Changing trends of disease burden of gastric cancer in China from 1990 to 2019 and its predictions:Findings from Global Burden of Disease Study
2021-03-13TongchaoZhangHuiChenXiaolinYinQiufengHeJinyuManXiaorongYangMingLu
Tongchao Zhang,Hui Chen,Xiaolin Yin,Qiufeng He,Jinyu Man,Xiaorong Yang,Ming Lu,
1Department of Epidemiology and Health Statistics,School of Public Health,Cheeloo College of Medicine,Shandong University,Jinan 250012,China;2 Clinical Epidemiology Unit,Qilu Hospital of Shandong University,Jinan 250012,China;3 Clinical Research Center of Shandong University,Jinan 250012,China
Abstract Objective:China is one of the countries with the heaviest burden of gastric cancer (GC) in the world.Understanding the epidemiological trends and patterns of GC in China can contribute to formulating effective prevention strategies.Methods:The data on incidence,mortality,and disability-adjusted life-years (DALYs) of GC in China from 1990 to 2019 were obtained from the Global Burden of Disease Study (2019).The estimated annual percentage change (EAPC) was calculated to evaluate the temporal trends of disease burden of GC,and the package Nordpred in the R program was used to perform an age-period-cohort analysis to predict the numbers and rates of incidence and mortality in the next 25 years.Results:The number of incident cases of GC increased from 317.34 thousand in 1990 to 612.82 thousand in 2019,while the age-standardized incidence rate (ASIR) of GC decreased from 37.56 per 100,000 in 1990 to 30.64 per 100,000 in 2019,with an EAPC of -0.41 [95% confidence interval (95% CI):-0.77,-0.06].Pronounced temporal trends in mortality and DALYs of GC were observed.In the next 25 years,the numbers of new GC cases and deaths are expected to increase to 738.79 thousand and 454.80 thousand,respectively,while the rates of incidence and deaths should steadily decrease.The deaths and DALYs attributable to smoking were different for males and females.Conclusions:In China,despite the fact that the rates of GC have decreased during the past three decades,the numbers of new GC cases and deaths increased,and will continue to increase in the next 25 years.Additional strategies are needed to reduce the burden of GC,such as screening and early detection,novel treatments,and the prevention of risk factors.
Keywords:Gastric cancer;disease burden;temporal trend;risk factor;prediction
Introduction
Gastric cancer (GC) is a malignant tumor that causes serious disease burden,being the fifth most commonly diagnosed cancer and the third cause of death (1,2).In 2018,there were more than 1,033,701 new cases of GC and an estimated 782,685 deaths from it,worldwide (3).China is a high incidence region of GC (4).According to the 2018 global cancer statistics,456,124 new GC cases and 390,182 deaths were estimated to have occurred in China,accounting for 44.1% and 49.9% of the cases worldwide,respectively (3).The high incidence and mortality in China highlight the urgency of preventing and treating GC.
GC is a multifactorial disease that can be caused by both environmental and genetic factors (5).Some of these factors are not modifiable (such as age,gender,and family genetic history),while others are potentially modifiable(such as smoking,alcohol consumption,and poor dietary habits) (5,6).These potentially modifiable factors make it possible to prevent and control the incidence of GC.Helicobacter pylori(H.pylori) infection is the main risk factor for the development of GC (7).The population infection rate ofH.pyloriis approximately 50% (8,9),while only about 1% of infected cases eventually develop into GC(9).Unhealthy lifestyles,such as smoking and alcohol consumption,also have been found to have a significant association with an increased risk of developing GC (5,6).In addition,dietary factors,such as the intake of salty food and low consumption of fruits and vegetables,may increase the risk of GC development (5).Moreover,sex is also a significant risk factor for GC (5,10),and the differences between the sexes may be attributed to their different lifestyles and dietary habits (5).Therefore,it is of great importance to develop prevention and control strategies for GC according a person’s sex.
China is one of the largest developing countries and has rapid economic growth.As the economy develops,people’s lifestyles and dietary factors change accordingly.It is important and necessary to understand the epidemiological trends and patterns of GC in China,as this is essential for formulating relevant prevention strategies to improve public health.The latest Global Burden of Diseases (GBD)study (2019) provides extensive data on the incidence,mortality,and disability-adjusted life-years (DALYs) of GC from 1990 to 2019,which made it possible for us to understand the disease burden of GC in China.Therefore,in this study,using the latest data of the GBD study (2019)in China,we comprehensively evaluated the national disease burden of GC and its temporal trends in relation to age,sex,and risk factors;and also predicted the numbers and rates of GC incidence and mortality in the next 25 years.Our research results should improve our understanding of the disease burden of GC,help us evaluate the effectiveness of current prevention strategies,and provide a more scientific basis for promoting the establishment of prevention strategies.
Materials and methods
Data sources
The detailed methods of GBD study (2019) have been reported in previous studies (11-15). The data on incidence,mortality,and DALYs were downloaded from the Institute for Health Metrics and Evaluation (IHME,http://ghdx.healthdata.org/gbd-results-tool). The codes used for GBD study analysis can be accessed through the following address:http://ghdx.healthdata.org/gbd-2019/code.In GBD Study,all estimates were generated with 95% uncertainty intervals (95% UIs),which were determined based on the 2.5th and 9.75th-ordered percentiles of 1,000 draws of the uncertainty distribution(14).In the database,we used the following screening rules for this study.First,the location name was“China”and the cause was“Stomach cancer.”Second,we chose“incidence,”“death,”and“DALYs”as measures.
