Laparoscopic vs. open surgery for gastrointestinal stromal tumors of esophagogastric junction:A multicenter,retrospective cohort analysis with propensity score weighting
2021-03-13WenjunXiongYutingXuTaoChenXingyuFengRuiZhouJinWanYongLiGuoxinLiWeiWang
Wenjun Xiong,Yuting Xu,Tao Chen,Xingyu Feng,Rui Zhou,Jin Wan,Yong Li,Guoxin Li,Wei Wang
1Department of Gastrointestinal Surgery,Guangdong Provincial Hospital of Chinese Medicine,the Second Affiliated Hospital of Guangzhou University of Chinese Medicine,Guangzhou 510120,China;2The Second Clinical Medical College,Guangzhou University of Chinese Medicine,Guangzhou 510405,China;3 Department of General Surgery,Nanfang Hospital,Southern Medical University,Guangzhou 510515,China;4Department of General Surgery,Guangdong Academy of Medical Science,Guangdong General Hospital,Guangzhou 510120,China;5Department of General Surgery,the Third Affiliated Hospital of Southern Medical University,Guangzhou 510500,China
Abstract Objective:Laparoscopic resection is increasingly performed for gastrointestinal stromal tumors (GISTs).However,the laparoscopic approach for GISTs located in the esophagogastric junction (EGJ-GIST) is surgically challenging.This study compares the efficacy of laparoscopic surgery and the open procedure for EGJ-GIST through the propensity score weighting (PSW) method.Methods:Between April 2006 and April 2018,1,824 surgical patients were diagnosed with primary gastric GIST at four medical centers in South China.Of these patients,228 were identified as EGJ-GISTs and retrospectively reviewed clinicopathological characteristics,operative information,and long-term outcomes.PSW was used to create the balanced cohorts.Results:PSW was carried out in laparoscopic and open-surgery cohorts according to year of surgery,sex,age,body mass index (BMI),tumor size,mitotic rates and recurrence risk.After PSW,438 patients consisting of 213 laparoscopic (L group) and 225 open surgery (O group) patients were enrolled.After PSW,the following measures in the L group were superior to those in the O group:median operative time [interquartile range (IQR)]:100.0(64.5-141.5) vs. 149.0 (104.0-197.5) min,P<0.001;median blood loss (IQR):30.0 (10.0-50.0) vs. 50.0 (20.0-100.0)mL,P=0.002;median time to liquid intake (IQR):3.0 (2.0-4.0) vs. 4.0 (3.0-5.0) d,P<0.001;median hospital stay(IQR):6.0 (4.0-8.0) vs. 7.0 (5.0-12.0) d,P<0.001;and postoperative complications (10.3% vs. 22.7%,P=0.001).The median follow-up was 55 (range,2-153) months in the entire cohort.No significant differences were detected in either relapse-free survival (RFS) [hazard ratio (HR):0.372,95% confidence interval (95% CI):0.072-1.910,P=0.236) or overall survival (OS) (HR:0.400,95% CI:0.119-1.343,P=0.138) between the two groups.Conclusions:Laparoscopic surgery for EGJ-GIST is associated with the advantages of shorter operative time,reduced blood loss,shorter time to liquid intake,and shorter length of stay,all without compromising postoperative outcomes and long-term survival.
Keywords:Esophagogastric junction;gastrointestinal stromal tumor;laparoscopic surgery;open surgery;propensity score weighting
Introduction
Gastrointestinal stromal tumors (GISTs) originate from the interstitial cells of Cajal and are the most common mesenchymal tumors of the digestive tract.GISTs may occur in any part of the digestive system but gastric GISTs(gGISTs) account for 50%-70% and are the most common primary tumors (1).The body of the stomach is by far the most common location of the primary tumor (70%-82%),while tumors at the esophagogastric junction (EGJ)contribute a small percentage (5.8%-13.5%) to the overall incidence (2-4).
Surgical resection,when feasible,has become the main treatment of choice for GISTs in recent years.With the development of laparoscopic techniques and instruments,laparoscopy has rapidly become a preferred approach,especially for gGISTs (5).Recent studies have demonstrated that efficacy of laparoscopic surgery for gGISTs is comparable to that of the open approach and even better with respect to short-term outcomes (2,6,7).
The indication for a laparoscopic procedure depends on the location,shape and size of the gGIST.The latest National Comprehensive Cancer Network (NCCN) and European Society for Medical Oncology (ESMO)Guidelines suggest that a laparoscopic resection may be considered for gGISTs in favorable anatomic locations(such as the greater curvature or anterior wall of the stomach) and discourage its use in patients who have large tumors (8,9).However,tumors located in the lesser curvature or posterior wall of the stomach,at the cardia,or at the prepyloric region were classified as unfavorable locations (10).Notably,the laparoscopic approach for GISTs located in the esophagogastric junction (EGJGIST) is rarely reported because of the complex anatomical factors and the difficulty of preserving cardia function,which is technically challenging (11,12).
In our previous study,we carried out four types of laparoscopic resection for EGJ-GIST.Surgery in all patients was completed successfully without operative complications,and no patient experienced recurrence within the follow-up period (13).However,this singlecenter,small-sample report does not reflect the overall status of surgical treatment for EGJ-GIST in China.There remain limited comparative data to date on the long-term outcomes in laparoscopic resection and open surgery for EGJ-GIST.
