Co-occurrence of Vitiligo and Psoriasis in an 11-Year-Old Girl: A Case Report
2021-01-09RongLiJiaAnZhangYiQunJiangMinZhiWuKunChen
Rong Li, Jia-An Zhang, Yi-Qun Jiang, Min-Zhi Wu∗, Kun Chen,∗
1Department of Physiotherapy, Hospital for Skin Diseases (Institute of Dermatology), Chinese Academy of Medical Sciences and Peking Union Medical College, Nanjing, Jiangsu 210042, China; 2Department of Dermatology, the Fifth People’s Hospital of Suzhou, Suzhou, Jiangsu 215000, China.
Abstract
Keywords: case report, psoriasis, vitiligo
Introduction
Psoriasis is a chronic inflammatory cutaneous disorder characterized by abnormal epidermal growth and differentiation. The lesions of psoriasis usually present as red,scaly patches,papules or plaques.Vitiligo is a depigmented disorder characterized by progressive epidermal melanocyte destruction. These two diseases affect population by approximately 2% and 0.4%, respectively.1Although these two diseases are really common in skin disorders,the co-occurrence is infrequent. There are some hypotheses related to its pathogenesis like isomorphic reaction,shared genetic basis of autoimmunity and inflammation, shared cellular immune pathways, and so on. Yet none of these theories have been confirmed and they lack the support of large samples.
Here we reported a case of an 11-year-old girl with psoriasis and vitiligo. Our reported case analysis found inner associations between psoriasis and vitiligo that were consistent in different etiology directions.Because psoriasis usually presents as red lesions and has the potential to develop the pale lesion of vitiligo in one patient,clinicians should pay attention to such co-occurrence and prescribe a proper strategy to deal with such patients.Although there have been various speculations that explained its cooccurrence, there is a lack of large epidemiologic population-based studies. The analysis and summary of the underlying association in co-occurrence of psoriasis and vitiligo may amplify future therapeutic options for both diseases.
Case report
An 11-year-old girl developed depigmented patches on her right chin for 6 months.The noticed areas of depigmented skin steadily increased in size with no clinical symptoms.Two months later, due to a cold, various erythematous hyperkeratotic lesions appeared gradually on her face and extremities.She then consulted in our hospital.The patient had no family history of vitiligo and psoriasis,laboratory tests showed no abnormalities.
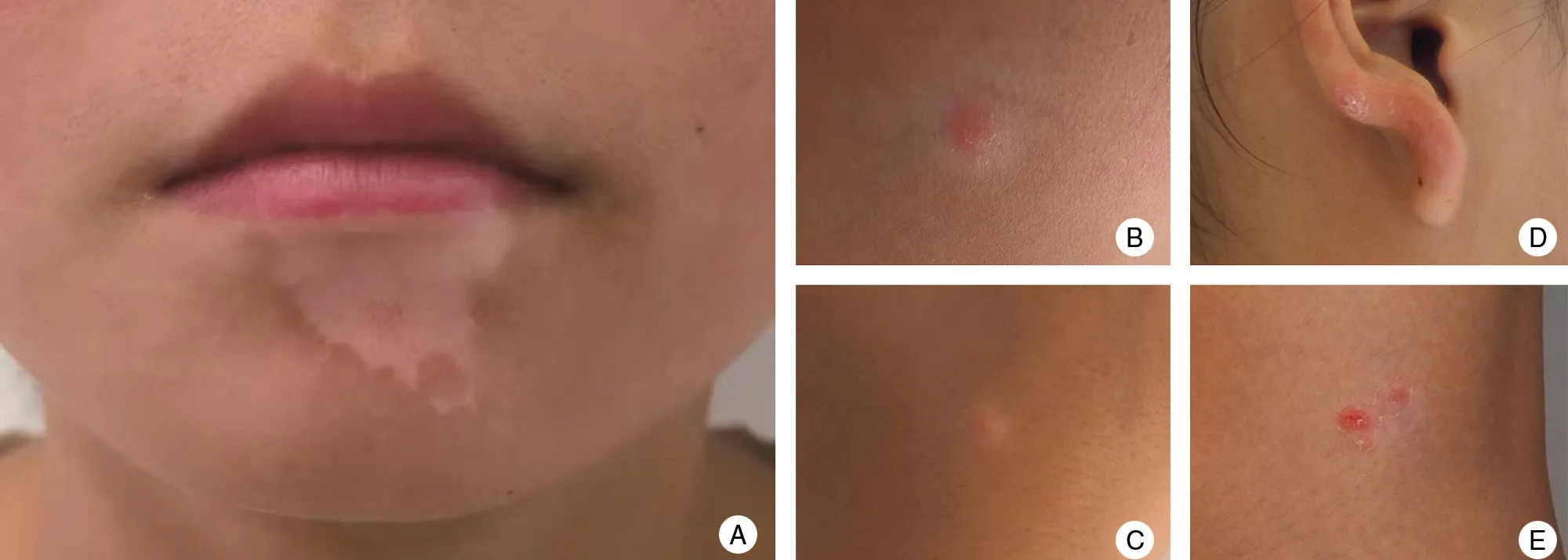
Figure 1. Clinical presentation of psoriasis comorbidity in the patient with vitiligo.Vitiligo lesion on her chin(A)and psoriasis lesions on her right cheek (B), right hand (C), right ear (D), and lower limbs (E).
