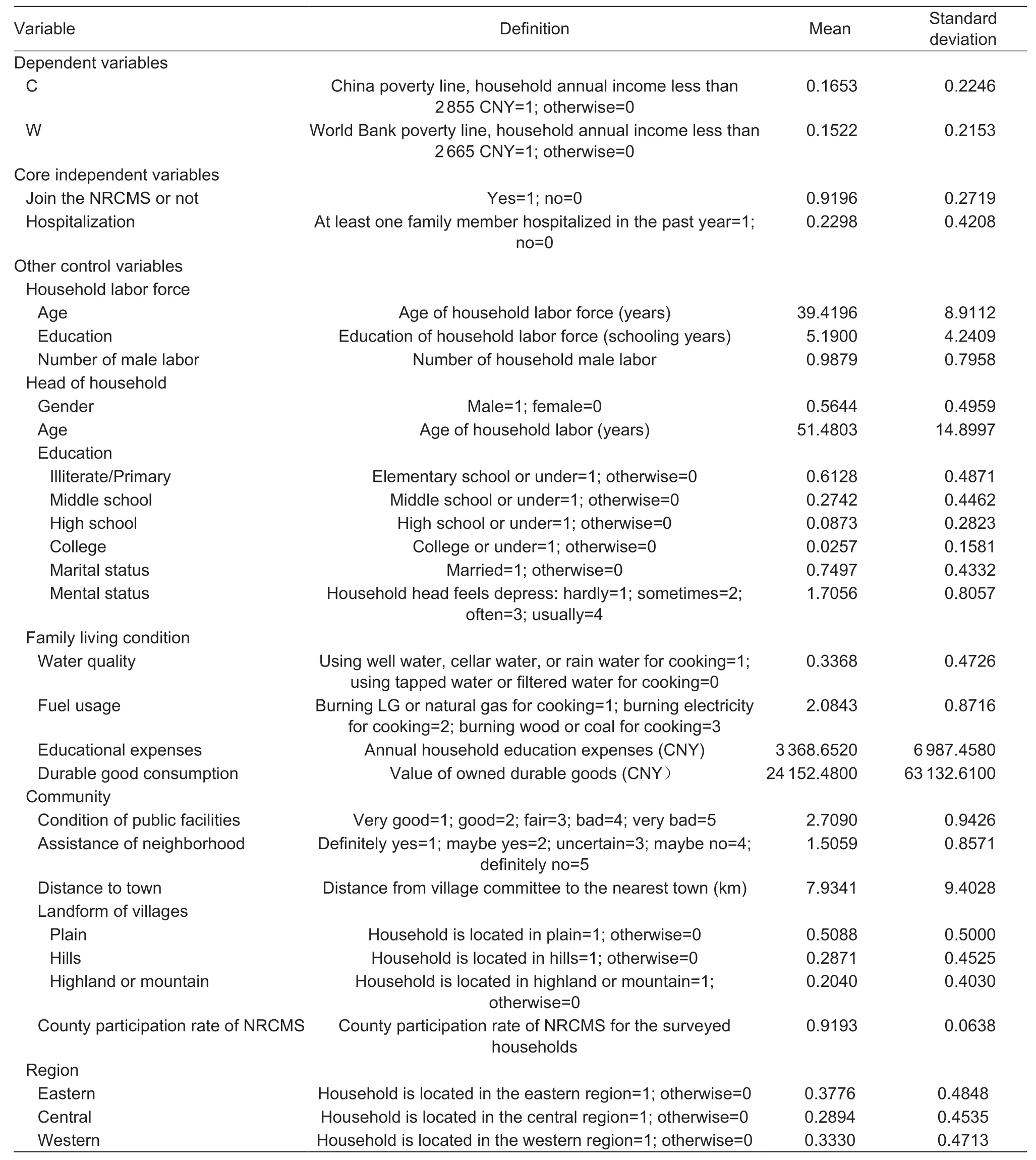
Table 1 Variable definition and descriptive statistics
3. Theoretical framework and econometric model
3.1.Theoretical framework
The study employs the classic Agricultural Household Model(AHM) as the foundation. The model was pioneered in Singhet al.(1986) to explore the farm household economic behavior,which was then widely used by researchers(Wanget al.2014; Hadleyet al.2019). A large number of empirical studies have been performed on the behaviors of supply,production,and consumption for the developing countries. The AHM considers a rural household the most fundamental and important economic component engaging in both consumption and production in the countryside to exhibit dual characteristics. Based upon the duality of rural households,we cannot simply analyze a households’economic behavior from one perspective as a consumer or a producer; instead,the theoretical model for the rural household should be composed of multiple interconnected equations. The basic assumptions are as follows. First,rural households pursue utility maximization; and the utility is affected by varied factors such as income. Second,the non-separability of income,consumption,and production determine the rural household economic behavior.Third,rural household labor forces are subject to time constraints;all time is allocated to leisure time,farming labor time,and non-farming labor time. Fourth,there is heterogeneity in the utility of households.
