Duplication of the common bile duct manifesting as recurrent pyogenic cholangitis: A case report
2021-02-05JunSeongHwangSungWooKo
Jun Seong Hwang, Sung Woo Ko
Abstract
Key Words: Double common bile duct; Common bile duct disease; Choledocholithiasis; Cholangitis; Endoscopic retrograde cholangiopancreatography; Case report
INTRODUCTION
Double common bile duct (DCBD) is an extremely rare congenital anomaly of the biliary system. Morphological classification of this anomaly was modified by Choiet al[1]in 2007 by adding a Type V, which is characterized by single drainage of the extrahepatic bile ducts. Only 7 cases of DCBD Type V have been reported so far. Herein, we report a rare case of DCBD Type V in an elderly woman who presented with recurrent pyogenic cholangitis.
CASE PRESENTATION
Chief complaints
A 77-year-old woman presented to the outpatient department of our hospital complaining of recurrent epigastric pain.
History of present illness
Patient’s symptoms started a month ago with recurrent episodes, with no history of fever, chills, or vomiting.
History of past illness
The patient had a history of laparoscopic cholecystectomy for cholelithiasis 2 years earlier at another hospital. She had undergone endoscopic retrograde cholangiopancreatography (ERCP) twice for choledocholithiasis before undergoing cholecystectomy.
Personal and family history
The patient did not have a history of drinking or smoking. There was no remarkable family medical history.
Physical examination
Physical examination did not reveal tenderness or signs of peritoneal irrigation, and the bowel sounds were normal. At the outpatient clinic, her temperature was 36.7 °C, pulse rate was 70 beats/min, and blood pressure was 122/82 mm Hg.
Laboratory examinations
Blood analysis showed normal complete blood cell count, liver function test and Creactive protein.
Imaging examinations
Computed tomography (CT) imaging revealed a dilated CBD that harboured multiple choledocholithiasis (Figure 1A). After admission, ERCP was subsequently performed, and the stones were extracted using a Dormia basket (MTW Endoskopie, Wesel, Germany) (Figure 1B) after endoscopic papillary balloon dilatation by a CRETMballoon dilatation catheters (Boston Scientific Corporation, Natick, MA, United States). A 5 Fr endoscopic nasobiliary drainage (ENBD) catheter (ENBD-5, Cook Medical, Bloomington, IN, United States) was inserted at the end of the procedure. A day after the ERCP, tubographyviathe ENBD catheter was performed to confirm the presence of residual stones in the bile duct. However, no definite filling defects were observed on tubography (Figure 1C). The patient was discharged without any complications of ERCP. A day after discharge, she visited the emergency department with complaints of severe epigastric pain and fever. Her temperature was 38.2 °C, pulse rate was 79 beats/min, and blood pressure was 149/85 mm Hg. Laboratory findings were suggestive of cholestasis [aspartate aminotransferase, 210 U/L (normal: 0–35 U/L); alanine aminotransferase, 134 U/L (0-35); alkaline phosphatase, 201 U/L (30-120); gamma glutamyl transferase, 184 U/L (9-64); total bilirubin, 2.77 mg/dL (0.3-1.2); direct bilirubin, 1.32 mg/dL (0-0.2); and C-reactive protein 6.91 mg/dL]. A CT scan demonstrated another dilated extrahepatic bile duct draining the right lobe of the liver, which also contained stones in the distal portion (Figure 2A). An urgent ERCP was performed as the stones were impacted at the ampulla (Figure 2B), and the stones with pus were retrieved using a balloon catheter (Escort II®Double Lumen Extraction Balloon, Cook Medical, Bloomington, IN, United States). A 10 Fr, 5 cm endoscopic retrograde biliary drainage tube (Cotton-Leung Biliary Stent, Cook Medical, Bloomington, IN, United States) was then placed in the CBD.
Magnetic resonance cholangiopancreatography (MRCP) was performed to evaluate the delicate structures of the CBD and to check for any remnant stones. MRCP revealed DCBD independently draining the left and right lobes of the liver, that created a short segment intrapancreatic CBD (Figure 3A) without a communicating channel, that was consistent with the DCBD Type Va as classified by Choiet al[1,2]. Residual choledocholithiasis was also noted in the right CBD. There was no evidence of anomalous union of the pancreaticobiliary duct on MRCP.