Hence,we present a multicenter,retrospective study including patients with EGJ-GIST who underwent radical excision in four medical centers in China from April 2006 to April 2018.Selection bias was eliminated through propensity score weighting (PSW).The primary purpose of this study is to compare short-term efficacy and long-term outcomes of laparoscopicvs.open surgery for EGJ-GIST.
Materials and methods
Patients
This is a retrospective,multicenter,cohort study in China.From April 2006 to April 2018,there were 1,824 patients diagnosed with primary GIST who underwent resection in the Guangdong Provincial Hospital of Chinese Medicine,Guangdong General Hospital,Nanfang Hospital of Southern Medical University,and the Third Affiliated Hospital of Southern Medical University.Among them,228 patients with primary GISTs located in the EGJ were included in this study.All operations were performed by experienced surgeons.Of these patients,157 underwent a laparoscopic surgery (L group) and 71 underwent an open procedure (O group).Patients’ age,sex,body mass index(BMI),tumor size,operative duration,blood loss,time to liquid intake,length of postoperative hospital stay,postoperative recovery and complications,and pathological results were reviewed.Risk stratification was evaluated according to the modified National Institutes of Health(NIH) risk classification scheme (14).The complications were classified according to the Clavien-Dindo classification scheme (15).Approval was obtained from the Institutional Review Board of Guangdong Provincial Hospital of Chinese Medicine and the registration number was ZE2020-298.
After PSW,438 patients were selected for the comparison,213 with laparoscopy (L group) and 225 with open surgeries (O group).The flow diagram for the study subject screening and group assignment is shown inFigure 1.
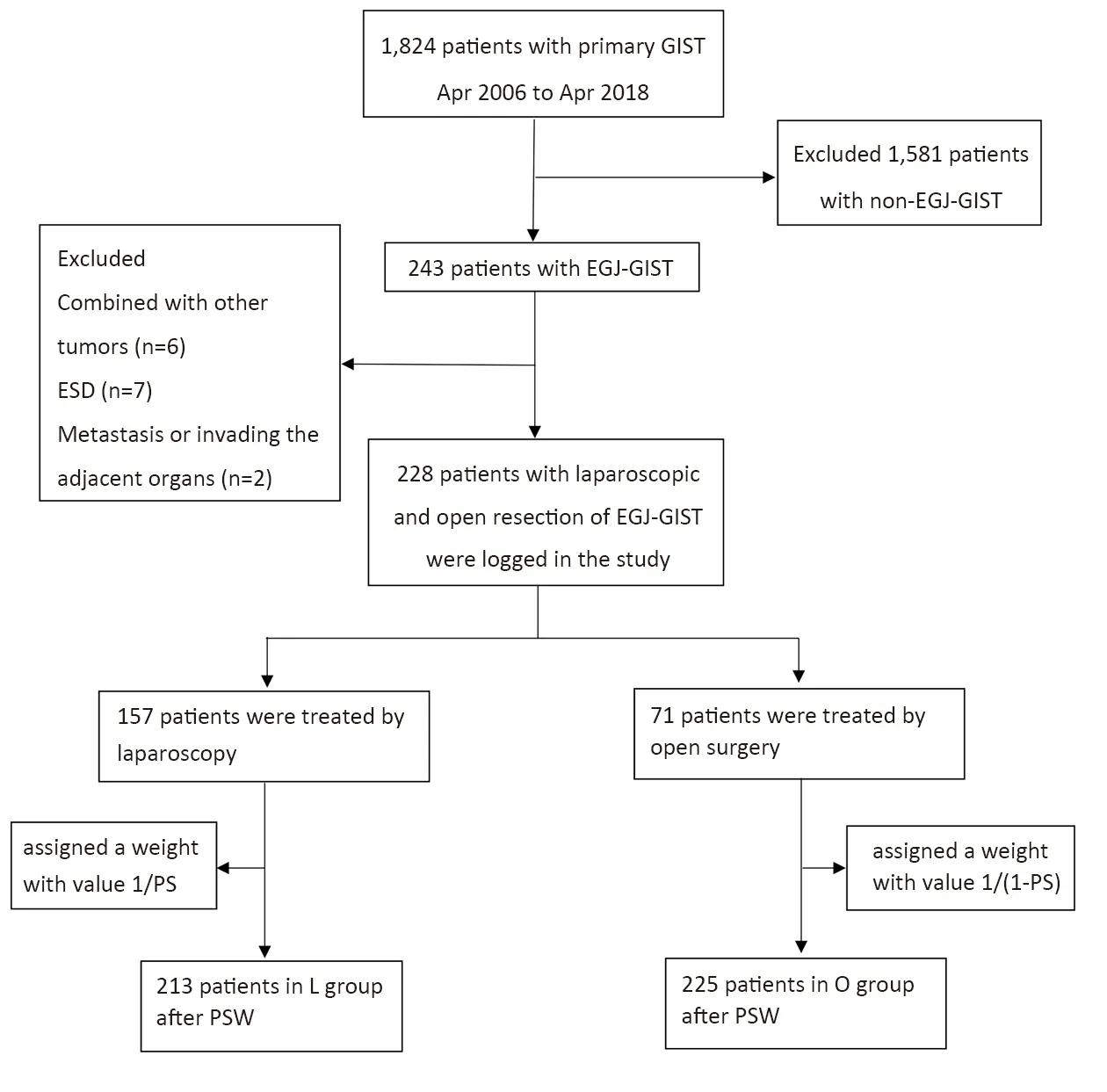
Figure 1 Flow diagram extracting eligible cases for comparison,GIST,gastrointestinal stromal tumor;EGJ-GIST,gastrointestinal stromal tumor in esophagogastric junction;ESD,endoscopic submucosal dissection;PS,propensity scores;PSW,propensity score weighting.
