Multi-center investigation of breast reconstruction after mastectomy from Chinese Society of Breast Surgery:A survey based on 31 tertiary hospitals (CSBrS-004)
2021-03-13FengXuChuqiLeiHengCaoJunLiuJieLiHongchuanJiangChineseSocietyofBreastSurgery
Feng Xu,Chuqi Lei,Heng Cao,Jun Liu,Jie Li,Hongchuan Jiang,Chinese Society of Breast Surgery
1Department of Breast Surgery,Beijing Chao-Yang Hospital,Capital Medical University,Beijing 100020,China
Abstract Objective:Multi-center data on the current status and trends of breast reconstruction after mastectomy in China are lacking.Herein,we conducted a cross-sectional survey to investigate the current clinical practice pattern of postmastectomy breast reconstruction among Chinese female patients with breast cancer.Methods:A standardized questionnaire used to collect information on breast reconstruction among females diagnosed with breast cancer was distributed by 31 members of the Chinese Society of Breast Surgery between January 1,2018 and December 31,2018.Information was collected on tumor characteristics,treatment,mesh application,nipple-areola complex (NAC) preservation,postoperative complications,bilateral reconstruction,patient satisfaction and local recurrence.The overall rate of breast reconstruction was assessed,and the characteristics were compared across patient groups with different reconstruction approaches.Results:A total of 1,554 patients underwent breast reconstruction after total mastectomy,with a reconstruction rate of 9.6%.Among them,1,190 were implant-based,and 262 underwent autologous reconstructions,while 102 cases underwent a combination of both.Patients who underwent implant-based reconstruction were younger than those who received autologous reconstruction (40.1±4.6 vs .45.0±5.9,P=0.004).Compared to patients with autologous reconstruction,mesh application (25.5% vs .6.5%),NAC preservation (51.8% vs .40.5%) and reconstruction failure (1.8% vs.0) were more frequently reported among those with implant-based reconstruction.There was no significant difference in general satisfaction across three reconstruction approaches,though patients with autologous reconstruction reported the highest aesthetic satisfaction among the three groups (P=0.044).Conclusions:Implant-based breast reconstruction remains the dominant choice among patients,while autologous reconstruction was associated with higher aesthetic satisfaction.Our multi-center investigation based on the findings of the tertiary hospitals of Chinese Society of Breast Surgery may guide a future series of clinical studies on breast reconstruction in China.
Keywords:Breast cancer;mastectomy;breast reconstruction;questionnaire survey;patient satisfaction
Introduction
Breast cancer is the most common malignancy among women in China (1,2).The principal treatment approach for early breast cancer is still the surgical approach.However,the traditional mastectomy results in the loss of breasts and damage in appearance,which in turn may cause mental illnesses such as decreased self-confidence,anxiety and depression (3).For females who are not suitable candidates for breast-conservation,breast reconstruction is the primary approach used to restore the shape of breasts.Nevertheless,as indicated in a survey on breast reconstruction after mastectomy among Chinese female patients in 2012,the reconstruction rate after total mastectomy was only about 4.5% (4),which was much lower than that reported in western countries.Though,with the significant improvement in both disease-free survival and overall survival (5),breast cancer care has evolved from simple disease control to the recovery of breast shape and function (6).Furthermore,with the continuous improvement of living conditions,demand for breast reconstruction among Chinese female patients with breast cancer has also been increasing.However,to date,there is a lack of multi-center data on breast reconstruction necessary to re-evaluate the current status of breast reconstruction after mastectomy,especially in China.Consequently,we conducted a questionnaire-based crosssectional survey based on the Chinese Society of Breast Surgery (CSBrS) so as to investigate the current clinical practice pattern of postmastectomy breast reconstruction in China.
Materials and methods
Survey objectives and methods
A convenience sampling method was used among members of CSBrS according to geographical distribution.The CSBrS is a non-profit national social organization engaged in breast surgery research,clinical treatment and prevention under the Chinese Medical Association.The member hospitals are representative of many provinces,cities and autonomous regions across the country.Herein,we selected 31 hospitals representative of Eastern,Central and Western China.Firstly,the CSBrS issued a survey project notification letter to the interviewed hospitals by email and afterward conducted relevant training for respondents who were to complete the standardized questionnaire.All the reports were reviewed by principal investigators after the questionnaires were completed.The inclusion criteria were the following:1) the enrolled hospitals were accredited by CSBrS;and 2) the annual operation volume of breast cancer is more than 200.The exclusion criteria were as follows:1) breast reconstruction surgery for benign breast lesions;or 2) incomplete questionnaire-relevant data.This study was subject to approval by the Ethics Review Board of Affiliated Beijing Chao-Yang Hospital,Capital Medical University,and was registered with the China Clinical Trial Registry (No.ChiCTR1900025226).