The objective function and constraints for a rural household’s decision making,including the decision of NRCMS participation in the constraints,are composed in the following equations:
Utility-maximization objective function:
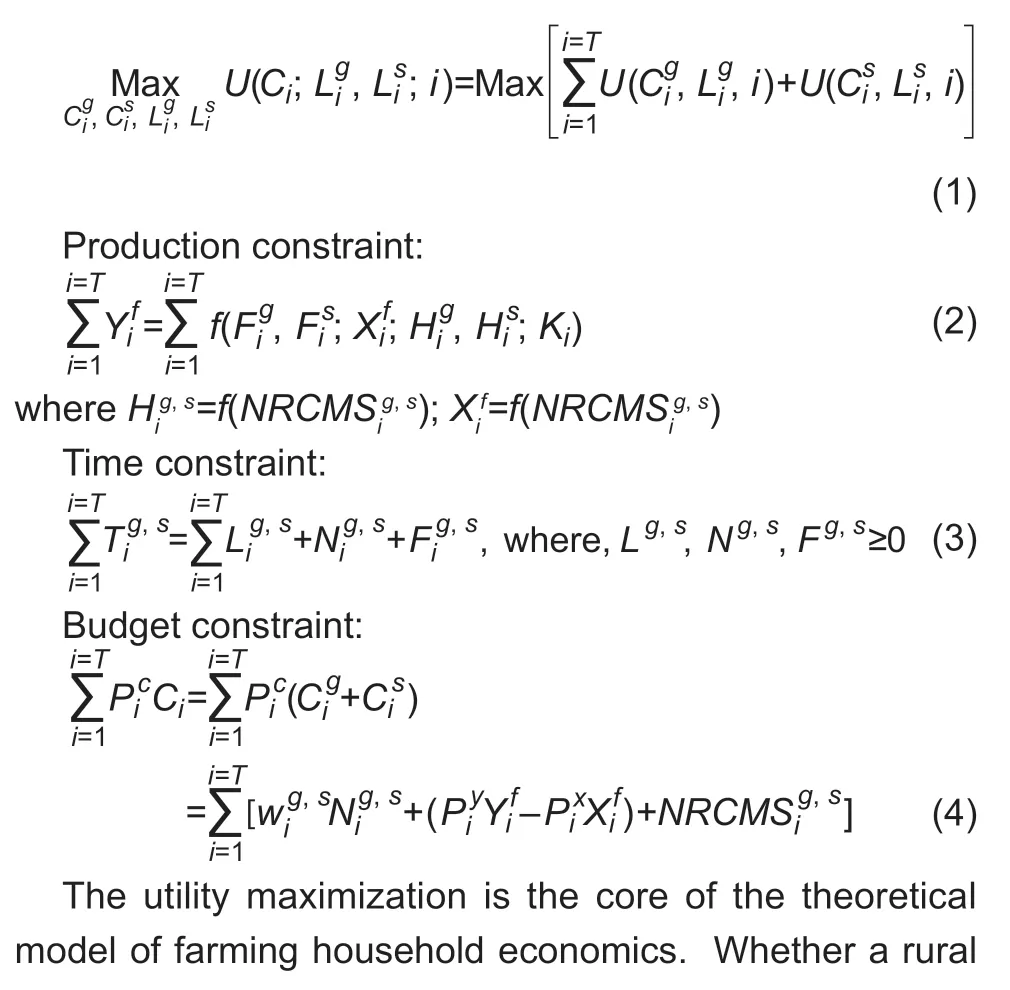
If the partial derivative is positive,it implies the NRCMS participation enhances labor productivity and raises labor supply; the substitute effect dominates. In contrast,if the partial derivative is negative,it implies the NRCMS participation provides the incentive for more leisure time.Labor supply declines with the income effect. It is required to explore the net effect of NRCMS on rural household income by empirical research.