Definition of EGJ-GIST
EGJ-GIST is defined as a gGISTs with an upper border of less than 5 cm from the esophagogastric line (16).
Surgical procedure
Laparoscopic approach
Following general anesthesia,patients were placed in the supine position with legs separated.Pneumoperitoneum was established to an insufflation pressure of 10-15 mmHg.Five trocars were used.Before the procedure,we used a gastroscope to identify the tumor location and estimate the distance between the upper border of the tumor and the esophagogastric line before the procedure.
There are four types of laparoscopic resection for EGJGIST:wedge resection;resection by opening whole layers of the stomach wall and closing with sutures or a linear stapler;mucosa-preserving resection;and proximal gastrectomy with pyloroplasty.After mobilization,one of these was selected according to various criteria such as tumor location and size,distance between the upper border of the tumor and esophagogastric line,and manner of growth.
Open approach
On Sundays my father always wore that dull(,) gray apron1() – the one with the race cars all over it. The ritual2(,) began after breakfast when Dad always announced: Go ahead everyone. I ll take care of the dishes! With that my mother disappeared into the folds of the Sunday paper. Off came the suit coat he had worn to church that morning. Up went the shirtsleeves() . On went that apron. For the next hour Dad did the dishes, singing ballads3(,) like I Had a Hat When I Came In and Who Put the Chow in Mrs. Murphy s Chowder?
Patients under general anesthesia were placed in the supine split-leg position.A midline incision with 8-15 cm was typically performed to expose the tumors adequately.All incisions were covered using a protective sleeve.Wedge resection,proximal gastrectomy,total gastrectomy,or multiple organ resection was performed,depending on the tumor size and location.
Follow-up
The clinical data were collected from medical records,and the survival information was obtained from telephone or outpatient visit follow-up by investigators at each medical center.The follow-up data included postoperative adjuvant therapy,survival and recurrence.The latest follow-up date for the study was in June 2018.Recurrent disease was defined as new lesions identified by postoperative endoscopy,abdominal computed tomography scan,or magnetic resonance imaging;recurrent disease was found most often in the liver and/or peritoneum.In addition,the recurrence event was confirmed by an experienced team(8,9).Relapse-free survival (RFS) was defined as the time from surgery to the first recurrence of disease and overall survival (OS) was calculated as the time from surgery to the date of death.Median follow-up time was 55 (range:2-153) months in the entire cohort.
Statistical analysis
Data management and statistical analyses were performed usingIBM SPSS Statistics (Version 20.0;IBM Corp.,New York,USA) and R software (Version 4.0.3;R Foundation for Statistical Computing,Vienna,Austria).PSW was implemented to reduce covariate confounding.Propensity scores (PS),reflecting the conditional probability of each surgical approach,were calculated by generalized linear models,in which the connecting function was logit fuction(family=binomial).Patients in the laparoscopy cohort were assigned a weight with the value 1/PS,while patients in the open cohort were assigned a weight with the value 1/(1-PS).The propensity model included variables that may have affected the distribution of patients in different operative types or outcomes including year of surgery,sex,age,BMI,tumor size,mitotic rate and recurrence risk.In propensity score matching (PSM),seven covariates (year of surgery,sex,age,BMI,tumor size,mitotic rate and recurrence risk) that may have affected the distribution of patients in different operative types or outcomes were selected to calculate the propensity score.The reason for choosing 2010 as the cutoff point for year of surgery was that the year was when imatinib was approved in China to be effective for use as adjuvant therapy for primary GIST after complete resection (10).
Quantitative data were normally distributed and homogeneity of variance was showed as,using thettest for comparison.Non-normal distribution of measurement quantitative data was represented as the median and interquartile range (IQR),using the Wilcoxon rank-sum test.Differences in categorical data between groups were determined by the Chi-square test or Fisher’s exact test.Survival was calculated using the Kaplan-Meier method,and Cox regression was used for comparing the differences between the groups.The inverse probability of treatment weighting (IPTW) was used to estimate the effect value of factors.Cox regression was performed within the weighted sample to compare survival curves by study cohorts.A P<0.05 was considered to be significant.
Results
In total,228 patients with EGJ-GIST were enrolled:64 patients from Guangdong Provincial Hospital of Chinese Medicine,66 from Guangdong General Hospital,62 from Nanfang Hospital of Southern Medical University,and 36 from the Third Affiliated Hospital of Southern Medical University. Comparisons of demographic data and clinicopathological information between the two groups of patients are summarized inTable 1.There was no statistically significant difference between the baseline characteristics of L and O groups except for BMI.After PSW,a weighted sample of almost perfectly balanced covariates between the L and O group cohorts was created(Table 1),which were the same after PSM.