The age-standardized rates for the incidence and mortality of GC were estimated using the World Health Organization (WHO) World Standard Population Distribution (2000-2025).For the prediction of GC burden,the predicted Chinese population was obtained from the United Nations World Population Prospects 2019 Revision,by year,sex,and age (https://population.un.org/wpp/Download/Standard/Population/).
This study was approved by the Ethics Committee of Qilu Hospital of Shandong University.For the GBD is a publicly available database,all participants’ data were anonymous.
Evaluation of GC burden
The incidence and mortality of GC in the GBD dataset were determined in the following ways:1) based on all the data sources that reported GC incidence and mortality(with international disease classification codes),the mortality-to-incidence ratio (MIR) was calculated using a linear-step mixed-effects model (the covariates were Healthcare Access and Quality Index,age,and sex),and the estimates were smoothed and adjusted using spatiotemporal Gaussian process regression (13,15,16);2) we calculated mortality estimates by multiplying cancer register incidence data by the MIR (13,15,16);3) all these data were used as input to follow the Cause of Death Ensemble model process to determine the cancer-specific mortality of GC(13,15,16);and 4) we divided cancer-specific mortality of GC estimates by the MIR to generate incidence (13,15,16).
Statistical analysis
Descriptive analysis for GC incidence,mortality,and DALYs was performed by 5-year age groups,sex,and year;we plotted the temporal trend of these indicators from 1990 to 2019.The age information of incidence and DALYs of GC was considered to be the age at diagnosis,while the age information of the death of GC represented the age at death.Age was divided into 18 age-specific groups by every 5 years,and the ages of 0-14 years were combined into one age group.The indicator of estimated annual percentage change (EAPC) was used to reflect the temporal trend of the age-standardized incidence rate(ASIR),the age-standardized mortality rate (ASMR),and the age-standardized DALYs rate.EAPC was calculated according to a regression model fitted to the natural logarithm of the rate,namelyln(rate)=α+β× (calendar year)+ε.EAPC was defined as 100 × (exp(β) -1);its 95%confidence interval (95% CI) was also calculated in the fitted model (16,17).
For the risk factors,the comparative risk assessment(CRA) framework was used to estimate the proportion of DALYs attributable to two well-established risk factors for GC by age and sex:smoking and the high-sodium diet(12,13).CRA was conducted through the following six key steps:1) including risk-outcome pairs with convincing or probable evidence based on research (18,19);2)summarizing the relative risk of potential exposure based on systematic reviews and meta-regression (18,19);3)estimating the exposure levels and distributions using the spatiotemporal Gaussian process regression,DisMod-MR 2.1,and other methods (18,19);4) defining the theoretical minimum risk exposure level as the exposure level associated with the minimum risk determined from published trials and cohort studies (18,19);5) calculating the population attributable fractions (PAFs) and attributable burden (18,19);and 6) estimating the PAFs and attributable burden for combinations of risk factors by considering the mediation of different risk factors through other risk factors (18,19).
The package Nordpred in the R program,which has been shown to perform well in predicting the trend of cancer incidence (20-22),was used to perform an ageperiod-cohort (APC) analysis to predict the numbers and rates of the incidence and mortality of GC in the next 25 years,taking into account both the change in rates and the population structure.The Nordpred package can apply the power5 and poisson APC models to perform the prediction(https://rdrr.io/github/haraldwf/nordpred/man/nordpred.html).In our study,we used the power5 APC model to perform the prediction.The basic APC model isg(λij)=μ+αi+βj+γk,(default link function isλij^ 0.2,whereμrepresents the intercept,andαi,βj,andγkrepresent the effect of age,period,and cohort,respectively) (23).Moreover,to facilitate comparison with the predicted results,based on the observed data of GC in 2019,we estimated the numbers and rates of GC events,assuming that they remained stable,decreased (optimistic reference),and increased (pessimistic reference) by 1% per year.The ggplot2 and RcolorBrewer packages of the open-source R program (Version 3.6.2;R core team,R Foundation for Statistical Computing,Vienna,Austria) were used to perform the visualization of the results.
Results
Incidence,mortality and DALYs of GC in 2019
In 2019,the number of incident cases and ASIR of GC were 612.82 thousand (95% UI:513.00,728.89) and 30.64 per 100,000 (95% UI:25.82,36.15) among the total Chinese population,respectively (Table 1).GC contributed to 421.54 thousand (95% UI:353.52,493.18) deaths in 2019,and the total population of ASMR was 21.72 per 100,000 (95% UI:18.31,25.31) (Table 2).GC caused 9,824.99 thousand (95% UI:8,191.72,11,632.86) DALYs in 2019,and the age-standardized rate of DALYs was 481.15 per 100,000 (95% UI:403.20,567.36) (Table 3).The number and age-standardized rates of incidence,mortality and DALYs for males were more than 2 times higher that for females (Tables 1-3).
In 2019,the numbers of incident cases and deaths of GC reached a peak among the total population aged 70-74 years (Tables 1,2),and these trends were similar for males and females (Figure 1A,B).The number of DALYs reached a peak at 65-69 years old among the total population and both sexes (Table 3,Figure 1C).Meanwhile,the numbers of incident cases,deaths and DALYs were lower among males than females in individuals over 90 years old (Figure 1).