Physical examination showed no abnormal results.Dermatological examination revealed that irregular shaped and well-defined depigmented patches were observed on her chin (Fig. 1A). Also, scaly erythematous plaques were found on various sites,such as the right cheek(Fig. 1B), the right hand (Fig. 1C), the ear (Fig. 1D), and lower limbs(Fig.1E).All these lesions were positive for the Auspitz sign.The results of laser scanning confocal of the psoriasis lesion on her right hand were as followed(Fig.2):hyperkeratosis, incomplete keratinization, hyperplasia of the epidermis, apical dermal papilla, capillary tortuous dilatation, hyperemia, and peritubular inflammatory infiltration. The depigmented patch on her chin was positive for Wood’s lamp examination (Fig. 3).
Therefore, the clinical diagnosis of co-occurrence of vitiligo and psoriasis was made. Topical agents like tacrolimus and steroids were prescribed for her lesions.After 12 weeks, all of these lesions improved greatly, the patient gave the informed consent for her case report and is still in the follow-up by the current writing.
Discussion
Vitiligo and psoriasis are common diseases in dermatology department, although co-occurrence of psoriasis and vitiligo is rare and the triggers of the co-occurring mechanism are still elusive. In our case, psoriasis was the subsequent lesion following occurrence of the vitiligo lesion after two months.
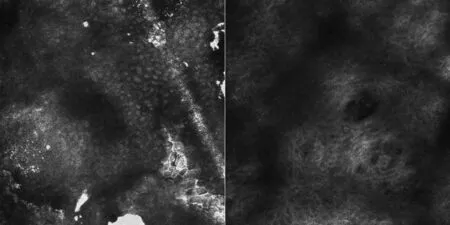
Figure 2. Laser scanning confocal of psoriasis lesions on the right hand of psoriasis comorbidity in the patient with vitiligo.(A)Hyperkeratosis,incomplete keratinization with hyperplasia of the epidermis. (B)Apical dermal papilla and capillary tortuous dilatation.

Figure 3. Wood's lamp examination of the vitiligo lesion on the chin of psoriasis comorbidity in the patient with vitiligo.
Piebaldism is a rare autosomal dominant disorder that should be differentiated from our case. Vitiligo can explicitly be distinguished from piebaldism by characteristics of piebaldism,including congenital,nonprogressive,patchy absence of pigmentation of the skin (leukoderma)and overlying hair(poliosis)due to lack of melanocytes in the affected regions.1In this reported case,the girl has no family history of piebaldism and the depigmented patches on her chin developed postnatally and soon progressed during the course.
Patients who presented with initial psoriasis with subsequent lesions of vitiligo have also been reported since 1955,2-14but some researchers argued that these phenomena may have been caused by chance.Such give a hint that these two diseases may have a similar mechanism in its etiology, yet its association is still elusive. Many explanations of co-occurrence of vitiligo and psoriasis have been implicated in the etiology,which can be mainly divided into three ways: (1) isomorphic reaction, (2)shared genetic basis of autoimmunity and inflammation,and(3)shared cellular immune pathways,including Th1,Th17, and related cellular molecules such as tumor necrosis factor (TNF)-α, interferon (IFN)-α,and interleukin (IL)-17. Related articles are summarized in Table 1.
In terms of environmental conditions, one of the most impressive factors is that the trauma could cause isomorphic reaction in both diseases.3Yet only if these two diseases presented simultaneously could support that it is isomorphic reaction that plays a role in its cooccurrence.The presentation of vitiligo in our patient was two months earlier than psoriasis,and the patient did not feel pain before the occurrence of vitiligo, so such speculation may not explain this phenomenon well.