Tables 2,3show the comparison of intraoperative and postoperative outcomes.The L group was superior to the O group in most characteristics whether before or after PSW,including operative time,blood loss,time to liquid intake,hospital stay,and postoperative complications (allP<0.05),which were the same after PSM except for blood loss (P=0.051).By contrast,after PSW,the distance between the upper border of the tumor to the esophagogastric line was significant (P=0.002).In addition,four patients in the L group were converted to laparotomy because of a particular tumor location,difficulty in visual field exposure,or technical issues with laparoscopy.
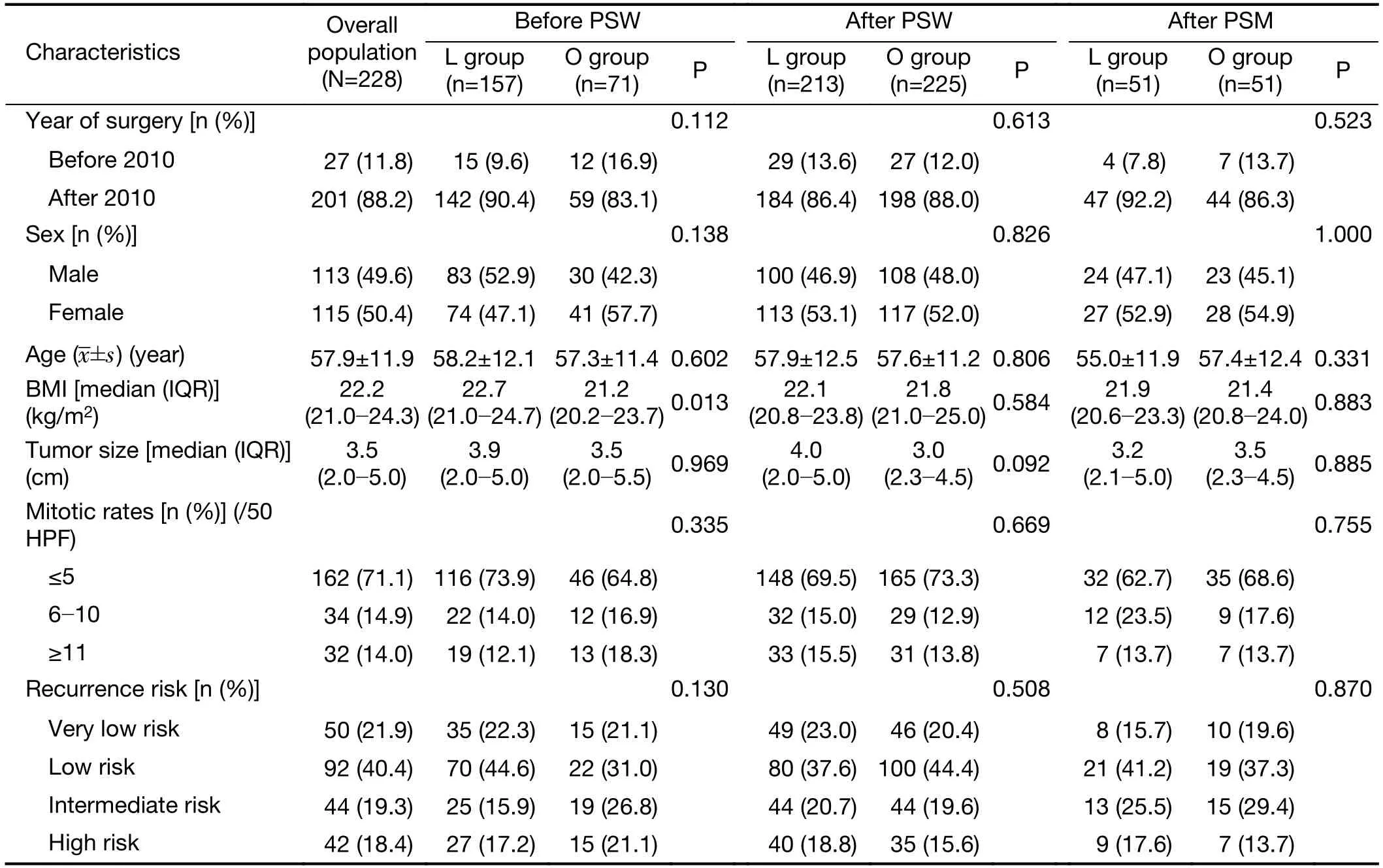
Table 1 Comparison of demographic data and clinicopathological characteristics
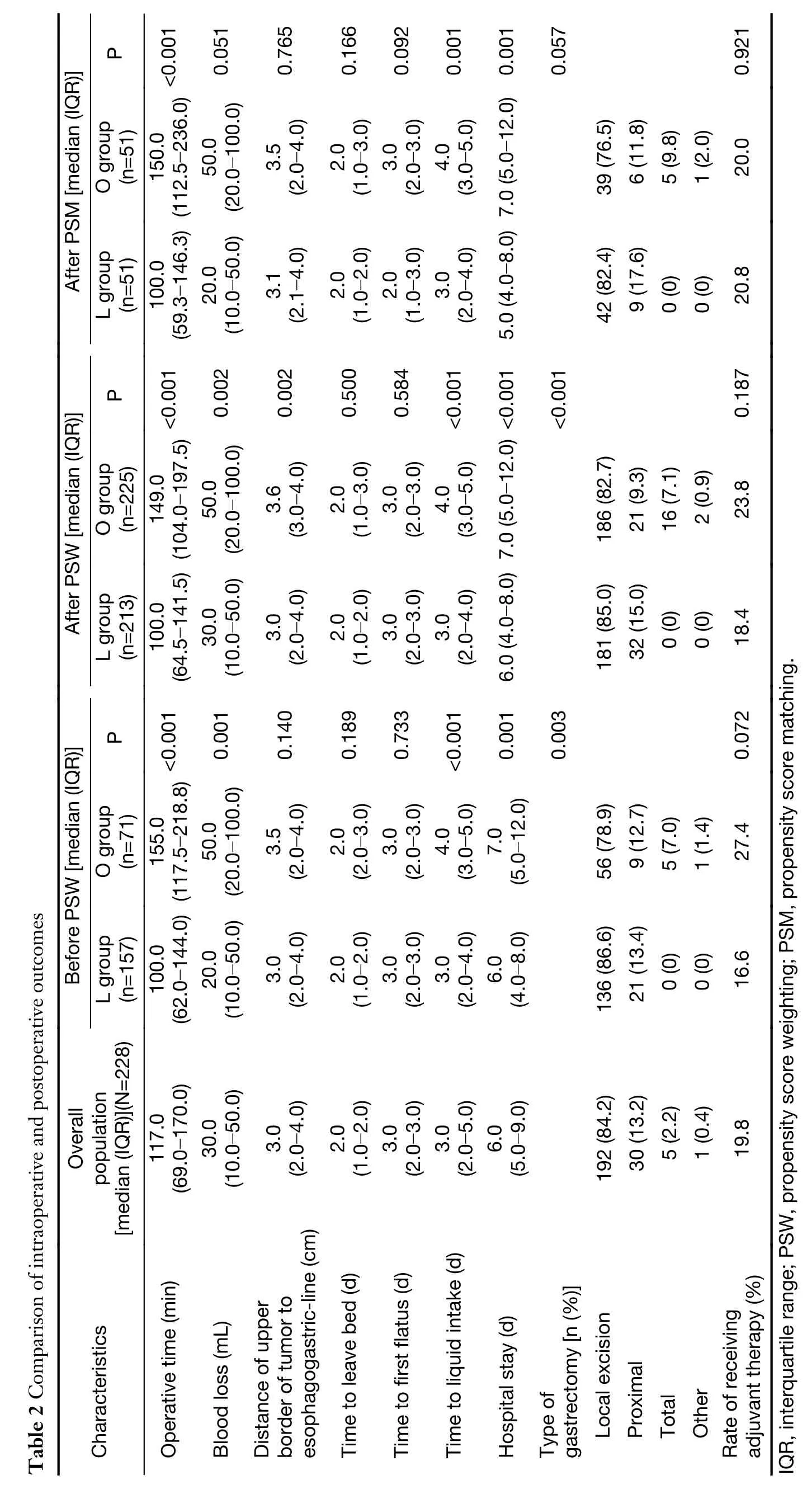
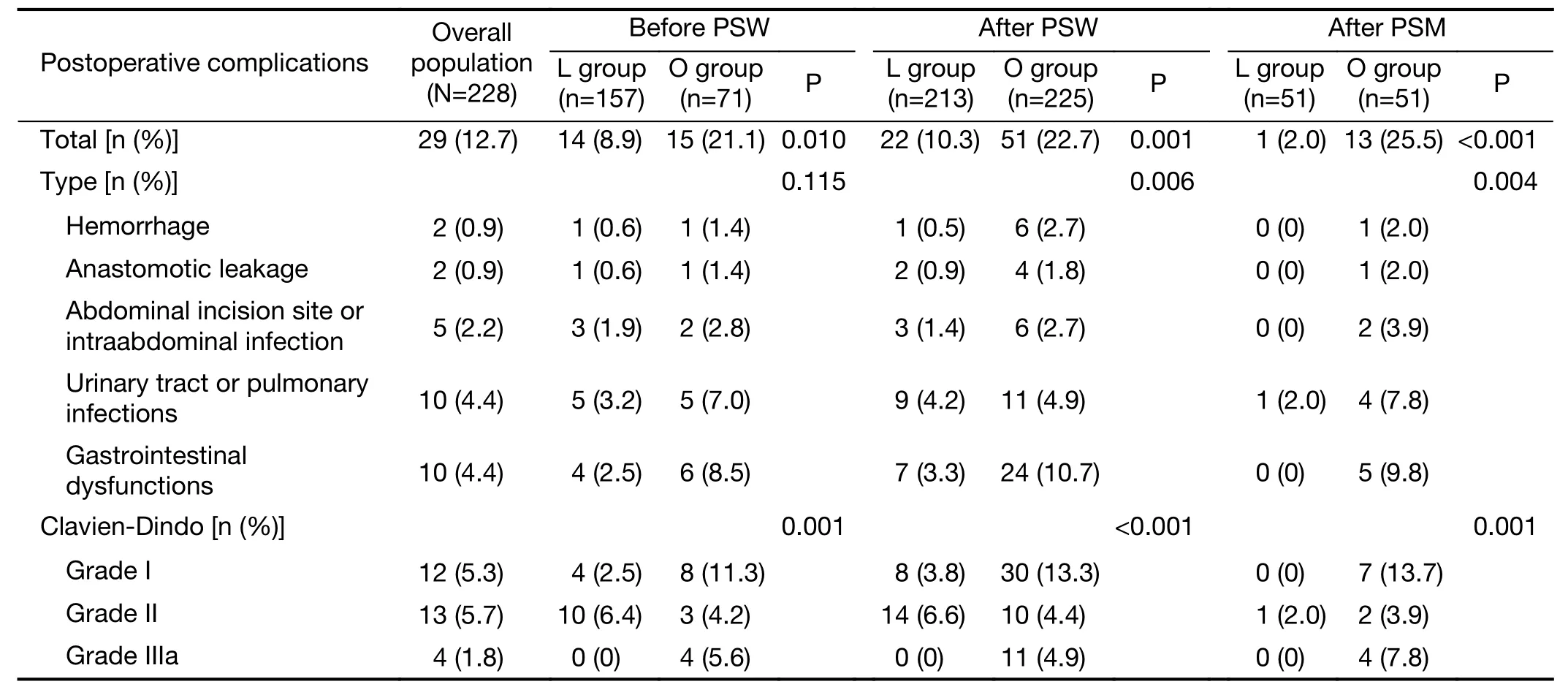
Table 3 Comparison of postoperative complication
Before PSW,the rate of receiving adjuvant therapy was 16.6% for the L group and 27.4% for the O group(P=0.072,Table 2).The 1-,3-and 5-year RFS rates were 100%,98.2% and 98.2% in L group and 100%,92.8% and 92.8% in the O group,respectively.The 1-,3-and 5-year OS rates were 99.3%,98.4% and 97.0% in the L group and 100.0%,96.1% and 88.5% in the O Group,respectively.There were insignificant differences in RFS(HR:0.366,95% CI:0.074-1.816,P=0.219,Table 4,Figure 2A) and OS (HR:0.294,95% CI:0.082-1.050,P=0.059,Table 4,Figure 2B).