FINAL DIAGNOSIS
The final diagnosis was DCBD that manifested as recurrent pyogenic cholangitis due to the residual choledocholithiasis.
TREATMENT
To remove the residual stones, subsequent ERCP was performed, and both CBDs were cannulated successfully under fluoroscopic guidance (Figure 3B). After stone removal, two ENBD tubes were placed separately in both bile ducts to achieve sufficient biliary drainage. Tubography was performed a day after ERCP and did not reveal any definite filling defects suggestive of residual stones in either CBD (Figure 3C).
OUTCOME AND FOLLOW-UP
The patient was discharged after resolution of cholangitis, and is being followed up for 9 mo after the procedure without recurrence of cholangitis.
DISCUSSION
DCBD is an extremely rare congenital anomaly of the biliary system. Since Vesarius first reported it in 1543, only 24 cases had been reported in the western literature until 1986[3]. However, cases of DCBD are reported more often in the eastern literature. A total of 47 patients reported in the Japanese literature were reviewed by Yamashitaet al[4]in 2002; furthermore, Chenet al[5], reported 24 Chinese cases in 2014.
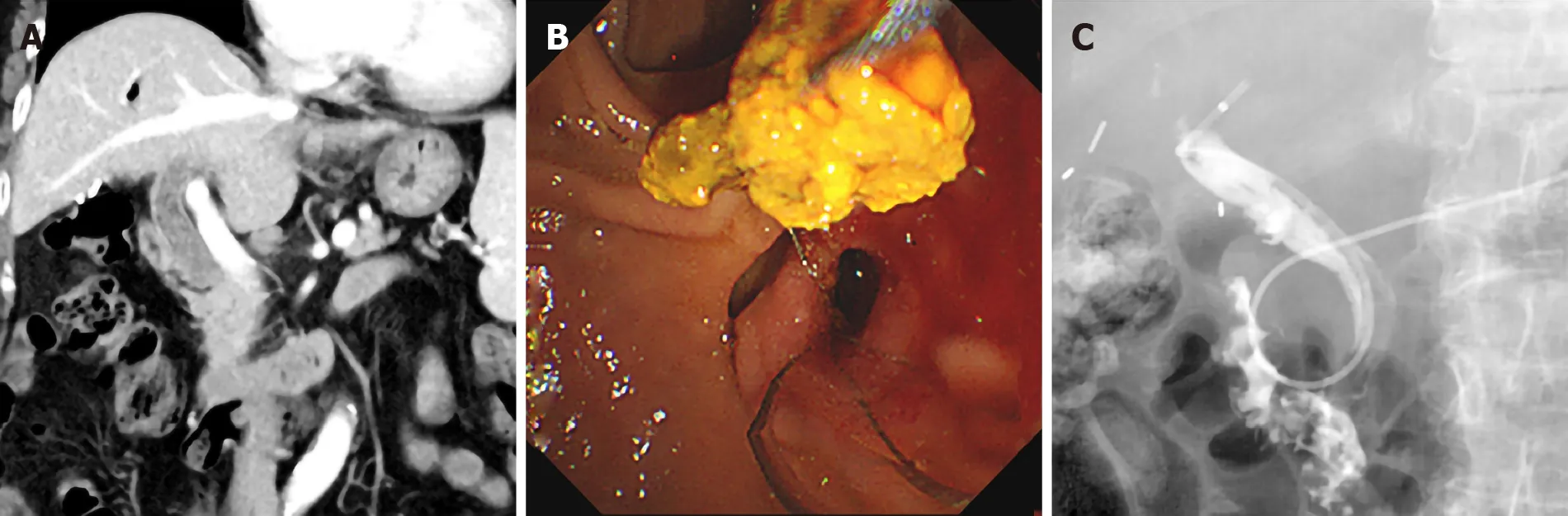
Figure 1 Computed tomography imaging and endoscopic retrograde cholangiopancreatography. A: Computed tomography revealed multiple stones in the common bile duct; B: Stones were removed by Endoscopic retrograde cholangiopancreatography using a Dormia basket; and C: Follow-up tubography using an endoscopic nasobiliary drainage showed no definite filling defects in the common bile duct.