The age-specific rates for incidence and mortality reached a peak among the total population aged 85-89 years (Tables 1,2);meanwhile,the age-specific rates for DALYs reached a peak at 75-79 years old (Table 3).The trends of age-specific rates of incidence and DALYs amongboth males and females were similar to the trends for the total population,while the trends of age-specific rates of mortality differed between males and females.The agespecific rates of mortality peaked at 90-94 years old in males,while the age-specific rates of mortality increased with increasing age in females.Furthermore,the numbers and rates of incidence,deaths and DALYs were concentrated in the elderly population (≥60 years old)(Figure 1).
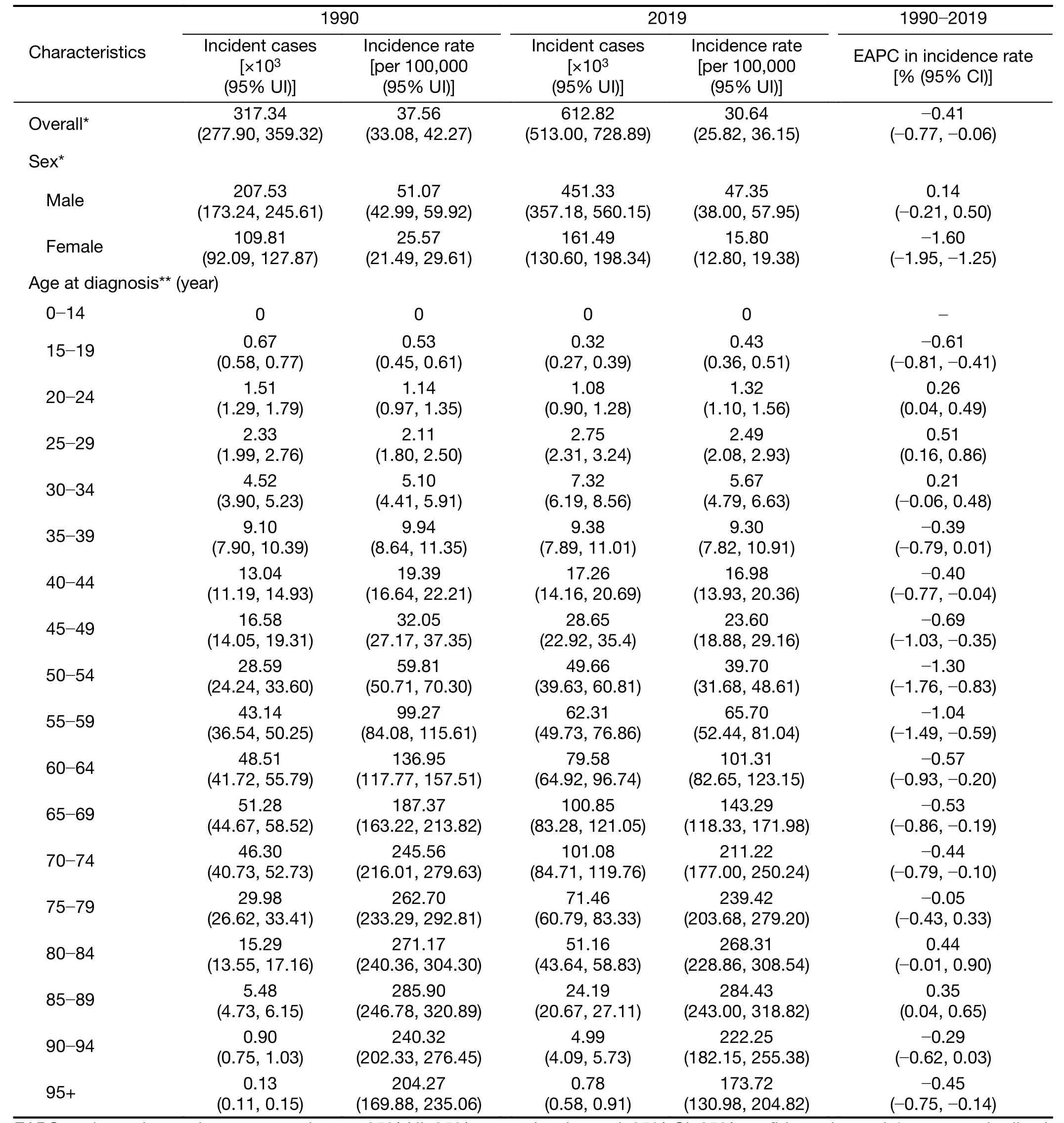
Table 1 Number of incident cases and incidence rate of gastric cancer in China in 1990 and 2019 and EAPC from 1990 to 2019

Table 2 Number of deaths and mortality rate of gastric cancer in China in 1990 and 2019 and EAPC from 1990 to 2019
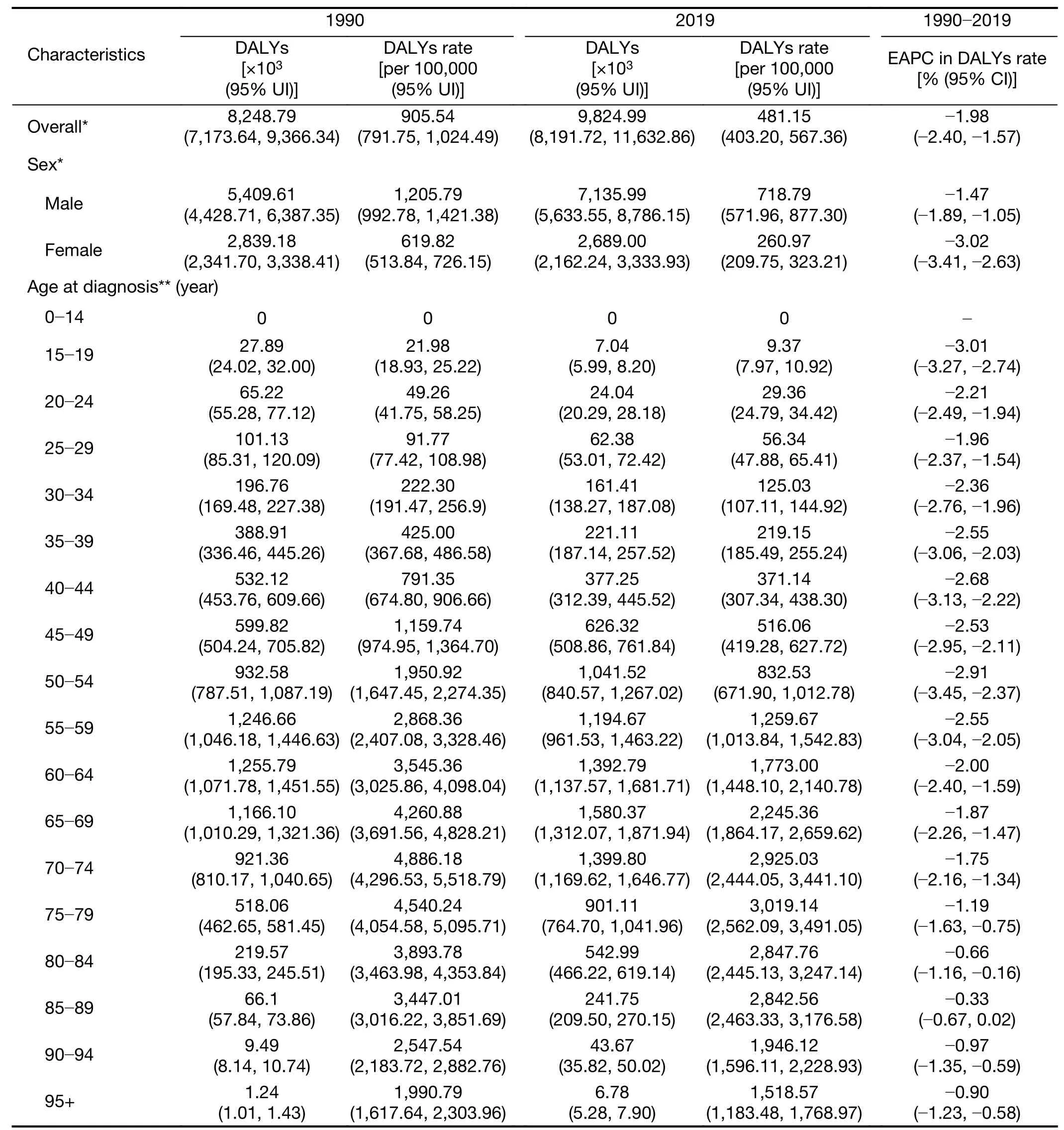
Table 3 Number of DALYs and DALYs rate of gastric cancer in China in 1990 and 2019 and EAPC from 1990 to 2019
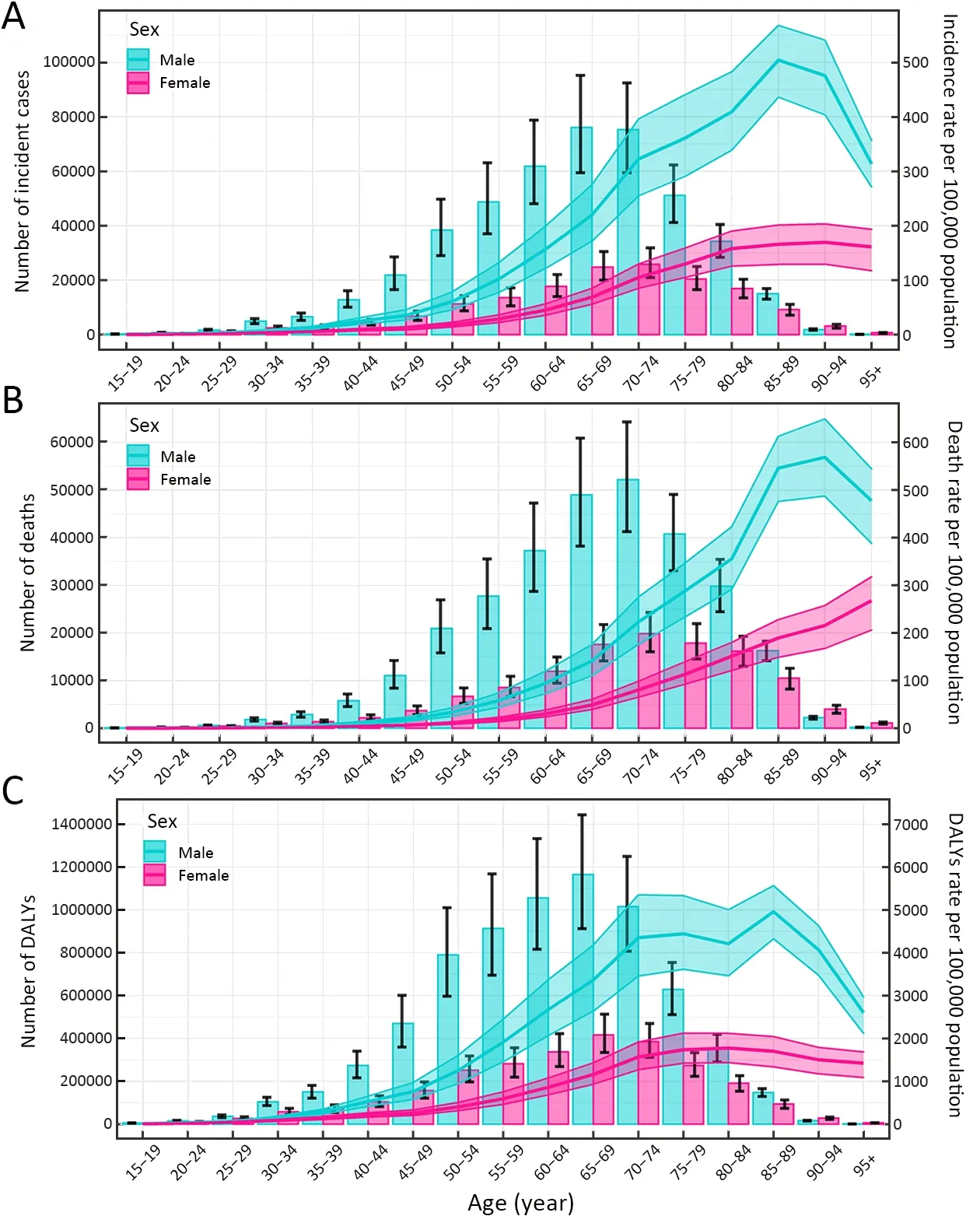
Figure 1 Numbers and rates of incidence (A),death (B) and DALYs (C) of gastric cancer by age and sex in 2019 in China.Shading represents the upper and lower limits of the 95% uncertainty intervals (95% UIs).DALYs,disability-adjusted life-years.
Temporal trends of incidence,mortality and DALYs of GC from 1990 to 2019
From 1990 to 2019,the numbers of incident cases,deaths and DALYs of GC all significantly increased among the total population (Tables 1-3).The number of incident cases increased by more than two times among males ≥65 years old and females ≥80 years old during the study period(Figure 2A).The ASIR was 37.56 per 100,000 (95% UI:33.08,42.27) in 1990,which decreased in 2019,with