After PSW,the rate of receiving adjuvant therapy was 18.4% for the L group and 23.8% for the O group(P=0.187,Table 2).There were insignificant differences in either RFS (HR:0.372,95% CI:0.072-1.910,P=0.236) or OS (HR:0.400,95% CI:0.119-1.343,P=0.138) between the two groups (Table 4).
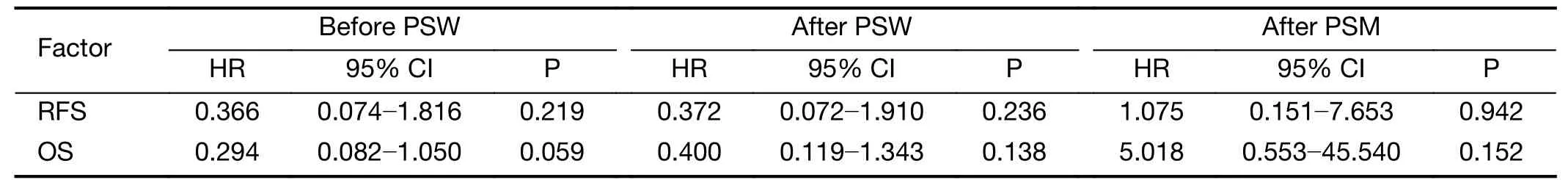
Table 4 Comparison of long-term survival
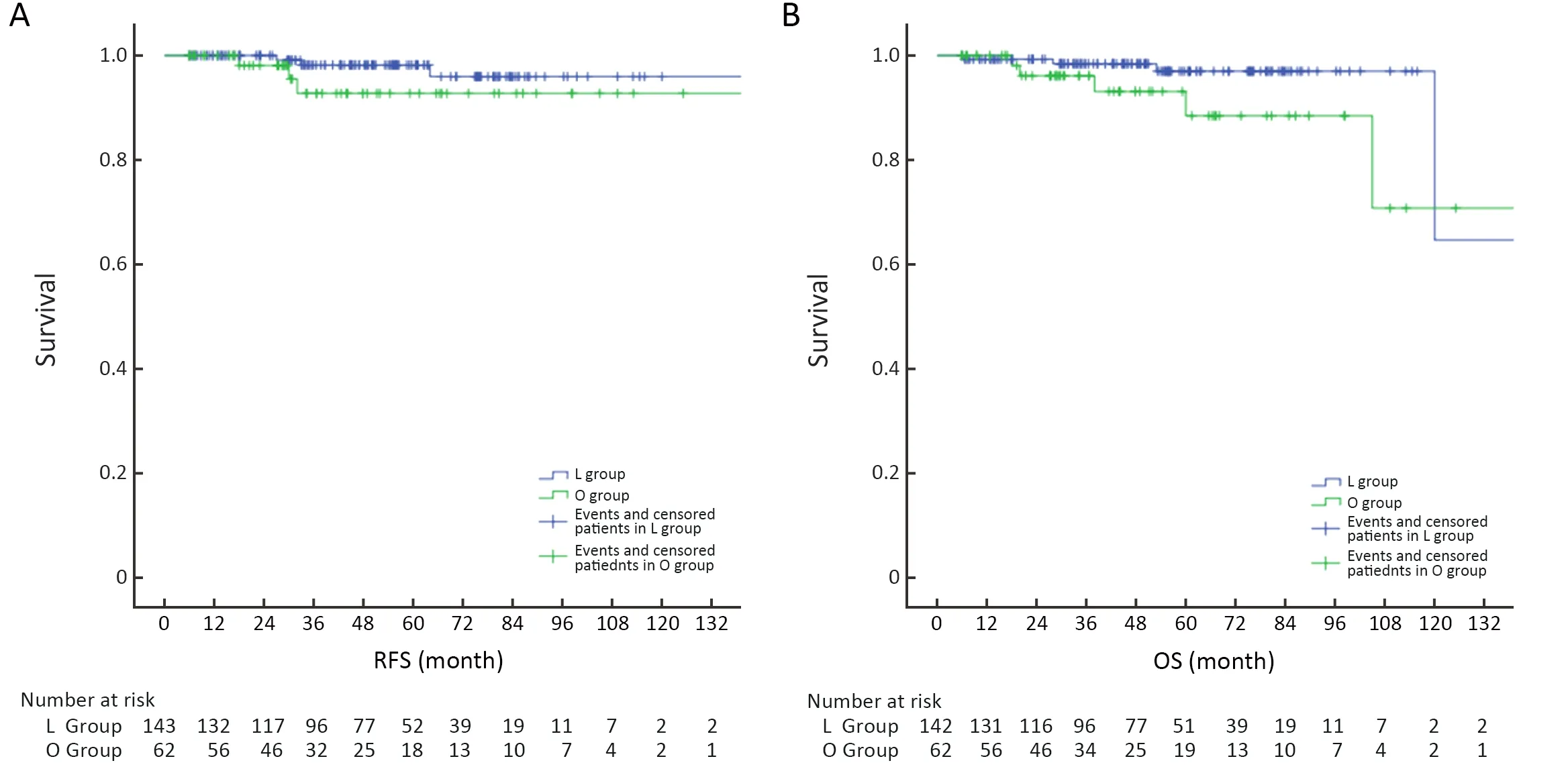
Figure 2 Comparison of RFS and OS.(A) RFS before PSW (P=0.219);(B) OS before PSW (P=0.059).RFS,relapse-free survival;OS,overall survival;PSW,propensity score weighting.
After PSM,the rate of receiving adjuvant therapy was 20.8% for the L group and 20.0% for the O group(P=0.921,Table 2).There were insignificant differences in either RFS (HR:1.075,95% CI:0.151-7.653,P=0.942) or OS (HR:5.018,95% CI:0.553-45.540,P=0.152) between the two groups (Table 4).
Discussion
In the current study,we evaluated the efficacy and safety of laparoscopic surgery for regional and resectable EGJ-GIST and accumulated long-term follow-up data from multiple institutions for comparison with open surgery.Since the first laparoscopic resection was reported by Lukaszczyket al.in 1992 (17),laparoscopic surgery has become the main treatment for GIST patients in recent years.More patients with localized or potentially resectable GISTs prefer laparoscopic to open surgery because it is less traumatic and has a more rapid recovery.Nevertheless,because of the higher risk of tumor rupture and the difficulty of preserving function,the laparoscopic approach for EGJ-GIST is considered technically challenging and is