Questionnaire design
Data were collected using a self-designed standardized questionnaire,which included four following parts:1) the basic information of surgeons and their hospitals;2) the number of breast cancer surgery and reconstruction cases in the enrolled hospitals from January 1,2018 to December 31,2018;3) the characteristics of patients with breast reconstruction including age,body mass index (BMI),chemotherapy and radiotherapy,mesh application,nippleareola complex (NAC) preservation,complication,locoregional recurrence,and bilateral reconstruction;and 4) the number of patients with general satisfaction and aesthetic satisfaction.
Some concepts are identified and explained during the questionnaire design process.Reconstruction volume was defined as the annual breast reconstruction surgeries per each hospital;doctor’s workload referred to the number of surgeries performed per year for each doctor.One-step implant-based reconstruction was used in the case of skinsparing mastectomy (SSM) or nipple-areola complex sparing mastectomy (NSM),where a permanent prosthesis is immediately implanted after subcutaneous glandectomy,and is often used in combination with biological or synthetic meshes.Two-step implant reconstruction referred to a tissue expander that was first implanted after mastectomy and then was replaced with a permanent prosthesis after 4-6 months of expansion (7).Reconstruction failure was identified as implant or flap loss due to wound infection,implant exposure,or flap necrosis.Secondary repair after reconstruction implied the use of transfer flaps for repair of the complications.Satisfaction was assessed on the basis of the Michigan Breast Reconstruction Outcomes Study (8),where general satisfaction and aesthetic satisfaction were separately appraised by patients who responded to the questions using a five-point Likert scale.The results were further classified into two groups where:score above 4 was considered as“satisfied”and a score below 4 was considered as“dissatisfied”.
Approaches of breast reconstruction
For patients with autologous or implant-based breast reconstruction,standard SSM or NSM was performed.Patients were divided into three groups by the approaches utilized for breast reconstruction.Autologous reconstructions included latissimus dorsimyocutaneous flaps (LDMF),pedicle transverse rectus abdominous myocutaneous (pTRAM) flaps,and free tissue transfers using abdominal flaps including free TRAM,musclesparing TRAM,and deep inferior epigastric perforator flap(DIEP).Implant-based reconstructions included tissue expander-implant placement and prosthetic placement alone. Patients who underwent a combination of autologous and implant-based reconstructions were grouped as a“combination group”.
Statistical analysis
Reconstruction rates were compared across groups by region (Eastvs.Centralvs.West),GDP capita (<8vs.8-12vs.>12),hospital type (general hospitalvs.specialist hospital),number of beds (<50vs.≥50),number of surgeons (<15vs.≥15),mastectomy volume (<500vs.≥500),and doctors’ workload (<40vs.40-60vs.>60) using the nonparametric Wilcoxon’s rank-sum test for two-group comparisons and the Kruskal-Wallis test for three-group comparisons.Descriptive patterns for groups of different reconstruction approaches were compared using the Fishers’ exact test and Pearson Chi-square test for categorical variables,and analysis of variance (ANOVA) for continuous variables (i.e.,age and BMI).Statistical analyses were performed using IBM SPSS statistical (Version 20.0;IBM Corp.,New York,USA).All statistical tests were based on two-sided probability,and P<0.05 was considered as statistically significant.
Results
Basic information of respondents
Questionnaires were eventually collected from 31 members of CSBrS based on the inclusion and exclusion criteria.Among all these respondents,27 were from general tertiary hospitals,3 were from cancer hospitals,and 1 was from a maternity hospital.Eighteen hospitals were located in the eastern region,5 in the central region and 8 in the western region,covering 16 provinces,2 autonomous regions,and 4 municipalities directly under the central government.Mastectomy was performed in 18 hospitals with an annual surgical volume of less than 500,in 9 hospitals with an annual surgical volume of 500-1,000,and in 4 hospitals with an annual surgical volume of more than 1,000.