an EAPC of -0.41 (95% CI:-0.77,-0.06) in the total population (Table 1).The ASIR of females decreased more significantly than that of males during this period[EAPC=-1.60,95% CI:(-1.95,-1.25)vs.EAPC=0.14,95% CI:(-0.21,0.50),respectively](Table 1).Additionally,overall downward trends in the incidence rates were observed among both sexes in most age-specific groups,while short-term upward trends were observed between 2000 and 2010 (which was more pronounced among males)(Figure 2B).
The ASMR decreased from 1990 [37.73 per 100,000(95% UI:33.20,42.39)]to 2019,with an EAPC of -1.68(95% CI:-2.09,-1.27) (Table 2).A decreasing trend of age standardized DALYs was also observed during this period,and the EAPC was -1.98 (95% CI:-2.40,-1.57) (Table 3).Overall downward trends in mortality and DALYs rates were observed in most age-specific groups and both sexes;from 2000 to 2010,the mortality and DALYs rates showed a short-term upward trend,especially among males and females aged ≥75 years old (Figure 2C,D).
Mortality and DALYs rates of GC attributable to risk factors and their temporal trends from 1990 to 2019
In all age-specific groups,the mortality that was attributed to smoking was the highest among males and the lowest among females (Figure 3A).Trends in the first increase and then decrease of GC mortality attributable to a highsodium diet and smoking were observed in most agespecific groups and both sexes,and the overall downward trends were observed during the past three decades (Figure 3A).Moreover,the temporal trends of the rates of DALYs attributable to a high-sodium diet and smoking were similar to those of mortality (Figure 3B).