controversial.As is stated in ESMO and NCCN guidelines(8,9),laparoscopic surgery is not encouraged for GISTs located in certain anatomic sites such as the EGJ.In 2018,we reported four types of laparoscopic surgery for EGJGIST.Complications and recurrence within the follow-up period had not been reported in patients who underwent laparoscopic reaction for EGJ-GIST (13),which indicated the safety and feasibility of the technique.
In this retrospective cohort study using laparoscopic resection,we found a median operation time of 100.0 min,median intraoperative blood loss of 20.0 mL,median time to oral intake of 3.0 d,median length of hospital stay of 6.0 d,and a postoperative complication rate of 8.9%.Comparatively,the open reaction was associated with longer operative time,more blood loss,longer time to liquid intake,slower hospital discharge,and higher postoperative complications regardless of whether PSW was performed or not.This might suggest that laparoscopic surgery induces less trauma and facilitates quicker recovery with improved short-term effects,as has been reported in previous studies (2,6,10).
Although there have been advances in laparoscopic technique as well as in minimally invasive surgical instruments,it is still hard to expose the EGJ field in the laparoscopic approach,especially in cases of digestive tract reconstruction.In our study,there were four cases of conversion to laparotomy in the L group.In one case,the tumor was located in the posterior gastric wall and it was difficult to expose the anatomical area via laparoscopy because of extensive abdominal adhesions.Among the others,two tumors were hard to excise laparoscopically because of extensive intra-peritoneal adhesions,and in one case the tumor was estimated to have a high risk of rupture.In addition,intraoperative tumor rupture is a worse prognostic factor than a positive margin because patients with a ruptured GIST have a nearly 100% risk of recurrence (18,19).Consequently,we recommend that the laparoscopic treatment of EGJ-GIST should be carried out only in a medical unit with a strong laparoscopic technology foundation.
Our study shows that operative time in laparoscopic surgery is significantly shorter than in open surgery.Although some studies have reported that laparoscopic resection takes longer operative time than open resection,this might be related to tumor size and location (5,20).In this study,EGJ-GIST tumor size was treated as a covariate,and PSW was used to reduce selection bias.Unlike the findings in Goh’s study and Lee’s study of tumors of similar size and location,operative time in laparoscopic resection was significantly shorter than in open resection in this research (5,20).We considered that might be a result of the abundant laparoscopic experience with GIST resection in this unit.In addition,the distance from the upper border of the tumor to the esophagogastric line became statistically significant after PSW,which might suggest this factor is meaningful in choosing the surgical approach.