Risk factors affecting breast reconstruction volume
Table 1shows that the level of GDP per capita,region,hospital type,number of beds and breast surgeons were not related to the reconstruction volume.However,there was a strong correlation between the reconstruction volume and the doctors’ workload per person-year (P<0.001),between the reconstruction volume and mastectomy volume per year (P=0.001).We further found that the choice of different reconstruction procedures was not associated with the aforementioned risk factors.
Basic information about breast reconstruction
Among 16,187 female breast cancer patients who underwent a mastectomy in 2018,1,554 patients underwent reconstructions after mastectomy,resulting in an overall reconstruction rate of 9.6%. Among patients who underwent reconstruction,direct-to-prosthesis reconstruction was the most commonly employed reconstruction approach (n=785,50.5%),followed by expander-assisted reconstruction (n=405,26.1%),LDMF reconstruction(n=140,9.0%),TRAM/DIEP reconstruction (n=109,7.0%),and combination of implant-based and autologous reconstruction (n=102,6.6%),while lipofilling reconstruction was only performed for 13 patients(Figure 1).Bilateral breast reconstruction was reported for 100 patients.
Characteristics of patients who underwent breast reconstruction are shown inTable 2.The mean age of patients who received reconstruction was 40.67 years old,with a mean BMI of 23.6 kg/m2.A total of 773 patients underwent NAC sparing approaches,while 334 patients were treated with a mesh-based technique.Most patients(n=821,52.8%) received chemotherapy,while 208 patients(13.4%) were treated with radiotherapy.
Compared to patients who underwent autologous reconstruction or a combination of autologous and implant-based reconstruction,patients with implant-based reconstruction were younger (40.1±4.6vs.45.0±5.9vs.41.3±7.9;P=0.036) and were more likely to receive meshbased techniques (25.5%vs.6.5%vs.12.7%;P<0.001) and NAC sparing approaches (51.8%vs.40.5%vs.49.0%;P=0.004),while patients with a combination of autologous and implant-based reconstructions were more likely to receive chemotherapy than other two groups of patients(65.7%vs.52.9%vs.47.7%;P=0.009).