3.2.Econometric model
Based on the above theoretical framework,we develop the econometric model by using the large-scale micro-survey data to test the impact of the NRCMS on the health poverty alleviation of rural households in China. According to eq.(6),we take the first order condition with respect to the NRCMS participation for utility-maximization to obtain the impact of the NRCMS on rural household income can be expressed as:

whereIncomejdenotes thejth household income. If it is lower than the poverty line,then it defines the households up to thejth are in poverty; the rest of households are not in poverty. We can replace the income variable by the discrete bivariate random variable,Povertyj,in which
The system factor,NRCMSj,the core independent variable in our study,indicates whether the householdjparticipates in the NRCMS to determine the poverty. The vectorΠsummaries the other explanatory variables other than the participation in NRCMS,including the household labor force vector variables,the head of household vector variables,the family living condition vector variables,and the community variables. In order to control the heterogeneous impact by regional differences on empirical results,we introduce the regional dummy variables in whichα0is a constant term;α1andα2are parameters to be estimated;andε0is the random error term.
A cry came up in answer, O servant of God! we have been in the well a long time; in God s name get us out! After trying a thousand schemes, I drew up two blind women
The household labor force vector variables include the average age of household labor,the average schooling years of household labor,and the number of male labor.As suggested by Chenget al.(2014) to illustrate the nonlinear impact,we add the square terms of the average age and the schooling years of household labor. The head of household vector variables include gender,age,education,marriage,and mental status which is also considered in Huang (2017). Family living condition vector variables include whether family members are hospitalized,water quality and fuel types for cooking,educational expense,and the value of durable good consumption measured in Baiet al.(2013). The community vector variables count the condition of public facilities,the neighborhood assistance,the distance to town,and the landform of the village (Qi 2011; Huang 2017).
Unlike universal insurance,it is a self-decision making for a rural household to participate in the NRCMS. In the enrollment process,although all levels of local governments have done a lot of promotion,the central government still insists on the principle of voluntary participation.Participation in the NRCMS will have a certain impact on the poverty (income) of rural households; on the other hand,the poverty (income) of rural households will also affect the decision to participate in the NRCMS. As a result,the endogenous issue exists between the poverty variable and the NRCMS participation variable to cause the possible biased estimates in the regression results. To resolve the problem,we follow the setting in Qinet al.(2014,2018) to adopt the NRCMS participation rate in counties as the instrumental variable for household participation.This variable is highly correlated to whether a household participates in the NRCMS but relatively independent from the household poverty (income) to serve as an ideal instrumental variable (Wooldridge 2018).
It is an appropriate choice of the Probit model to construct the estimated equation in eq.(9) in which a dichotomous dependent variable is associated with the large sample size.If the test results indicate an endogenous problem between the variables,then we will switch to the IVProbit model for estimation. Otherwise,the ordinary Probit model is accurate enough to dominate. To reduce the data anomalies,we also take the logged value of the educational expense and the value of durable good consumption. In the next section,there are three empirical tests to verify the impact of NRCMS on rural household poverty alleviation. First,we use the China’s national poverty line as the dependent variable. Then a heterogeneity test follows for varied income groups and regional differences. Finally,we use the World Bank poverty line as the dependent variable to perform a robustness test.