The proportions of DALYs that were attributed to risk factors (smoking and a high-sodium diet) were different between males and females.Smoking was the most significant contribution among males,accounting for more than 27.5% of DALYs from 1990 to 2019;the proportions of DALYs of GC attributable to smoking for males were about 10 times higher than that for females.A high-sodium diet was the most significant contribution among females,accounting for more than 8.7% of DALYs from 1990 to 2019 (Figure 3C).
Moreover,during this period,the proportions of DALYs attributable to both smoking and a high-sodium diet did not change significantly among sexes in any age-specific groups.During this period,the proportions of DALYs attributable to smoking among females increased in those>45 years old,while the proportions attributable to a highsodium diet decreased in females >75 years old.Among males,from 1990 to 2019,the proportions of DALYs attributable to smoking decreased in the 70-89 year-old age group,while the proportions attributable to a highsodium diet decreased in males >80 years old (Figure 3D).
Predictions of incidence and mortality of GC from 2020 to 2044
Based on GBD data of GC from 1990 to 2019 in China,we further predicted the numbers and rates of incidence and mortality in the next 25 years (Figure 4).In the next 25 years,the rates of incidence and mortality among both males and females should show a downward trend (Figure 4A),while the numbers of new cases and deaths of GC should continue to increase from 2020 to 2044 (Figure 4B,C).In 2044,the overall new GC cases should increase to 738.79 thousand (Figure 4B) and the number of GC deaths should increase to 454.80 thousand (Figure 4C).In 2044,among males,the numbers of incident cases and deaths should increase to 546.76 thousand and 320.66 thousand,respectively (Figure 4B,C).Among females,the numbers of incident cases and deaths should increase to 192.04 thousand and 134.14 thousand in 2044,respectively (Figure 4B,C).The numbers of incident cases and deaths for males should be more than twice as high as that for females.