Overall,84 complications,including 22 cases ofreconstruction failure and 34 cases of secondary repair,were reported,with an overall complication rate of 5.4%.No statistical differences in complications were observed across three reconstruction approaches,though complications were slightly more frequently observed in the implant-based reconstruction group.Also,reconstruction failure was more common in the implantbased group than in the autologous group.
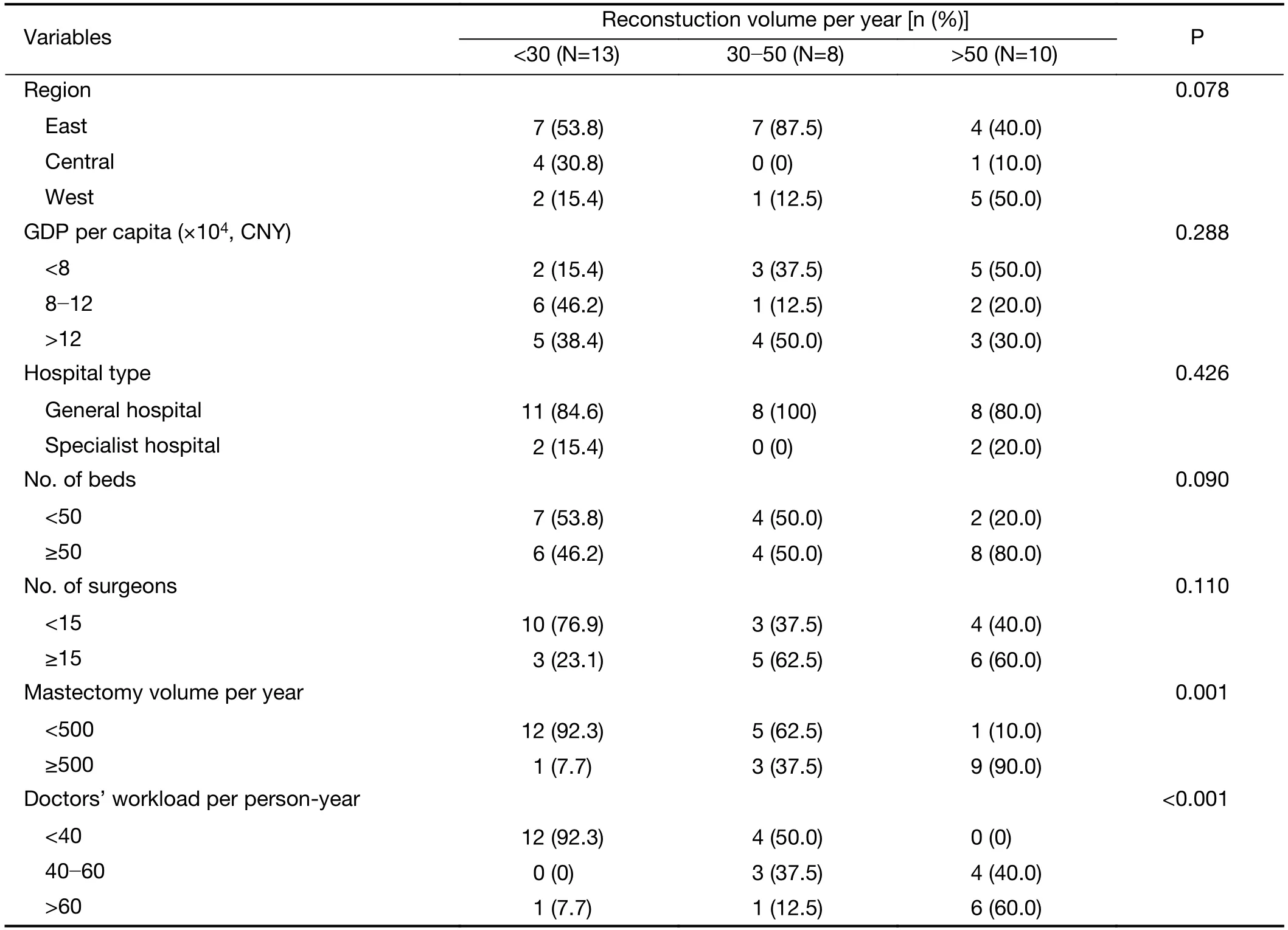
Table 1 Risk factors affecting reconstruction volume
At 12-month post-surgery,a large proportion of patients who underwent reconstruction reported general satisfaction (n=1,124,72.3%),and aesthetic satisfaction(n=1,112,71.6%).No significant differences across the three reconstruction methods were observed in terms of general satisfaction (71.7%vs.75.6%vs.71.6%,P=0.437).However,the autologous reconstruction group had the highest aesthetic satisfaction compared to the other two groups (77.9%vs.70.2%vs.71.6%,P=0.044).At a minimum follow-up of 1 year,there were 3 cases of local recurrence,all of which were in the group of implant-based reconstruction.
Discussion
In this multi-center cross-sectional study,we found that the overall rate of postmastectomy breast reconstruction among Chinese female patients was 9.6% in 2018.Implantbased reconstruction was the most commonly used reconstruction approach.However,both complications and failure after breast reconstruction were more frequently observed among patients who underwent implant-based reconstruction,though the former was not statistically significant. Patients with autologous reconstruction reported the highest aesthetic satisfaction compared to the other two reconstruction approaches. The doctor’s workload was linked to a higher probability of receiving breast reconstruction after mastectomy.