Figure 2 Computed tomography imaging and endoscopic retrograde cholangiopancreatography. A: Follow-up computed tomography demonstrated choledocholithiasis in the extrahepatic bile duct draining the right lobe of the liver; B: An impacted stone was identified at the ampulla of Vater.
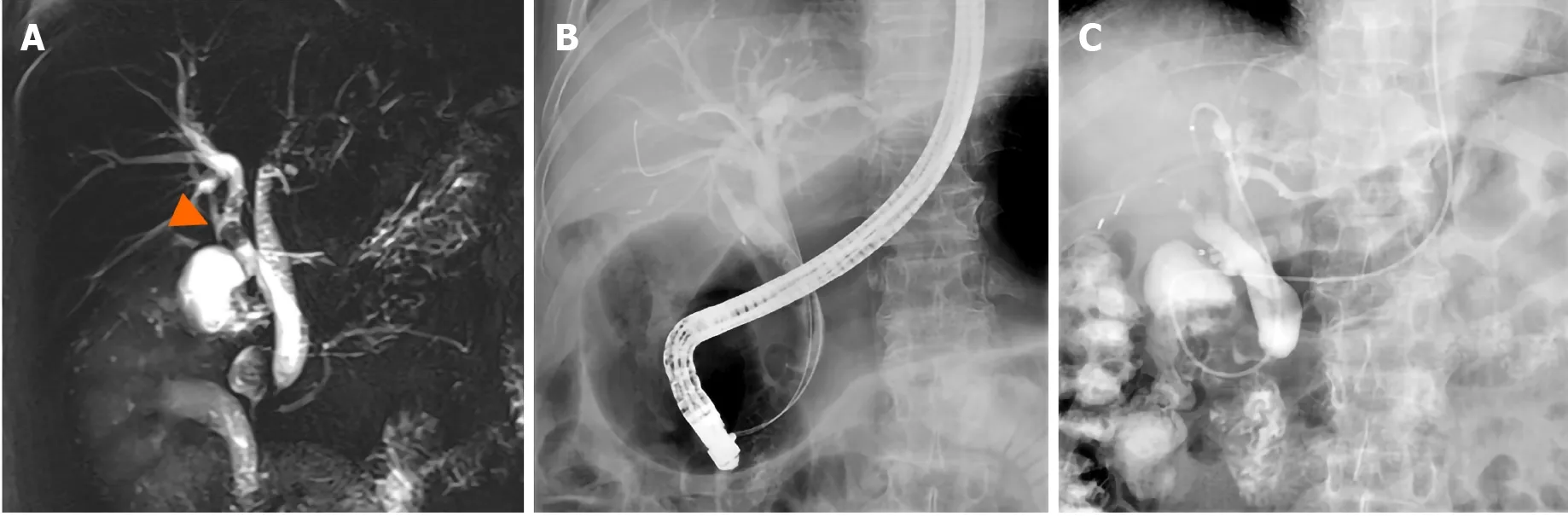
Figure 3 Magnetic resonance cholangiopancreatography. A: Magnetic resonance cholangiopancreatography showed duplicated common bile duct (CBD) independently draining the left and the right robes of the liver, to create a short segment intrapancreatic CBD without communicating channel. Residual stones were identified in the right CBD (white arrowhead); B: Both CBD was accessed using guidewire on Endoscopic retrograde cholangiopancreatography; and C: No definite filling defects were identified in both CBD on tubography using an endoscopic nasobiliary drainage.
The mechanism of this biliary system anomaly is considered to be due to an abnormality during embryogenesis. The presence of two bile ducts is normal anatomically during early human embryogenesis[6]. However, failure of the second bile duct to regress results in the persistence of an accessory extrahepatic bile duct[1].
Morphological classification of this anomaly was first suggested by Gooret al[7]. Goor’s classification was revised by Saitoet al[2], and recently Choiet al[1], modified it by adding a Type V, which is characterized by single drainage of the extrahepatic bile ducts. According to the classification by Choiet al[1], the types of DCBD are as follows: Type I, CBD divided by septum; Type II, CBD bifurcates at the distal end and drains into each opening independently; Type III, duplicated biliary drainage with (Type IIIa) or without (Type IIIb) intrahepatic communicating channels; Type IV, duplicated biliary drainage with one or more communicating channels; Type V, duplicated extrahepatic bile duct rejoined as a single drainage with (Type Va) or without (Type Vb) communicating channels (Figure 4). Our case corresponds to Type Va in the classification by Choiet al[1].
