Endoscopic mucosal ablation - an alternative treatment for colonic polyps: Three case reports
2021-01-15AntonioMendozaLaddJoaquinEspinozaCesarGarcia
Antonio Mendoza Ladd, Joaquin Espinoza, Cesar Garcia
Abstract
Key Words: Endoscopy; Mucosal ablation; Colon polyp; Argon plasma coagulation; Alternative; Safe; Case report
INTRODUCTION
Endoscopic mucosal resection (EMR) and/or endoscopic submucosal dissection (ESD) is now the standard of care for non-dysplastic, dysplastic and early malignant lesions of the gastrointestinal tract. Thesine qua nonof these techniques is the adequate formation of a submucosal cushion prior to resection, in order to avoid damage of the muscularis propria and hence, perforation. However, these resection techniques require rigorous training, are prone to complications and are not always available at all centers. Recently the submucosal cushion principle has been adopted in the management of dysplastic Barrett’s esophagus (BE) prior to ablation with argon plasma in a technique called Hybrid APC[1]. We explored this concept in the management of 3 flat colonic polyps.
CASE PRESENTATION
Chief complaints
All patients presented in this case series had colon polyps requiring treatment.
History of present illness
All three patients originally presented to their gastroenterology providers for routine colon cancer screening or surveillance and were referred to our endoscopy center.
History of past illness
Case 1:Hypertension (HTN), DM2.
Case 2:DM2, HTN, hypercholesterolemia and treated tuberculosis.
Case 3:Hypercholesterolemia and osteoarthritis.
Imaging examinations
Case 1:An 85 y/o M with previous medical history (PMH) described above was referred for evaluation of a cecal polyp. Colonoscopy revealed a 4 cm 0-IIa +Is lesion in the cecum that involved the IC valve (Figure 1A). Due to morphology of the lesion and the risk of incomplete resectionviaEMR (we did not perform ESD at our center at the time), removal was not attempted. The lesion was biopsied and pathological analysis established it was a tubular adenoma with no dysplasia. The patient was offered referral to an outside facility for ESD. However due to his lack of medical insurance, referral was not a possibility. Therefore, endoscopic mucosal ablation (EMA) was offered. After detailed explanation of the potential risks and benefits, he agreed to the procedure. The colonoscopy was repeated 2 mo later. The lesion was injected with a mix of O’rise gelTM(Boston Scientific, Natick, MA, United States) + epinephrine at 1:10000 to create the submucosal cushion. The lesion raised easily. Once raised, ablation of the lesion was performed using Argon Plasma Coagulation in forced coagulation mode at 1 L/min, 60 W, effect 2 (Video). The patient did well and was discharged the same day of the procedure. Colonoscopy 1 year later showed a scar with no evidence of polyp recurrence (Figure 1B). Biopsies of the scar confirmed eradication of the lesion.
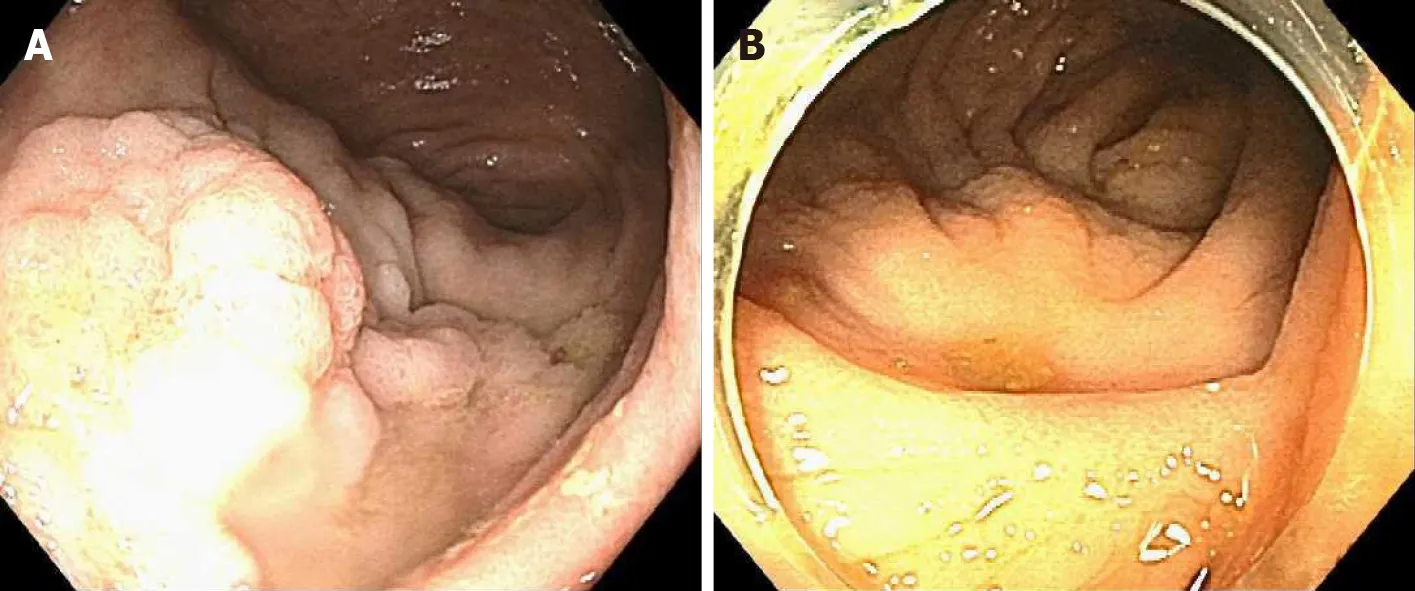
Figure 1 Colonoscopy. A: 0-IIa +Is lesion in the cecum involving the IC valve; B: Post endoscopic mucosal ablation scar.