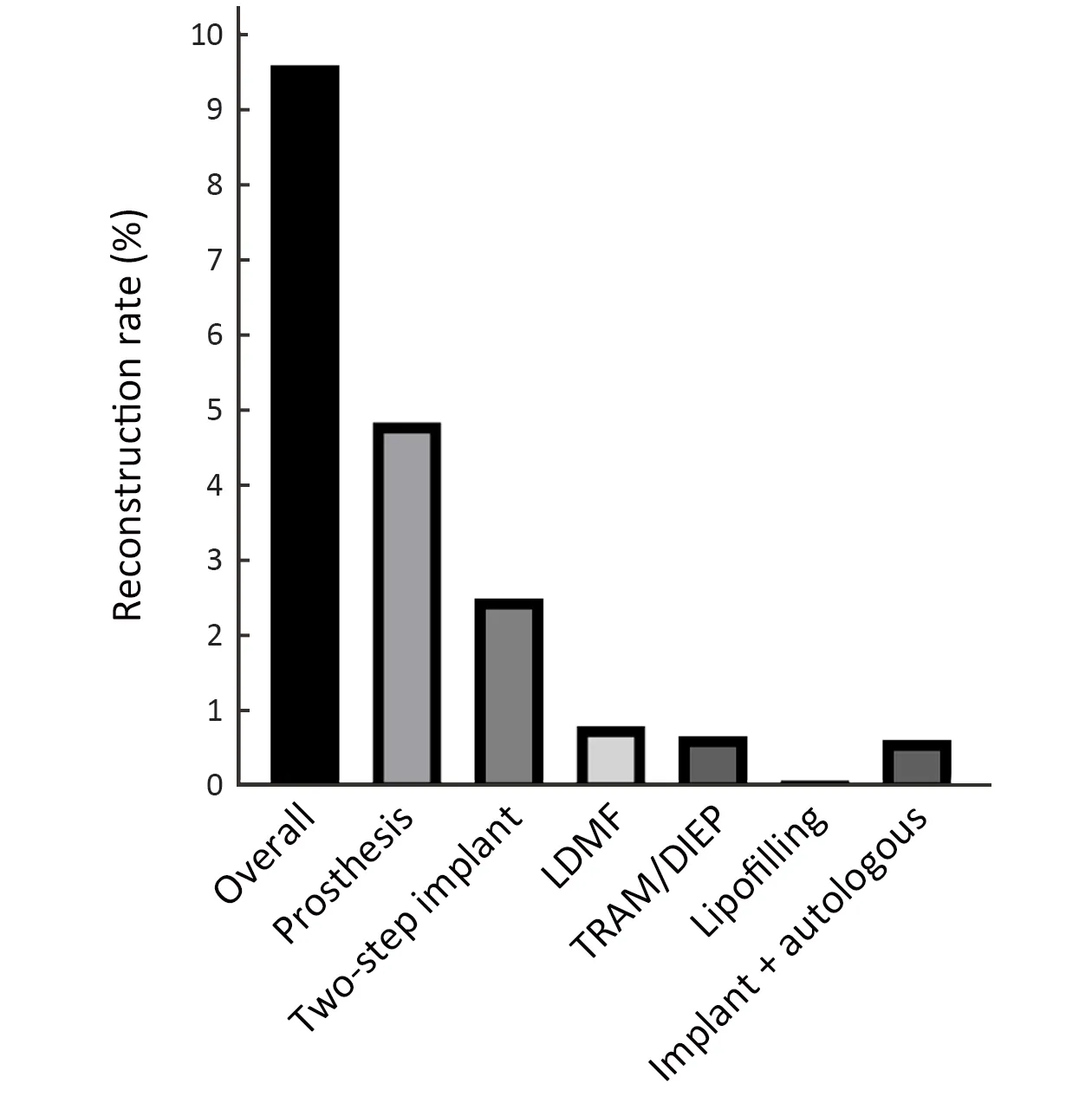
Figure 1 Distribution of different reconstruction procedures in 2018. LDMF,latissimus dorsimyocutaneous flap; TRAM,transverse rectus abdominous myocutaneous flap;DIEP,deep inferior epigastric perforator flap.
Over recent years,high-quality clinical studies,such as the MROC study (9),have increasingly focused on breast reconstruction and have changed patient outcomes after reconstruction.More and more patients are requesting breast reconstruction.Our results showed that the proportion of breast reconstruction in CSBrS was 9.6% in 2018.Though this rate has been higher than that previously reported in 2012,it is still much lower than the global rates.The nationwide rate of reconstruction in the UK has been around 10% until 2005,after which it increased to 23.3% by 2013-2014 (10),while the average rate of reconstruction in the United States in 2010 was 45%,surging to 54% in 2015 (11).