Discussion
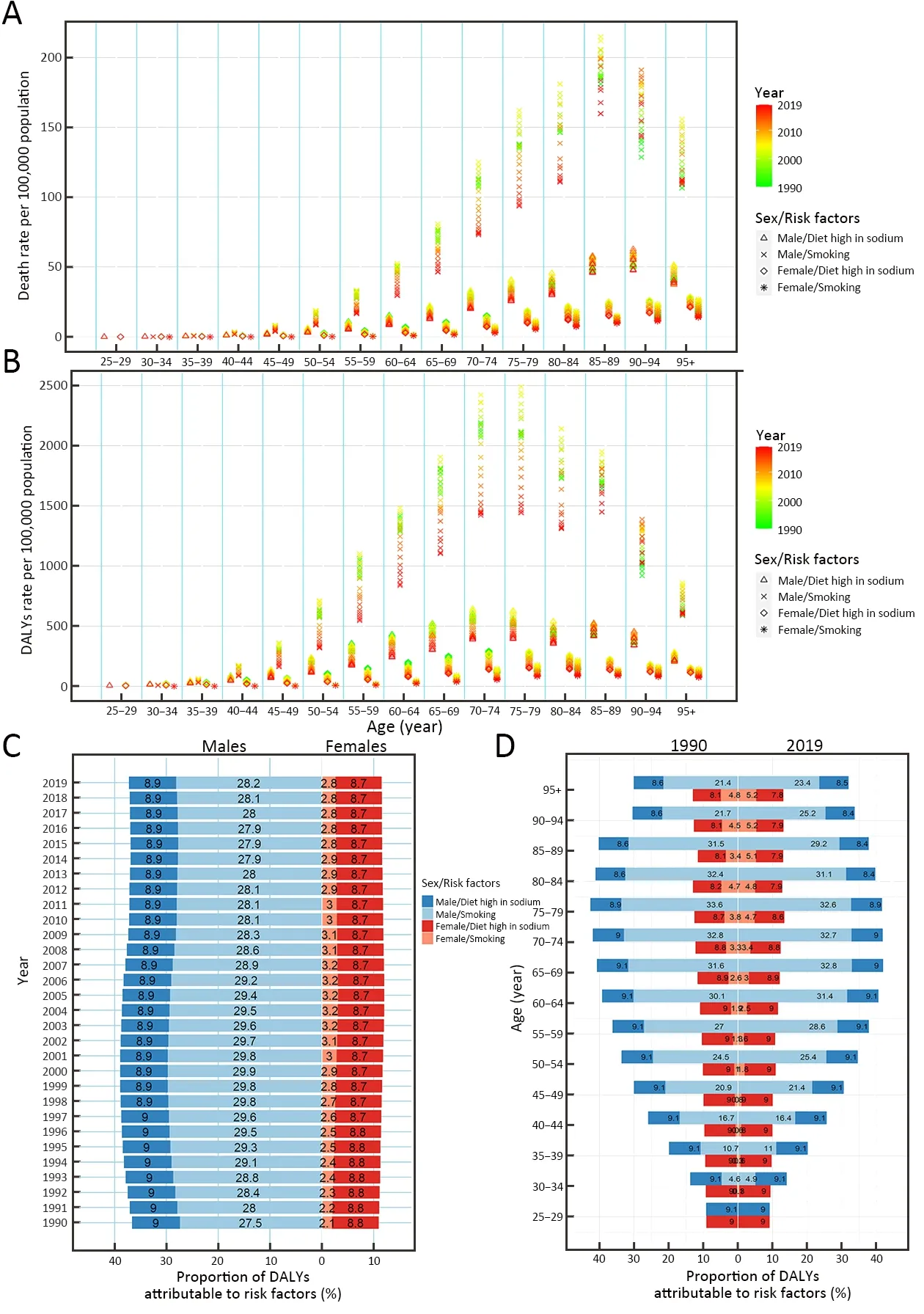
Figure 3 Rates of death,rates and proportions of DALYs attributable to risk factors by age and sex,from 1990 to 2019 in China.Rates of death (A) and DALYs (B) of gastric cancer attributable to risk factors by age and sex,from 1990 to 2019 in China;proportions of DALYs attributable to risk factors by sex from 1990 to 2019 in China (C);and proportions of DALYs attributable to risk factors by age and sex in 1990 and 2019 in China (D).DALYs,disability-adjusted life-years.
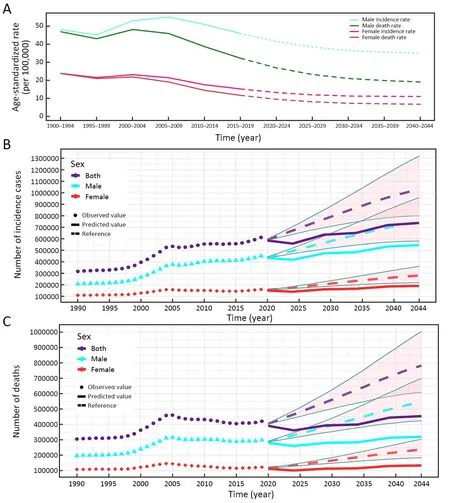
Figure 4 Temporal trends and forecasted rates of incidence and death (A),and number of incident cases (B) and deaths (C) of gastric cancer by sex,from 2020 to 2044 in China.Solid lines and dash lines represent the observed and the predicted the number of incident cases and deaths of gastric cancer;shading represents a 1% decrease and increase interval based on the 2019 rate.DALYs,disability-adjusted lifeyears.