Very few cases of DCBD Type V have been reported. Ever since Choiet al[1]reported the first case of DCBD Type V, only 7 cases have been reported[8]. To the best of our knowledge, this patient is the eighth case of DCBD Type V to be reported. Among the previously reported cases, 5 cases were diagnosed with choledocholithiasis[3,8-11]. There were 2 cases[9,11]that had choledocholithiasis in both extrahepatic bile ducts; one underwent surgery as the stones were not completely removed using ERCP[11], and another case successfully underwent stone extraction in one session of ERCP[9]. In our case, the patient presented with recurrent pyogenic cholangitis because a DCBD was not initially suspected due to the rarity of the anomaly. Therefore, two sessions of ERCP were needed to remove all choledochal stones in this case.
MRCP is the examination of choice to evaluate the anatomy of the biliary tree and its variations[12]. It has several advantages over ERCP such as (1) non-invasiveness; (2) no radiation hazard; and (3) less operator dependence[13]. It also has advantages over CT; it does not require intravenous contrast media and provides comprehensive anatomy of the biliary tract in a single image due to its capability to acquire images in any desired plane[14]. As very few biliary endoscopists and radiologists have ever encountered DCBD even in high-volume centres[9], in this case, the right CBD was mistaken for a residual cystic duct on initial CT because the patient had already undergone cholecystectomy. However, the precise anatomy of CBD was clarified through MRCP, and this extremely rare congenital anomaly could be diagnosed. Therefore, MRCP should always be considered in patients with suspected biliary tract anomalies.
Despite the extremely rare nature of this condition, it is crucial to consider the possibility of this congenital anomaly. Gooret al[7]reported a case of inadvertent transection of the CBD during laparoscopic cholecystectomy because of the failure to recognize the presence of DCBD. It is substantial to establish complete stone clearance during ERCP, because residual stone is a probable risk factor for recurrent cholangitis[15]. Although we performed ENBD to confirm the residual stones, the stones in the ancillary bile duct were completely concealed because only one of the two CBDs was assessed during the index procedure. It may be quite challenging to access both bile ducts in a DCBD Type V because it shares a short segment of the draining duct. In a case reported by Kimet al[11], stones in the right CBD were extracted surgically owing to inadequate access to the right duct. Although only one duct was accessible initially in our case, we were able to successfully cannulate both bile ducts after recognizing DCBD.
CONCLUSION
We herein report an extremely rare case of duplication of the extrahepatic bile duct Type V associated with recurrent cholangitis. Although this condition is rare, it is very crucial for biliary endoscopists to be aware of this disease because choledocholithiasis in the unrecognized ancillary bile duct can significantly affect the prognosis of patients.
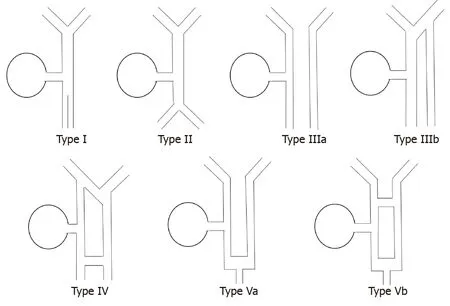
Figure 4 Illustration of Choi’s double common bile duct classification.
杂志排行
World Journal of Gastroenterology的其它文章
- Pleiotropy within gene variants associated with nonalcoholic fatty liver disease and traits of the hematopoietic system
- Preoperative maximal voluntary ventilation, hemoglobin, albumin, lymphocytes and platelets predict postoperative survival in esophageal squamous cell carcinoma
- Clinic-pathological features of metabolic associated fatty liver disease with hepatitis B virus infection
- Effect of remote ischemic preconditioning among donors and recipients following pediatric liver transplantation: A randomized clinical trial
- Could saline irrigation clear all residual common bile duct stones after lithotripsy? A self-controlled prospective cohort study