In terms of the implant reconstruction,direct-to-implant and two-stage expander-assisted reconstruction (12) are the mainstream of breast reconstruction,which made up 6.6%of the overall number of reconstructions in our study.Similar to our study,Ilonzoet al.(13) reported a significant increase in implant reconstruction,rising from 15.54% in 2005 to 33.30% in 2014 in the United States,thus exceeding autologous tissue (flap) reconstruction.This operation could avoid the consequent damage to the body caused by the acquisition of the donor tissue (14).Moreover,postoperative recovery is fast,which is favored by more doctors and patients.In the present study,the implant-based reconstruction accounted for 84% of all bilateral breast reconstruction.The implant achieves a highdegree of symmetry in bilateral breast reconstruction as a synthetic material,turning it into the preferred method for many respondents.Furthermore,our results showed that the population of patients in the implant reconstruction group was younger and more likely to utilize mesh and NAC preservation techniques,which were considerably higher than that of the autologous reconstruction group.Obviously,young women whose autologous tissue is not abundant enough for reconstruction might choose prosthesis implantation to achieve an aesthetically pleasing symmetrical appearance (15).Besides,it has been confirmed that the increase in mesh application,such as ADM and Tiloop Bra,has a good clinical outcome for the thickening of the breast-covering tissue after mastectomy(16).Similarly,NAC sparing in mastectomy has also been reported to positively impact patient satisfaction,body image,and psychological adjustment (17).
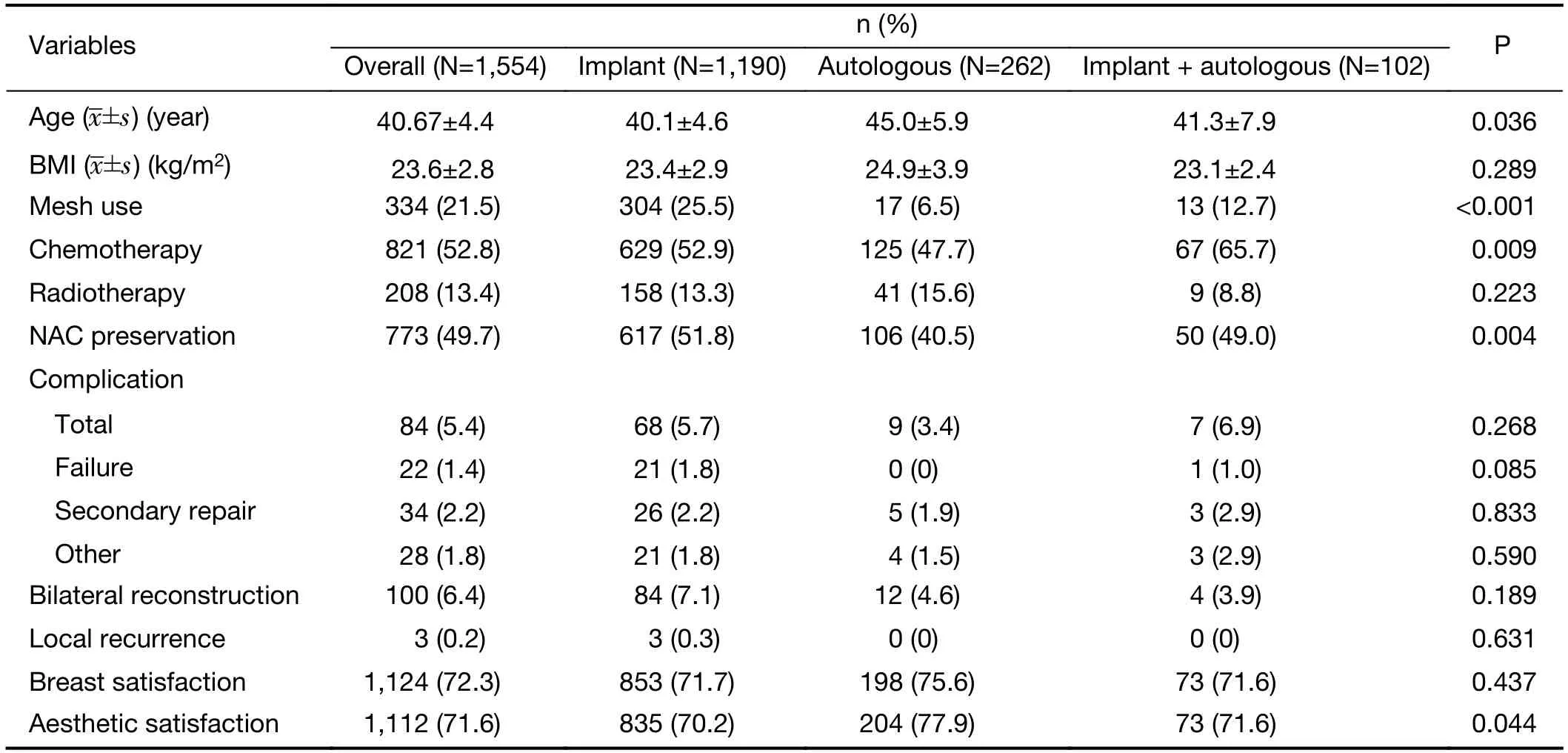
Table 2 Clinical characteristics of breast cancer patients categorized by reconstruction type in 2018
Notably,despite the advantages of a short operation time and hospitalization time,prosthesis reconstruction had the highest fail-to-complete reconstruction rate in our study.Regarding locoregional recurrence (LRR),only three cases developed LRR in the implant group because of the relatively short follow-up time.Orzalesiet al.reported that after a follow-up period of 6 years,LRR accounted for 2.9%,with 0.7% death records among Italian women (18).As an allogeneic tissue,the incidence of capsule formation and contracture around the prosthesis is extremely high,which can cause severe asymmetry of the breast,decreased aesthetics,and in some cases even pain and rupture of the prosthesis,calling for replacement surgery (19).In addition,the prosthesis is most likely to be affected by radiotherapy than autologous tissues (20).
For surgeons,autologous tissue reconstruction,which takes a longer learning curve,is the most arduous reconstruction technique.Nonetheless,this method naturally shapes the breast,and the cosmetic effect lasts for a long time (21).In our study,the most commonly used autologous flaps were latissimus dorsi musculocutaneous flaps,which were suitable for small and medium-sized breast reconstruction.However,in Europe and the United States,the deep inferior epigastric perforator flaps were the most commonly used flaps,which provided a larger