4.Results and discussion
4.1.IVProbit model
Table 2 shows the regression results of the IVProbit model of the impact of the NRCMS on rural households’ health poverty alleviation. Model (1) is the basic model that includes the characteristics of household labor,head of households,family living condition,and regional dummy variables. Model (2) is an expansion to include additional community characteristics. The results of the endogenous test (i.e.,the Wald test) indicate that both models reject the exogenous null hypothesis at significantly lowP-values at 0.0300 and 0.0103,respectively. It is noted that the IVProbit model using the instrumental variable method resolves the serious endogenous problems successfully in both models. In Model (1),the coefficient sign of whether to join the NRCMS is negative at a significance level at 5%. It confirms that the NRCMS significantly reduces the probability of rural households falling into poverty. The coefficient of the same NRCMS variable in Model (2) even decreases more from–1.4148 to–2.1018 at a significance level of 1%. The result implies that the positive impact of the NRCMS on rural households’ health poverty alleviation is not only confirmed but also becomes more substantial if the community characteristic variables are considered.
We ignore the possible correlation between the two core independent variables,NRCMS participation and hospitalization here. First the correlation coefficient of NRCMS participation and hospitalization is only 0.0652 to confirm the independence. Second,as Sunet al.(2009)indicated,the low compensation ratio of NRCMS doesnot reduce the participating rural households’ burden of medical expenses. The total out-of-pocket payments of hospitalization may even increase after NRCMS participation (Wagstaff and Lindelow 2008; Wagstaffet al.2009). The coefficient of hospitalization measures that,if at least one family member was sick and hospitalized in the past year,whether the household’s risk of falling into poverty is increased or not. Table 2 shows that the coefficients in both models are positive at a significance level of 5%. The result indicates that household members’ illness is one of the key causes to trap a rural family in poverty. From medical service providers’ perspective,China’s medical costs have been rising rapidly in recent years creating a huge financial burden on patients. From the perspective of medical service takers,once a family member is hospitalized for an illness,the hospitalized is out of the labor market and requires the care from the other family members. The household income can drop significantly due to the double loss of household labor force. Compared with urban households,rural residents generally face limited channels of earnings.Once a family member needs to be hospitalized,the adverse impact on household income and development is greater than that on the other.
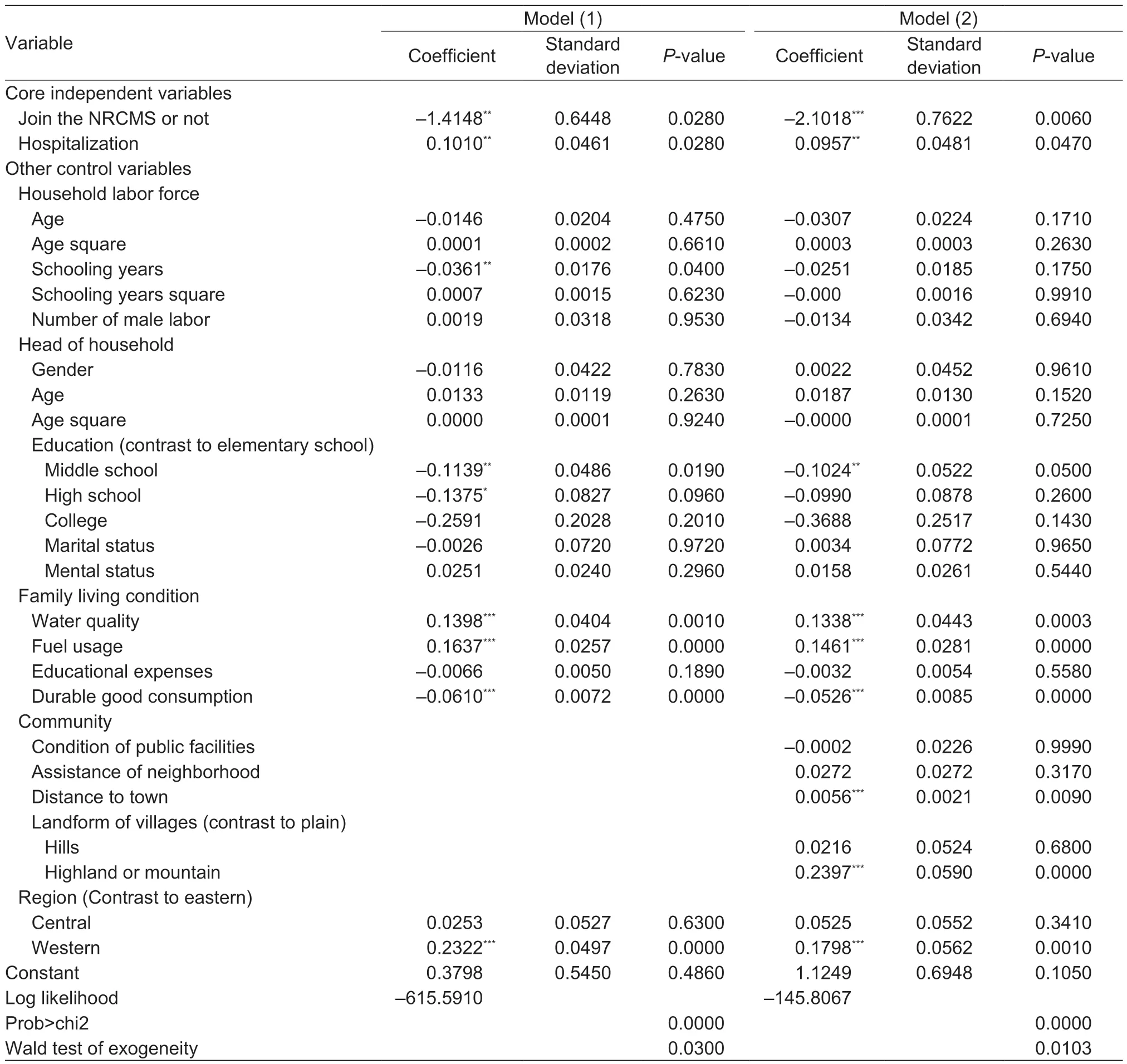
Table 2 Results of IVProbit model for the impact of New Rural Cooperative Medical Scheme (NRCMS) participation