Case 2:This was a 69 y/o M with PMH described above who was referred for removal of polyp recurrence after a previous EMR. Colonoscopy showed a 0-IIa lesion of approximately 3 cm at the previous EMR scar in the hepatic flexure (Figure 2A). The lesion was biopsied prior to ablation. After the biopsy, EMA was performed in a similar manner as in case 1 (video). The biopsy of the lesion revealed a tubular adenoma with no dysplasia. Colonoscopy at 11 mo showed a healthy scar with no signs of polyp recurrence (Figure 2B). Biopsy of the scar confirmed eradication.
Case 3:A 79 y/o F with a PMH described above was referred for evaluation of a flat polyp. Colonoscopy revealed a 2 cm 0-IIa lesion in the hepatic flexure (Figure 3A). The lesion was biopsied prior to ablation. Ablation ensued as described above (video). Biopsy of the lesion revealed tubular adenoma features with no dysplasia. Colonoscopy 13 mo later revealed a healthy scar with no polyp recurrence (Figure 3B). Biopsy of the scar confirmed eradication.
FINAL DIAGNOSIS
All patients were diagnosed with TA with no dysplasia.
TREATMENT
All patients were treated with the EMA technique.
OUTCOME AND FOLLOW-UP
All patients had follow-up colonoscopy at 1 year and biopsy of the ablation site revealed no evidence of recurrence.
DISCUSSION
EMA is a combination of established resection and ablation techniques already utilized in different sections of the GI tract. The EMA technique has been previously applied successfully in gastric lesions. Kothariet al[2]successfully treated a flat dysplastic lesion at the GJ anastomosis of a patient with a previous Roux-en-Y gastric bypass[2]. Estifanet al[3]also obtained adequate results using EMA to treat lesion recurrence after an ESD for intestinal metaplasia in the incisura[3]. The only available report of the application of this technique in the colon was published by Tsiamouloset al[4]. In contrast to ours, this case series included only recurrent lesions after prior endoscopic resection. They reported no complications and a recurrence rate of 82% at one year.

Figure 2 Colonoscopy. A: 0-IIa lesion in previous endoscopic mucosal resection site in hepatic flexure; B: Post endoscopic mucosal ablation scar.

Figure 3 Colonoscopy. A: 0-IIa lesion in the hepatic flexure; B: Post endoscopic mucosal ablation scar.
When utilizing EMA, a natural concern is the risk of complications such as perforation. However, studies in porcine models have demonstrated that ablation with argon plasma does not cause injury to the musclularis propria when a submucosal cushion is created[5,6]. This finding led to the novel technique of Hybrid APC. In this technique, a submucosal cushion is created and the affected mucosa is ablated. This technique has been applied in the treatment of BE and has shown promising results[1].
The advantages of EMA include its simplicity, safety and its availability in most community endoscopy centers. The main disadvantage is that it does not produce a surgical specimen for pathological analysis. Although previous biopsy of the lesion can give preliminary information about the histology, it may not reflect that of the entire lesion. Therefore, endoscopists should only use EMA in colonic polyps when endoscopic resectionviaEMR or ESD is not available. Furthermore, this technique should not be utilized when the preparation of the colon is poor due to the risk of colonic explosion[7,8].
CONCLUSION
To our knowledge, this is the first report of the use of EMA in treatment naïve colonic lesions. We encountered no complications and our recurrence rate at 1 year was 0% with biopsies of the scars confirming eradication in all cases. Our results suggest that EMA is safe and effective in the treatment of colonic polyps when endoscopic resection is not possible or available.
杂志排行
World Journal of Gastroenterology的其它文章
- Chinese guidelines on the management of liver cirrhosis (abbreviated version)
- Altered metabolism of bile acids correlates with clinical parameters and the gut microbiota in patients with diarrhea-predominant irritable bowel syndrome
- Alteration of fecal tryptophan metabolism correlates with shifted microbiota and may be involved in pathogenesis of colorectal cancer
- Relationship between the incidence of non-hepatic hyperammonemia and the prognosis of patients in the intensive care unit
- Tuberous sclerosis patient with neuroendocrine carcinoma of the esophagogastric junction: A case report
- Role of pancreatography in the endoscopic management of encapsulated pancreatic collections – review and new proposed classification