amount of tissues,decreased incidence of flap necrosis,and lowered complications in the abdomen (22).Over recent years,autologous lipofilling has been applied by domestic breast surgeons in tumor plastic surgeries.Our study revealed that fat transplantation was used in 13 cases accounting for 5%of autologous reconstruction.Among these cases,Bravaassisted autologous fat grafting was used for three patients.Our single-center experience indicated that autologous lipofilling combined with BRAVA could improve the surgical procedures and result in natural breast and body contours.Nevertheless,large multi-center studies are warranted to evaluate fat grafting’s efficacy and safety in breast reconstruction.
Since Alderman brought forward the Michigan Breast Reconstruction Outcomes Study to the world in 2000,evaluating patient-reported satisfaction after reconstruction has become a useful tool to obtain the life quality and an effective way to evaluate the effectiveness of reconstruction surgery.Large-scale multi-center studies comparing the different types of breast reconstruction are currently lacking,especially in China.Our results showed no significant differences in overall general satisfaction between three types of reconstruction;however,the autologous reconstruction group had the highest aesthetic satisfaction,which was consistent with previous reports.Fraconet al.(23) evaluated the satisfaction score of 109 reconstruction patients (59 with implants and 50 with autologous reconstruction) and found that autologous breast reconstruction led to higher patient satisfaction than implant breast reconstruction.Yuehet al.(24) compared perforator flaps with more commonly practiced methods and found that autologous,abdominal-based reconstructions had the highest satisfaction rates across all four reconstructive techniques.However,the singleinstitution experience of Fudan University Shanghai Cancer Center (25) confirmed that the type of breast reconstruction might not influence patient satisfaction in a Chinese population.The difference might be due to the relatively lower BMI index and smaller breast size of most patients in China.
Our results showed a definite correlation between the reconstruction volume and the doctor’s workload.However,the level of GDP per capita,region,number of beds and breast surgeons were not related to reconstruction volume.There are other domestic factors that might limit the development of breast reconstruction in China.First,most hospitals have not yet formed a multidisciplinary treatment model for breast cancer,and the cooperation between oncology surgery and plastic surgery is still lacking.Secondly,the training module and certification system have not yet been formed;thus,doctors interested in reconstruction cannot receive specialized and systematic training.Moreover,most patients are even unaware of the safety,aesthetics,and complications of breast reconstruction.On the one hand,it is not conducive to large-scale development of breast reconstruction;on the other hand,the cost of surgery for breast reconstruction is not proportional to the difficulty of surgery,which further reduces the enthusiasm of surgeons for breast reconstruction.