The results of some other significant variables are also noteworthy. In Model (2),among the household labor force variables,the older the average age,the lower the probability of the household falling into poverty. More working experiences and a higher share of income based on working experiences can explain the result. The longer the schooling years of the household labor force also significantly reduce the probability of falling into poverty.It is expected to see a more educated labor can adopt modern agricultural production skills well and fit the current production regulations quickly to improve the household income. The household head variables results show that gender makes no difference in the probability of falling in poverty. As the age of the head of household increases,the probability of the family falling into poverty increases,but the impact is non-linear. All the education levels,marital status,and mental status of the household head have no significant effect on poverty alleviation.
4.2.Heterogeneity test
Table 3 shows the heterogeneity testing results for the impact of the NRCMS on the rural households’ poverty alleviation in two dimensions,income and regions. Income,divided into four groups,were categorized equally according to the annual per capita household net income,as the lowincome group,the lower-middle-income group,the uppermiddle-income group,and the high-income group. Regions,divided into three groups for interviewed households were the eastern region,the central region,and the western region. The results show that the NRCMS significantly reduced the probability of falling into poverty for the rural households in the low-income group and lower-middleincome group with the significantly estimated coefficients–1.8279 and–3.8739,respectively. It implies that the NRCMS has the greatest impact on lower-middle-income households for poverty alleviation. The lower-middleincome group is also the target group most vulnerable to falling back into poverty once bailed out. Different from the impact of residential insurance in the urban area (Huang 2017),the participation of the NRCMS for rural households does not exhibit a “moving-on-up-to-the-target” effect; that is,only the higher income group has a greater and growing participation rate in health insurance. It indicates that the NRCMS has achieved the expected policy goal to reduce the probability of falling into poverty for lower-income people.The grouping results by region show that the impact of NRCMS in the western region is particularly significant. In China,the overall economic and social developments are relatively slow in the western region. The rural residents in the western region are more vulnerable to family risks such as illness or accident and have fewer channels to resist risks. The results also show that the participation of NRCMS has effectively reduced the risk to fall into povertyfor rural households in the western region.