It is important for the surgeon to identify EGJ-GIST accurately during laparoscopic resection,and therefore intraoperative endoscopy plays an increasingly important role.In recent years,with the application of intraoperative endoscopy and the development of minimally invasive instruments,laparoscopic endoscopic cooperative surgery is getting more attention.A multicenter study in Japan showed that laparoscopic and luminal endoscopic cooperative surgery was a safe and feasible procedure (4).In this study there were 17 tumors located at the EGJ,but no patient experienced local or distant tumor recurrence during the follow-up period.Additionally,many new laparoscopic methods with endoscopy assistance were investigated,showing that using intraoperative endoscopy provides a safe and effective method of examination for complete resection of EGJ-GIST and the integrity of the cardia (21-23).
With the rapid advances in the development of endoscopic skill and endoscopic instruments,endoscopic resection has been used for treatment of local GISTs (24).There are a number of research studies showing that compared with surgical resection,endoscopic resection is safe and feasible and has a certain advantage in small gastric GISTs,although perforation and postoperative bleeding could not be totally avoided during and after resection (25-27).However,comparative long-term safety studies of endoscopic resection of GIST are lacking,especially for EGJ-GIST.The reason is that it is hard to preserve cardia function and avoid complications such as cardia stenosis and dysfunction of the cardia sphincter in achieving complete resection of the tumor using endoscopy.Consequently,endoscopic resection is not commonly recommended for EGJ-GIST.
Unlike surgery for other solid tumors,lymphadenectomy is not conventionally performed during GIST surgery because nodal involvement is rare in these patients (i.e.,1.1%-3.4% of cases),which not only decreases the surgical trauma but also relates to the quality of long-term survival(28,29).On the other hand,there are few reports and longterm prognosis data on GIST near the EGJ because of this complex anatomical relationship.Furthermore,studies have shown that most of GISTs carry a mutation in theKITgene (9,30-32),which has led to development of imatinib and other successful drugs.Since imatinib was approved in China in 2010 (10) as effective for use as adjuvant therapy for primary GIST after complete resection,it has greatly prolonged the survival time and improved the quality of life of GIST patients (33-35).The latest NCCN and ESMO guidelines recommend imatinib adjuvant therapy for highrisk GIST patients (8,9),while the Chinese consensus guidelines (2017) advocate that patients with moderate and high risk of recurrence as the adaptive population (36).In the current study,before PSW,the rate of receiving adjuvant therapy was 16.6% for the L group and 27.4% for the O group,which was not a statistically significant difference (P=0.054).After PSW,the rate of receiving adjuvant therapy was 18.4% for the L group and was similar when compared to the O group (23.8%) (P=0.187).In addition,one patient received a neoadjuvant therapy.Based on Choi criteria (37),he was assessed at 6 months as having a partial response (PR).He then had laparoscopic resection and was alive during the follow-up period.
At present,the use of laparoscopic treatment compared with that of laparotomy for GIST still remains controversial.Some studies report the oncological outcome of GIST as based on tumor biology rather than resection type (34,35,38),whereas some studies have found the longterm outcome in the laparoscopic approach superior to that of open surgery for tumors in favorable locations (2,10).In addition,some randomized control trials comparing open and laparoscopic approaches for colorectal or esophageal cancer have already observed the positive impact of a laparoscopic approach on OS (39,40).However,few studies have compared the long-term outcome between laparoscopic resection and open resection for EGJ-GIST.
In the present report,we use PSW to overcome the different distributions of covariates in the study,achieving the goals of reducing selection bias and increasing credibility.There was no statistical difference in the RFS and OS between the L and O groups whether before or after PSW,but it has been shown preliminarily that laparoscopy has some advantages for long-term prognosis and survival,especially OS.The advantages of laparoscopic surgery might be shown more definitively with a large enough sample size.
In EGJ-GIST,to determine whether laparoscopic surgery can improve the survival rate and long-term prognosis of patients better than open surgery,we need larger samples and more multicenter and randomized controlled clinical trials.
Conclusions
Laparoscopic resection is a safe and efficacious treatment for EGJ-GIST,providing the advantages of shorter operative time,reduced blood loss,earlier time to liquid intake,and quicker hospital discharge,all without compromising postoperative outcomes and survival.
Acknowledgements
None.
Footnote
Conflicts of Interest:The authors have no conflicts of interest to declare.
杂志排行
Chinese Journal of Cancer Research的其它文章
- Colorectal cancer burden and trends:Comparison between China and major burden countries in the world
- Changing trends of disease burden of gastric cancer in China from 1990 to 2019 and its predictions:Findings from Global Burden of Disease Study
- Clinical characteristics and clinicopathological correlations of bilateral breast cancer in China:A multicenter study from Chinese Society of Breast Surgery (CSBrS-006)
- Multi-center investigation of breast reconstruction after mastectomy from Chinese Society of Breast Surgery:A survey based on 31 tertiary hospitals (CSBrS-004)
- Radiotherapy combined with nimotuzumab for elderly esophageal cancer patients:A phase II clinical trial
- Pattern of No.12a lymph node metastasis in gastric cancer