This study has a few limitations.Although this study is a large-scale questionnaire-based survey on breast reconstruction,the included subjects were limited to hospitals accredited to CSBrS and did not cover primary hospitals,thus potentially overestimating the proportion of breast reconstruction.In addition,the questionnaire did not cover plastic surgery,so the status of breast reconstruction in this field is not clearly understood.
Conclusions
In general,the rate of breast reconstruction after mastectomy performed by 31 tertiary hospitals of CSBrS was greater than previously reported,but the proportion is still low.Patients choosing implant reconstruction remain the dominant population,especially for immediate breast reconstruction.How to effectively avoid or reduce the complications and reconstruction failure rates and improve patient’s satisfaction are problems faced by a number of breast surgeons.Our study calls for a multidisciplinary cooperation model that would enable breast surgeons to receive more breast reconstruction training to promote the development of breast reconstruction in China.
Acknowledgements
This study was supported by the Project of the Science and Technology Commission of Beijing Municipality (No.D16110000816002,No.Z181100002218001).
Thanks to the following members of Chinese Society of Breast Surgery for providing breast cancer patient data:Jianguo Zhang,the Second Affiliated Hospital of Harbin Medical University;Rui Ling,Xijing Hospital,Air Force Military Medical University;Yinhua Liu,Xuening Duan,Peking University First Hospital;Zhenzhen Liu,Henan Cancer Hospital and the Affiliated Cancer Hospital of Zhengzhou University;Shu Wang,Peking University People’s Hospital;Dedian Chen,Yunnan Cancer Hospital&the Third Affiliated Hospital of Kunming Medical University &Yunnan Cancer Center;Zhongwei Cao,Inner Mongolia People’s Hospital;Xiang Qu,Beijing Friendship Hospital,Capital Medical University;Jiandong Wang,Chinese People’s Liberation Army General Hospital;Dahua Mao,Affiliated Wudang Hospital of Guizhou Medical University;Zhigang Yu,the Second Hospital of Shandong University;Jian Huang,the Second Affiliated Hospital of Medical School of Zhejiang University;Zuowei Zhao,the Second Hospital of Dalian Medical University;Yi Zhao,Shengjing Hospital of China Medical University;Wei Zhu,Zhongshan Hospital,Fudan University;Feng Jin,the First Affiliated Hospital of China Medical University;Jun Jiang,Southwest Hospital,Army Medical University;Erwei Song,Sun Yat-sen Memorial Hospital of Sun Yat-sen University;Guosheng Ren,the First Affiliated Hospital of Chongqing Medical University;Ailin Song,the Second Hospital of Lanzhou University;Zhiming Fan,the First Hospital of Jilin University;Qiang Zou,Huashan Hospital,Fudan University;Jinping Liu,Sichuan Academy of Medical Sciences &Sichuan Provincial People’s Hospital;Jianghua Ou,the Tumor Affiliated Hospital of Xinjiang Medical University,the Third Clinical College of Xinjiang Medical University;Kejin Wu,Obstetrics and Gynecology Hospital of Fudan University;Yonghui Luo,the Second Hospital of Nanchang University;Hua Kang,Xuanwu Hospital,Capital Medical University;Shui Wang,the First Affiliated Hospital of Nanjing Medical University;Xingsong Tian,Shandong Provincial Hospital;Yunjiang Liu,the Fourth Affiliated Hospital of Hebei Medical University.
Footnote
Conflicts of Interest:The authors have no conflicts of interest to declare.
杂志排行
Chinese Journal of Cancer Research的其它文章
- Colorectal cancer burden and trends:Comparison between China and major burden countries in the world
- Changing trends of disease burden of gastric cancer in China from 1990 to 2019 and its predictions:Findings from Global Burden of Disease Study
- Clinical characteristics and clinicopathological correlations of bilateral breast cancer in China:A multicenter study from Chinese Society of Breast Surgery (CSBrS-006)
- Laparoscopic vs. open surgery for gastrointestinal stromal tumors of esophagogastric junction:A multicenter,retrospective cohort analysis with propensity score weighting
- Radiotherapy combined with nimotuzumab for elderly esophageal cancer patients:A phase II clinical trial
- Pattern of No.12a lymph node metastasis in gastric cancer