The co-occurrence of psoriasis and vitiligo can also be explained by a common genetic basis for autoimmunity and inflammation. In the cytoplasm, inflammasome multiprotein complexes may activate proinfammatory cytokines to influence the co-occurrence of psoriasis and vitilige.11Yen et al.1found that there were increasing evidence of genetic predisposition to various autoimmune diseases in their genome-wide association studies. Marie et al.5reported that inflammasome markers had been identified in the skin of patients with co-occurring psoriasis and vitiligo, which indicated that inflammasome-related genetic sequence variants had significant association with the psoriasis in generalized vitiligo patients.Some authors also found that co-occurrence of these two diseases was related to systematic diseases like cardiovascular diseases.6A recent case-control study showed that a positive family history of cardiovascular disease could be a strongly implicative factor in the co-occurrence of vitiligo and psoriasis.7The relevance between the cardiovascular risk factors and skin diseases perhaps could be explained by a shared genetic susceptibility. The nucleotide polymorphisms of the classical human leukocyte antigen gene are shared in vitiligo and psoriasis, and the same locus of thehistocompatibility complex may lead to genetic susceptibility.12What’s more, a range of theories have been proposed to explain the co-occurrence of the two diseases,mostly related to autoimmune conditions.1,8-9Patients of concomitant disease often reported with arthritis and thyroiditis, which suggests that autoimmune disorders may induce the development of these diseases.
The third mainstream explanation is related to a shared cellular immune pathways in psoriasis and vitiligo,including Th1 and Th17. TNF-α may play an important role in the pathogenesis of diseases via Th1- and Th17-mediated autoimmune inflammation of the skin. TNF-α had already been testified in psoriasis. Recently, some evidences have indicated that it also affected the recession of vitiligo. Etanercept, a kind of TNF-α inhibitor, was effective in treatment of psoriasis and was also prescribed for several cases of vitiligo.1,7A patient with psoriasis confined to vitiligo area received the treatment of 50mg twice a week for 12 consecutive weeks and then 25mg for the subsequent 12 weeks.After the treatment,his lesions of psoriasis greatly improved and vitiligo lesions also showed a sign of decreasing and repigmentation.13Such a clinical application demonstrated that TNF-α could serve as a key element in inflammatory cascade in psoriasis and induce the activation of B-cells that produce autoantibody damaging the melanocytes.1,8,14Besides, evidences that support IFN having a role in its pathogenesis have also been found. Several psoriasis cases related to IFN-α-2a have been reported1and theories like IFN-α-2a could promote the development of vitiligo via autoantibodies or cytotoxic T-cells have also been speculated. A convincing example of this was a 10-year-old girl with hepatitis B infection,who took IFN-α-2a(3 MU,three times a week)and gradually developed psoriasis and vitiligo.Even if she stopped the administration of IFN-α-2a,these lesions still presented.13But its definite association was not clear and some researchers also suspected that it was just a coincidence.14Furthermore, IL-17A may also contribute to its developments. Anti-IL-17A monoclonal antibody like secukinumab had been effectively applied in the treatment of psoriasis8and the level of IL-17 was elevated in the group of vitiligo patients compared with normal groups.6Thus,it is perhaps a molecule that affects the cooccurrence of these two diseases.
In terms of treatment, steroid-containing ointments or immunosuppressants like tacrolimus ointments that could be prescribed for these two diseases and narrowband ultraviolet B phototherapy treatment all have a good therapeutic response in these two diseases. Meanwhile,Damsky et al.10reported that tofacitinib, which was an inhibitor of the Janus kinase (JAK), had positive effect in the treatment of both psoriasis and vitiligo. Tofacitinib could block stimulation of Th17 cells to reduce the production of IL-17 in psoriasis by inhibiting JAK/STAT signaling pathway-dependent cytokines. In vitiligo patients, tofacitinib could mediate IFN-γ and the JAKSTAT pathway to reduce the targeted destruction of melanocytes caused by T cells.1Such an application of tofacitinib demonstrated that it may be a promising initial remedy in both diseases.
In summary, we reported a patient with the cooccurrence of psoriasis and vitiligo, which is rarely seen and sometimes may serve as a hint of systematic disease.Although there had been various speculations that explained its co-occurrence, some authors believed it was just a coincidence because there is a lack of large epidemiologic population-based studies. Hence, further investigations are needed to determine whether such condition is just a coincidence or not.Once such patients are encountered,a comprehensive analysis and evaluation of the patient and a proper treatment strategy should be applied.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (No. 81872545) and Introduction Project of Suzhou Clinical Medical Expert Team(No.SZYJTD201811).
杂志排行
国际皮肤性病学杂志的其它文章
- Instructions for Authors
- Platelet-Rich Plasma for Androgenetic Alopecia in Women: A Single-Center Case Series Study in Qatar
- Intracranial Abnormalities of Infantile Hemangiomas in the Head and Neck Regions:A Retrospective MRI Study
- Efficacy and Safety of Prednisolone Monotherapy Versus Prednisolone Plus Methotrexate in Erythema Nodosum Leprosum(Type 2 Lepra Reaction)
- The Past 70 Years in Control of Syphilis in China: Elimination and Responses to Resurgence
- Hair Matrix Cyst