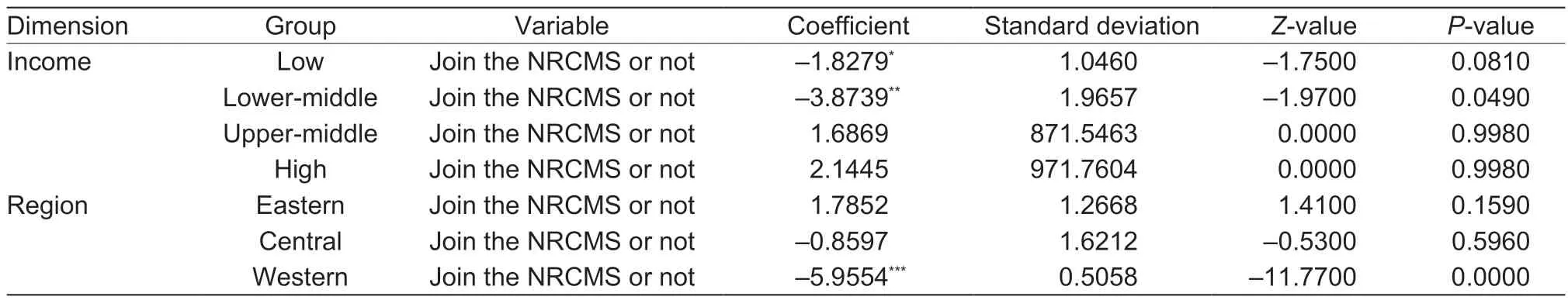
Table 3 Results of heterogeneity test for the impact of New Rural Cooperative Medical Scheme (NRCMS) participation1)
4.3.Robustness test
Table 4 shows the results of the robustness test on the impact of NRCMS. We adopt the World Bank’s poverty line as a benchmark to test whether the NRCMS has a stable impact on poverty alleviation in rural China. Similar to Table 3,the Model (1) and Model (2) in Table 4 exhibit the basic model and the extended model,including community characteristic variables. The results of both models confirm the robustness of the significant positive impact of NRCMS participation on rural household poverty alleviation. All the coefficient signs and statistical significances of variables are consistent with those in Table 2 by using the China’s national poverty line as the standard.
It is a common goal for all nations in the global community to eliminate poverty and promote prosperity. Diverse in natural resources,human capital,government policies,and economic development,every country worldwide faces the poverty problem at varied stages. Global organizations such as the World Bank and the United Nations have been working hard in poverty reduction. Since the 21st century,the progress to resolve global poverty reduction has been remarkable in East Asia,the Pacific,and South Asia. Among those countries,China has been contributing substantially to poverty reduction in the world. Although the extreme poverty rate has dropped,new types of poverty have alsoemerged around the world. For example,the proportion of people without health facilities in East Asia and the Pacific has risen; the income of the bottom 40% of the sub-Saharan Africa’s population has declined; East Asia,the Pacific,as well as the Latin America and the Caribbean,have the most prominent transfer of poverty to the rural areas. The focus of global geographic poverty has also shifted from South Asia to the African continent (Liet al.2019). Just a single disease,Malaria,causes Africa to lose 1.30% of GDP each year (WHO 2016). China has been willing to share the experience of poverty alleviation,based upon its diverse geographical regions and economic developments,especially with the developing countries and regions.