China is one of the countries with the highest burden of GC in the world (13,24).In the past,few studies analyzed the burden of GC in China (24-26),and the latest disease burden of GC is still unknown.Therefore,in our study,using the latest data of the GBD study (2019),we did a more comprehensively and in-depth analysis of the disease burden of GC and its temporal trends by age,sex,and risk factors,and uniquely,we predicted the numbers and rates of incidence and mortality in the next 25 years in China.First of all,in 2019,there were 612.82 thousand new cases and 421.54 thousand deaths attributed to GC in China,and the ASIR and ASMR were 30.64 per 100,000 and 21.72 per 100,000,respectively.In our study,the numbers and rates of incidence and deaths in 2019 were higher than those estimated by the International Agency for Research on Cancer (IARC) and related studies in China;the reasons for these differences might be related to the difference in reporting years (reported in 2018 and 2015,respectively),the coverage points of data collection,and the estimation models.
China contributes the largest numbers of GC incident cases,deaths and DALYs,worldwide (13).The numbers of incident cases,deaths and DALYs all significantly increased from 1990 to 2019 in China among the total population,and our model predicted the numbers of new cases and deaths of GC should continue to increase in the next 25 years in both sexes.Meanwhile,the rates of incidence,mortality and DALYs showed an overall decreasing trend in the past three decades among the total population,which is consistent with previous studies (25,26).Although the rates of incidence and mortality of GC showed downward trends in the world and China,the disease burden of GC in China is still heavy (25) and these rates are higher than the average levels of the world (27).
Many factors produced the high disease burden of GC in China.Firstly,China has the largest population in the world,with a population of approximately 1.42 billion,accounting for almost one-fifth of the world’s population(28-30).The large population base contributes to higher numbers and rates of incidence,mortality and DALYs,which can have a significant impact on the world (29).Meanwhile,China is transforming into an aging nation(31,32).This trend may cause the numbers and rates of incidence,mortality and DALYs to be concentrated in the elderly population (especially ≥60 years old),which is consistent with our results.Secondly,China has operated a screening program for the populations with a high risk of GC (25),and significant improvement has been made in the early diagnosis and treatment of GC (24).A series of screening and early detection programs have been formulated and implemented by the Chinese government since 2005 (26,33,34).These programs were first implemented in 11 high-risk regions in China,and then expanded to all provinces in 2019 (34).The target population of the current screening program is 40-69 years old of both sexes (26).The implementation of screening and early detection programs might be an important explanation for our results.The improvement of medical conditions and the implementation of public health strategies and screening programs would result in a decline in the rates of mortality and DALYs of GC,and on the other hand,the detection rate of new cases would increase,thereby keeping the incidence rate from declining substantially.However,it is expected from the prediction model that the future incidence rate will steadily decrease.Thirdly,with the improvement of public health and the changing of lifestyles in China (35),the risk factors (such as smoking,alcohol consumption,a high-sodium diet andH.pyloriinfection) have been effectively controlled,leading to a decline in the rates of mortality and DALYs.Lastly,the improvements in socioeconomic status might be also an important reason (26).The rapid economic development of China (especially in the past 10 years) has greatly improved the living standards of residents and their personal awareness of diseases,which might have resulted in a decline in the rates of incidence,mortality and DALYs in our study.In summary,the large population base,aging of the population,implementation of screening and early detection programs,controlling risk factors,and improvements in socioeconomic status,together contribute to the high disease burden of GC in China.
Although the overall decreasing trends in the rates of incidence,mortality and DALYs were observed in all agespecific groups and both sexes,these indicators showed a short-term upward trend from 2000 to 2010.The screening and early detection programs were initially implemented in 2005 in China (34),which might have led to an increase in the detection of the number of new cases in the following years.The other possible reason for this observed result might be that China had implemented a series of prevention strategies,including tobacco-control strategies since 2005 (36,37) and a salt-consumption program since 2007 (38).In addition,an increase in deathdata collection points might also be a reason.The deaths data were reported by the China Disease Surveillance Points system:145,161 and 605 disease surveillance points were used from 1991 to 2003,2004 to 2012,and 2013 to 2017,respectively (15);from 2008 to 2017,all the deaths data were reported through the online reporting system of the Chinese Center for Disease Control and Prevention (15).
We further found that the risk factors of smoking and a high-sodium diet played an important role in the GC burden,and might also be the main cause of differences between males and females.Smoking is one of the wellknown risk factors,and the GC burden caused by smoking is different between males and females.In our study,the proportion of DALYs attributable to smoking was about 10 times higher in males than females.In China,the smoking prevalence rates of males and females were 52.9% and 2.4% in 2010,respectively (39,40),which may be an important reason for the gender differences.Moreover,in 2010,the prevalence of GC was the highest among males in the 45-64 years age group (63.0%) (40),which may increase the burden of disease for males over 45 years old in the future.Consistent with our speculation,we observed higher proportions of DALYs of GC attributable to smoking in males in the 50-94 years age group (>25%) in 2019.China has formulated many tobacco control strategies and mobilized all people to participate (36,37,41).The WHO Framework Convention on Tobacco Control(FCTC) was ratified by China in 2005,and tobacco control has made progress during the past decade (36,37).A slight downward trend in the proportion of DALYs attributable to smoking was observed in our study.The mechanisms of the effect of smoking on GC are unclear currently.Overall,smoking is associated with the development of precursor lesions of GC;in addition,tobacco smoke contains a variety of chemical carcinogens (especially nitrosamines and other nitroso compounds) (42,43).These chemical carcinogens may bind to DNA and affect the normal function of DNA,eventually leading to GC (42,43).