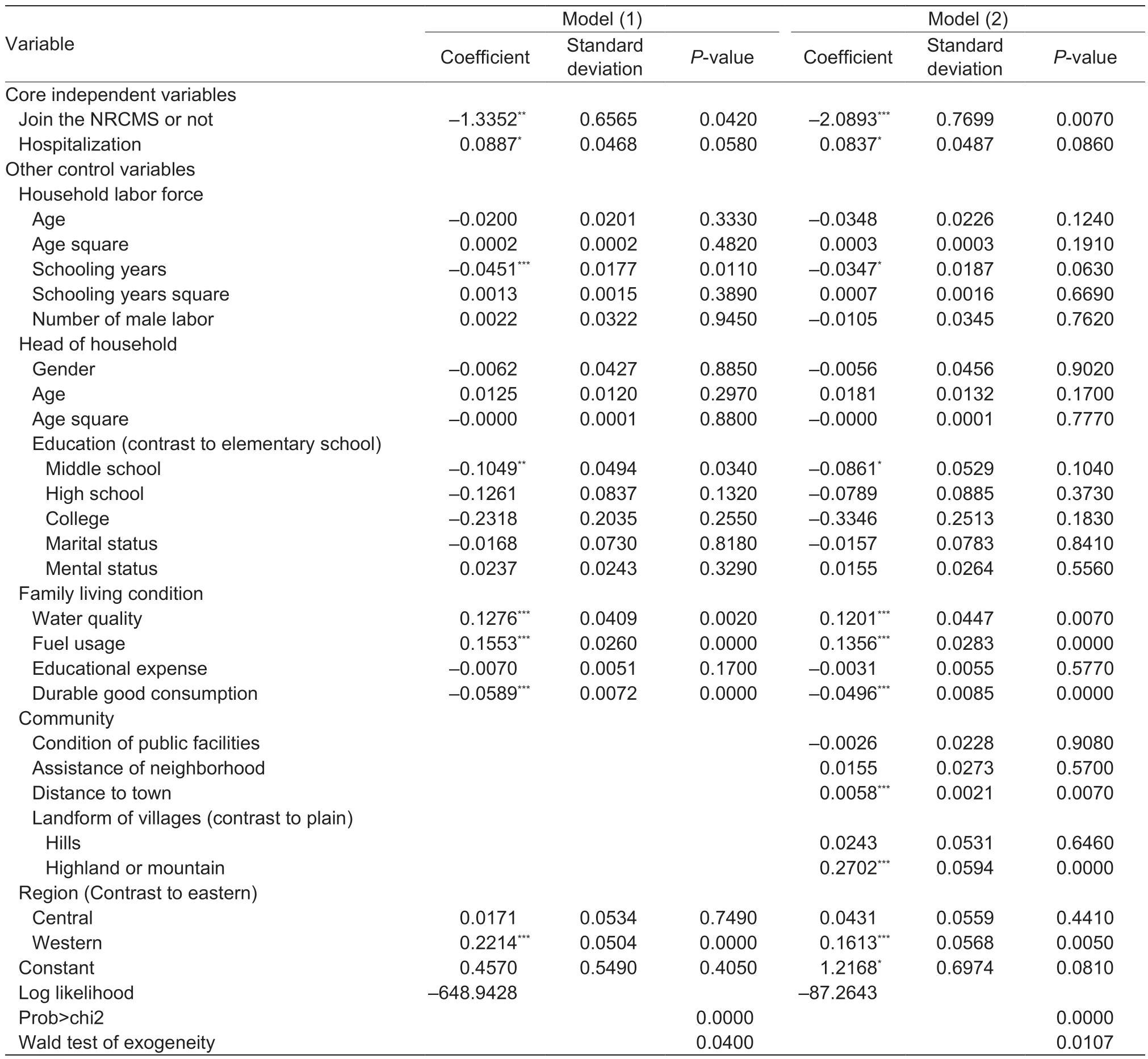
Table 4 Results of robustness test for the impact of New Rural Cooperative Medical Scheme (NRCMS) participation
5.Conclusion and policy recommendations
This study investigates the impact of the New Rural Cooperative Medical Scheme (NRCMS) on rural households for poverty alleviation in China.We employ the instrumental variable method,the IVProbit model,to analyze the national data from the rural-resident field survey by the China Family Panel Studies (CFPS) in 2016 and test the results empirically.The China’s national poverty line serves as a benchmark for the dependent variable proxy; it is also grouped with the two dimensions of income and region to test the heterogeneity. We also use the World Bank poverty line as another benchmark for the dependent variable proxy to test the robustness of the empirical results. Our results indicate that,first,NRCMS has significantly reduced the probability of Chinese rural households trapped into poverty,according to either China or the World Bank poverty line.The high risk of back to poverty,caused by the family members who are ill for hospitalization,has been effectively lowered by the support of NRCMS. The positive impact of the NRCMS on poverty alleviation in China is substantial.Second,the impact of NRCMS on rural households’ poverty alleviation vary among different income groups. It bails out the low-income households,especially those in the lowermiddle-income group,from falling back to poverty due to illness. However,the NRCMS plays no role in preventing poverty due to illness for the middle-and high-income groups. Third,the NRCMS substantially moderates the risk of rural households in the western region falling into poverty,much more significant than that on the eastern and central regions. The regional differences exist among the impact of NRCMS on poverty alleviation in China.