High-salt consumption is an important risk factor for GC and may increase the risk of it through the following mechanisms.Firstly,high-salt consumption may irritate the gastric mucosa,inducing intestinal metaplasia,and lead to atrophic gastritis (44,45).Secondly,high-salt consumption can promote the carcinogenesis progress of gastric dysplasia or GC among person infected withH.pylori(44-46).Moreover,high-salt foods (such as salted fish,preserved foods and processed meats) may also contain nitrate and nitrite,which may promote the formation of Nnitroso compounds (44).From our study,we found that the proportion of DALYs attributable to a high-sodium diet was more than 8.7% in China in 2019;and a slightly downward trend in the proportion of DALYs attributable to a high-sodium diet was observed among males and females.Since 2007,China developed the“China Healthy Lifestyle for All”initiative to improve people’s health literacy,which includes important content about the control of salt intake (38).With the control of saltconsumption program,the rates of death and DALYs attributable to a high-sodium diet has slightly decreased in the past three decades.However,the GC burden caused by a high-sodium diet is still relatively high.Therefore,more comprehensive prevention and control measures should be taken to further reduce the burden of GC caused by highsalt intake.
We should discuss other important risk factors for GC that were not contained in the database.H.pyloriis a wellknown risk factor for GC,and is classified as a class I human carcinogen (47,48).In our study,although we could not evaluate the GC burden caused byH.pylori,we could speculate that the proportion of DALYs attributable toH.pyloriinfection might be high.In 2015,about 4.4 billion people worldwide wereH.pylori-positive (49).In the Western world,the prevalence ofH.pylorihas greatly decreased,while in developing countries,the prevalence ofH.pyloriis still at a high level (49).The prevalence ofH.pyloriis 55.8% in China,which is higher than in Japan(51.7%) and Korea (53.9%) (49).In China,because of wider population-based screening (28),increased awareness of the treatment ofH.pyloriinfection (28),the development of an effective vaccine (50),and the improvement in socioeconomic status,the prevalence ofH.pylorishows a decreasing trend (decreased 0.9% annually)(51),which may contribute to the decrease in the rates of mortality and DALYs.In addition,other reported risk factors for GC include alcohol consumption,infection with the Epstein-Barr virus,socioeconomic status,a low intake of fruits and vegetables,obesity and gastroesophageal reflux disease,poor oral health,radiation,and a family history of GC (5,52-54).
There are some limitations in our study.Firstly,we only assessed the disease burden of GC at the national level and could not conduct a more detailed assessment at the provincial level.Secondly,we could not divide GC into the cardia GC and non-cardia GC.The temporal trend of the incidence and risk factors for these two subtypes of GC are different (5,52).Smoking,age,sex,radiation and family history are common risk factors for both types of GC;while obesity and gastroesophageal reflux disease are specific risk factors for cardia GC;H.pyloriinfection,low socioeconomic status and a high-salt diet are associated with an increased risk of non-cardia GC (5,53).Thirdly,we could not evaluate the GC burden caused by other important risk factors because the GBD database does not contain the corresponding data.Fourthly,since the data were a summary of several sites,the limitation of report omission might exist,which might result in the underestimation of our results.Although the data used to estimate incidence and mortality in the GBD study were fitted,filled,and corrected through various models,including a linear step mixed-effects model and spatiotemporal Gaussian process regression,our findings are consistent with those of previous studies.However,we should not ignore the fact that the proportion of the population covered by these systems has changed during the past three decades,which needs to be fully considered when interpreting our results.
Conclusions
We provide a comprehensive analysis of the burden of GC in China.During the past three decades,benefitting from the implementation of prevention strategies and the improvement of medical technology,the rates of incidence and mortality decreased.However,the number of new cases and deaths increased and will further increase in the next 25 years due to the aging population and high-risk behaviors (such as smoking,a high-sodium diet andH.pyloriinfection).Therefore,focusing on the risk factors,more detailed prevention and control strategies should be formulated for males and females and people in different age groups.Further effort is also needed to mobilize the entire population to participate,which may have a positive effect on variations in the incidence of GC.On the other hand,strategies and measures for improving the level of early diagnosis and developing new treatment techniques should be proposed to reduce the mortality of GC.
Acknowledgements
This study was supported by the National Key Research and Development Program of China (No.2017YFC0907003); the National Natural Science Foundation of China (No.81973116 and 81573229);and the Joint Research Funds for Shandong University and Karolinska Institute (No.SDU-KI-2020-03).
Footnote
Conflicts of Interest:The authors have no conflicts of interest to declare.
杂志排行
Chinese Journal of Cancer Research的其它文章
- Colorectal cancer burden and trends:Comparison between China and major burden countries in the world
- Clinical characteristics and clinicopathological correlations of bilateral breast cancer in China:A multicenter study from Chinese Society of Breast Surgery (CSBrS-006)
- Multi-center investigation of breast reconstruction after mastectomy from Chinese Society of Breast Surgery:A survey based on 31 tertiary hospitals (CSBrS-004)
- Laparoscopic vs. open surgery for gastrointestinal stromal tumors of esophagogastric junction:A multicenter,retrospective cohort analysis with propensity score weighting
- Radiotherapy combined with nimotuzumab for elderly esophageal cancer patients:A phase II clinical trial
- Pattern of No.12a lymph node metastasis in gastric cancer