The findings in this paper have important policy implications. In order to reduce and eliminate poverty in China,we propose the following for policymaking:First,lift up the actual compensation ratio of the NRCMS. The conventional policy packages for cost control include deductible,cap line,co-pay ratio and compensation scope to limit the moral hazard problem. However,it often ends up in a situation where patients’ actual compensation ratio is significantly different from the nominal compensation ratio.A higher actual compensation ratio of NRCMS is expected to raise the participation rate of rural households for poverty alleviation. Second,reconstruct the payment schedule for the NRCMS. Given the current low per capita funding of the NRCMS,if the cost control of medical services cannot be exercised efficiently,the impact of the NRCMS on rural households’ poverty alleviation will be greatly reduced. For example,the payment method of Diagnosis Related Groups(DRGs) and the prepayment method based on the total medical amount,which has been practiced in the United States and in some pilot regions in China,have shown good control over medical expenses. Third,improve the overall quality of the medical and health service system in the western region. Not only increase the capacity of the township and village-level health institutions,but the local government should also intensify the training of medical staffs. It is also important to promote the local patients seeking medical treatment in the township and village medical institutions associated with the remote technical supports from the higher-level medical institutions in the metropolitan area. By doing so,the number of out-of-county consultations will be reduced to maintain the NRCMS funds to provide insurance for more rural residents. Fourth,reinforce the medical security system for the marginal poor who are at a high risk of falling into poverty at any time. It might be necessary to integrate all the funds from the NRCMS,the critical illness insurance,the medical assistance,and the Red Cross charitable assistance,to coordinate the total usage and payment to achieve the health poverty alleviation. Fifth,provide a healthy environment in rural areas including drinking water safety,clean fuels for cooking,and toilet facilities. It is also important to promote the self-governance of the environment in rural areas. The income of rural households can be also boosted.
Our study can be extended and modified in the following directions. First,how the mechanism of NRCMS affects the rural household health poverty alleviation needs to be explored in depth. The NRCMS is supposed to have complicated effects on health status,labor migration,labor supply,consumption,savings,and investment. The combined impact on household income may take a longer time to prevail. Second,the panel data of CFPS will be investigated to explore the dynamic decision making and equilibrium. The time fixed effect will be also controlled.Third,it is worth exploring the impact of the NRCMS on personal poverty. Although our result indicates that if a person becomes ill,then the whole family is very likely to fall into poverty,the uneven allocation of available resources within a family may lead to quite different results for each individual. More detailed data to distinguish resource allocation among individual members will lead to a more accurate identification for the health poverty alleviation.
Acknowledgements
We gratefully acknowledge the supports by the National Social Science Fund of China (18FGL014),the Key Project of Humanities and Social Science Base of Anhui Province of China (SK2019A0491),the Humanities and Social Science Foundation of the Ministry of Education of China(18YJA790065),the Social Science Foundation of Anhui Province of China (AHSKY2017D01),the Outstanding Scholar Project of Anhui Province of China (gxbjZD12),the Key Project of the Social Science Foundation of Anhui Province of China (AHSKY2020D44),and the 2019 Major Project of the Social Science Foundation of Anhui Province of China (AHSKZD2019D04).
Declaration of competing interest
The authors declare that they have no conflict of interest.
杂志排行
Journal of Integrative Agriculture的其它文章
- Paths out of poverty
- The power of informal institutions:The impact of clan culture on the depression of the elderly in rural China
- Does empowering women benefit poverty reduction? Evidence from a multi-component program in the lnner Mongolia Autonomous Region of China
- Status and path of intergenerational transmission of poverty in rural China:A human capital investment perspective
- The effects of social security expenditure on reducing income inequality and rural poverty in China
- Synthesize dual goals:A study on China’s ecological poverty alleviation system